Abstract
Context:
Although the risk of osteoarthritis development after acute knee injury has been widely studied, the long-term consequences of knee overuse injury are not well understood.
Objective:
To identify the relationship between gait-related risk factors associated with osteoarthritis and the development of iliotibial band syndrome (ITBS) in members of a single University Army Reserve Officers' Training Corps unit.
Design:
Prospective cohort study.
Setting:
Biomechanics laboratory.
Patients or Other Participants:
Sixty-eight cadets undergoing standardized physical fitness training.
Intervention(s):
Three-dimensional lower extremity kinematics (240 Hz) and kinetics (960 Hz) were collected for 3 bilateral trials during shod running at 4.0 m/s ± 10%. Injury tracking was conducted for 7 months of training.
Main Outcome Measure(s):
Biomechanical variables, including varus thrust and knee-adduction moment, were compared between the injured and control groups.
Results:
Twenty-six cadets with no history of overuse injury served as the control group, whereas 6 cadets (7 limbs) who developed ITBS that required them to modify their training program or seek medical care (or both) served as the injured group. Maximum varus velocity was higher (P = .006) and occurred sooner during stance (P = .04) in the injured group than in the control group, indicating greater varus thrust. Maximum knee-varus angle and maximum knee-adduction moment were higher (P = .02 and P = .002, respectively) and vertical stiffness was lower (P = .03) in the injured group.
Conclusions:
Measures of dynamic varus stability appeared to be altered in individuals who developed ITBS. Biomechanical knee variables previously identified as increasing the risk for knee osteoarthritis were also associated with the development of ITBS in healthy adults.
Key Words: osteoarthritis, knee overuse injury, neuromuscular control
Key Points
Increased dynamic varus (varus velocity and knee-adduction moment) during loading were risk factors for the development of iliotibial band syndrome in University Army Reserve Officers' Training Corps members.
The risks for iliotibial band syndrome identified in this study have been attributed to lack of neuromuscular control and previously identified as indicative of osteoarthritis risk and severity.
Overuse injuries to the lower extremity are of particular concern in active populations, accounting for 50% to 75% of all injuries in recreational runners and 35% of all musculoskeletal injuries in members of the military.1–3 Previous researchers4 found that up to 80% of individuals who used running as a key component of their physical training experienced overuse injuries requiring a decrease in or cessation of training. Investigators examining overuse injuries to the lower extremity have commonly focused on the lower leg and injuries such as medial tibial stress syndrome and tibial stress fractures5,6; however, in active populations and runners, overuse injuries at or around the knee, such as iliotibial band syndrome (ITBS) and patellofemoral pain, are most common.1,2,7–10
The prevalence of knee injuries in active individuals, including athletes, has fostered a broad range of research into risk factors for injury development as well as the long-term effects of these conditions.4,9,11–16 However, although the risk of long-term consequences, such as osteoarthritis (OA), has been examined in individuals with a history of acute knee injuries, particularly anterior cruciate ligament tears,12,15 less is known about the implications of knee overuse injuries for the long-term development of OA.
Previous authors13,17,18 suggested that sport participation and the repeated loading often associated with overuse injuries increased the risk for OA development, though the relationship between a specific overuse injury such as ITBS and the development of OA is not clear. A number of potential risk factors for the development of ITBS have been identified or proposed, including decreased knee-flexion angle at heel strike,19,20 increased peak hip-adduction angle,10,21 peak knee internal-rotation angle,10,21 peak knee-adduction moment (KAM),22 and iliotibial band strain rate.23 One biomechanical variable that may indicate increased ITBS strain rate is varus thrust. Varus thrust has been associated with increased risk and severity of OA24,25 but has not, to our knowledge, been examined relative to overuse injuries in younger individuals. Varus thrust has been defined as a rapid, abrupt onset of varus alignment24 and reported in degrees,26,27 though the definition suggests that angular velocity may be a more appropriate indicator.28 Knee-adduction moment has also been widely studied as a risk factor for OA development and progression29–31 but has received little attention as a risk for overuse injuries.
Army Reserve Officers' Training Corps (ROTC) cadets are a homogeneous group of participants with a rigorous standardized training regimen that provides an ideal population for prospectively investigating risk factors for knee overuse injuries and for developing potential prevention strategies.7 The purpose of our study was to prospectively identify gait-related risk factors for the development of ITBS in members of a single ROTC unit. Specific variables of interest included varus velocity and KAM.28–31
METHODS
Research Design
A single-cohort, cross-sectional analysis of running gait was performed. The prospective risk of developing a knee overuse injury was determined by assessing cadets' running gait before a physical training cycle and tracking injury development via ongoing medical care by Board of Certification-certified athletic trainers (ATs). We identified prospective biomechanical injury risk factors by comparing the gait mechanics of those cadets who did or did not develop ITBS over the course of the training cycle (approximately 7 months during the academic year).
Participants
Sixty-eight cadets (44 men, 24 women, age = 18–34 years) participating in an ROTC physical training program volunteered for this study. The institutional human subjects committee approved the study, and all participants gave informed consent before data collection. Participants completed a medical and injury history questionnaire that assessed previous acute and overuse injuries to each segment of the lower extremity. All participants were free of any injury to the lower extremity that might have precluded full participation in ROTC training at the time of enrollment. Height was measured with a wall-mounted stadiometer (Seca Telescopic Stadiometer; Country Technology Inc, Gays Mills, WI), and body mass was determined with a scale (model 442; Detecto, Webb City, MO). Body composition was estimated via skinfolds measured in duplicate by the same member of the research team using Lange calipers (BETA Technology, Santa Cruz, CA) at 3 sex-specific sites as described previously.32,33 Descriptive data are presented in Table 1.
Table 1. .
Participants' Descriptive Data (Mean ± SD)
| Characteristic |
Overall (N = 32 limbs) |
Group |
P Value |
|
| Injured (n = 7 limbs) |
Control (n = 26 limbs) |
|||
| Age, y | 22.4 ± 3.1 | 23.2 ± 3.4 | 22.3 ± 3.1 | .75 |
| Height, cm | 172.9 ± 9.8 | 175.0 ± 11.0 | 172.4 ± 9.7 | .35 |
| Mass, kg | 73.7 ± 13.5 | 73.5 ± 12.3 | 73.7 ± 14.0 | .98 |
| Body mass index, m/kg2 | 24.6 ± 3.4 | 23.9 ± 1.9 | 24.7 ± 3.7 | .26 |
| Body fat, % | 12.6 ± 7.9 | 14.9 ± 9.8 | 12.0 ± 7.8 | .69 |
Instrumentation and Protocol
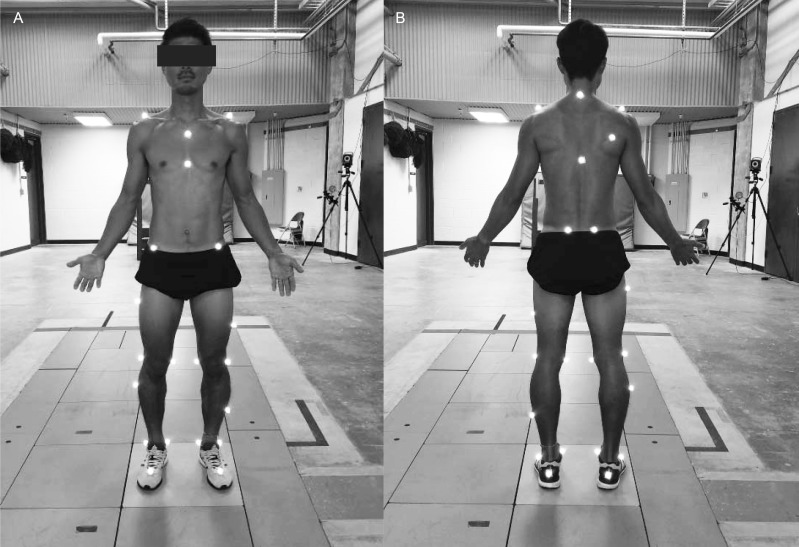
Gait analysis was completed during the month before the start of the 7-month training cycle at a single data-collection session in which participants were instructed to wear the running shoes they used for daily training.34 Nonstandardized shoes were worn so that we could most closely capture the gait biomechanics each individual would experience during training sessions. Kinematic data were collected using a 3-dimensional motion-capture system (Vicon Inc, Centennial, CO) positioned along an 18-m runway and 27 retroreflective markers (Figure 1). Kinetic data were recorded using a force plate (Advanced Mechanical Technology Inc, Boston, MA) embedded flush with the runway. Kinematic data were collected at 240 Hz, time synchronized with the kinetic data collected at 960 Hz, and then smoothed using a Woltring filter with a 10-Hz mean squared error cutoff. Nexus (Vicon Inc) and Visual 3D (C-Motion Inc, Germantown, MD) software was used to capture, reduce, and analyze the gait data.
Figure 1. .
Marker locations for kinematic data collection. A, Anterior view. B, Posterior view.
Before biomechanical analysis, participants completed a self-directed warm-up, and familiarization running trials were conducted to ensure a consistent running velocity. Running velocity was ascertained using Speedtrap II infrared sensors (Brower Timing Systems, Draper, UT) placed 4 m apart and centered on the force plate. A running trial was considered successful if the participant ran at the prescribed velocity (4.0 m/s ± 10%)34 and landed with the entire foot on the force plate without apparent targeting.6 Three successful trials were recorded for each leg, and the mean of these trials was used for analysis.35,36
The subsequent training program lasted approximately 7 months and consisted of 1- to 2-hour training sessions 3 or 4 times per week as a group. These training sessions included a wide range of aerobic, plyometric and body-weight resistance exercises and calisthenics-based activities. Aerobic activities included medium-distance runs (∼2 mi [3.2 km]), relay-type activities, team-based field games (eg, ultimate Frisbee and football), and longer marches or runs as a squad. Plyometrics, body-weight resistance, and calisthenics exercises included interval training activities, push-ups, pull-ups, sit-ups, and similar full-body nonaerobic activities.
Data Analysis
An AT provided ongoing medical care throughout the evaluation period and assessed all potential overuse injuries to the lower extremity. Participants were included in the control group if they reported no history of lower extremity overuse injury and did not develop a lower extremity injury during the study period. We defined injury as a condition requiring a reduction in the amount or level of physical training or activity or the need for medical advice or treatment.35 Participants who developed injuries involving the knee with an insidious onset, associated with repetitive physical activities,7 and subsequently diagnosed by the AT or physician as ITBS were assigned to the injury group. The data from participants who developed other lower extremity overuse (eg, medial tibial stress syndrome, Achilles tendinitis, or plantar fasciitis) or acute injuries were excluded from analysis.
Vertical stiffness (Kvert) was calculated as the maximum vertical ground reaction force in kilonewtons divided by the change in vertical center-of-mass displacement in meters.37 Due to a significant positive correlation (r = 0.63, P < .001) between Kvert and body mass, Kvert was scaled for body mass.38
All statistical procedures were conducted using SPSS (version 20; IBM Corp, Armonk, NY). Multiple factorial general linear model 2-way analyses of variance (group: injured versus control; sex; group × sex) were used to assess differences in kinetic and kinematic gait variables between the injured and control groups. To account for any confounding effects of combining sexes when examining biomechanical variables associated with injury, differences between the injury and control groups were only considered relevant when the interaction effect (group × sex) was not significant, indicating that the effect of the biomechanical variable on injury was not different between sexes. Multiple 1-way analyses of variance were used to compare anthropometric characteristics between groups. An α level of P < .05 was identified as a significant difference. Data from only the right leg of each participant in the control group were used in the analysis; all injured limbs were included in the analysis for the injury group, including both limbs of 1 individual who developed bilateral ITBS. All kinetic moment variables were reported as external moments.
RESULTS
A total of 68 participants (44 men, 24 women) completed the initial overuse injury history questionnaire and biomechanical analysis. Twenty-six participants (38.2%; 20 men, 6 women) remained injury free during the study period, did not report a previous lower extremity overuse injury, and were assigned to the control group. A total of 20 participants (29.4%) developed lower extremity overuse injuries during the study period. Six of these 20 participants (30%) developed ITBS diagnosed as serious enough to require modifications to training or received medical care during the study period and were assigned to the injury group for analysis. One of these 6 participants experienced bilateral ITBS, resulting in 7 total injured limbs (men: 1 left leg, 1 right leg, 1 bilateral; women: 2 left legs, 1 right leg) analyzed. The remaining participants were excluded from analysis because they (1) developed a lower extremity overuse injury other than ITBS (n = 13); (2) did not complete the study due to midyear graduation, pursuing basic training, or dropping out of ROTC (n = 5); or (3) sustained an acute injury or other condition that precluded the inclusion of their data in the final analysis (n = 17).
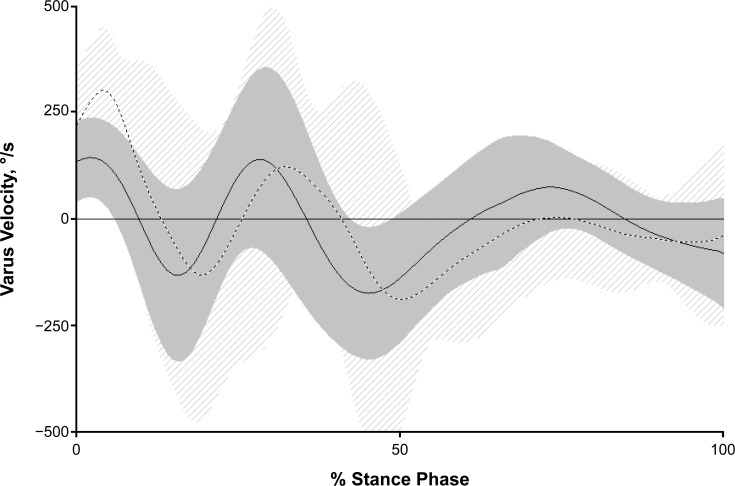
Participants in the control group were not directly matched to those who developed ITBS for any anthropometric or body composition variables; however, such variables collected at the beginning of the study were not different between the control group and those who developed knee overuse injuries (Table 1). The frontal-plane knee variables of maximum knee varus, knee-varus velocity, and external KAM, as well as the timing of maximum varus velocity during stance, were different between controls and those who developed ITBS during the testing period (Table 2). Additionally, varus velocity varied between control and injured participants throughout the stance phase (Figure 2). Maximum vertical ground reaction force (injured: 23.4 ± 1.1 N/kg; control: 25.3 ± 2.2; P = .12) and loading rate (injured: 1.5 × 104 ± 0.2 × 104 N/s; control: 1.6 × 104 ± 0.3 × 104; P = .95) were not different between groups.
Table 2. .
Between-Groups Comparison of Biomechanical Variables (Mean ± SD)
| Biomechanical Variable |
Group |
P Value |
|
| Injured (n = 7 limbs) |
Control (n = 26 limbs) |
||
| Kinematics | |||
| Maximum knee varus, ° | 12.0 ± 4.4 | 7.3 ± 5.2 | .02a |
| Maximum knee-varus velocity, °/s | 281.6 ± 117.0 | 183.4 ± 73.3 | .006a |
| Mean knee-varus velocity, °/s | 124.9 ± 40.4 | 63.4 ± 40.8 | .001a |
| Time of maximum knee-varus velocity, % stance | 15.7 ± 13.8 | 34.5 ± 24.2 | .04a |
| Kinetics | |||
| Maximum knee-adduction moment, Nm/kg | 2.6 ± 0.5 | 2.0 ± 0.5 | .002a |
| Maximum hip-adduction moment, Nm/kg | 2.3 ± 0.3 | 1.8 ± 0.4 | .01a |
| Ground reaction forces | |||
| Maximum vertical ground reaction force, N/kg | 23.4 ± 1.1 | 25.3 ± 2.2 | .12 |
| Loading rate, N/s | 1.5 × 104 ± 0.2 × 104 | 1.6 × 104 ± 0.3 × 104 | .95 |
| Vertical stiffness, kN·m−1·kg−1 | 0.55 ± 0.05 | 0.62 ± 0.10 | .03a |
Indicates difference (P < .05).
Figure 2. .
Knee-varus velocity (mean ± standard deviation) during stance phase for participants who developed iliotibial band syndrome (dashed line) compared with control participants (solid line).
DISCUSSION
The most important finding of our prospective injury study was the identification of dynamic varus variables, including varus thrust and KAM, as risk factors for ITBS. These variables have been commonly associated with OA risk and progression28–31 but have been given little consideration relative to the development of overuse injuries. The identification of these variables as risk factors for soft tissue overuse injury to the knee in otherwise healthy younger adults may indicate a relationship that has not been previously recognized between soft tissue overuse injury to the knee and risk for the eventual development of knee OA.
A number of frontal-plane variables, including maximum knee-varus angle, maximum varus velocity, and maximum KAM, were higher, and maximum varus velocity occurred earlier during stance in the injured group (Table 2). These differences were noted despite nonsignificant differences between groups in 2 important kinetic variables: maximum vertical ground reaction force and loading rate. These findings suggest that it was not greater overall force during loading or a greater rate of loading force that led to ITBS in the injury group. Rather, the manner and timing in which force was applied to the knee during loading may have led to increased soft tissue loading, increased strain rates, and overuse injury. Additionally, changes in frontal-plane joint velocity and associated variables were interpreted as a decrease in dynamic varus stability during loading among the injured participants.
The differences in dynamic varus stability between the injured and control groups in our study have not, to our knowledge, been examined previously relative to overuse injuries in otherwise healthy young people. However, similar differences, previously identified as “varus thrust,” have been reported as indicators of progression and severity of knee OA.24,25 Varus thrust was defined by Chang et al24,25,28(p1668) as the “dynamic worsening or abrupt onset of varus alignment as the limb accepts weight,” though their initial examinations were qualitative in nature. Subsequent researchers26,27 have examined varus thrust relative to joint angle (in degrees). However, as the initial definition and subsequent work by Chang et al24,25 suggested, the velocity at which the varus motion occurs is likely more important when considering dynamic varus stability. We noted this in our study: maximum knee-varus velocity varied between injured and control participants and throughout the stance phase (Figure 2). Furthermore, maximum and mean knee-varus velocity were higher (P = .006 and P = .001, respectively) among those who developed ITBS. These results support the contention of Hamill et al,23 using computer modeling, that strain rate may be more important than magnitude alone in these overuse injuries.
Recently, Chang et al39 proposed that compromised frontal-plane control, including decreases in muscular strength and control, may be the cause of varus instability. Combined with our findings, which demonstrated the role of dynamic frontal instability in the development of soft tissue overuse injury to the knee, the results indicate that prevention and treatment of these injuries should focus on improving deficits in muscular strength and control. This strategy is supported by the work of Dolak et al,40 who found greater improvements in participants with patellofemoral pain syndrome from increasing frontal-plane strength compared with sagittal-plane quadriceps strength.
Williams et al41 observed that differences in arch structure were associated with differences in lower extremity stiffness and demonstrated that specific injuries among runners varied based on arch structure and associated stiffness.37 Williams et al37,41 suggested that stiffness levels above or below an optimal zone lead to specific types of injury and that a decrease in lower extremity stiffness may indicate reliance on a soft tissue force-absorption mechanism, resulting in an increased risk of soft tissue injury, whereas an increase in lower extremity stiffness may indicate reliance on a bony force-absorption mechanism, leading to an increased risk of bony injury. However, to our knowledge, evidence supporting this theory relative to knee overuse injury has not been presented previously. Our finding, that lower extremity stiffness in the injured group was lower than that of the controls, as evidenced by the lower Kvert, provides support for the theory suggesting that lower extremity stiffness below an optimal point may lead to soft tissue overuse injury, in this case ITBS, due to overreliance on a soft tissue absorption mechanism.
Further consideration of an optimal range for lower extremity stiffness to avoid injury may seem, at first glance, to reduce the strength of any relationship between the risks for ITBS and subsequent OA because OA is a bony injury. Yet the mechanism behind OA development and progression is widely understood to be associated with increased force on the medial compartment during varus loading as opposed to overall increased bony absorption such as that associated with increased leg stiffness.29,42,43 Therefore, the decreased stiffness we identified can be understood to increase the risk of injury to the iliotibial band while simultaneously allowing increased loading of the medial compartment of the knee and potentially increasing the long-term risk for OA development and progression in some individuals.
A number of limitations may have affected the findings of our study. Although participants who reported an injury history were not included in the control group, previous injury to the lower extremity did not serve as an exclusion criterion for participants who subsequently developed ITBS during the study period. An injury history in those who developed ITBS may have introduced aspects of gait that were different from those in the control group but were not associated with the development of ITBS during the prospective injury-tracking period. Additionally, we chose to use right-leg data for all participants in the control group, which may constitute a limitation. An alternative approach is to use dominant or nondominant leg data from control participants; however, there is significant debate as to what constitutes dominant versus nondominant in an individual when applied to the lower extremity.44 The small number of women included in the study, in both the injured and control groups, may have produced inadequate power to examine interaction effects. However, we restricted the use of these nonsignificant interactions to assessing sex differences between biomechanical variables that were statistically different; that is, the effect size was large enough to produce adequate power at the given sample size. Finally, the training program followed by the ROTC members in this study was different from training programs typically used in traditional organized sport settings. None of the activities were sport skill specific, and the total volume of training was lower than in most organized training programs for high school or collegiate athletes. These aspects of the training program may constrain the generalizability of our results to highly competitive athletes in specific sports, particularly in sports that do not commonly employ skills or movements that require frontal-plane dynamic knee stability. Yet it may be argued that for other sports that commonly demand frontal-plane knee stability, the risks associated with injury in our study may be even more likely to be associated with ITBS, especially when paired with increased training volume. The broad range of activities and the overall volume of the ROTC training program were comparable with what a typical adult in recreational or competitive training may experience. Therefore, the results of our study may be most generalizable to this population.
In summary, we found that the primary risk factors for the development of ITBS were related to measures of dynamic varus stability, including maximum varus velocity (varus thrust) and KAM. These risk factors were similar to those previously reported only in individuals who developed knee OA. Prevention and treatment of ITBS should focus on improving dynamic varus stability by improving strength and neuromuscular control.
REFERENCES
- 1. Hauret KG, Jones BH, Bullock SH, Canham-Chervak M, Canada S. . Musculoskeletal injuries: description of an under-recognized injury problem among military personnel. Am J Prev Med. 2010; 38 suppl 1: S61– S70. [DOI] [PubMed] [Google Scholar]
- 2. Fields KB. . Running injuries - changing trends and demographics. Curr Sports Med Rep. 2011; 10 5: 299– 303. [DOI] [PubMed] [Google Scholar]
- 3. van Mechelen W. . Running injuries. A review of the epidemiological literature. Sports Med. 1992; 14 5: 320– 335. [DOI] [PubMed] [Google Scholar]
- 4. van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SM, Koes BW. . Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007; 41 8: 469– 480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Loudon JK, Reiman MP. . Lower extremity kinematics in running athletes with and without a history of medial shin pain. Int J Sports Phys Ther. 2012; 7 4: 356– 364. [PMC free article] [PubMed] [Google Scholar]
- 6. Milner CE, Davis IS, Hamill J. . Free moment as a predictor of tibial stress fracture in distance runners. J Biomech. 2006; 39 15: 2819– 2825. [DOI] [PubMed] [Google Scholar]
- 7. Almeida SA, Williams KM, Shaffer RA, Brodine SK. . Epidemiological patterns of musculoskeletal injuries and physical training. Med Sci Sports Exerc. 1999; 31 8: 1176– 1182. [DOI] [PubMed] [Google Scholar]
- 8. Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. . A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002; 36 2: 95– 101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yang J, Tibbetts AS, Covassin T, Cheng G, Nayar S, Heiden E. . Epidemiology of overuse and acute injuries among competitive collegiate athletes. J Athl Train. 2012; 47 2: 198– 204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ferber R, Noehren B, Hamill J, Davis IS. . Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010; 40 2: 52– 58. [DOI] [PubMed] [Google Scholar]
- 11. Almeida SA, Williams Maxwell K, Shaffer RA, Brodine SK. . Epidemiological patterns of musculoskeletal injuries and physical training. Med Sci Sports Exerc. 1999; 31 8: 1176– 1182. [DOI] [PubMed] [Google Scholar]
- 12. Barenius B, Ponzer S, Shalabi A, Bujak R, Norlen L, Eriksson K. . Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014; 42 5: 1049– 1057. [DOI] [PubMed] [Google Scholar]
- 13. Buckwalter JA. . Sports, joint injury, and posttraumatic osteoarthritis. J Orthop Sports Phys Ther. 2003; 33 10: 578– 588. [DOI] [PubMed] [Google Scholar]
- 14. Ferber R, Noehren B, Hamill J, Davis I. . Competitive female runners with a history of iliotibial band syndrome demonstrate atypical hip and knee kinematics. J Orthop Sports Phys Ther. 2010; 40 2: 52– 58. [DOI] [PubMed] [Google Scholar]
- 15. Risberg MA, Oiestad BE, Gunderson R, et al. Changes in knee osteoarthritis, symptoms, and function after anterior cruciate ligament reconstruction: a 20-year prospective follow-up study. Am J Sports Med. 2016; 44 5: 1215– 1224. [DOI] [PubMed] [Google Scholar]
- 16. Gray AM, Buford WL. . Incidence of patients with knee strain and sprain occurring at sports or recreation venues and presenting to United States emergency departments. J Athl Train. 2015; 50 11: 1190– 1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kujala UM, Kaprio J, Sarna S. . Osteoarthritis of weight bearing joints of lower limbs in former elite male athletes. BMJ. 1994; 308 6923: 231– 234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Spector TD, Harris PA, Hart DJ, et al. Risk of osteoarthritis associated with long-term weight-bearing sports: a radiologic survey of the hips and knees in female ex-athletes and population controls. Arthritis Rheum. 1996; 39 6: 988– 995. [DOI] [PubMed] [Google Scholar]
- 19. Miller RH, Lowry JL, Meardon SA, Gillette JC. . Lower extremity mechanics of iliotibial band syndrome during an exhaustive run. Gait Posture. 2007; 26 3: 407– 413. [DOI] [PubMed] [Google Scholar]
- 20. Orchard JW, Fricker PA, Abud AT, Mason BR. . Biomechanics of iliotibial band friction syndrome in runners. Am J Sports Med. 1996; 24 3: 375– 379. [DOI] [PubMed] [Google Scholar]
- 21. Noehren B, Davis I, Hamill J. . ASB clinical biomechanics award winner 2006 prospective study of the biomechanical factors associated with iliotibial band syndrome. Clin Biomech (Bristol, Avon). 2007; 22 9: 951– 956. [DOI] [PubMed] [Google Scholar]
- 22. Foch E, Milner CE. . Frontal plane running biomechanics in female runners with previous iliotibial band syndrome. J Appl Biomech. 2014; 30 1: 58– 65. [DOI] [PubMed] [Google Scholar]
- 23. Hamill J, Miller R, Noehren B, Davis I. . A prospective study of iliotibial band strain in runners. Clin Biomech (Bristol, Avon). 2008; 23 8: 1018– 1025. [DOI] [PubMed] [Google Scholar]
- 24. Chang A, Hayes K, Dunlop D, et al. Thrust during ambulation and the progression of knee osteoarthritis. Arthritis Rheum. 2004; 50 12: 3897– 3903. [DOI] [PubMed] [Google Scholar]
- 25. Chang A, Hochberg M, Song J, et al. Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk of developing knee osteoarthritis. Arthritis Rheum. 2010; 62 5: 1403– 1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hunt MA, Schache AG, Hinman RS, Crossley KM. . Varus thrust in medial knee osteoarthritis: quantification and effects of different gait-related interventions using a single case study. Arthritis Care Res. 2011; 63 2: 293– 297. [DOI] [PubMed] [Google Scholar]
- 27. Roda RD, Wilson JL, Wilson DA, Richardson G, Dunbar MJ. . The knee adduction moment during gait is associated with the adduction angle measured during computer-assisted total knee arthroplasty. J Arthroplasty. 2012; 27 6: 1244– 1250. [DOI] [PubMed] [Google Scholar]
- 28. Chang AH, Chmiel JS, Moisio KC, et al. Varus thrust and knee frontal plane dynamic motion in persons with knee osteoarthritis. Osteoarthritis Cartilage. 2013; 21 11: 1668– 1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Astephen JL, Deluzio KJ, Caldwell GE, Dunbar MJ. . Biomechanical changes at the hip, knee, and ankle joints during gait are associated with knee osteoarthritis severity. J Orthop Res. 2008; 26 3: 332– 341. [DOI] [PubMed] [Google Scholar]
- 30. Kuroyanagi Y, Nagura T, Kiriyama Y, et al. A quantitative assessment of varus thrust in patients with medial knee osteoarthritis. Knee. 2012; 19 2: 130– 134. [DOI] [PubMed] [Google Scholar]
- 31. Lo GH, Harvey WF, McAlindon TE. . Associations of varus thrust and alignment with pain in knee osteoarthritis. Arthritis Rheum. 2012; 64 7: 2252– 2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jackson AS, Pollock ML. . Generalized equations for predicting body density of men. Br J Nutr. 1978; 40 3: 497– 504. [DOI] [PubMed] [Google Scholar]
- 33. Jackson AS, Pollock ML, Ward A. . Generalized equations for predicting body density of women. Med Sci Sports Exerc. 1980; 12 3: 175– 181. [PubMed] [Google Scholar]
- 34. Bennell K, Crossley K, Jayarajan J, et al. Ground reaction forces and bone parameters in females with tibial stress fracture. Med Sci Sports Exerc. 2004; 36 3: 397– 404. [DOI] [PubMed] [Google Scholar]
- 35. Willems TM, De Clercq D, Delbaere K, Vanderstraeten G, De Cock A, Witvrouw E. . A prospective study of gait related risk factors for exercise-related lower leg pain. Gait Posture. 2006; 23 1: 91– 98. [DOI] [PubMed] [Google Scholar]
- 36. Willems TM, Witvrouw E, De Cock A, De Clercq D. . Gait-related risk factors for exercise-related lower-leg pain during shod running. Med Sci Sports Exerc. 2007; 39 2: 330– 339. [DOI] [PubMed] [Google Scholar]
- 37. Williams DS III, Davis IM, Scholz JP, Hamill J, Buchanan TS. . High-arched runners exhibit increased leg stiffness compared to low-arched runners. Gait Posture. 2004; 19 3: 263– 269. [DOI] [PubMed] [Google Scholar]
- 38. Padua DA, Arnold BL, Perrin DH, Gansneder BM, Carcia CR, Granata KP. . Fatigue, vertical leg stiffness, and stiffness control strategies in males and females. J Athl Train. 2006; 41 3: 294– 304. [PMC free article] [PubMed] [Google Scholar]
- 39. Chang AH, Lee SJ, Zhao H, Ren Y, Zhang LQ. . Impaired varus-valgus proprioception and neuromuscular stabilization in medial knee osteoarthritis. J Biomech. 2014; 47 2: 360– 366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dolak KL, Silkman C, Medina McKeon J, Hosey RG, Lattermann C, Uhl TL. . Hip strengthening prior to functional exercises reduces pain sooner than quadriceps strengthening in females with patellofemoral pain syndrome: a randomized clinical trial. J Orthop Sports Phys Ther. 2011; 41 8: 560– 570. [DOI] [PubMed] [Google Scholar]
- 41. Williams DS III McClay IS, Hamill J. . Arch structure and injury patterns in runners. Clin Biomech (Bristol, Avon). 2001; 16 4: 341– 347. [DOI] [PubMed] [Google Scholar]
- 42. Astephen JL, Deluzio KJ. . Changes in frontal plane dynamics and the loading response phase of the gait cycle are characteristic of severe knee osteoarthritis application of a multidimensional analysis technique. Clin Biomech (Bristol, Avon). 2005; 20 2: 209– 217. [DOI] [PubMed] [Google Scholar]
- 43. Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. . Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002; 61 7: 617– 622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Sadeghi H, Allard P, Prince F, Labelle H. . Symmetry and limb dominance in able-bodied gait: a review. Gait Posture. 2000; 12 1: 34– 45. [DOI] [PubMed] [Google Scholar]