Abstract
Objectives:
The objectives were to evaluate the degree of dye penetration of three different dental materials as esthetic veneer restorations on anterior teeth using stereomicroscope, and to provide reference for clinical choice.
Materials and Methods:
Sixty freshly extracted human maxillary central incisors were selected and randomly divided into three main groups of 20 each. Respectively, the teeth were prepared for veneer restoration by fiber-reinforced composite (FRC) (Everstick NET, Stick Tech), porcelain laminate veneer (PLV) (IPS Empress II(E-Max Press)) and 3M composites (3M ESPE) bonding with G-Cem resin cement (GC). After exposed to thermocycling (500cycles per day (5–55 °C, intervals: 30 s)) and immersed in 2% basic fuchsin dye solution for 24 h, the specimens were then sectioned buccolingual into three halves in a vertical plane parallel and measured dye penetration using stereomicroscope (Zeiss). The data collected was recorded by the dye penetration index (0–5) and statistically analysed using one-way analysis of variance (ANOVA) and T-tests using SPSS 13.
Results:
It is evident that the FRC group showed the lowest mean score of 0.333 mm, and the PLV group showed a highest mean score of 0.749 mm, as compared with the FRC group and the 3M composites group. Overall, when the three groups were compared for microleakage using ANOVA, there was significant difference among the groups.
Conclusions:
To evaluate the dye penetration of microleakage, the FRC showed a better marginal adaptability for veneer restoration. Therefore, within the limitation of this study, the use of FRC as veneer on anterior teeth can be suggested.
Introduction
Esthetic appearance has become crucial in modern dentistry. Discoloured anterior teeth are often considered as an esthetic detraction in this modern world. As a result, veneer restoration for anterior teeth has gained so much attention, due to the growing demand for beautiful smiles and white teeth with less invasive tooth preparation. Porcelain laminate veneer (PLV) has been used by dentists for several years. It has many advantages as a restorative method, because it is aesthetically pleasing, durable and easy to use.1,2 However, it also has a number of drawbacks, such as tooth sensitivity, secondary caries and restoration fracture. A 10-year prospective clinical observation study reported a survival rate of 92% at 5 years, which dropped to 64% at 10 years. The main reasons for failure were large marginal defects and fractures.3–6 Similarly, composite veneer also has its own limitations, such as marginal staining, wear, discolouration and lower fracture resistance.7
Owing to the increasing importance of esthetic appearance, studies in restorative dentistry are directed towards meeting the expectations of patients and dentists. To overcome drawbacks of above materials, a high strength restorative material called fiber-reinforced composite (FRC) (Everstick NET, Stick Tech) which has been reinforced with IPN (Interpenetrating Polymer Network) composition has been recently introduced in dentistry.8 The previous studies evaluated the application of the FRC in the fields of post core, periodontal splint, orthodontic retainer, full crown, adhesive fixed bridge, fixed bridge, inlay fixed partial dentures, dental implant restoration and the base in removable partial denture.9 Even then, there still lacks a clinical application in veneer restoration.
Generally speaking, the success of any material is assessed by its longevity, sealing ability and biocompatibility in an oral environment. Microleakage is considered to be a major factor influencing the longevity of dental restorations.10 The purpose of this in vitro study is to investigate the degree of dye penetration as an estimation of microleakage of esthetic veneer restorations on the tetracycline pigmentation anterior teeth with FRC, PLV and 3M composites being introduced in clinical practice using stereomicroscope. The null hypothesis was that there were no differences among the veneer restorations with three different materials in the depth of microleakage.
Materials and methods
Teeth preparation
An in vitro experimental study was designed to assess the marginal microleakage of three different dental materials in veneer restoration. This study was performed in the Shanghai Stomatological Hospital, Shanghai, China. The research protocol was approved by the local ethics committee.
Sixty human maxillary central incisors that were recently extracted within the last 3 months due to periodontal problems were selected for the study. All the teeth had no craze lines, decay, abrasion, previous restorations, structural deformities, or cervical lesions. Removal of calculus and debris was carried out by hand through scaling and then stored in normal saline, which was known to have no effect on dentinal permeability and the bond strength of cement for this study.11 The teeth were randomly divided into three main groups of 20 each, according to different restoration materials as follows (Figures 1 and 2):
Figure 1.

Division and restoration of samples.
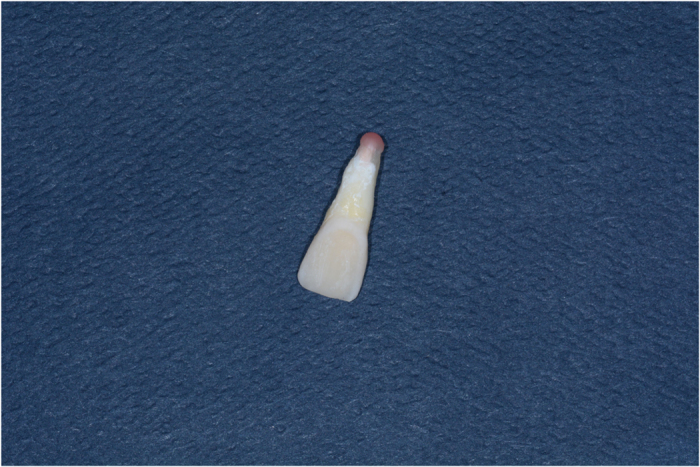
Figure 2.

The initial state of the tooth before restoration.
Group 1: Microleakage seen under veneer restorations with porcelain laminate veneer (PLV) (IPS Empress II (E-Max Press)).
Group 2: Microleakage seen under veneer restorations with FRC (EverstickNET, Stick Tech, Turku, Finland).
Group 3: Microleakage seen under veneer restorations with 3M composites (3 M ESPE).
Restorative procedure
All teeth were prepared for a veneer in the same manner by one investigator. The occlusal and buccal surfaces were reduced to 0.5 mm, respectively, with a 135° sloping shoulder finish line in the enamel. The required time for each tooth preparation was 10 min, and burs were replaced after every third tooth preparation.12
The impressions were obtained from each tooth using an additional polyvinyl sil oxane impression material (ESPE) and a custom-made tray (Major Tray, lot 06016A, Major Prodotti Dentori, S.p.A., Moncalieri, Italy) poured with type IV dental stone (Fujirock, GC). The veneer restorations were fabricated with three materials according to the grouping above.
The G-Cem resin cement (GC) was applied to the intaglio surface of the veneers, and the veneers were positioned on the teeth and held in place with finger pressure. The excess cement was removed, and the laminates were exposed to light on all margins for 60 s (Coltolux 50, Coltene/Whaledent), whereas all of the margins were covered with an isolation gel (Oxyguard, Kuraray) to prevent the formation of an oxygen-inhibited layer according to the manufacturers’ instructions. All preparations were performed by the same operator at room temperature and subsequently stored in an artificial oral environment (36 °C and 100% humidity) for 1 week (Figure 3).13
Figure 3.

The state of the tooth after veneer restoration.
Evaluation of microleakage
The specimens were then subjected to thermocycling for 500 cycles between 5±2 °C and 55±2 °C with a dwell time of 30 s in each bath and 20 s interval between baths at ambient air. Before the evaluation of the microleakage, the root apices and furcation areas were completely sealed with utility wax (Figure 4). To prevent dye penetration through the apex or dentinal tubules, all teeth received two coats of nail polish on the entire tooth surface except for the restoration and a 1 mm rim of tooth structure around the restoration margins.14 After sealing, the specimens were subsequently immersed in 2% basic fuchsin dye solution for 24 h, then removed from the dye, cleaned under tap water, and then left to dry for another 24 h according to manufacturer's instructions (Figure 5).
Figure 4.
Apical sealing with the wax.
Figure 5.
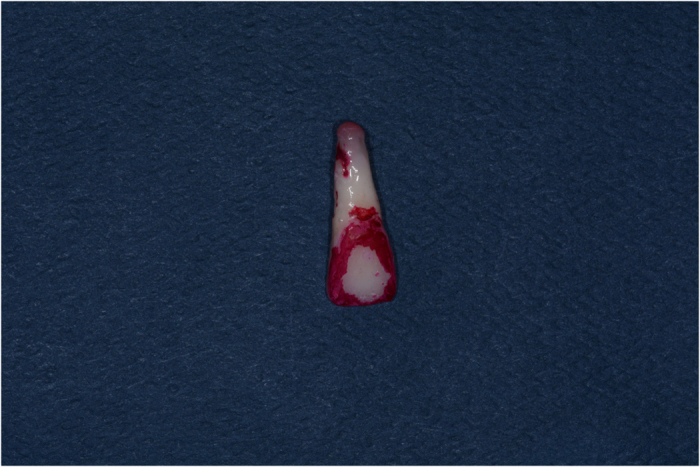
The state of the tooth after dyeing.
Later on, the specimens were fixed in translucent orthodontic resins and sectioned buccolingual into three halves in a vertical plane parallel to long axis of the tooth using diamond disc at slow speed with a water-cooled diamond saw (Leitz 1600) in the buccal area.15 All the samples were prepared by a single trained clinician and were assessed in a blind manner by two independent evaluators under a stereomicroscope (Zeiss) at ×40 magnification based on five-point scale to evaluate dye penetration(Figures 6,7,8).16 The microleakage scoring was done using the method, as per Radhika et al.17
0=No dye penetration;
1=Dye penetration limited to outer half of the axial wall;
2=Dye penetration limited to inner half of the axial wall;
3=Dye penetration reach the pulpal wall;
4=Dye penetration beyond the pulpal wall.
Figure 6.
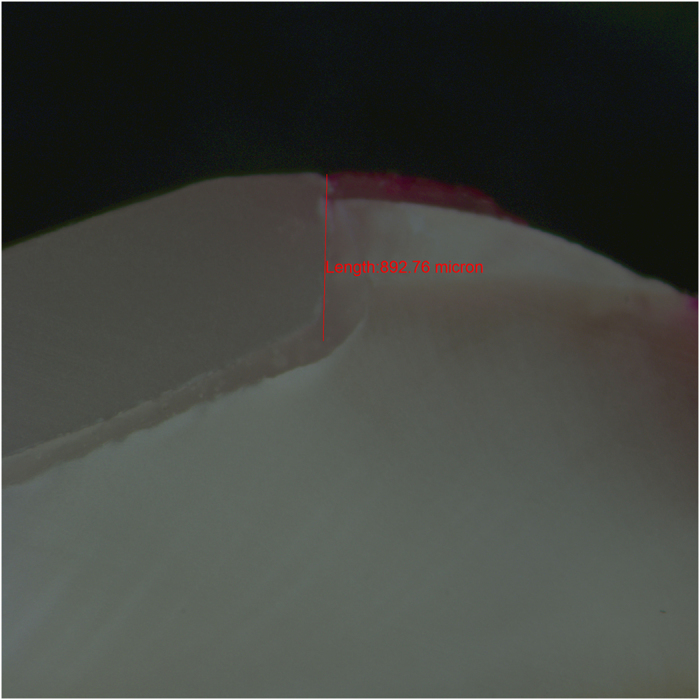
Longisection view of a tooth with porcelain laminate veneer restoration showing dye penetration.
Figure 7.
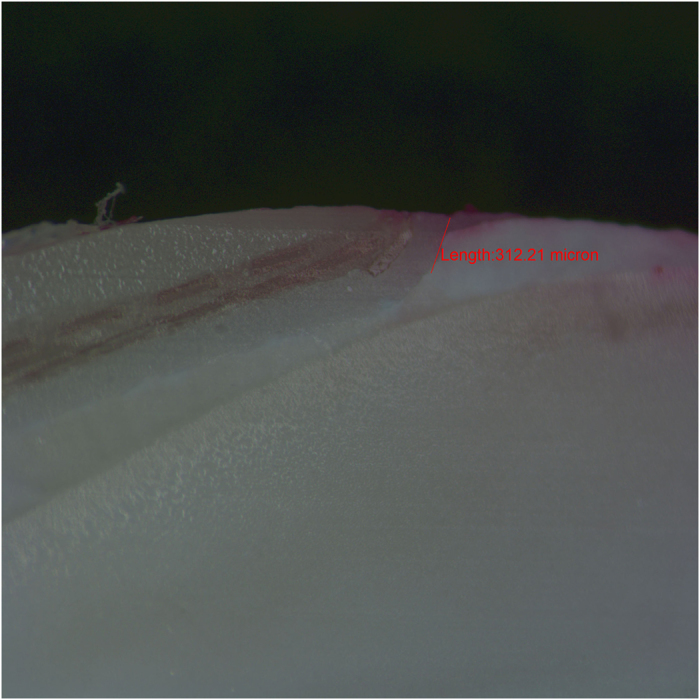
Longisection view of a tooth with everStick fibre reinforced composites resin veneer restoration showing dye penetration.
Figure 8.
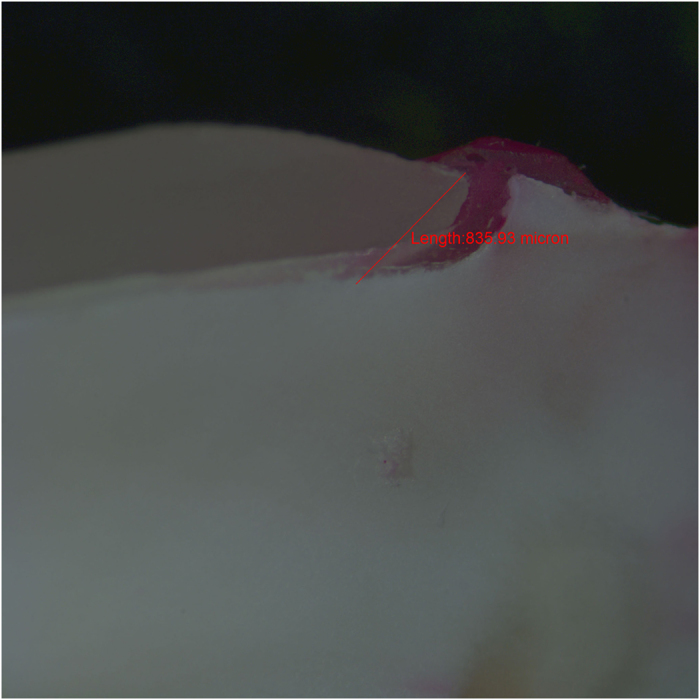
Longisection view of a tooth with 3M composites resin veneer restoration showing dye penetration.
Statistical analysis
Image analysis software was used to measure the linear dye penetration in microns. All data sets were subjected to normality testing using the Kolmogorov–Smirnov test. The mean microleakage values of the groups were statistically analysed by repeated-measures analysis of variance (ANOVA) using a statistics software (SPSS ver. 13, SPSS IBM SPSS; Chicago, IL, USA). T test was used to compare the different groups with each other and find out which group differs significantly. The differences with P<0.05 were considered statistically significant.
Results
Microleakage for each group was evaluated by stereomicroscope ×40 magnification and recorded using a parametric scale that gives a qualitative measurement of sealing effectiveness of restorative material (Table 1). As summarised in (Table 2/Figures 6,7,8), the microleakage data indicated that all the groups showed microleakage. The mean±s.d. leakage of samples from group 1 to group 3 was as follows gives a quantitative measurement (Table 2). The data collected was tabulated accordingly and was statistically analysed using one-way ANOVA (Table 2). It is evident that the PLV group showed a highest mean score of 0.749 mm, as compared with the FRC group and the 3M composites group, and the FRC group showed the lowest mean score of 0.333 mm. The P value was less than 0.05 indicating that the difference among the groups was statistically significant (Table 2).
Table 1. The qualitative measurement of sealing effectiveness of restorative materials.
| Groups |
Score |
||||
|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |
| Group 1(PLV) | 2 | 3 | 5 | 4 | 6 |
| Group 2(FRC) | 9 | 4 | 2 | 3 | 2 |
| Group 3 (3Mcomposites) | 4 | 5 | 3 | 2 | 6 |
Table 2. Mean and s.d. values and the statistical analysis of dye microleakage of the different materials in restoration margins (mm).
| Different materials | N | Mean±s.d. |
ANOVA |
|
|---|---|---|---|---|
| F | P-value | |||
| PLVa,b | 20 | 0.749±0.268 | 19.70 | 0.0023 |
| FRCa,c | 20 | 0.333±0.099 | 2.38 | 0.17 |
| 3M compositesb,c | 20 | 0.536±0.186 | 2.36 | 0.18 |
Abbreviation: ANOVA, analysis of variance.
Indicate significant difference between PLV and FRC (P<0.05).
Indicate significant difference between PLV and 3M composites (P<0.05).
Indicate significant difference between FRC and 3M composites (P<0.05).
Discussion
Studies have concentrated on improving tooth-coloured restorative materials and techniques to replace the lost dental tissue and improve the aesthetic state of the anterior teeth. Ceramic veneer has been used as cosmetic restoration of anterior teeth since the early 1960s. Although it had many advantages for its aesthetic, durable and easy to use, it also had a number of drawbacks such as brittleness and easily pulled off.18 Therefore, demand for esthetic materials has increased markedly in recent years. High strength, greater retention and colour suitability are among the most important properties of veneer materials. Recently, a new FRC called EverStick reinforced composites, which possess specific characteristics has been developed. It’s characteristics of simple, minimally invasive application that has a higher strength, with strong cohesive force and reversibility.19 Because of it’s minimally invasive nature, FRC can retain the healthy tissue of tooth. Also, provided is the possibility for other therapeutic method because of the reversibility.20,21 In addition, it shows less polymerisation shrinkage and can be bulk cured. Elasticity and low polymerisation shrinkage stress can reduce microleakage, postoperative sensitivity, and secondary caries.22
The marginal adaptability of restorations is necessary for successful restoration of teeth and is therefore regarded as an important determinant of their long-term success rate. The interface between restoration and dental substrate is an area of clinical concern that can result in secondary decay and marginal discolouration.23 Perfect adaptation is hard to accomplish because of inconsistent physical properties between tooth structure and restorative materials.24,25 Factors affecting the integrity of the interface are polymerisation shrinkage, hydroscopic expansion, light polymerisation concepts, thermal cycling, occlusal stresses, bonding agent and its placement.26,27 In our study, the teeth preparations were of the same dimensions, and the light-curing mode was the same for all the restoration specimens. Among these factors, polymerisation shrinkage would cause hidden leakage, also known as ‘microleakage’. Microleakage is the clinically undetectable passage of bacteria, fluids, molecules or ions and was commonly observed with various restorative materials. If not treated in time, it could cause pulpal pathology.28,29 Microleakage had been cited as the most important reason for restoration replacement, especially in anterior veneer restorations. So controlling and eliminating microleakage has always been an important goal of operative dentistry.30,31 Although most previous studies had demonstrated low levels of microleakage with different materials while also reporting that microleakage did not necessarily correlate with the materials, the long-term success rate of restorations was affected by several other factors such as the size of the marginal gap and the manipulation of manipulator—the results of the present study indicated a correlation between the materials used and microleakage.32 In order to eliminate the effect of marginal adaptability as a confounding factor and to evaluate the sealing ability of different materials in potential open areas of restoration margins, we investigated the sealing ability of the restorations with three different materials but the same preparation and resin adhesive.
Various methods to detect microleakage were suggested, including the dye leakage method, the use of colour producing microorganisms, radioactive isotopes, the air pressure method, neutron activation analysis, electrochemical studies, scanning electron microscopy, thermal and mechanical cycling, and chemical tracers. All of the three materials utilised in this study adopted the dye leakage method and exhibited some degree of microleakage. The FRC displayed very low microleakage and more satisfactory results for sealing of marginal adaptation, which was consistent with previous reports.33 In addition, polymerisation shrinkage of 3M composites may have caused higher stress at the tooth-restoration bond, although further studies were needed to compare the shrinkage of 3M composites with other resin composites. These results were in agreement with the present study.34 Moreover, the restoration margins in the present study were placed in enamel, which had been shown to display lower microleakage compared with enamel dentin. This result appeared to support the results obtained by Bayrak et al.35 However, problems associated with the microleakage remained a concern to clinicians and may compromise the longevity of restorations.
Results of this study showed that there was statistical significant difference among the three groups in microleakage. When group 2 was compared with group 1 and group 3, it was found that FRC group exhibited less microleakage than the PLV and 3M composites group. Another important factor—which can also affect the marginal microleakage—was the distance between the light-curing tip and the resin surface. When the distance between the light-curing tip and the restoration surface was >2 mm, the light intensity was significantly reduced. This might prevent adequate polymerisation of resin composite materials and was in accordance to previous studies.36 As dentists, we should incessantly search for techniques that eliminate, or at least reduce, microleakage to a minimum.
The main limitation of this study was that it was performed in laboratory conditions; however, the best way to test restorative materials would be in the oral cavity. More clinical experience was needed to confirm the results in real clinical situations. Furthermore, only three types of dental materials were evaluated. However, microleakage has not been assessed in non-adapted margins compared with adapted margins in previous studies.12 Within the limitations of this study, it was concluded that FRC exhibited better sealing ability in compared with PLV and 3M composites. Further studies of long-term strength and marginal sealing are required to confirm the results of the present study. Furthermore, clinical trials should be conducted on the long-term efficacy of different materials for anterior teeth veneer restorations.
Conclusions
Within the limitation of this study and regarding the results, it is concluded that all the restorative systems tested in this study exhibited microleakage. This was inevitable and irrespective to type of material being used, and the microleakage was lower in the FRC group compared with the group of PLV and 3M composites.
Acknowledgments
We thank the Shanghai Health Bureau for supporting this research (Grant# 20134162). We thank colleagues, dental laboratory and Shanghai Ninth People’s Hospital prosthodontics laboratory for the help in the study.
Ethics statement
The research has been conducted in full accordance with the World Medical Association Declaration of Helsinki and we had obtained consent from all participants involved in our study. Also, we had obtained the verbal consent which was approved by the committee of Shanghai association of medical ethics.
Footnotes
The authors declare no conflict of interest.
References
- Beier US, Kapferer I, Burtscher D, Dumfahrt H. Clinical performance of porcelain laminate veneers for up to 20 years. Int J Prosthodont 2012; 25: 79–85. [PubMed] [Google Scholar]
- Shadman N, Kandi SG, Ebrahimi SF, Shoul MA. The minimum thickness of a multilayer porcelain restoration required for masking severe tooth discoloration. Dent Res J (Isfahan) 2015; 12: 562–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke FJ. Survival rates for porcelain laminate veneers with special reference to the effect of preparation in dentin: a literature review. J Esthet Restor Dent 2012; 24: 257–265. [DOI] [PubMed] [Google Scholar]
- Gresnigt MM, Ozcan M, Kalk W, Galhano G. Effect of static and cyclic loading on ceramic laminate veneers adhered to teeth with and without aged composite restorations. J Adhes Dent 2011; 13: 569–577. [DOI] [PubMed] [Google Scholar]
- Gresnigt MM, Kalk W, Özcan M. Clinical longevity of ceramic laminate veneers bonded to teeth with and without existing composite restorations up to 40 months. Clin Oral Investig 2013; 17: 823–832. [DOI] [PubMed] [Google Scholar]
- Öztürk E, Bolay Ş, Hickel R, Ilie N. Shear bond strength of porcelain laminate veneers to enamel, dentine and enamel-dentine complex bonded with different adhesive luting systems. J Dent 2013; 41: 97–105. [DOI] [PubMed] [Google Scholar]
- Dalli M, Bahsi E, Sahbaz C, Ince B, Akkus Z, Ercan E. Atilgan a comparison of microleakage scores of five different types of composite resins. Biotechnol Biotechnol Equip 2010; 24: 2122–2126. [Google Scholar]
- Pekka K. Vallittu. Interpenetrating polymer networks (IPNs) in dental polymers and composites. J Adh SciTechnol 2009; 23: 961–972. [Google Scholar]
- Juloski J, Beloica M, Goracci C. Shear bond strength to enamel and flexural strength of different fiber-reinforced composites. J Adh Dent 2013; 15: 123–130. [DOI] [PubMed] [Google Scholar]
- Makarewicz D, Le Bell-Rönnlöf AM, Lassila LV. Effect of cementation technique of individually formed fiber-reinforced composite post on bond strength and microleakage. Open Dent J 2013; 26: 68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adanir N, Ureyen Kaya B, Kececi AD. Fracture resistance of roots restored with four different fiber-reinforced composite posts. Med Princ Pract 2015; 24: 538–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abd El Halim S, Zaki D. Comparative evaluation of microleakage among three different glass ionomer types. Oper Dent 2011; 36: 36–42. [DOI] [PubMed] [Google Scholar]
- Diwanji A, Dhar V, Arora R, Madhusudan A, Rathore AS. Comparative evaluation of microleakage of three restorative glass ionomer cements: An in vitro study. J Nat Sci Biol Med 2014; 5: 373–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi S, Disfani R, Ghazvini K, Lomee M. Sealing ability of orthograde MTA and CEM cement in apically resected roots using bacterial leakage method. Iran Endod J 2013; 8: 109–113. [PMC free article] [PubMed] [Google Scholar]
- Rekha CV, Varma B. Jayanthi Comparative evaluation of tensile bond strength and microleakage of conventional glass ionomercement, resin modified glass ionomer cement and compomer: An in vitro study. Contemp Clin Dent 2012; 3: 282–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvarenga FA, Andrade MA, Pinellic C, Rastelli ANS, Victorino KR, Loffredo LCM. Accuracy of digital images in the detection of marginal microleakage: an in vitro study. J Adhes Dent 2012; 14: 335–338. [DOI] [PubMed] [Google Scholar]
- Radhika M, Sajjan GS, Kumaraswamy BN, Mittal N. Effect of different placement techniques on marginal microleakage of deep class-II cavities restored with two composite resin formulations. J Conserv Dent 2010; 13: 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layton DM, Clarke M. A systematic review and meta-analysis of the survival of non-feldspathic porcelain veneers over 5 and 10 years. Int J Prosthodont 2013; 26: 111–124. [DOI] [PubMed] [Google Scholar]
- Bijelic J, Garoushi S, Vallittu PK. Fracture load of tooth restored with fiber post and experimental short fiber composite. Open Dent J 2011; 29: 58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Bell-Rönnlöf AM, Lassila LV, Kangasniemi I. Load-bearing capacity of human incisor restored with various fiber-reinforced composite posts. Dent Mater 2011; 27: 107–115. [DOI] [PubMed] [Google Scholar]
- Davis P, Melo LS, Foxton RM. Flexural strength of glass fibre-reinforced posts bonded to dual-cure composite resin cements. Eur J Oral Sci 2010; 118: 197–201. [DOI] [PubMed] [Google Scholar]
- Tacken MP, Cosyn J, De Wilde P, Aerts J, Govaerts E, Vannet BV. Glass fibre reinforced versus multistranded bonded orthodontic retainers: A 2 year prospective multi-centre study. Eur J Orthod 2010; 32: 117–123. [DOI] [PubMed] [Google Scholar]
- Alptekin T, Ozer F, Unlu N, Cobanoglu N, Blatz MB. Invitro evaluations of microleakage around class I amalgam and composite restorations. Operat Dent 2010; 35: 641–648. [DOI] [PubMed] [Google Scholar]
- Kanika VG, Pradhuman V, Ashwaryan T. Evaluation of microleakage of various restorative materials: an invitro study. J Life Sci 2011; 3: 29–33. [Google Scholar]
- Larson TD. The clinical significance of marginal fit. Northwest Dent 2012; 91: 22–29. [PubMed] [Google Scholar]
- Moorthy A, Hogg CH, Dowling AH, Grufferty BF, Benetti AR, Fleming GJ. Cuspal deflection and microleakage in premolar teeth restored with bulk-fill flowable resin-based composite base materials. J Dent 2012; 40: 500–505. [DOI] [PubMed] [Google Scholar]
- Gogna R, Jagadis S, Shashikal K. A comparative in vitro study of microleakage by a radioactive isotope and compressive strength of three nanofilled composite resin restorations. J Conserv Dent 2011; 14: 128–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristina L, Boaro C, Goncalves F, Guimaraes TC, Ferracane JL, Versluis A et al. Polymerization stress, shrinkage and elastic modulus of current low shrinkage restorative composites. Dent Mater 2010; 26: 1144–1150. [DOI] [PubMed] [Google Scholar]
- Pakdel A. The effect of bonding agents on the microleakage of fissure sealants (in vitro). J Res Dent Sci Summer 2014; 11: 77–82. [Google Scholar]
- Yuksel E, Zaimoglu A. Influence of marginal fit and cement types on microleakage of all-ceramic crown systems. Braz Oral Res 2011; 25: 261–266. [DOI] [PubMed] [Google Scholar]
- Dennison JB, Sarrett DC. Prediction and diagnosis of clinical outcomes affecting restoration margins. J Oral Rehabil 2012; 39: 301–318. [DOI] [PubMed] [Google Scholar]
- Hooshmand T, Mohajerfar M, Keshvad A, Motahhary P. Microleakage and marginal gap of adhesive cements for noble alloy full cast crowns. Oper Dent 2011; 36: 258–265. [DOI] [PubMed] [Google Scholar]
- Ovul K, Arzu T-M, Ahmet S. Marginal adaptation and microleakeage of directly and indirectly made fiber reinforced composite inlays. Open Dent J 2011; 5: 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yavari HR, Samiei M, Shahi S, Aghazadeh M, Jafari F, Abdolrahimi M. Microleakage comparison of four dental materials as intra-orifice barriers in endodontically treated teeth. Iran Endod J 2012; 7: 25–30. [PMC free article] [PubMed] [Google Scholar]
- Bayrak S, Sen TE, Tuloglu N. The effects of surface pretreatment on the microleakage of resin-modified glass-ionomer cementrestorations. J Clin Pediatr Dent 2012; 36: 279–284. [DOI] [PubMed] [Google Scholar]
- Sarı T, Özyesil AG. Microleakage of teeth restored with different adhesive dowel systems: an in vitro study. J Prosthodont 2014; 23: 45–49. [DOI] [PubMed] [Google Scholar]


