Abstract
Background:
The metabolic syndrome (MetS) is a complex disorder and a major health concern in developing countries. Data on MetS in Indian population show multiplicity. There are no published reports about the prevalence of MetS in population of Saurashtra region, Gujarat. The aim of this study is to assess the prevalence of MetS and its components in adult population of this region.
Methods:
This cross-sectional observational study was carried out among 473 participants who attended free health checkup camps. Demographics, personal details along with anthropometric, clinical, and biochemical data were recorded. The MetS was diagnosed as per the definition provided by Joint Interim Statement 2009.
Results:
The overall prevalence of MetS among studied population was found to be 41.01% (females 44.21% and males 37.91%). Abdominal obesity (66.38%), low high-density lipoprotein-cholesterol (64.69%), and high blood pressure (40.59%) appeared as the most prevalent components. MetS showed a significant association with age, body mass index, total cholesterol, habit of chewing tobacco, and history of hypertension and hyperglycemia.
Conclusion:
The high prevalence of MetS shows that population of Saurashtra is at an increased risk of cardiovascular disease (CVD) and diabetes. This highlights the need for extensive diabetes and CVD prevention and control program in this region.
Keywords: Abdominal obesity, dyslipidemia, metabolic syndrome, Saurashtra
INTRODUCTION
The metabolic syndrome (MetS) is a global health issue, characterized by clustering of various interlinked risk factors such as abdominal obesity, hypertension, hyperglycemia, dyslipidemia, pro-inflammatory state, and a prothrombotic state.[1] Degree and prevalence of MetS vary with ethnicity, genetic susceptibility, and geographic location.[2] Data on MetS in Indian population also show multiplicity may be either due to difference in the defining criteria of MetS or the ethnic and cultural complexity of different regions.[3] Marked shift in lifestyle, affluence in urbanization, and oil- and sugar-rich dietary habits have pushed ethnic Gujarati people to the forefront as contributors to cardiovascular disease (CVD) risk factors.[4] There are no published reports available about prevalence of MetS in population of Saurashtra region, Gujarat. Hence, the study was planned to evaluate the prevalence of MetS and its components in adult population of Saurashtra and to find its association with various anthropometric and biochemical indicators.
METHODS
Study design
A cross-sectional observational study was conducted in the field practice area of a Medical College of Surendranagar district of Saurashtra, Gujarat, after approval from the Institutional Ethics Committee on Human Research. A total 534 participants were screened through the free health checkup camps arranged at four different places of field practice area. All individuals ranging in age from 20 to 80 years were included in the study. Participants with self-reported pregnancy state, individuals using steroids, antibiotics, or needing hospitalization and those who refused to give written consent were excluded from the study. The details of demographics, personal, and family history of diseases, personal habit/s, and medication use were collected from each individual. Four hundred and seventy-three participants were included in the study after obtaining signed informed consent.
Measurements
The body mass index (BMI), hip circumference (HC), waist circumference (WC), and blood pressure were measured using standard methods.[5,6,7]
Fasting venous blood samples were collected for the estimation of various biochemical parameters, namely, fasting blood glucose, total cholesterol, triglyceride, low-density lipoprotein-cholesterol, and high-density lipoprotein-cholesterol (HDL-C) using approved standard laboratory methods.
Definition of metabolic syndrome
MetS was defined as the presence of ≥3 of the following five risk factors:[8]
Abdominal obesity: WC ≥90 cm in men and ≥80 cm in women
Hypertriglyceridemia: Triglycerides ≥150 mg/dL or on treatment (Rx) to lower triglycerides
Low HDL-C: <40 mg/dL in men and <50 mg/dL in women or on Rx to increase HDL-C
High blood pressure: Systolic blood pressure (SBP) ≥130 mmHg and/or diastolic blood pressure (DBP) ≥85 mmHg or on antihypertensives
High fasting blood sugar (FBS): ≥100 mg/dL or on Rx for hyperglycemia.
Data analysis
All statistical analysis was performed with Sigma plot 12.0 for Windows (Systat Software, Inc., SigmaPlot). The unpaired t-test and analysis of variance with post hoc Tukey test were used for comparisons of means of normally distributed variables whereas nonparametric variables were analyzed using Mann–Whitney and Kruskal–Wallis with post hoc Dunn's test. Pearson's Chi-square test was used to compare proportions. The odds ratios (ORs) and their 95% confidence intervals were done using 2 × 2 contingency tables. The significance level 5% was adopted for all hypothesis tests.
RESULTS
A total of 473 participants were studied. Almost 93% of the participants had at least one abnormal parameter, as per the MetS criteria used.
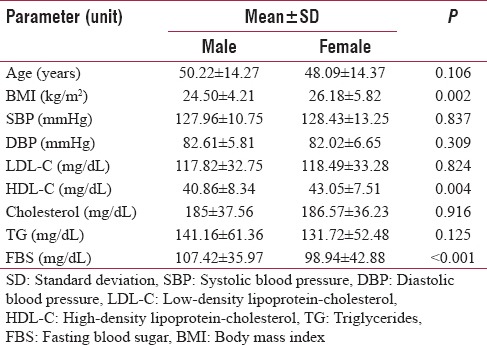
Out of total participants, 26.9% were <40 years of age, 44.6% aged between 40 and 59 years of age, and 28.5% were >60 years of age. Among the total participants as per BMI, World Health Organization classification,[9] 56% females and 45% males were found ≥25 kg/m2. Prevalence of ≥25 kg/m2 was found high in 40–59-year age group. Almost 40% of the participants declared about their habit of smoking, alcohol consumption, and chewing tobacco. Habit of smoking and chewing tobacco was found more prevalent in the age group of 40 years and above, whereas alcohol consumption was more prevalent in <40 years of age. Increasing incidence of taking antihypertensive and hypoglycemic drugs was observed in both sexes with advancing age. Gender-specific comparison of anthropometric and biochemical parameters showed higher values of FBS, WC, and waist-to-hip ratio in males and higher values of BMI, HC, and HDL-C in females [Table 1].
Table 1.
Gender specific comparison of anthropometric and biochemical variable
The overall prevalence of MetS was 41.01% with 44.21% in females and 37.91% in males. The prevalence of MetS was more in females, but the observed difference was not significant between genders. Abdominal obesity (66.38%), low HDL-C (64.69%), and high blood pressure (40.59%) were the most prevalent components, and the constellation of these variables has been found in almost 53% of the participants identified with MetS. Overall prevalence of MetS and components such as high blood pressure and high FBS showed a significant positive relation with advancing age [Figure 1].
Figure 1.
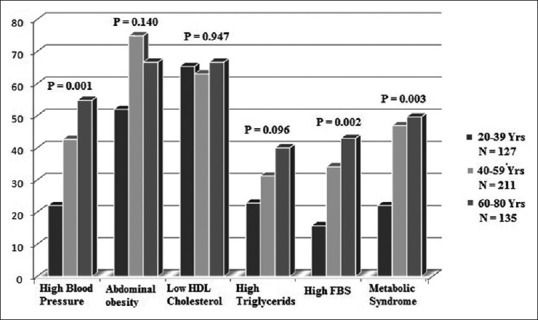
Age-specific prevalence of metabolic syndrome components. High FBS: High fasting blood sugar
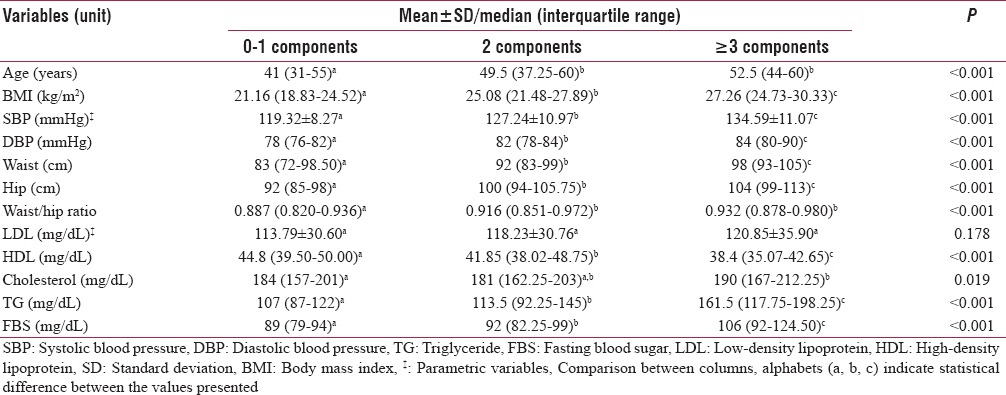
In groups based on the number of positive MetS components, analysis of comparing variance among the groups showed a progressive variation in the values of anthropometric and biochemical variables with increasing number of the MetS components. Participants presenting with two or more components showed higher values of age and waist-to-hip ratio compared to those who presented one or no component. Participants with MetS showed a higher level of cholesterol compared to participants with no MetS [Table 2].
Table 2.
Comparison of variables as per number of positive components leading to metabolic syndrome
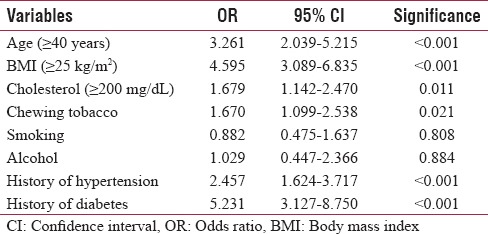
In this study population, individuals aged 40 years or more were 3.26 times more likely to have MetS as compared to individuals with lesser age. Individuals with ≥25 kg/m2 of BMI and ≥200 mg/dl of cholesterol had 4.6 and 1.68 times more risk to have MetS than the individuals with lesser BMI and cholesterol, respectively. The risk of MetS was increased by 1.67 times in individuals having habit of chewing tobacco. Individuals on oral hypoglycemic and/or insulin had 5.32 times and individuals on antihypertensive drugs had 2.46 times more risk to have MetS [Table 3].
Table 3.
Odds ratio for different variables and metabolic syndrome
DISCUSSION
South Asia is home to one of the largest population of people with MetS. The prevalence of MetS in South Asians varies according to region, extent of urbanization, lifestyle patterns, and cultural/socioeconomic factors.[10] This study showed an overall MetS prevalence of 41.01% with abdominal obesity, low HDL-C, and high blood pressure as the most prevalent components. MetS was found higher in females and showed significant rise with age. Similar MetS prevalence (41.1%) findings were reported by the study conducted in urban Asian Indian adults in 2003.[11] Little higher prevalence of MetS was reported by the studies conducted in population of Eastern India (43.2%)[12] and in a higher socioeconomic population of Ahmedabad, Gujarat (42.6%).[13] On the contrary, lower prevalence of MetS was observed by the studies conducted in Chennai, India (25.8%),[14] Sri Lanka (27.1%),[15] and Nepal (22.5%).[16] Such variation in MetS prevalence might be either due to difference in nutritional habits or regional cultural/socioeconomic difference in studied population. However, all these studies have identified the incidence of female preponderance and increased prevalence of MetS with advancing age. These studies also identified dyslipidemia, abdominal obesity, and high blood pressure, as most prevalent MetS components. The common observations of these Asian studies including current study are in agreement with Asians predisposition for MetS and subsequent risk for the development of CVD and type 2 diabetic mellitus (T2DM). This might be due to fact that among Asian Indians, the promoter polymorphisms − 482T and 455C of APOC3 gene are shown to be associated with the MetS.[17] However, further explanations are needed to develop cause-effect relationship through cohort and genetic studies.
In the present study, values of BMI, SBP, DBP, WC, HC, triglycerides, and FBS were increased, and HDL-C value was decreased with increased number of MetS components. Simultaneous rise in the value of variables with increasing number of MetS components present might be due to these variables influencing each other. Participants presented with two or more components showed higher values of age and waist-to-hip ratio compared to those who have one or no component. These observations might be an indication of the unsatisfactory health profile even in those who were not identified as MetS [Table 2]. Apart from that, the presence of two MetS components could be an evidence of impending elevated values of anthropometric indicators of obesity and atherogenic dyslipidemia leading to full-fledged MetS with advancing age. Hence, appropriate preventive measures should be taken to restrict further progression of syndrome and T2DM/CVD risk with advancing age.
For each component of the MetS and associated factors, there is a complex interaction between aging and obesity.[18] The risk of metabolic and CVDs increases with age. This study confirms the advancement of age and BMI as strong risk factors associated with MetS; with an OR of 3.26 and 4.6 for age and BMI, respectively. This association goes hand in hand with increasing prevalence of CVD and T2DM among the older population, which is evident through the increasing prevalence of potent risk factors such as hypertension, hyperglycemia, and hypertriglyceridemia with age [Figure 1]. In addition to these variables, the MetS is also found to be associated with hypercholesterolemia and history of hypertension and hyperglycemia, in the current study. These observations might be an expression of the emergent pathophysiology of MetS. Diabetes and hypertension share common pathways to interact and influence each other and may aggravate the process of development of MetS and subsequent morbidity.[2] A study reported by E S Ford in 2005 showed 12%–17% and 30%–52% relative risk of CVD and diabetes among the MetS patients, respectively.[19] This and our findings reiterate the importance and relevance of early identification of the MetS in impaired fasting glucose and hypertensive patients which could assist the physicians to assess the risk of development of CVD and diabetes.
Tobacco chewers had a significantly greater prevalence of resting tachycardia, hypertension, dyslipidemia, and diabetes compared to nontobacco users. Smokeless tobacco use is associated with increased cardiovascular risk factors such as MetS and diabetes.[20] the current study had shown the significant higher prevalence of MetS among the tobacco chewers compared to nontobacco chewers. Hence, tobacco chewing comes out as a significant risk factor in the development of MetS which is in agreement with published work of others.[21] In some studies, cigarette smoking was found to be associated with risk of MetS in heavy smokers and showed a positive dose-dependent association between smoking and high triglyceride levels.[22] Mild-to-moderate alcohol consumption has a favorable influence on serum lipids, WC, and fasting serum insulin.[23] While our findings about smoking and alcohol were not found significant in association with MetS, these results corroborated with the study conducted in Sri Lankan adults.[15]
CONCLUSION
This was the first study conducted in one of the underdeveloped regions of Gujarat, which is passing through vigorous industrialization and urbanization phase. Change in lifestyle and food habits due to this analogous to the increased worsening of the glucose and lipid metabolism associated with age. Hence, individuals identified with MetS at earlier of age would benefit most from lifestyle adjustment. The high prevalence of MetS and increasing trend of CVD risk factors such as BMI, blood pressure, lipid profile, and FBS values shows that the population of Saurashtra is at increased risk for CVD and diabetes. This highlights the need for extensive diabetes and CVD prevention and control program in the region.
Limitations
The main limitation of the present study is the innate characteristics of a cross-sectional study; specifically, as the associations between MetS and variables cannot be interpreted as causal associations. The adopted sampling technique may have influenced the prevalence of MetS. Hence, the prevalence obtained cannot be extrapolated to the general population. Data procured on personal habits of smoking, chewing tobacco, and alcohol consumption are self-reported and maybe encounter a subjective bias.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are grateful to Dr. NPGopinath, Professor emeritus, Department of Physiology and Additional Dean, C U Shah Medical College, Surendranagar, for his valuable suggestions and support. We are also thankful to resident doctors and technical staff members for their support.
REFERENCES
- 1.Grundy SM, Brewer HB, Jr, Cleeman JI, Smith SC, Jr, Lenfant C. American Heart Association, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 2.Kaur J. A comprehensive review on metabolic syndrome. Cardiol Res Pract. 2014;2014:943162. doi: 10.1155/2014/943162. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 3.Kotokey R, Kalita D, Agarwala R, Purkayastha S. Prevalence of metabolic syndrome in urban population of Dibrugarh town of upper Assam. J Indian Coll Cardiol. 2013;3:52–6. [Google Scholar]
- 4.Pandya H, Lakhani JD, Dadhania J, Trivedi A. The prevalence and pattern of dyslipidemia among type 2 diabetic patients at rural based hospital in Gujarat, India. Indian J Clin Pract. 2012;22:36–44. [Google Scholar]
- 5.Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. Int J Epidemiol. 2014;43:655–65. doi: 10.1093/ije/dyu058. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert Consultation. Geneva, 8-11 December 2008. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 7.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 8.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, et al. Harmonizing the metabolic syndrome: A Joint Interim Statement of the International Diabetes Federation Task force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 9.Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i. [PubMed] [Google Scholar]
- 10.Pandit K, Goswami S, Ghosh S, Mukhopadhyay P, Chowdhury S. Metabolic syndrome in South Asians. Indian J Endocrinol Metab. 2012;16:44–55. doi: 10.4103/2230-8210.91187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults – A population study using modified ATP III criteria. Diabetes Res Clin Pract. 2003;60:199–204. doi: 10.1016/s0168-8227(03)00060-3. [DOI] [PubMed] [Google Scholar]
- 12.Prasad DS, Kabir Z, Dash AK, Das BC. Prevalence and risk factors for metabolic syndrome in Asian Indians: A community study from urban Eastern India. J Cardiovasc Dis Res. 2012;3:204–11. doi: 10.4103/0975-3583.98895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel N, Patel H, Gunjalia A. Prevalence of metabolic syndrome in higher socioeconomic class of Ahmedabad, Gujarat, India. Int J Med Sci Public Health. 2016;5:35–9. [Google Scholar]
- 14.Deepa M, Farooq S, Datta M, Deepa R, Mohan V. Prevalence of metabolic syndrome using WHO, ATPIII and IDF definitions in Asian Indians: The Chennai urban rural epidemiology study (CURES-34) Diabetes Metab Res Rev. 2007;23:127–34. doi: 10.1002/dmrr.658. [DOI] [PubMed] [Google Scholar]
- 15.Katulanda P, Ranasinghe P, Jayawardana R, Sheriff R, Matthews DR. Metabolic syndrome among Sri Lankan adults: Prevalence, patterns and correlates. Diabetol Metab Syndr. 2012;4:24. doi: 10.1186/1758-5996-4-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sharma SK, Ghimire A, Radhakrishnan J, Thapa L, Shrestha NR, Paudel N, et al. Prevalence of hypertension, obesity, diabetes, and metabolic syndrome in nepal. Int J Hypertens. 2011;2011:821971. doi: 10.4061/2011/821971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Misra A, Misra R, Wijesuriya M, Banerjee D. The metabolic syndrome in South Asians: Continuing escalation and possible solutions. Indian J Med Res. 2007;125:345–54. [PubMed] [Google Scholar]
- 18.Alexander CM, Landsman PB, Grundy SM. The influence of age and body mass index on the metabolic syndrome and its components. Diabetes Obes Metab. 2008;10:246–50. doi: 10.1111/j.1463-1326.2006.00695.x. [DOI] [PubMed] [Google Scholar]
- 19.Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: A summary of the evidence. Diabetes Care. 2005;28:1769–78. doi: 10.2337/diacare.28.7.1769. [DOI] [PubMed] [Google Scholar]
- 20.Gupta R, Gupta N, Khedar RS. Smokeless tobacco and cardiovascular disease in low and middle income countries. Indian Heart J. 2013;65:369–77. doi: 10.1016/j.ihj.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shafique K, Zafar M, Ahmed Z, Khan NA, Mughal MA, Imtiaz F, et al. Areca nut chewing and metabolic syndrome: Evidence of a harmful relationship. Nutr J. 2013;12:67. doi: 10.1186/1475-2891-12-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Calo WA, Ortiz AP, Suárez E, Guzmán M, Pérez CM. Association of cigarette smoking and metabolic syndrome in a Puerto Rican adult population. Int J Prev Med. 2014;5:849–56. [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 23.Freiberg MS, Cabral HJ, Heeren TC, Vasan RS, Curtis Ellison R. Third National Health and Nutrition Examination Survey, et al. Alcohol consumption and the prevalence of the metabolic syndrome in the US: A cross-sectional analysis of data from the Third National Health and Nutrition Examination Survey. Diabetes Care. 2004;27:2954–9. doi: 10.2337/diacare.27.12.2954. [DOI] [PubMed] [Google Scholar]


