INTRODUCTION
Sugar sweetened beverages (SSBs) are the number one source of added calories from sugar in the Western diet. SSB intake doubled in the US over the last 30 years and is currently the single largest contributor to daily caloric intake (Popkin, 2010; Welsh, Sharma, Grellinger, & Vos, 2011). The average American consumes nearly 45 gallons of SSBs a year – the equivalent of 39 pounds of extra sugar annually (Babey, Jones, Yu & Goldstein, 2009). SSBs contribute to obesity and other chronic diseases including Type-2 Diabetes, heart disease and hypertension (Berkey, Rockett, Field, Gillman & Colditz, 2004; Centers for Disease Prevention [CDC], 2010).
Expenses related to overweight and obesity accounted for an estimated 27% of the growth in healthcare expenditures between 1987 and 2001; these costs are projected to double every decade and to make up 16–18% of total US health-care costs by 2030 (Wang et al., 2011). Healthcare institutions across the nation recognize the urgent need to facilitate and contribute to the reduction of obesity. A recent comprehensive review of the literature concludes that there is sufficient evidence that reducing SSB consumption will decrease the prevalence as well as the risk of obesity and related diseases, especially Type 2 Diabetes (Hu, 2013).
The Centers for Disease Control and Prevention (CDC) recommends specific strategies for the reduction of SSBs for obesity prevention in priority settings, including medical care facilities. Recommended strategies include limiting access to SSBs, promoting access to and consumption of more healthful alternatives to SSBs, and decreasing the relative cost of more healthful beverages (CDC, 2010; CDC, 2009).
BACKGROUND
Hospital interventions to reduce the sale of SSB consumption by educating employees, patients and families are important because hospitals serve as role models for the community. To date, there are only two studies that evaluated hospital-based educational interventions to reduce the sale of SSBs – both conducted at Boston area hospital cafeterias. The first, a multi-phased intervention including an educational campaign and price increase of SSBs followed by a combination of the two, showed a significant decrease in sales of regular sodas (Block, Chandra, McManus, & Willett, 2010). The second study was a two-phase six-month intervention that included a complex food and beverage rating system, point of purchase color-coded labeling, menu redesign and a choice architecture intervention to increase visibility and convenience of healthy items in the cafeteria. The results of this study showed an increase in the sale of healthy beverages (and foods) compared to less healthy items (Thorndike, Sonnenberg, Riis, Barraclough, & Levy, 2012). A longitudinal follow-up study at the same hospital found that the sale of healthier foods and beverages was maintained for 24 months after the initial intervention, indicating that changes in the food environment can potentially promote longer term behavior change (Thorndike, Rils, Sonnenberg, & Levy, 2014).
Although these studies suggest that it is possible to decrease purchasing of SSBs, these interventions were conducted in the context of multi-phase, fully-funded research studies. Considering that SSBs constitute a large portion of the average American’s caloric intake, it may be prudent for hospitals with limited resources and a desire to prevent obesity to begin by implementing strategies aimed at decreasing the sales of SSBs. Thus, the purpose of the current study was to examine whether an intervention focused specifically on limiting access to SSBs and promoting consumption of more healthful drinks could reduce the sales of SSBs while maintaining overall beverage sales in a hospital setting. Further, this article outlines best practice strategies by sharing the process that informed the Rethink Your Drink campaign at Rady Children’s Hospital in San Diego, California (RCHSD).
METHODS
Formative Research
The Wellness Committee at RCHSD identified the reduction of SSBs as a priority and began initial planning of a hospital-wide initiative. Knowing the project would have greater visibility and a higher chance of success when it was supported by hospital’s executive leadership, the committee’s first step was to establish organizational support. In 2012, RCHSD executive leadership set an operational goal for the upcoming fiscal year to reduce the sales of SSBs within the hospital. Upon approval of the goal, a small Working Group (SSB WG) was created to conduct formative research, plan, implement and evaluate the program. Champions were identified from key departments to join the SSB WG, including a Program Manager from the Community Health Department, the Food Services Director, a Registered Dietician and a Communications department representative. With no dedicated staff and very limited resources, this group met weekly and recruited two interns to assist with planning and implementation.
Initially, the SSB WG reviewed the literature including best practice publications and toolkits specifically related to strategies for SSB reduction (CDC, 2010; Boston Public Health Commission, 2011; Healthier Hospitals Initiative, 2012). Next, the group identified other hospitals that had successfully implemented programs and strategies to reduce SSBs. Key informant interviews were conducted with leaders of these programs. Case studies were then developed for more than 12 hospitals across the country, summarizing their approach (education, environmental and policy modifications); resources developed; greatest challenges and successes; data collection systems; and outcomes. About half of the hospitals reviewed had completely eliminated SSBs and the other half chose to focus on reduction of SSB purchasing.
An important next step was to establish a high level Advisory Team with representation from a broad range of departments as well as executive leadership to provide feedback and support to the SSB WG and assist with operational decisions as needed. The Advisory Team included the SSB WG and representatives from nursing, pharmacy, gift shop, dietary services, medical groups, marketing, human resources and executive leadership. Upon review of the case study and formative research, the Advisory Team solicited feedback from employees to determine whether to eliminate or to reduce SSBs within the hospital.
Employee Survey
A ten-question survey was developed to assess employee SSB consumption, attitudes about SSBs, and perceptions of health effects of SSBs. The survey was distributed via email to all 4,500 hospital employees with an incentive of inclusion in a lottery for a $50 gift card after completing the survey. Thirty percent of the surveys were returned (1,328 surveys). Results showed that 76.4% of respondents reported consuming less than three SSB drinks in the past seven days and only 23.6 % reported consuming at least one or more SSBs per day. Interestingly, 60% of respondents “strongly disagreed” with the statement “SSBs have no negative health effects on those who drink them regularly” and 70% “somewhat” or “strongly agreed” with the statement “employees of children’s hospitals should set a positive health example for the patients they treat.” Furthermore, 87% “somewhat” or “strongly agreed” with the statement “education and public messaging is the best way to encourage less consumption of SSBs” and 88% “somewhat” or “strongly agreed” with the statement “Rady Children’s should model healthy lifestyle by increasing healthy drink options.” The survey included an open-ended question asking employees to use the space to “share any additional thoughts regarding SSBs at RCHSD.” A total of 229 respondents included comments in this section; of those, approximately 35% were related to the idea that employees should be allowed the choice of SSBs.
Intervention Planning and Development
After consideration of the formative research findings and the employee survey, the Advisory team decided to decrease SSB options, increase non-SSBs options and focus the intervention on educating employees about making healthy drink choices. The team decided to utilize a similar stoplight approach to that outlined in the Healthy Beverage Toolkit published by the Boston Public Health Commission, whereby all drinks are color coded as “red”, “yellow” or “green” based on sugar content. This intervention was named “Rethink Your Drink (RYD)”, and was implemented over 12 months and evaluated to determine its effectiveness to reduce sales of SSBs relative to non-SSBs.
Classification of drinks as Red, Yellow and Green
The stoplight labeling system was chosen to emphasize education with drinks labeled as red (high in sugar or SSBs defined as over 12 grams of sugar per 12 ounces); yellow (low in sugar or artificially sweetened defined as 6 to 12 grams of sugar per 12 ounces or contains artificial sugar); or green (no added sugar and no sweeteners defined as 0 to 5 grams of sugar per 12 ounces). In addition, some drinks were identified as “other” and included beverages into which sugar could be added after purchasing and therefore were not coded by color. These drinks were mostly hot beverages, including coffee, tea, and hot water. The hospital’s Communications Department designed a customized stoplight graphic to be used on all collateral materials based on the criteria established.
Data collection
Prior to baseline, cash registers were programmed to code beverages sold as red, yellow, green or other. Daily product mix reports captured information, which was entered into a spreadsheet for data analyses. Protocols were developed to train cashiers to ask about the content of self-serve fountain drinks for which content could not be assessed visually. To reduce bias, cashiers and customers (via prompts at the cash registers) were told that the department was conducting a study to assess customers’ drink preferences. For coding fidelity, quality checks were conducted during the baseline period in the form of secret shoppers at least twice per month at each location, discrepancies reported to the Director of Nutrition Services and retraining implemented as needed to ensure compliance.
Data was collected at locations where beverages were sold at Rady Children’s Hospital, including the main cafeteria, delicatessen, hospital grab & go, Starbucks cart and patient room service. Data was collected using an ABA design; three-month baseline period, 12-month intervention, and four months post-intervention. Descriptive data was collected including number of items of each beverage color sold each month and the percentage of total beverage sales these purchases represented.
Intervention
In October 2012, the RYD campaign was launched at RCHSD in San Diego, California and continued through September 2013. RCHSD provides care to more than 192,000 children annually. The hospital cafeteria is open to hospital employees, physicians, patients and visitors seven days a week, accounting for approximately 38,000 transactions per month, 25,000 of those for beverages. The intervention took place at the main hospital cafeteria, delicatessen, hospital grab & go, Starbucks cart and patient room service.
The RYD educational intervention included flyers and point of sale education posters describing the traffic light system (Insert Figure 1 here), table-top tents, and an education handout designed for children. Displays included green beverage tastings, a display which included a wheel barrow holding 40 pounds of sugar (annual sugar intake for a person drinking one daily SSB), and a handmade interactive electronic display where customers could guess what color certain beverages were (Insert Figure 2 here). Displays and drink demonstrations were rotated on a quarterly basis to different areas of the hospital (main cafeteria, delicatessen, hospital lobby and entrance to the acute care pavilion). Environmental changes included repositioning all beverages in coolers in the cafeteria and vending machines so that green drinks were placed at eye level and red drinks placed at the bottom. Also, color coded labels were added to the cafeteria coolers corresponding with the drinks on each shelf. Policy changes included eliminating SSBs from room service menus – although they were provided upon request.
Figure 1.
RYD Poster
Figure 2.

Displays
RESULTS
SSB Sales Data
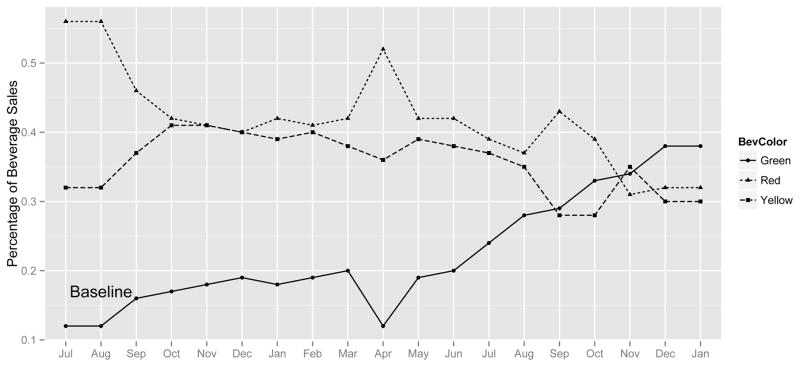
The effect of the intervention on beverage sales over time was examined via linear regression using dummy coded indicators for beverage color with red as the reference group. Drinks labeled as other were not included in the statistical analysis because they were mostly hot beverages and the intervention focused on cold beverages. Table 1A shows the results of the linear regression examining the number of beverages sold over time. During the data collection period, we observed the largest impact in increased sales of green beverages compared to red with a strong interaction noted between number of green beverages sold and time (p<0.001). Table 1B shows the results of linear regression examining the percentage of net sales for each beverage color over time. The percentage of monthly red sales significantly decreased over time (p <0.001) from an average of 56% during the baseline period to 32% at the end of the data collection period. The slope of the change in percentage of red sales is represented by β for the intercept in Table 1B and is positive because red is the reference group, even though the percentage of red sales decreased over time. In contrast, there was a strong interaction between the percentage of monthly green sales and time (p<0.001), with green beverage sales increasing from an average of 12.2% during baseline to 38% at the end of the data collection period. The rate of change in percentage of yellow drinks over time was not significantly different than red (p = 0.05) (see Figure 3). Sales revenue for all drinks has remained constant during this period: average total monthly revenue during the baseline period was $34,624, the average total monthly revenue during the 12-month intervention was $35,390 and the average total monthly revenue during the four-month post-intervention period was $34,955.
Table 1.
Linear regression of sales data over time using Red as reference beverage color
| A: Change in sales of beverages over time | |||
|---|---|---|---|
| Beverage Color | β | Standard Error | P-value |
|
| |||
| Intercept | 6228 | 319 | <0.001 |
|
| |||
| Green | −4689 | 452 | <0.001 |
|
| |||
| Yellow | −475 | 452 | 0.29 |
|
| |||
| Time | −60 | 33 | 0.07 |
| Interaction with Time | |||
|
| |||
| Green × Time | 257 | 47 | <0.001 |
|
| |||
| Yellow × Time | −18 | 47 | 0.7 |
| B: Change in percentage of beverages sold over time | |||
|---|---|---|---|
| Beverage Color | β | Standard Error | p-value |
|
| |||
| Intercept | 0.347 | 0.013 | <0.001 |
|
| |||
| Green | −0.260 | 0.019 | <0.001 |
|
| |||
| Yellow | −0.090 | 0.019 | <0.001 |
|
| |||
| Time | −0.007 | 0.001 | <0.001 |
|
| |||
| Interaction with Time | |||
|
| |||
| Green × Time | 0.014 | 0.001 | <0.001 |
|
| |||
| Yellow × Time | 0.003 | 0.001 | 0.05 |
Note: In the main effects model, the negative sign for the slope of Green beverages indicates this slope is in the opposite direction of Red (the reference group), which has decreasing sales over time
Figure 3.
Percentage of Beverages Sales By Color Over Time
DISCUSSION
Our data demonstrate that a focused intervention in a hospital setting significantly decreased the sales of SSBs (red drinks) and simultaneously led to a significant increase in the sales of non-SSBs, in particular beverages with no sugar or artificial sweetener added (green drinks). The intervention included strategies to educate and encourage consumers to make healthy drink choices as well as simple environmental changes to reinforce those choices. The “Rethink Your Drink” initiative utilized a stoplight system designed to educate consumers about the amount of sugar in common beverages and to physically position beverages in the coolers to encourage healthy choices. Sales data analyzed showed a 36% decrease in the monthly sales of red drinks and a 241% increase in the monthly sales of green drinks from baseline to the end of the data collection period.
Other studies have shown success in decreasing the sale of SSBs in a hospital setting (Block et al., 2010; Thorndike et al., 2012). Our intervention used an ABA design with a 12–month intervention which showed greater decrease in SSB sales than the previous two studies, although direct comparisons can not be made due to methodological and sample differences. This longer intervention phase may account for the greater decrease in SSB sales compared to the other studies and may suggest that longer lasting interventions can result in improved and sustained results. Also, the color coding systems were slightly different, which may have resulted in different proportions of each beverage color at baseline compared to the other studies.
Strengths of this study include a small implementation group, generalization to other community service organizations, and objective sales data. Of note, this intervention was planned and implemented by a small working group with no dedicated staff and very limited resources. This study was unfunded outside of the the time and effort of the RCHSD staff. The simplicity of the intervention and promising results suggest this may provide a model approach for other small hospitals that can be easily replicated. In fact, this initiative has generated interest from other organizations both locally and nationally via requests for consultation, presentations and webinars. Furthermore, local advocate groups have adapted this RYD initiative, including the San Diego County Dental Society and Dental Hygienists Society. Furthermore, membership organizations of a collaboration of local healthcare systems have adopted a healthy beverage standard and the stoplight approach using the RCHSD initiative as a model. Another strength of this study was the ability to collect objective sales and revenue data over an extended period of time as a result of permanent modifications of cash registers to recode beverage sales data.
This study has several limitations that need to be considered. First, there was no control group so we can not definitively conclude that the changes in SSB sales were due to the intervention. Also, differences in methods make it difficult to compare these study results with other studies. For example, diet sodas were coded as yellow in our study and in others were considered green (Thorndike et al., 2010), which could have contributed to the very low percentage of green drinks sold at baseline in this study.
CONCLUSIONS
This is the first study in a hospital setting to document a change in SSB sales utilizing an education intervention implemented by a small workgroup focused on SSBs without modifying price. It may be prudent for other hospitals with limited resources to focus on strategies to decrease SSB intake, and this article can serve as an implementation guide. Simple modifications of cash registers for coding and inputting sales data will facilitate the ability to collect beverage sales data, an objective measure that will allow for assessment of results over time. Considering SSBs are the largest source of added sugar in Americans’ diets, and can account for a large percentage of a person’s daily calorie intake, it is important to develop replicable interventions, such as this one, to reduce consumption of SSBs.
Contributor Information
Phyllis Hartigan, Program Consultant for the Center for Healthier Communities at Rady Children’s Hospital in San Diego, CA.
Dana Patton-Ku, Physician, Division of Pediatric Gastroenterology, Hepatology and Nutrition at Rady Children’s Hospital in San Diego, CA and Post-doctoral Fellow, Department of Pediatrics, University of California, San Diego.
Cheri Fidler, Director of the Center for Healthier Communities at Rady Children’s Hospital in San Diego, CA.
Kerri N. Boutelle, Professor; Pediatrics and Psychiatry, and Director of the Center for Healthy Eating and Activity Research at UCSD.
References
- Babey SH, Jones M, Yu H, Goldstein H. UCLA Center for Health Policy Research. 2009. Bubbling over: soda consumption and its link to obesity in California. [PubMed] [Google Scholar]
- Berkey CS, Rockett HR, Field AE, Gillman MW, Colditz GA. Sugar-added beverages and adolescent weight change. Obesity research. 2004;12(5):778–788. doi: 10.1038/oby.2004.94. [DOI] [PubMed] [Google Scholar]
- Block JP, Chandra A, McManus KD, Willett WC. Point-of-purchase price and education intervention to reduce consumption of sugary soft drinks. American Journal of Public Health. 2010;100(8):1427. doi: 10.2105/AJPH.2009.175687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boston Public Health Commission. Healthy Beverage Toolkit. 2011 Retrieved from: www.bphc.org/whatwedo/healthy-eatingactive-living/healthy-beverages/Documents/HealthyBeverageToolkitFinal.pdf.
- Centers for Disease Control and Prevention (CDC) The CDC guide to strategies for reducing the consumption of sugar-sweetened beverages. Atlanta, GA: CDC; 2010. [Google Scholar]
- Sobush K, Keener D, Goodman K, Lowry A, Kakietek J, Zaro S. Recommended community strategies and measurements to prevent obesity in the United States. US Department of Health & Human Services, Centers for Disease Control and Prevention; 2009. [PubMed] [Google Scholar]
- Healthier Hospital Initiative. Healthier Foods: How to Guide. 2012 Retrieved from http://healthierhospitals.org/sites/default/files/IMCE/public_files/hhi-howto-foods-final.pdf.
- Hu FB. Resolved: there is sufficient scientific evidence that decreasing sugar-sweetened beverage consumption will reduce the prevalence of obesity and obesity-related diseases. Obesity Reviews. 2013;14(8):606–619. doi: 10.1111/obr.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popkin BM. Patterns of beverage use across the lifecycle. Physiology & behavior. 2010;100(1):4–9. doi: 10.1016/j.physbeh.2009.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorndike AN, Sonnenberg L, Riis J, Barraclough S, Levy DE. A 2-phase labeling and choice architecture intervention to improve healthy food and beverage choices. American Journal of Public Health. 2012;102(3):527–533. doi: 10.2105/AJPH.2011.300391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorndike AN, Riis J, Sonnenberg LM, Levy DE. Traffic-light labels and choice architecture: promoting healthy food choices. American journal of preventive medicine. 2014;46(2):143–149. doi: 10.1016/j.amepre.2013.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. The Lancet. 2011;378(9793):815–825. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. The American journal of clinical nutrition. 2011;94(3):726–734. doi: 10.3945/ajcn.111.018366. [DOI] [PMC free article] [PubMed] [Google Scholar]