Abstract
Background:
We aim to compare the degree of pain control and complications in three types of anesthesia using periprostatic nerve block (PPNB) plus intrarectal local anesthesia (IRLA), low-dose spinal anesthesia, and intravenous (IV) sedation in patients undergoing transrectal ultrasound (TRUS)-guided prostate biopsy.
Materials and Methods:
In this clinical trial study, 106 patients were participated from December 2015 to December 2016 at Alzahra Hospital, Isfahan, Iran. Patients were randomly allocated into three groups to receive PPNB plus IRLA (n = 36), low-dose spinal anesthesia (n = 35) and IV sedation (n = 35) before TRUS-guided prostate biopsy. Pain scores were recorded using a 10 point visual analog scale right after the biopsy was done. Early and late complications were assessed using a questionnaire after the procedure and in follow-up of patients.
Results:
Overall, the pain score in the low-dose spinal anesthesia group was significantly lower than PPNB plus IRLA and IV sedation groups (P < 0.001). The differences in pain scores between PPNB plus IRLA group and IV sedation group were not significant (P = 0.30). Urinary retraction and fever were significantly more frequent in low-dose spinal anesthesia and IV sedation, retrospectively (P = 0.04, P = 0.03). No significant difference in late complications was found among the groups.
Conclusion:
This study demonstrates that low-dose spinal anesthesia is superior to PPNB plus IRLA and IV sedation in terms of pain controlling and was associated with higher tolerance of the examination and patient comfort.
Keywords: Intravenous sedation, nerve block, pain, prostate biopsy, spinal anesthesia, trans rectal ultrasonography
INTRODUCTION
Transrectal ultrasound (TRUS)-guided prostate biopsy is a gold standard method for diagnosis of prostate cancer.[1] Pain during biopsy procedure is mainly caused by two component, initially probe insertion and manipulation in to the anal canal, then, peneteration of needle in prostate texture.[2] Adequate probe manipulation is necessary to obtain enough samples from different parts of prostate spatially the far-lateral region and the apical region which are usually missed in the first biopsy.[3,4] Therefore, to achieve an effective biopsy procedure and increase rate of cancer detection probe manipulation is necessary which lead to more patient discomfort.[5,6] Hence, better pain relieving resulted in increased cancer detection rate.
Despite using different anesthetic agents and method still patients report different degrees of pain and discomfort.[2,7] Hence, evaluating pain control ability of each method is an important goal help to benefit available methods (more effectiveness) in a more effective manner.
In a recent review, Yan et al. concluded that the combination of periprostatic nerve block (PPNB) and intrarectal local anesthesia (IRLA) is the most effective method in pain refining.[8] Several other studies, similarly recommend using PPNB for all patients undergoing TRUS biopsy.[9,10,11]
On the other hand, some authors believe that periprostatic blockade cannot reduce pain during prostate biopsy properly.[12,13]
Moreover, there are numerous controversial reports on efficacy of IV sedation and spinal anesthesia.[14,15,16,17]
According to these controversies in literatures, we designed this study to compare the efficacy of pain control and complications of these three anesthetic methods which are widely used during prostate biopsy to determine the most effective method.
MATERIALS AND METHODS
Patients and study design
One hundred and ten patients who underwent TRUS-guided prostate biopsy from December 2015 to December 2016 at Al-Zahra Hospital were included in this prospective randomized clinical trial study.
The indication for biopsy was abnormal prostatic findings on digital rectal examination (DRE) or imaging, and/or increased serum prostate-specific antigen (PSA). Exclusion criteria included coagulopathy, anticoagulation/antiplatelet therapy, using tricyclic antidepressants or monoamine oxidase inhibitors drugs, active anorectal pathology, abnormal urine analysis, chronic prostatitis and allergy to local anesthetics.
Study design and purpose were explained to all participants. Each participant was giving and signed a written informed consent.
They were then randomized by a computer generated schedule to undergo TRUS-guided prostate biopsy using PPNB plus IRLA (Group 1), low-dose spinal anesthesia (Group 2), and IV sedation (Group 3). The research protocol approved by regional Ethics Committee of Isfahan University of Medical Sciences with the registration number of 395590.
Biopsy technique and anesthesia
All the patients received 500 mg ciprofloxacin 24 h before and 2 h before the prostate biopsy and continued for 4 days after procedure, twice a day.[12]
In the lateral decubitus position, DRE was performed for all patients before ultrasound probe Insertion to evaluate nodularity and prostate size.
The TRUS-guided biopsies were performed using a biplanar 7.5 MHz probe, and 12 biopsy samples were taken from each patient using an 18G biopsy needle.
In Group I (PPNB plus IRLA), patients received 10 ml lidocaine gel intrarectally by a gavage syringe, after 5 min, 5 ml 2% lignocaine hydrochloride was injected into the neurovascular bundle at the basolateral aspect of the prostate gland under TRUS guidance, using a 23G, 200 mm needle. The injection site in the neurovascular bundle was identified between the seminal vesicle and the base of prostatic.[2] The prostatic volume was measured and then biopsies were taken of the prostate gland.
Group II (spinal anesthesia) received 1.5 ml bupivacaine 0.5% through a 25G spinal needle at L3–L 4 in the lateral decubitus position.
Group III (IV sedation) received 25 μg/kg midazolam, 2 μg/kg fentanyl, and 1 mg/kg ketamine through an antecubital vein, 5 min before taking the biopsies.
For patients in Group I (PPNB plus IRLA) and Group III (IV sedation), to ensure the blindness of the patient to the anesthesia method preferred, the urologist touched and pressed the patient's back with the back of an needle with the patient in sitting position and told the patient that anesthesia was applied.
Assessment of pain and complications
Pain presence and intensity w measured using a visual analog scale (VAS) ranges from 0 (no pain) to 10 (unbearable pain).[18]
After the procedure, another physician (who was not aware of the type of anesthesia used), presented the pain scale to the patients and asked about the intensity of pain after taking biopsy.
Patients were observed for immediate complications such as urinary retraction, fever or sepsis at least 2 h after biopsy and were discharged home if they voided successfully or had no immediate complications.
After 2 weeks, patients were reevaluated for late complications such as urinary retraction, fever or any events leading to rehospitalization through completing a questionnaire in their follow-up clinic appointment or by calling them.
For measuring PSA level, a blood sample was sent to a laboratory for analysis. In addition, prostate volume measurements by TRUS were performed.
Statistical analysis
Results were analyzed using SPSS Software version 20 (SPSS, Inc., Chicago, IL, USA). Continuous variables were presented as mean and standard deviation. Qualitative variables were presented as (n [%]). The differences between the treatment groups in age, PSA level, prostate volume, and VAS pain score were compared using the one-way ANOVA test. A Chi-square test was used to test differences between groups for lower urinary tract symptoms (LUTS), nodularity, history of urinary retraction, and early/late complications. P < 0.05 was considered statistically significant.
RESULTS
In this trial, from 123 initially enrolled patients, 106 patients completed the trial. Thirty-seven patients were included in Group I (PPNB plus IRLA), 36 in Group II (spinal anesthesia), and 37 in Group III (IV sedation) [Figure 1].
Figure 1.
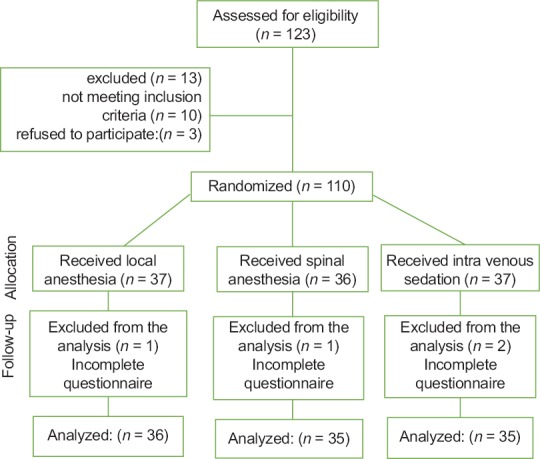
Study flow diagram
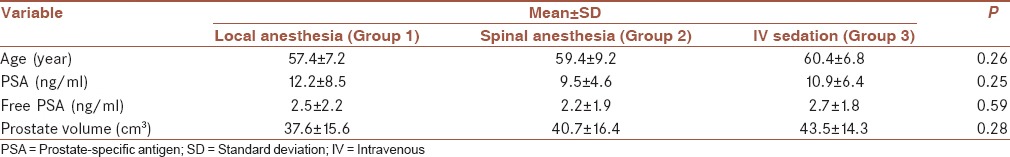
Mean age of patients was 60.3 ± 8 years, mean free PSA value was 2.4 ± 1 ng/ml mean of PSA value was 10.8 ± 6 ng/ml and prostate volume measured with TRUS was 40.5 ± 15 g, with no statistical difference in none of parameters between the three groups [Table 1].
Table 1.
Demographics of patients and prostate characteristics in laboratory data and ultrasonographic
All patients underwent a DRE immediately before the probe insertion and were examined for nodularity and prostate size. There was no statistical difference between groups in term of these variables [Table 2].
Table 2.
Patient's history and Prostate characteristics in digital rectal exam
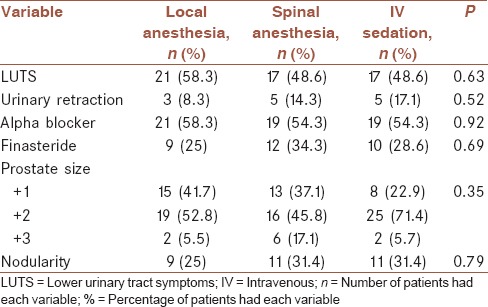
Table 2 shows the history of LUTS, urinary retraction, and drug usage in patients of three groups. No statistical significance was seen in these variables among three groups.
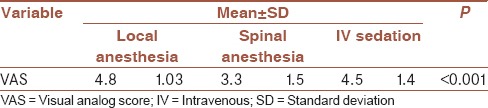
Table 3 shows VAS scores from each group after taking biopsies. Patients in Group 2 who had low-dose spinal anesthesia reported significantly less pain in comparison with the two other groups (P < 0.001). The differences in pain scores between PPNB plus IRLA group and IV sedation treated group were not statistically significant (P = 0.30), [Table 3].
Table 3.
Patient visual analog scale score
In evaluating early complications, there was a significant difference between groups in terms of urinary retraction and fever. Urinary retraction most occur in low-dose spinal anesthesia treated group (P = 0.04), and the most frequent occur of fever was in IV sedation received group (P = 0.03). There was no significance difference in terms of sepsis among groups (P = 0.77), [Table 4].
Table 4.
Patient early complications and late complications
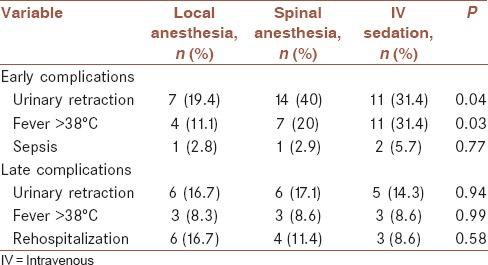
No significant difference in late complications including urinary retraction, fever >38 C and rehospitalization was found among the groups [Table 4].
There were no major postoperative complications, including transient neurologic symptoms and delirious sate, in none of groups. The cause for the rehaspitalizations was sepsis, which requires inpatient antibiotic treatment in all cases, and patients were treated and discharged within 72 h. No additional complications were recorded on follow-ups.
DISCUSSION
The recent trend in using an extend number of core biopsies to detection prostate cancer with a higher accuracy[19] is associated with more discomfort and pain patients experience.[20] So that, it become important for urologist to understand and overcome pain associated with this procedure.
Furthermore, adequate probe manipulation to obtain an effective biopsy procedure and increase rate of cancer detection lead to more patient discomfort.[5] Hence, better pain relieving resulted in increased cancer detection rate.
Today using options for analgesia during prostate biopsy includes: IRLA, PPNB, and oral or intrarectal drug analgesia and intravenous (IV) or inhalation anesthesia depending on clinician preference.
In this study, we compared the efficacy of PPNB plus local anesthesia, low-dose spinal anesthesia, and IV sedation for reducing pain during the procedure. Our results indicated that application of low-dose spinal anesthesia is superior to PPNB plus IRLA, and IV sedation in terms of pain controlling and was associated with higher tolerance of the examination and patient comfort.
This is the first prospective clinical trial to compare the efficacy of these three methods in pain controlling.
PPNB plus IRLA is one of the most applicable and popular anesthesia methods in clinical practice for prostate biopsy. However, PPNB does not provide adequate analgesic effect (reduction in pain level) for patients.[12] Thus, urologists still investigate different methods to find out the most effectiveness anesthesia method.
Numerous studies regarding anesthesia techniques compared the efficacy of PPNB with other anesthesia methods showed a higher tolerance and lower VAS score for PPNB groups.[9,10,11,21,22]
On the other hand, several other studies indicated that PPNB with or without IRLA have not a complete analgesic effect during prostate biopsy.[12,13]
Spinal anesthesia has been known to be an ideal anesthesia for perianal surgery. However, the amount of bupivacaine which is used for routine anorectal surgeries, causing motor block of the lower extremities and hemostatic instability.[23] In regard to these side effects, spinal anesthesia has not been used for procedure such as prostate biopsy which is considered as a minor surgery.
Obi et al. compared PPNB with spinal anesthesia using 2.5 mg bupivacaine They reported that spinal anesthesia provides better analgesia than PPNB.[14] Currently, Kucur et al.reduced the dose of bupivacaine to 1.5 mg for spinal anesthesia and compare it with PPNB technique. They achieved higher patient's satisfaction with no motor blockade and no more complication in spinal anesthesia than PPNB group.[24] In the current study, similarly, we also used low-dose spinal anesthesia (1.5 mg bupivacaine) and observed lower VAS score in compare with other anesthetic methods. There were no motor blockade or hemostatic instability and on more major complication than other methods.
Some other studies discuses general anesthesia and state different benefit for using this method.[25,26,27]
In a prospective study, Turgut et al. compare the efficacy of sedation using midazolam and PPNB using lidocaine. They reported a higher reduction in the level of discomfort in group received sedation and admired the great anal relaxation which is achieved in this method.[15]
One the other hand, Nishikawa et al.[16] and Sundarathiti et al.[17] compared spinal anesthesia with IV sedation with propofol, they find out both anesthesia methods provides acceptable pain relief, but spinal anesthesia was more preferable than propofol, with respect to costs and safety.
The strength of our clinical trial was its novelty. This was the first randomized clinical trial which compared these three applicable methods.
The limitations of current study were small sample size and lack of a placebo or control group which received no analgesic.
We recommend studies with larger sample size with control group to confirm our findings.
CONCLUSION
This study demonstrates that low-dose spinal anesthesia is superior to PPNB plus IRLA and IV sedation in terms of pain controlling and was associated with higher tolerance of the examination and patient comfort.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Heidenreich A, Bastian PJ, Bellmunt J, Bolla M, Joniau S, van der Kwast T, et al. EAU guidelines on prostate cancer. Part 1: Screening, diagnosis, and local treatment with curative intent-update 2013. Eur Urol. 2014;65:124–37. doi: 10.1016/j.eururo.2013.09.046. [DOI] [PubMed] [Google Scholar]
- 2.Machado MT, Aragão AJ, Rodrigues AO, Wroclawski ER. Periprostatic local anesthesia in transrectal ultrasound-guided prostate biopsy: Is it possible to improve pain tolerance? Int Braz J Urol. 2002;28:323–9. [PubMed] [Google Scholar]
- 3.Bjurlin MA, Carter HB, Schellhammer P, Cookson MS, Gomella LG, Troyer D, et al. Optimization of initial prostate biopsy in clinical practice: Sampling, labeling and specimen processing. J Urol. 2013;189:2039–46. doi: 10.1016/j.juro.2013.02.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Presti JC, Jr, Chang JJ, Bhargava V, Shinohara K. The optimal systematic prostate biopsy scheme should include 8 rather than 6 biopsies: Results of a prospective clinical trial. J Urol. 2000;163:163–6. [PubMed] [Google Scholar]
- 5.Temiz MZ, Kandirali E, Colakerol A, Tuken M, Semercioz A. Local anesthesia type affects cancer detection rate in transrectal ultrasound guided prostate biopsy. Int Braz J Urol. 2015;41:859–63. doi: 10.1590/S1677-5538.IBJU.2014.0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ravery V, Goldblatt L, Royer B, Blanc E, Toublanc M, Boccon-Gibod L, et al. Extensive biopsy protocol improves the detection rate of prostate cancer. J Urol. 2000;164:393–6. [PubMed] [Google Scholar]
- 7.Collins GN, Lloyd SN, Hehir M, McKelvie GB. Multiple transrectal ultrasound-guided prostatic biopsies – True morbidity and patient acceptance. Br J Urol. 1993;71:460–3. doi: 10.1111/j.1464-410x.1993.tb15993.x. [DOI] [PubMed] [Google Scholar]
- 8.Yan P, Wang XY, Huang W, Zhang Y. Local anesthesia for pain control during transrectal ultrasound-guided prostate biopsy: A systematic review and meta-analysis. J Pain Res. 2016;9:787–96. doi: 10.2147/JPR.S117451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nambirajan T, Woolsey S, Mahendra V, Walsh IK, Lynch TH, Keane PF, et al. Efficacy and safety peri-prostatic local anaesthetic injection in trans-rectal biopsy of the prostrate: A prospective randomised study. Surgeon. 2004;2:221–4. doi: 10.1016/s1479-666x(04)80004-0. [DOI] [PubMed] [Google Scholar]
- 10.Hiros M, Selimovic M, Spahovic H, Sadovic S, Spuzic-Celic E. Transrectal ultrasound-guided prostate biopsy, periprostatic local anesthesia and pain tolerance. Bosn J Basic Med Sci. 2010;10:68–72. doi: 10.17305/bjbms.2010.2740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ingber MS, Ibrahim I, Turzewski C, Hollander JB, Diokno AC. Does periprostatic block reduce pain during transrectal prostate biopsy. A randomized, placebo-controlled, double-blinded study? Int Urol Nephrol. 2010;42:23–7. doi: 10.1007/s11255-009-9621-2. [DOI] [PubMed] [Google Scholar]
- 12.Singh SK, Kumar A, Griwan MS, Sen J. Comparative evaluation of periprostatic nerve block with and without intraprostatic nerve block in transrectal ultrasound-guided prostatic needle biopsy. Korean J Urol. 2012;53:547–51. doi: 10.4111/kju.2012.53.8.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cantiello F, Cicione A, Autorino R, Cosentino C, Amato F, Damiano R, et al. Pelvic plexus block is more effective than periprostatic nerve block for pain control during office transrectal ultrasound guided prostate biopsy: A single center, prospective, randomized, double arm study. J Urol. 2012;188:417–21. doi: 10.1016/j.juro.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 14.Obi AO, Okafor VU, Nnodi PI. Prospective randomized trial of spinal saddle block versus periprostatic lignocaine for anesthesia during transrectal prostate biopsy. Urology. 2011;77:280–5. doi: 10.1016/j.urology.2010.07.468. [DOI] [PubMed] [Google Scholar]
- 15.Turgut AT, Ergun E, Koşar U, Koşar P, Ozcan A. Sedation as an alternative method to lessen patient discomfort due to transrectal ultrasonography-guided prostate biopsy. Eur J Radiol. 2006;57:148–53. doi: 10.1016/j.ejrad.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 16.Nishikawa K, Yoshida S, Shimodate Y, Igarashi M, Namiki A. A comparison of spinal anesthesia with small-dose lidocaine and general anesthesia with fentanyl and propofol for ambulatory prostate biopsy procedures in elderly patients. J Clin Anesth. 2007;19:25–9. doi: 10.1016/j.jclinane.2006.05.017. [DOI] [PubMed] [Google Scholar]
- 17.Sundarathiti P, Sirinan C, Seangrung R, Watcharotayangul J, Sithamwilai W. Selective spinal anesthesia versus intravenous propofol in transrectal ultrasound-guided prostate biopsy. J Med Assoc Thai. 2009;92:920–4. [PubMed] [Google Scholar]
- 18.Campbell W, Lewis S. Visual analogue measurement of pain. Ulster Med J. 1990;59:149. [PMC free article] [PubMed] [Google Scholar]
- 19.Elabbady AA, Khedr MM. Extended 12-core prostate biopsy increases both the detection of prostate cancer and the accuracy of gleason score. Eur Urol. 2006;49:49–53. doi: 10.1016/j.eururo.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 20.Scattoni V, Zlotta A, Montironi R, Schulman C, Rigatti P, Montorsi F, et al. Extended and saturation prostatic biopsy in the diagnosis and characterisation of prostate cancer: A critical analysis of the literature. Eur Urol. 2007;52:1309–22. doi: 10.1016/j.eururo.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Izol V, Soyupak B, Seydaoglu G, Aridogan IA, Tansug Z. Three different techniques for administering analgesia during transrectal ultrasound-guided prostate biopsy: A comparative study. Int Braz J Urol. 2012;38:122–8. doi: 10.1590/s1677-55382012000100017. [DOI] [PubMed] [Google Scholar]
- 22.Yurdakul T, Taspinar B, Kilic O, Kilinc M, Serarslan A. Topical and long-acting local anesthetic for prostate biopsy: A prospective randomized placebo-controlled study. Urol Int. 2009;83:151–4. doi: 10.1159/000230015. [DOI] [PubMed] [Google Scholar]
- 23.Parnass SM, Schmidt KJ. Adverse effects of spinal and epidural anaesthesia. Drug Saf. 1990;5:179–94. doi: 10.2165/00002018-199005030-00003. [DOI] [PubMed] [Google Scholar]
- 24.Kucur M, Goktas S, Kaynar M, Apiliogullari S, Kilic O, Akand M, et al. Selective low-dose spinal anesthesia for transrectal prostate biopsy: A Prospective and randomized study. J Endourol. 2015;29:1412–7. doi: 10.1089/end.2015.0450. [DOI] [PubMed] [Google Scholar]
- 25.Sur RL, Borboroglu PG, Roberts JL, Amling CL. A prospective randomized comparison of extensive prostate biopsy to standard biopsy with assessment of diagnostic yield, biopsy pain and morbidity. Prostate Cancer Prostatic Dis. 2004;7:126–31. doi: 10.1038/sj.pcan.4500713. [DOI] [PubMed] [Google Scholar]
- 26.Kang SG, Tae BS, Min SH, Ko YH, Kang SH, Lee JG, et al. Efficacy and cost analysis of transrectal ultrasound-guided prostate biopsy under monitored anesthesia. Asian J Androl. 2011;13:724–7. doi: 10.1038/aja.2011.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsuji FH, Chambó RC, Agostinho AD, Trindade Filho JC, de Jesus CM. Sedoanalgesia with midazolam and fentanyl citrate controls probe pain during prostate biopsy by transrectal ultrasound. Korean J Urol. 2014;55:106–11. doi: 10.4111/kju.2014.55.2.106. [DOI] [PMC free article] [PubMed] [Google Scholar]


