Abstract
Objective:
To evaluate the current evidence concerning kinematic and kinetic strategies adopted during dynamic landing tasks by patients with anterior cruciate ligament reconstruction (ACLR).
Data Sources:
PubMed, Web of Science.
Study Selection:
Original research articles that evaluated kinematics or kinetics (or both) during a landing task in those with a history of ACLR were included.
Data Extraction:
Methodologic quality was assessed using the modified Downs and Black checklist. Means and standard deviations for knee or hip (or both) kinematics and kinetics were used to calculate Cohen d effect sizes and corresponding 95% confidence intervals between the injured limb of ACLR participants and contralateral or healthy matched limbs. Data were further stratified by landing tasks, either double- or single-limb landing. A random-effects–model meta-analysis was used to calculate pooled effect sizes and 95% confidence intervals.
Data Synthesis:
The involved limbs of ACLR patients demonstrated clinically and significantly lower knee-extension moments during double-legged landing compared with healthy contralateral limbs and healthy control limbs (Cohen d range = −0.81 to −1.23) and decreased vertical ground reaction forces when compared with healthy controls, regardless of task (Cohen d range = −0.39 to −1.75).
Conclusions:
During single- and double-legged landing tasks, individuals with ACLR demonstrated meaningful reductions in injured-limb knee-extension moments and vertical ground reaction forces. These findings indicate potential unloading of the injured limb after ACLR, which may have significant implications for secondary ACL injury and long-term joint health.
Key Words: biomechanics, joint moments, injuries
Key Points
During dynamic tasks, patients with a history of anterior cruciate ligament reconstruction shifted joint loading to the contralateral limb as shown by reductions in knee-joint moments and vertical ground reaction forces in the injured limb.
Biomechanical risk factors for secondary anterior cruciate ligament injury are likely different than those for primary injury.
Rupture of the anterior cruciate ligament (ACL) is a debilitating sport-related injury, and many patients elect to undergo surgical reconstruction (ACLR) and aggressive rehabilitation. Roughly 80% of these injuries occur from a noncontact mechanism during dynamic activity,1,2 which suggests that the ACL injury risk is greatly influenced by movement strategies during these activities.3,4 The literature3,5,6 assessing ACL injury risk has most commonly used variations of landing maneuvers to replicate high-risk scenarios, as the majority of ACL injuries occur during these maneuvers. More importantly, previous researchers have identified specific movement strategies at the hip and knee that place individuals at a greater risk for ACL injury. In particular, reduced flexion,7–9 excessive abduction,4,10 and excessive internal-rotation angles at the knee11–13 and reduced flexion,7–9 excessive adduction,14 and excessive internal-rotation angles at the hip14–16 during landing are thought to increase the ACL injury risk. Abnormal joint loading in the frontal plane of the knee4,17,18 is also thought to increase the risk of ACL injury.
The ability to prospectively identify differences in landing strategies between those who go on to sustain an ACL injury and those who do not has prompted the development of ACL injury-prevention programs that focus on neuromuscular and biomechanical interventions for the purpose of correcting these potentially hazardous movement patterns and reducing injury rates.19–21 Although recent assessments have demonstrated ACL injury-prevention programs to be effective in reducing the injury risk,22,23 many of the studies24,25 have focused on young female athletes, with less information known regarding their male counterparts.
Approximately 250 000 ACL ruptures occur annually in the United States.3 Approximately 40% of these individuals will not return to their preinjury activity levels.26 Those who do return to activity, in particular, those who are young and involved in pivoting and cutting sports, face rates of ACL reinjury that are reported to be as high as 20% to 25%,27–30 with a 15-times greater risk of subsequent ACL injury compared with the risk of initial ACL injury.27
Similar to the initial ACL injury risk, subsequent rupture is likely a result of poor movement strategies that were not addressed during ACLR and therapeutic rehabilitation. In fact, Paterno et al28 demonstrated that increased frontal-plane movement at the knee and transverse-plane moment at the hip significantly predicted secondary ACL injury, providing evidence that altered movement strategies may influence the risk of a second ACL injury.4 However, despite the increased risk for secondary ACL injury compared with the risk for primary injury, a comprehensive understanding of the lower extremity biomechanical adaptations observed after ACLR is lacking. This information would guide clinicians and researchers to a more systematic strategy for evaluating the reinjury risk in these patients. Improving the knowledge base regarding potentially modifiable biomechanical risk factors will also aid in the development of targeted interventions for patients with ACLR. Although observed differences in landing biomechanics between patients with ACLR and healthy controls will not supply direct evidence for the risk factors of future injury, it will be an initial step in identifying specific patterns of lower extremity movement for clinicians to monitor and for researchers to investigate in terms of how these movement patterns may influence future injury risk and prevention strategies.
Therefore, the purpose of our investigation was to systematically evaluate the current evidence concerning kinematic and kinetic strategies demonstrated by patients after ACLR. Specifically, we looked to assess the hip and knee biomechanics of the involved limb and compare them with those of the contralateral uninjured limb as well as healthy control limbs during dynamic landing assessments (vertical jumps, drop jumps).
METHODS
Literature Search Strategy
An online search using the PubMed and Web of Science databases was performed on June 4, 2016, to obtain pertinent peer-reviewed articles. The search strategy consisted of the terms anterior cruciate ligament OR ACL AND reconstruction, AND landing biomechanics OR kinematics OR kinetics. We assessed the titles of all articles retrieved by the search engines for their relevance and further evaluated those with merit. In addition, reference sections from pertinent articles were checked to locate any relevant articles that were not revealed during the initial search.
Selection Criteria
To be included, an article needed to be original research and written in English. No limitations were placed on the date of publication. All included articles evaluated kinematics or kinetics (or both) during a landing task in the injured limb of those with a history of ACLR compared with their own uninjured contralateral limb or participants in a healthy control group. Each investigation also provided means and standard deviations (SDs) for knee or hip kinematics that were assessed at the point of initial contact (IC) during the landing task, peak joint angle throughout the landing phase of the task, or total joint range of motion (joint excursion) throughout the primary landing phase of the task. In addition, peak kinetics and vertical ground reaction forces (vGRFs) over the course of the landing task were also included in this analysis. After reviewing the potential articles, we agreed on the final manuscripts to be included in this review.
Assessing Methodologic Quality
A modified version of the Downs and Black checklist was used to assess the methodologic quality of the included studies.31 The modified Downs and Black checklist is a valid and reliable instrument used for assessing both randomized and nonrandomized investigations.31 This assessment carries a maximum score of 15, with scores of ≥12 indicating high methodologic quality, 10–11 indicating moderate quality, and ≤9 representing low quality.31,32 This classification was not used to assess the studies for the inclusion or exclusion criteria but only to assess each one's methodologic quality. We independently reviewed and scored each article based on the Downs and Black checklist and agreed on the methodologic quality of 18 of the 20 included articles and discussed the remaining articles until a consensus was reached (see the Supplemental Table, available online at http://dx.doi.org/10.4085/1062-6050-334-16.S1).
Data Management and Statistical Approach
Each author reviewed every article. Data regarding hip and knee kinematics and kinetics were extracted and entered into an Excel spreadsheet (Microsoft Corp, Redmond, WA). Specifically, frontal-, sagittal-, and transverse-plane knee and hip angles at IC and peak and joint angle excursions were extracted from each study where applicable. In addition, peak knee and hip moments and peak vGRF were also extracted for analysis. Data were analyzed by limb using 2 comparisons: (1) the ACLR limb compared with the contralateral uninjured limb and (2) the ACLR limb compared with a healthy matched control limb. In addition, the type of landing task (single-legged or double-legged landing) was also collected and used to stratify data by task. When comprehensive data or means and SDs were not provided, we contacted the corresponding author via e-mail to request appropriate data.
Means and SDs from each variable of interest were used to calculate standardized Cohen d effect sizes (ACLR limb − comparison limb/pooled SD) with associated 95% confidence intervals (CIs). Therefore, a negative effect size indicated the ACLR limb had a lower value than the comparison limb. Effect sizes were classified as weak (d ≤ 0.2), small (d = 0.2–0.5), moderate (d = 0.5–0.8), or large (d ≥ 0.8).33 Differences between comparison groups in individual studies were established if the CI associated with an effect size did not cross 0 (y-axis). In addition, we used a random-effects–model meta-analysis approach to calculate pooled effect sizes and 95% CIs for each group of variables.
Other pertinent information collected from each study was demographics, activity level, time since surgery, sex, and graft type when reported.
RESULTS
Literature Search
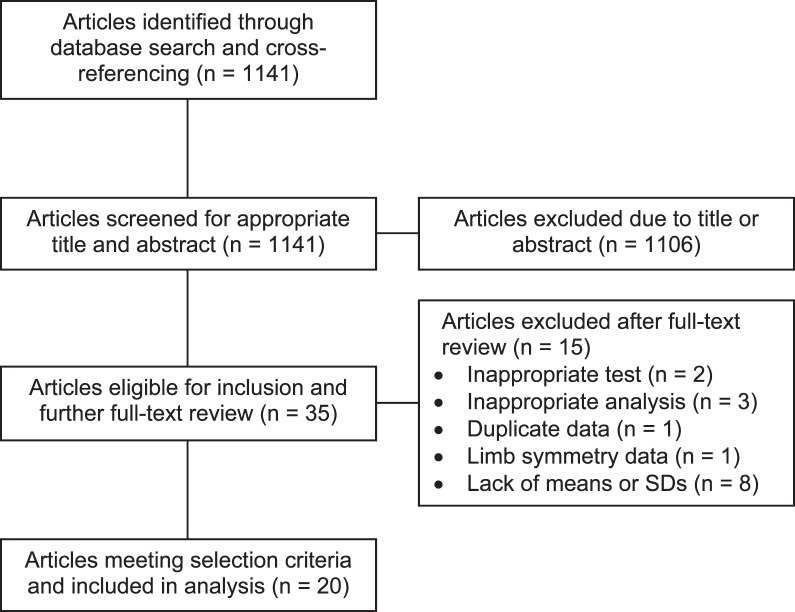
The initial database search and cross-referencing yielded 1141 articles. A total of 35 articles were eligible for inclusion beyond title and abstract review, and each of us further evaluated the full texts of these articles. Two articles were removed because they evaluated a horizontal hopping task as opposed to a landing task.34,35 Three articles used a clinical assessment of landing (Landing Error Scoring System) with no objective kinematic or kinetic data and were therefore removed.36–38 One article28 was removed, as it was a further analysis of data from another published study that was already included in this review.39 Another article40 was removed for publishing only limb symmetry scores as opposed to data for individual limbs. Eight additional articles41–48 were removed because the authors did not report means SDs or reply to requests for data. Therefore, 20 articles39,49–67 met the selection criteria and were included in the analysis (Figure 1). Of the included articles, 8 used double-limb landing tasks and 12 used single-limb landing tasks.
Figure 1. .
Flow chart of literature search. Abbreviation: SD, standard deviation.
Only 4 of the included studies provided separate data for cohorts within the ACLR groups. Nyland et al58 and Miranda et al56 reported individual data for males and females, Nyland et al59 reported data by the activity levels of the ACLR participants, and Mohammadi et al57 separated data by graft type (bone-patellar tendon-bone and semiten-dinosis-gracilis autografts). These data are reported separately for the corresponding articles.
Methodologic Quality
Five of the 20 studies (25%) were classified as high quality, 11 (55%) were of moderate quality, and 4 (20%) were of low quality (see the Supplemental Table).
Hip Kinematics
A total of 19 data points from 9 studies were analyzed for hip-flexion angles (Table 1A). A homogeneous effect (4/4 studies fell left of the y-axis) was present for reduced peak and IC hip-flexion angles in the ACLR limb during double-limb landing; however, 3 of 4 CIs crossed 0 (Cohen d range = −0.19 to 1.06). The combined effect for all 4 data points was moderate, with effect sizes not crossing zero (Cohen d = −0.52; 95% CI = −0.92, −0.12; Table 1A). During single-limb landing, the effect for increased hip-flexion angles at IC in the ACLR limb was homogeneous (4/4) when compared with both contralateral limbs and healthy controls (Cohen d range = 0.33 to 0.77; Table 1A). However, the effects were inconclusive or heterogeneous for sagittal-plane hip-joint excursion and peak hip-flexion angle (Cohen d range = −0.74 to 0.99; Table 1A).
Table 1A. .
Between-Groups Comparisons and Cohen d Effect Sizes of Sagittal-Plane Hip-Joint Angles
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Hip-Flexion Angle |
ACL Contralateral-Limb Hip-Flexion Angle |
Healthy Hip-Flexion Angle |
|||||||
| Decker et al50 (2002) | Double | 11 | 11 | 22.6 ± 5.8 | NA | 29.8 ± 7.7 | IC | −1.06 (−1.96, −0.17) | −1.48 |
| Decker et al50 (2002) | Double | 11 | 11 | 29.7 ± 6.2 | NA | 31.2 ± 6.7 | JE | −0.23 (−1.07, 0.61) | −0.33 |
| Delahunt et al52 (2012) | Double | 13 | 16 | 45.9 ± 8.6 | NA | 47.5 ± 8.4 | JE | −0.19 (−0.92, 0.54) | −0.29 |
| Delahunt et al52 (2012) | Double | 14 | 14 | 29.7 ± 6.8 | NA | 34.6 ± 6.4 | JE | −0.73 (−1.49, 0.02) | −1.11 |
| Combined pooled effect size (95% CI) | −0.52 (−0.92, −0.12) | ||||||||
| Vairo et al66 (2008) | Single | 14 | 14 | 29.7 ± 9.0 | NA | 23.6 ± 6.5 | IC | 0.77 (0.00, 1.54) | 5.05 |
| Webster et al67 (2012) | Single | 15 | 11 | 32.1 ± 6.7 | NA | 27.5 ± 6.7 | IC | 0.68 (−0.12, 1.48) | 4.11 |
| Ortiz et al60 (2008) | Single | 14 | 15 | 45.9 ± 7.1 | NA | 49.5 ± 6.9 | Peak | −0.51 (−1.25, 0.23) | −3.59 |
| Vairo et al66 (2008) | Single | 14 | 14 | 31.7 ± 8.8 | NA | 24.2 ± 6.0 | Peak | 0.99 (0.20, 1.77) | 6.21 |
| Webster et al67 (2012) | Single | 15 | 11 | 52.0 ± 12.1 | NA | 50.3 ± 12.1 | Peak | 0.14 (−0.64, 0.92) | 0.89 |
| Combined pooled effect size (95% CI) | 0.40 (−0.13, 0.94) | ||||||||
| Vairo et al66 (2008) | Single | 14 | 14 | 29.7 ± 9.0 | 25.6 ± 8.3 | NA | IC | 0.47 (−0.28, 1.20) | 3.22 |
| Webster et al67 (2012) | Single | 15 | 11 | 32.1 ± 6.7 | 30.0 ± 5.9 | NA | IC | 0.33 (−0.46, 1.10) | 2.06 |
| Vairo et al66 (2008) | Single | 14 | 14 | 31.7 ± 8.8 | 27.7 ± 9.6 | NA | Peak | 0.43 (−0.32, 1.20) | 2.96 |
| Webster et al67 (2012) | Single | 15 | 11 | 52.0 ± 12.1 | 49.3 ± 12.4 | NA | Peak | 0.22 (−0.56, 1.00) | 1.39 |
| Nyland et al58 (2010), males | Single | 35 | 35 | 56.8 ± 7.2 | 57.5 ± 7.2 | NA | Peak | −0.10 (−0.57, 0.41) | −1.70 |
| Nyland et al58 (2010), females | Single | 35 | 35 | 50.8 ± 7.2 | 52.4 ± 7.5 | NA | Peak | −0.22 (−0.69, 0.34) | −3.79 |
| Orishimo et al61 (2010) | Single | 13 | 13 | 35.7 ± 8.2 | 43.4 ± 12.3 | NA | JE | −0.74 (−1.53, 0.11) | −4.50 |
| Nyland et al59 (2013), highly active | Single | 20 | 20 | 56.3 ± 11.6 | 54.0 ± 9.4 | NA | JE | 0.22 (−0.41, 0.83) | 2.17 |
| Nyland et al59 (2013), moderately active | Single | 24 | 24 | 53.7 ± 10.3 | 56.5 ± 11.0 | NA | JE | −0.26 (−0.83, 0.37) | −3.13 |
| Nyland et al59 (2013), sometimes active | Single | 26 | 26 | 51.4 ± 12.7 | 54.1 ± 11.2 | NA | JE | −0.23 (−0.77, 0.31) | −2.91 |
| Combined pooled effect size (95% CI) | −0.04 (−0.23, 0.15) | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; double, double-limb landing; IC, initial contact; JE, joint excursion; NA, not applicable; single, single-limb landing.
A total of 5 data points from 5 studies were analyzed for hip-adduction angles (Table 1B). A homogeneous effect (2/2) occurred for increased frontal-plane hip-excursion and peak hip adduction in the ACLR limb during double-limb landing when compared with healthy controls (Cohen d range = 0.71 to 1.15; Table 1B), demonstrating a strong combined effect (Cohen d = 0.91; 95% CI = 0.37, 1.45). During single-limb landing, the effects were heterogeneous for all hip-adduction variables (Cohen d range = −0.67 to 0.31; Table 1B).
Table 1B. .
Between-Groups Comparisons and Cohen d Effect Sizes of Frontal-Plane Hip-Joint Angles
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Hip-Adduction Angle |
ACL Contralateral-Limb Hip-Adduction Angle |
Healthy Hip-Adduction Angle |
|||||||
| Goerger et al55 (2014) | Double-limb landing | 12 | 20 | 0.02 ± 9.6 | NA | −6.8 ± 9.5 | Initial contact | 0.71 (−0.03, 1.45) | 5.05 |
| Delahunt et al51 (2012) | Double-limb landing | 13 | 16 | 5.2 ± 5.0 | NA | −0.4 ± 4.8 | Joint excursion | 1.15 (0.36, 1.93) | 7.12 |
| Combined pooled effect size (95% CI) | 0.91 (0.37, 1.45) | ||||||||
| Ortiz et al60 (2008) | Single | 14 | 15 | 4.1 ± 4.4 | NA | 4.3 ± 5.0 | Peak | −0.05 (−0.78, 0.68) | −0.36 |
| Webster et al67 (2012) | Single | 15 | 11 | 10.3 ± 3.9 | NA | 11.5 ± 3.8 | Peak | 0.31 (−0.48, 1.09) | 1.92 |
| Delahunt et al52 (2012) | Single | 14 | 14 | 5.0 ± 6.0 | NA | 9.0 ± 5.8 | Joint excursion | −0.67 (−1.43, 0.08) | −4.59 |
| Combined pooled effect size (95% CI) | −0.14 (−0.69, 0.40) | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; NA, not applicable; single, single-limb landing.
A total of 5 data points from 3 studies were analyzed for hip internal-rotation angles. A homogeneous effect (5/5) was identified for increased transverse-plane hip excursion and peak hip internal rotation in the ACLR limb during both double-limb and single-limb landing when compared with the contralateral limb and healthy controls (Cohen d range = 0.11 to 0.96; Table 1C). However, 3 of 5 CIs crossed zero. Compared with healthy controls, a moderate combined effect indicated that ACLR participants landed with increased internal rotation at the hip during single-limb landing tasks (Cohen d = 0.56; 95% CI = 0.12, 1.00; Table 1C).
Table 1C. .
Between-Groups Comparisons and Cohen d Effect Sizes of Transverse-Plane Hip-Joint Angles
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Hip Internal-Rotation Angle |
ACL Contralateral-Limb Hip Internal-Rotation Angle |
Healthy Hip Internal-Rotation Angle |
|||||||
| Delahunt et al51 (2012) | Double-limb landing | 13 | 16 | 0.5 ± 7.7 | NA | −5.8 ± 5.5 | Joint excursion | 0.96 (0.19, 1.73) | 3.90 |
| Combined pooled effect size (95% CI) | NA | ||||||||
| Ortiz et al60 (2008) | Single | 14 | 15 | 5.0 ± 5.0 | NA | 1.8 ± 2.1 | Peak | 0.82 (0.06, 1.57) | 3.39 |
| Webster et al67 (2012) | Single | 15 | 11 | 9.1 ± 10.6 | NA | 7.9 ± 10.4 | Peak | 0.11 (−0.67, 0.89) | 0.45 |
| Delahunt et al51 (2012) | Single | 13 | 16 | 3.2 ± 8.1 | NA | −1.1 ± 4.2 | Joint excursion | 0.75 (−0.01, 1.51) | 3.12 |
| Combined pooled effect size (95% CI) | 0.56 (0.12, 1.00) | ||||||||
| Webster et al67 (2012) | Single | 15 | 11 | 9.1 ± 10.6 | 2.0 ± 8.8 | NA | Joint excursion | 0.71 (−0.09, 1.50) | 4.27 |
| Combined pooled effect size (95% CI) | NA | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; NA, not applicable; single, single-limb landing.
Knee Kinematics
A total of 23 data points from 12 studies were analyzed for knee-flexion angles (Table 2A). Heterogeneous effects were demonstrated for peak knee-flexion angle, sagittal-plane knee-joint excursion, and knee-flexion angle at IC for both double- and single-limb landing tasks (Cohen d range = −1.16 to 1.72; Table 2A). All combined effects for knee-flexion angle yielded weak results with inconclusive CIs.
Table 2A. .
Between-Groups Comparisons and Cohen d Effect Sizes of Sagittal-Plane Knee-Joint Angles
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Knee-Flexion Angle |
ACL Contralateral-Limb Knee-Flexion Angle |
Healthy Knee-Flexion Angle |
|||||||
| Decker et al50 (2002) | Double | 11 | 11 | 26.3 ± 7.7 | NA | 29.9 ± 5.9 | IC | −0.52 (−1.36, 0.33) | −2.57 |
| Delahunt et al51 (2012) | Double | 13 | 16 | 62.0 ± 10.1 | NA | 69.5 ± 6.7 | JE | −0.89 (−1.66, −0.13) | −5.87 |
| Decker et al50 (2002) | Double | 11 | 11 | 47.7 ± 5.5 | NA | 46.5 ± 4.0 | JE | 0.23 (−0.61, 1.07) | 1.27 |
| Combined pooled effect size (95% CI) | −0.40 (−1.06, 0.24) | ||||||||
| Rudroff46 (2003) | Double | 30 | 30 | 20.8 ± 2.1 | 17.3 ± 1.9 | NA | Peak | 1.72 (1.13, 2.30) | 6.83 |
| Combined pooled effect size (95% CI) | NA | ||||||||
| Vairo et al66 (2008) | Single | 14 | 14 | 24.6 ± 12.9 | NA | 18.8 ± 7.7 | IC | 0.55 (−0.21, 1.30) | 1.77 |
| Webster et al67 (2012) | Single | 15 | 11 | 13.9 ± 4.9 | NA | 13.4 ± 4.9 | IC | 0.10 (−0.68, 0.88) | 0.32 |
| Miranda et al56 (2013) | Single | 10 | 10 | 18.9 ± 3.6 | NA | 21.9 ± 3.2 | IC | −0.85 (−1.76, 0.07) | −2.25 |
| Ortiz et al60 (2008) | Single | 14 | 15 | 57.7 ± 8.8 | NA | 57.8 ± 5.6 | Peak | −0.02 (−0.74, 0.71) | −0.05 |
| Tsai et al64 (2012) | Single | 10 | 10 | 67.6 ± 8.8 | NA | 79.1 ± 10.9 | Peak | −1.16 (−2.11, −0.21) | −2.96 |
| Vairo et al66 (2008) | Single | 14 | 14 | 37.0 ± 9.7 | NA | 27.8 ± 7.5 | Peak | 1.06 (0.27, 1.85) | 3.27 |
| Webster et al67 (2012) | Single | 15 | 11 | 58.3 ± 8.1 | NA | 63.1 ± 8.1 | Peak | −0.59 (−1.39, 0.20) | −1.82 |
| Miranda et al56 (2013) | Single | 10 | 10 | 36.6 ± 3.0 | NA | 37.1 ± 2.7 | Peak | −0.14 (−1.02, 0.74) | −0.39 |
| Delahunt et al52 (2012) | Single | 14 | 14 | 42.6 ± 9.2 | NA | 51.4 ± 7.6 | JE | −1.04 (−1.82, −0.26) | −3.27 |
| Combined pooled effect size (95% CI) | −0.21 (−0.69, 0.27) | ||||||||
| Vairo et al66 (2008) | Single | 14 | 14 | 24.6 ± 12.9 | 22.4 ± 6.2 | NA | IC | 0.22 (−0.53, 1.00) | 0.42 |
| Webster et al67 (2012) | Single | 15 | 11 | 13.9 ± 4.9 | 14.5 ± 5.9 | NA | IC | −0.11 (−0.89, 0.70) | −0.21 |
| Vairo et al66 (2008) | Single | 14 | 14 | 37.0 ± 9.7 | 33.0 ± 6.3 | NA | Peak | 0.49 (−0.27, 1.21) | 0.93 |
| Webster et al67 (2012) | Single | 15 | 11 | 58.3 ± 8.1 | 57.9 ± 8.8 | NA | Peak | 0.05 (−0.73, 0.80) | 0.09 |
| Nyland et al58 (2010), males | Single | 35 | 35 | 56.7 ± 11.2 | 56.9 ± 10.9 | NA | Peak | −0.02 (−0.49, 0.53) | −0.04 |
| Nyland et al58 (2010), females | Single | 35 | 35 | 50.3 ± 7.6 | 51.0 ± 7.6 | NA | Peak | −0.09 (−0.56, 0.40) | −0.21 |
| Orishimo et al61 (2010) | Single | 13 | 13 | 10.5 ± 5.0 | 12.3 ± 4.9 | NA | JE | −0.36 (−1.14, 0.42) | −0.68 |
| Nyland et al59 (2013), highly active | Single | 20 | 20 | 56.1 ± 12.1 | 52.4 ± 11.8 | NA | JE | 0.31 (−0.31, 0.90) | 0.65 |
| Nyland et al59 (2013), moderately active | Single | 24 | 24 | 57.0 ± 19.6 | 57.9 ± 16.8 | NA | JE | −0.05 (−0.62, 0.57) | −0.11 |
| Nyland et al59 (2013), sometimes active | Single | 26 | 26 | 49.0 ± 11.9 | 51.5 ± 12.1 | NA | JE | −0.21 (−0.75, 0.30) | −0.46 |
| Combined pooled effect size (95% CI) | −0.0006 (−0.19, 0.19) | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; double, double-limb landing; IC, initial contact; JE, joint excursion; NA, not applicable; single, single-limb landing.
A total of 7 data points from 5 studies were analyzed for knee-adduction angles (Table 2B). A homogeneous effect (3/3) was noted for decreased peak knee-adduction angle and frontal-plane knee-joint excursion in the ACLR limb during double-limb landing when compared with healthy controls (Cohen d range = −1.05 to −0.61; Table 2B), resulting in a moderate combined effect with CIs that did not cross zero (Cohen d = −0.73; 95% CI = −1.12, −0.34; Table 2B). However, during single-limb landing, the effects were heterogeneous for peak knee adduction (Cohen d range = −0.76 to 0.49; Table 2B), yielding a weak and inconclusive combined effect size (Cohen d = −0.15; 95% CI = −0.88, 0.56).
Table 2B. .
Between-Groups Comparisons and Cohen d Effect Sizes of Frontal-Plane Knee-Joint Angles
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Knee-Adduction Angle |
ACL Contralateral-Limb Knee-Adduction Angle |
Healthy Knee-Adduction Angle |
|||||||
| Goerger et al55 (2014) | Double | 20 | 20 | −4.2 ± 5.7 | NA | −0.4 ± 5.7 | Peak | −0.65 (−1.28, −0.01) | −6.66 |
| Delahunt et al51 (2012) | Double | 13 | 16 | 3.0 ± 4.5 | NA | 8.9 ± 6.4 | JE | −1.05 (−1.83, −0.27) | −6.16 |
| Goerger et al55 (2014) | Double | 20 | 20 | −11.7 ± 7.7 | NA | −6.9 ± 7.7 | JE | −0.61 (−1.24, 0.02) | −5.84 |
| Combined pooled effect size (95% CI) | −0.73 (−1.12, −0.34) | ||||||||
| Ortiz et al60 (2008) | Single | 14 | 15 | −7.2 ± 5.8 | NA | −9.8 ± 5.3 | Peak | 0.49 (−0.25, 1.23) | 3.46 |
| Webster et al67 (2012) | Single | 15 | 11 | −3.9 ± 3.7 | NA | −3.1 ± 3.2 | Peak | −0.23 (−1.01, 0.55) | −1.43 |
| Delahunt et al52 (2012) | Single | 14 | 14 | −3.6 ± 3.9 | NA | −1.1 ± 2.7 | JE | −0.76 (−1.52, 0.00) | −5.09 |
| Combined pooled effect size (95% CI) | −0.15 (−0.88, 0.56) | ||||||||
| Webster et al67 (2012) | Single | 15 | 11 | −3.9 ± 3.7 | −3.1 ± 6.1 | NA | Peak | −0.16 (−0.94, 0.60) | −0.55 |
| Combined pooled effect size (95% CI) | NA | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; double, double-limb landing; JE, joint excursion; NA, not applicable; single, single-limb landing.
A total of 9 data points from 8 studies were analyzed for knee internal-rotation angles. We found a homogeneous effect (2/2) for increased transverse-plane knee-joint excursion in the ACLR limb when compared with healthy controls during double-limb landing; however, CIs for both crossed zero (Cohen d range = −0.47 to −0.21; Table 2C). Effects were heterogeneous when compared with the contralateral limb during double-limb landing (Cohen d range = −0.46 to 2.05; Table 2C). During single-limb landing, heterogeneous effects were present for knee internal rotation for both comparison limbs (Cohen d range = −1.94 to 0.02; Table 2C). All combined effects for knee internal-rotation angle yielded weak results with inconclusive CIs.
Table 2C. .
Between-Groups Comparisons and Cohen d Effect Sizes of Transverse-Plane Knee-Joint Angles
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Knee Internal-Rotation Angle |
ACL Contralateral-Limb Knee Internal-Rotation Angle |
Healthy Knee Internal-Rotation Angle |
|||||||
| Delahunt et al52 (2012) | Double | 14 | 14 | 13.6 ± 0.50 | NA | 15.2 ± 7.0 | JE | −0.21 (−0.94, 0.53) | −0.77 |
| Goerger et al55 (2014) | Double | 20 | 20 | 13.2 ± 8.2 | NA | 17.1 ± 8.2 | JE | −0.47 (−1.10, 0.16) | −1.30 |
| Combined pooled effect size (95% CI) | −0.39 (−0.87, 0.07) | ||||||||
| Sato et al63 (2013) | Double | 10 | 10 | 10.3 ± 4.9 | 12.4 ± 4.3 | NA | Peak | −0.46 (−1.34, 0.40) | −2.22 |
| Goitis et al68 (2013) | Double | 20 | 20 | 20.3 ± 2.8 | 15.2 ± 2.1 | NA | JE | 2.05 (1.29, 2.81) | 13.63 |
| Lam et al42 (2011) | Double | 10 | 10 | 8.9 ± 3.0 | 8.2 ± 2.6 | NA | JE | 0.25 (−0.63, 1.10) | 1.24 |
| Combined pooled effect size (95% CI) | 0.62 (−0.88, 2.14) | ||||||||
| Ortiz et al60 (2008) | Single | 14 | 15 | −10.5 ± 10.7 | NA | 5.6 ± 5.1 | Peak | −1.94 (−2.83, −1.06) | −1.07 |
| Webster et al67 (2012) | Single | 15 | 11 | 21.1 ± 17.8 | NA | 24.3 ± 20.5 | Peak | −0.17 (−0.95, 0.61) | −0.10 |
| Delahunt et al51 (2012) | Single | 13 | 16 | 12.13 ± 6.0 | NA | 12.0 ± 6.6 | JE | 0.02 (−0.71, 0.75) | 0.01 |
| Combined pooled effect size (95% CI) | −0.67 (−1.84, 0.48) | ||||||||
| Webster et al67 (2012) | Single | 15 | 11 | 21.1 ± 17.8 | 22.7 ± 18.8 | NA | Peak | −0.09 (−0.87, 0.70) | −0.08 |
| Combined pooled effect size (95% CI) | NA | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; double, double-limb landing; JE, joint excursion; NA, not applicable; single, single-limb landing.
Hip Kinetics
A total of 7 data points from 5 studies were analyzed for internal hip-extension moments (Table 3A). There was a homogeneous effect (2/2) for reduced internal hip-extension moments in the ACLR limb when compared with healthy controls during double-limb landing, and neither CI crossed 0 (Cohen d range = −1.57 to −1.00; Table 3A). The combined effect for internal hip-extension moment during double-limb landing was strong with conclusive CIs (Cohen d = −1.19; 95% CI = −1.73, −0.64). During single-limb landing, heterogeneous effects were present for internal hip-extension moments when compared with both contralateral limbs and healthy controls (Cohen d range = −0.52 to 1.41; Table 3A); both combined effects were considered small with CIs that crossed zero.
Table 3A. .
Between-Groups Comparisons and Cohen d Effect Sizes of Sagittal-Plane Hip-Joint Moments
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Internal Hip-Extension Moment |
ACL Contralateral-Limb Internal Hip-Extension Moment |
Healthy Internal Hip-Extension Moment |
|||||||
| Decker et al50 (2002) | Double-limb landing | 11 | 11 | 25.38 ± 10.48 | NA | 44.33 ± 13.44 | Peak | −1.57 (−2.53, −0.62) | −1.39 |
| Goerger et al55 (2014) | Double-limb landing | 12 | 39 | 0.13 ± 0.06 | NA | 0.20 ± 0.06 | Peak | −1.00 (−1.67, −0.32) | −0.98 |
| Combined pooled effect size (95% CI) | −1.19 (−1.73, −0.64) | ||||||||
| Vairo et al66 (2008) | Single | 14 | 14 | 0.24 ± 0.06 | NA | 0.28 ± 0.09 | Peak | −0.52 (−1.28, 0.23) | −3.55 |
| Webster et al67 (2012) | Single | 14 | 11 | 1.90 ± 0.49 | NA | 1.08 ± 0.68 | Peak | 1.41 (0.53, 2.29) | 7.08 |
| Combined pooled effect size (95% CI) | 0.43 (−1.46, 2.32) | ||||||||
| Vairo et al66 (2008) | Single | 14 | 14 | 0.24 ± 0.06 | 0.27 ± 0.07 | NA | Peak | −0.46 (−1.21, 0.29) | −0.25 |
| Orishimo et al61 (2010) | Single | 13 | 13 | 5.50 ± 3.80 | 5.30 ± 2.10 | NA | Peak | 0.07 (−0.70, 0.83) | 0.04 |
| Webster et al67 (2012) | Single | 14 | 14 | 1.90 ± 0.49 | 1.98 ± 0.81 | NA | Peak | −0.12 (−0.86, 0.62) | −0.06 |
| Combined pooled effect size (95% CI) | 0.17 (−0.60, 0.25) | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; NA, not applicable; single, single-limb landing.
Knee Kinetics
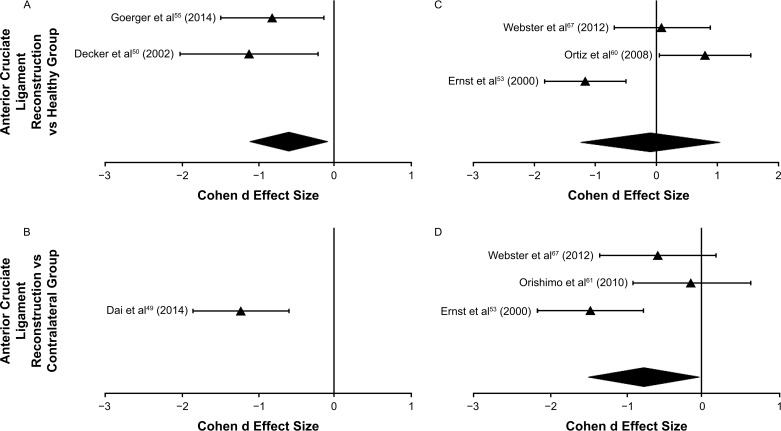
A total of 9 data points from 7 studies were analyzed for internal knee-extension moments (Table 3B, Figure 2). A homogeneous effect (3/3) was observed for reduced internal knee-extension moments in the ACLR limb when compared with contralateral limbs and healthy controls during double-limb landing, with no CIs crossing zero (Cohen d range = −1.23 to −0.81; combined Cohen d = −0.92; 95% CI = −1.45, −0.38; Table 3B, Figure 2). During single-limb landing, effects were heterogeneous when compared with healthy controls (Cohen d range = −1.16 to 0.80; combined Cohen d = −0.10; 95% CI = −1.27, 1.07; Table 3B, Figure 2) but homogeneous (3/3) for reductions in internal knee-extension moments when compared with the contralateral limb (Cohen d range = −1.46 to −0.14; combined Cohen d = −0.74; 95% CI = −1.51, −0.03; Table 3B, Figure 2).
Table 3B. .
Between-Groups Comparisons and Cohen d Effect Sizes of Sagittal-Plane Knee-Joint Moments
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Internal Knee-Extension Moment |
ACL Contralateral-Limb Internal Knee-Extension Moment |
Healthy Internal Knee-Extension Moment |
|||||||
| Goerger et al55 (2014) | Double | 12 | 39 | 0.16 ± 0.04 | NA | 0.20 ± 0.04 | Peak | −0.81 (−1.48, −0.14) | −7.03 |
| Decker et al50 (2002) | Double | 11 | 11 | 12.77 ± 3.21 | NA | 17.47 ± 4.97 | Peak | −1.12 (−2.02, −0.22) | −5.39 |
| Combined pooled effect size (95% CI) | −0.92 (−1.45, −0.38) | ||||||||
| Dai et al49 (2014) | Double | 23 | 23 | 0.10 ± 0.03 | 0.14 ± 0.03 | NA | Peak | −1.23 (−1.86, −0.60) | −11.93 |
| Combined Pooled effect size and 95% CI | NA | ||||||||
| Webster et al67 (2012) | Single | 14 | 11 | 1.09 ± 0.34 | NA | 1.06 ± 0.32 | Peak | 0.09 (−0.70, 0.88) | 0.56 |
| Ortiz et al60 (2008) | Single | 14 | 15 | 3.50 ± 0.69 | NA | 3.00 ± 0.55 | Peak | 0.80 (0.05, 1.56) | 5.41 |
| Ernst et al53 (2000) | Single | 20 | 20 | 1.30 ± 0.59 | NA | 1.91 ± 0.45 | Peak | −1.16 (−1.83, −0.49) | −10.00 |
| Combined pooled effect size (95% CI) | −0.10 (−1.27, 1.07) | ||||||||
| Webster et al67 (2012) | Single | 14 | 14 | 1.09 ± 0.34 | 1.30 ± 0.38 | NA | Peak | −0.58 (−1.34, 0.17) | −0.54 |
| Orishimo et al61 (2010) | Single | 13 | 13 | 3.30 ± 1.70 | 3.50 ± 1.10 | NA | Peak | −0.14 (−0.91, 0.63) | −0.13 |
| Ernst et al53 (2000) | Single | 20 | 20 | 1.30 ± 0.59 | 2.09 ± 0.49 | NA | Peak | −1.46 (−2.15, −0.76) | −1.37 |
| Combined pooled effect size (95% CI) | −0.74 (−1.51, −0.03) | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; double, double-limb landing; NA, not applicable; single, single-limb landing.
Figure 2. .
A between-groups comparison of sagittal-plane knee-joint moments during, A and B, double-limb and, C and D, single-limb landing tasks. Effect sizes and associated 95% confidence intervals based on peak (triangle) values are presented in the accompanying forest plot. The large, solid black diamond at the bottom of the graph represents the pooled effect size for all included data points.
A total of 3 data points from 2 studies were analyzed for internal knee-abduction moments, during single-limb landing only (Table 3C). Effects were homogeneous when compared with both the contralateral and healthy control limbs. Effect sizes showed that internal knee-abduction moments were increased in the ACLR limb compared with the healthy controls (Cohen d range = 0.83 to 0.94; combined Cohen d = 0.88; 95% CI = 0.32, 1.44); however, they were decreased compared with the contralateral limb (Cohen d = −0.51).
Table 3C. .
Between-Groups Comparisons and Cohen d Effect Sizes of Frontal-Plane Knee-Joint Moments
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Internal Knee-Abduction Moment |
ACL Contralateral-Limb Internal Knee-Abduction Moment |
Healthy Internal Knee-Abduction Moment |
|||||||
| Webster et al67 (2012) | Single | 14 | 11 | 0.85 ± 0.40 | NA | 0.52 ± 0.40 | Peak | 0.83 (0.00, 1.65) | 1.65 |
| Ortiz et al60 (2008) | Single | 14 | 15 | 0.20 ± 0.20 | NA | 0.07 ± 0.01 | Peak | 0.94 (0.17, 1.70) | 1.96 |
| Combined pooled effect size (95% CI) | 0.88 (0.32, 1.44) | ||||||||
| Webster et al67 (2012) | Single | 14 | 14 | 0.85 ± 0.40 | 1.03 ± 0.30 | NA | Peak | −0.51 (−1.26, 0.24) | −3.46 |
| Combined pooled effect size (95% CI) | NA | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; NA, not applicable; single, single-limb landing.
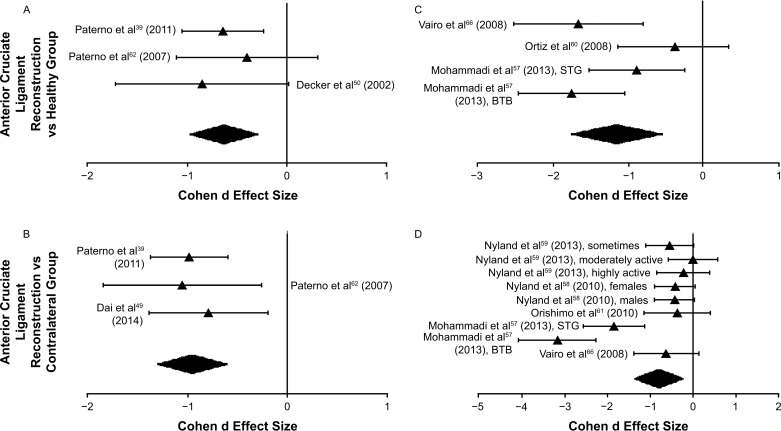
Peak vGRF
A total of 19 data points from 10 studies were analyzed for peak vGRF (Table 4, Figure 3). There was a homogeneous effect (19/19) for reduced peak vGRF in the ACLR limb during both double and single limb landing when compared with contralateral and healthy control limbs (Cohen d range = −3.16 to 0.00). Comparisons demonstrated effect sizes with CIs that did not cross 0 when the ACLR limb was compared with the contralateral limb during double-limb landing (Table 4, Figure 3). All combined effect sizes demonstrated moderate to strong effects with CIs that did not cross 0 (Figure 3A: combined Cohen d = −0.62; 95% CI = −0.94, −0.29; Figure 3B: combined Cohen d = −0.94; 95% CI = −1.24, −0.63; Figure 3C: combined Cohen d = −1.15; 95% CI = −1.77, −0.53; Figure 3D: combined Cohen d = −0.79; 95% CI = −1.31, −0.28).
Table 4. .
Between-Groups Comparisons and Cohen d Effect Sizes of Peak Vertical Ground Reaction Forces
| Study |
Task |
ACL Reconstruction Sample Size |
Comparison Group Sample Size |
Mean ± SD |
Landing Phase |
Cohen d Effect Size (95% CI) |
Weighted Effect Size |
||
| ACL Reconstruction-Limb Vertical Ground Reaction Force |
ACL Contralateral-Limb Vertical Ground Reaction Force |
Healthy Vertical Ground Reaction Force |
|||||||
| Paterno et al39 (2011) | Double | 56 | 42 | 1.77 ± 0.35 | NA | 2.01 ± 0.40 | Peak | −0.64 (−1.05, −0.23) | −14.74 |
| Paterno et al62 (2007) | Double | 14 | 18 | 1.50 ± 0.30 | NA | 1.60 ± 0.20 | Peak | −0.40 (−1.11, 0.30) | −3.11 |
| Decker et al50 (2002) | Double | 11 | 11 | 3.16 ± 1.03 | NA | 4.00 ± 0.95 | Peak | −0.85 (−1.72, 0.02) | −4.30 |
| Combined pooled effect size (95% CI) | −0.62 (−0.94, −0.29) | ||||||||
| Paterno et al39 (2011) | Double | 56 | 56 | 1.77 ± 0.35 | 2.16 ± 0.44 | NA | Peak | −0.98 (−1.37, −0.59) | −24.55 |
| Paterno et al62 (2007) | Double | 14 | 14 | 1.50 ± 0.30 | 2.00 ± 0.60 | NA | Peak | −1.05 (−1.84, −0.26) | −6.52 |
| Dai et al49 (2014) | Double | 23 | 23 | 1.61 ± 0.47 | 2.02 ± 0.56 | NA | Peak | −0.79 (−1.39, −0.19) | −8.44 |
| Combined pooled effect size (95% CI) | −0.94 (−1.24, −0.63) | ||||||||
| Vairo et al66 (2008) | Single | 14 | 14 | 3.72 ± 0.51 | NA | 5.11 ± 1.07 | Peak | −1.66 (−2.52, −0.80) | −8.77 |
| Ortiz et al60 (2008) | Single | 14 | 15 | 4.36 ± 0.76 | NA | 4.62 ± 0.55 | Peak | −0.39 (−1.13, 0.34) | −2.80 |
| Mohammadi et al57 (2013), semitendinosis-gracilis autograft | Single | 21 | 21 | 1.80 ± 0.50 | NA | 2.20 ± 0.40 | Peak | −0.88 (−1.52, −0.25) | −8.48 |
| Mohammadi et al57 (2013), bone-patellar tendon-bone autograft | Single | 21 | 21 | 1.50 ± 0.40 | NA | 2.20 ± 0.40 | Peak | −1.75 (−2.46, −1.04) | −13.43 |
| Combined pooled effect size (95% CI) | −1.15 (−1.77, −0.53) | ||||||||
| Nyland et al59 (2013), sometimes active | Single | 26 | 26 | 3.00 ± 0.50 | 3.30 ± 0.60 | NA | Peak | −0.54 (−1.10, 0.01) | −1.57 |
| Nyland et al59 (2013), moderately active | Single | 24 | 24 | 3.20 ± 0.50 | 3.20 ± 0.40 | NA | Peak | 0.00 (−0.57, 0.57) | 0.00 |
| Nyland et al59 (2013), highly active | Single | 20 | 20 | 3.40 ± 0.40 | 3.50 ± 0.50 | NA | Peak | −0.22 (−0.84, 0.40) | −0.60 |
| Nyland et al58 (2010), females | Single | 35 | 35 | 3.12 ± 0.33 | 3.26 ± 0.33 | NA | Peak | −0.42 (−0.90, 0.05) | −1.30 |
| Nyland et al58 (2010), males | Single | 35 | 35 | 3.27 ± 0.36 | 3.42 ± 0.36 | NA | Peak | −0.42 (−0.89, 0.06) | −1.28 |
| Orishimo et al61 (2010) | Single | 13 | 13 | 4.20 ± 1.50 | 4.70 ± 1.30 | NA | Peak | −0.36 (−1.13, 0.42) | −0.84 |
| Mohammadi et al57 (2013), semitendinosis-gracilis autograft | Single | 21 | 21 | 1.80 ± 0.50 | 2.50 ± 0.20 | NA | Peak | −1.84 (−2.56, −1.12) | −4.58 |
| Mohammadi et al57 (2013), bone-patellar tendon-bone autograft | Single | 21 | 21 | 1.50 ± 0.40 | 2.50 ± 0.20 | NA | Peak | −3.16 (−4.07, −2.25) | −6.63 |
| Vairo et al66 (2008) | Single | 14 | 14 | 3.72 ± 0.51 | 4.19 ± 0.94 | NA | Peak | −0.62 (−1.38, 0.14) | −1.49 |
| Combined pooled effect size (95% CI) | −0.79 (−1.31, −0.28) | ||||||||
Abbreviations: ACL, anterior cruciate ligament; CI, confidence interval; double, double-limb landing; NA, not applicable; single, single-limb landing.
Figure 3. .
A between-groups comparison of peak vertical ground reaction forces during, A and B, double-limb and, C and D, single-limb landing tasks. Effect sizes and associated 95% confidence intervals based on peak (triangle) values are presented in the accompanying forest plot. The large, solid black diamond at the bottom of the graph represents the pooled effect size for all included data points. Abbreviations: BTB, bone-patellar tendon-bone autograft; STG, semitendinosis-gracilis autograft.
DISCUSSION
In this review, we sought to systematically evaluate the kinematic and kinetic patterns of the hip and knee during dynamic landing assessments in patients with a history of ACLR. Our main findings were that (1) the involved limb of patients with ACLR demonstrated smaller knee-extension moments during double-legged landings compared with the healthy contralateral limb and healthy controls in 100% of the included studies (3/3; 1 low, 1 moderate, and 1 high quality; Table 3B, Figure 2) and (2) there was a homogeneous effect demonstrating decreased vGRF of the ACLR limb when compared with the contralateral limb (12/12 included data points) and healthy controls (7/7 included data points) regardless of task, with 47.4% (9/19) of the included data points demonstrating a large, conclusive effect size with CIs that did not cross zero (Table 4, Figure 3). Importantly, the methodologic quality of the studies that supplied conclusive effect sizes for vGRF were all of moderate39,62 or high57,66 quality. These findings are supported by the strong combined effect sizes with CIs not crossing 0. Both findings suggest an alteration in the loading of the involved limb, which may have significant implications for rehabilitation strategies as well as the subsequent risk of knee-joint injury.
Based on the available studies, it appears that patients with ACLR landed with lower peak knee-extension moments in their involved limb during a double-legged landing task (Table 3B). The reduction in knee-extension moments during double-limb landing is not supported in the ACL injury-prevention literature, as no current evidence suggests that asymmetries in knee-extension moment were present before the initial ACL injury. Therefore, these data likely mean that alterations leading to asymmetry in knee-extension moment occurred in response to the injury. A reduction in knee-joint loading was also observed during other activities in patients with ACLR, such as level-ground walking gait69,70 and stair ambulation,71,72 indicating that compensatory biomechanics persisted across tasks. The reduction in knee-extension moment during gait resulted from either insufficient quadriceps strength, which meant the muscle was unable to eccentrically distribute force properly,73,74 or from planned biomechanical adaptations due to pain or psychological favoring of the healthy limb.75 Interestingly, the data were inconclusive regarding the effect of ACLR on knee-extension moments during single-legged landing. It is possible that during double-legged landing and other tasks involving both limbs, patients with ACLR were able to effectively shift the load to the contralateral limb, thereby unloading the forces on the injured limb. However, this strategy would not be available to patients during single-limb tasks. The current evidence illustrates that reductions in knee-extension moment during double-limb tasks is likely attributable to physical and psychological factors associated with the injury, such as pain, fear avoidance, and quadriceps weakness. Further investigation is warranted to determine the influence of a reduction in knee-extension moment on secondary injury risk, such as ACL reinjury and posttraumatic osteoarthritis.
Previous researchers76,77 have identified kinematic strategies at the knee and hip during landing tasks that are present before injury and increase the risk for initial ACL injury; thus, it was plausible to expect these alterations would also be present in patients after ACLR. Surprisingly, we observed no conclusive effect for differences in any of the kinematic variables at the knee or hip during landing. The effect sizes associated with kinematic adaptations were mostly heterogeneous, demonstrating that the injured limbs of patients with ACLR may land with more (2/12 included studies),46,66 less (3/12 included studies),51,52,64 or no difference (7/12 included studies)50,56,58–61,67 in knee flexion compared with uninjured limbs and healthy controls (Table 2A). Peak knee-adduction angle and frontal-plane knee-joint excursion yielded the strongest evidence for kinematic alterations at the knee, with lower knee-adduction angles (3/3 included studies; Table 2B) in the involved limb compared with healthy controls during double-legged landing. Yet similar to the effects associated with knee-extension moment, this finding was only present during double-legged landing, and the data were inconclusive regarding the effect of ACLR on knee-adduction angle during single-legged landing. Authors of a previous study78 suggested that individuals use different energy-dissipation strategies during double- and single-legged landing tasks and indicated that frontal-plane biomechanics at the knee during single-legged landing may expose individuals to a greater risk of traumatic knee injuries, such as secondary ACL rupture. Future research would benefit from further evaluation of double- and single-legged landings.
At the hip, large effects associated with reductions in peak internal hip-extension moment (Table 3A) in the ACLR involved limb compared with healthy controls and similar to data regarding internal knee-extension moments and knee-adduction angles were only detected during double-legged landings. Of note, however, only 2 groups50,55 reported hip-extension moments. Multiple large or homogeneous (or both) effects were noted for increased peak hip adduction and frontal-plane hip-joint excursion (3/5 included studies)51,55,67 and increased transverse-plane hip-joint excursion compared with contralateral healthy limbs (1/1 included studies)67 and healthy matched controls (4/4 included studies), with varying levels of methodologic quality among the included studies (Table 1B and C).51,52,60,67 Our findings are clinically concerning given that excessive adduction14 and internal rotation of the hip14–16 have been shown to increase the risk of primary and secondary ACL injury during a double-limb landing. However, the data included in this review were ultimately heterogeneous for alterations in hip kinematics or kinetics.
Because reduced flexion,7–9 excessive abduction,4,10 and excessive internal rotation11–13 at the knee have previously been identified as risk factors for initial ACL injury risk, we expected to observe some, if not all, of these alterations in the involved limbs of patients with ACLR. After reviewing the included articles further, some evidence suggests that sex may have had an effect on the observed results in knee kinematics. Only 2 groups56,58 stratified their data by sex, and both concluded that males used knee-flexion strategies more consistent with healthy individuals, whereas females experienced reduced peak knee-flexion range of motion and reduced sagittal-plane knee-joint excursions during landing. Reductions in knee-flexion angle, as well as other alterations at the knee, such as increased abduction, were also predictive of initial ACL injury risk and were more prevalent in females than in males before ACL injury.4,9,79 Males and females demonstrated differences in landing mechanics before ACL injury, and females also showed an increased risk of initial noncontact ACL injury,80 so it is possible we might have observed differences in knee kinematics in this review if the data could have been separated by sex. Unfortunately, this comparison was not possible based on the available data. Further, only 1 set of investigators57 stratified data based on graft type and concluded that patients with bone-patellar tendon-bone autografts demonstrated lower peak vGRF than those with semitendinosis-gracilis autografts, potentially due to greater impairments in quadriceps function. Future researchers should compare both sex and graft type to understand biomechanical alterations during landing tasks after ACLR and to identify separate secondary injury risk factors.
Anterior cruciate ligament injury-prevention programs have been established based on modifiable biomechanical risk factors noted during landing assessments in the laboratory. Our intention was to review the current literature and identify conclusive biomechanical alterations in patients with ACLR with the goal of offering clinicians and researchers valuable information to better understand reinjury risk and prevention strategies in these patients. Unfortunately, based on this review, it is clear that the existing data were insufficient to establish any consistent biomechanical alterations in patients with ACLR. It remains plausible that the same risk factors for initial ACL injury risk may also help to identify those who will experience a second ACL rupture. However, patients with ACLR may exhibit a unique set of risk factors associated with the injury and surgical process that expose them to secondary ACL injury. Or landing biomechanics may not fully explain the secondary ACL injury risk and other factors such as muscle strength, symptoms, and psychological function may better account for differences in ACLR patients and their risk for secondary ACL injury. Future authors should focus on prospective investigations to address biomechanical alterations, neuromuscular deficits, and psychological function to determine the combination of risk factors that contribute to secondary ACL injury and should also stratify by sex and graft type.
Clinical Implications
The risk of secondary ACL rupture remains higher than that of the initial ACL injury,27 likely due to either poor movement strategies that were present before injury or lingering impairments that were not addressed by surgical reconstruction and therapeutic rehabilitation. Fortunately, movement strategies are modifiable and represent an important target for successful clinical intervention. Di Stasi et al81 thoroughly assessed the ability of neuromuscular-training interventions to target deficits associated with secondary ACL injury risk. They provided evidence for specific exercises, including lunge and tuck-jump progressions, knee and trunk stability programs, and multidirectional exercises, to improve the abnormal biomechanics we identified. Based on our findings, clinicians should consider exercise and assessment progressions that focus on gradual restoration of involved-limb vGRFs and symmetry in knee-extension moments. Further evidence suggests that feedback-augmented exercises, with the use of audio, visual, or other forms of external information (eg, feedback from a force plate with the intent of influencing peak vGRFs), may be beneficial for reversing the specific impairments identified in this investigation, such as decreased knee-extension moments and vGRFs.82–84 Based on these findings, interventions must be tailored to the specific deficits of the individual patient after ACLR; however, using these guidelines as an evidence-based starting point may help clinicians to focus their efforts more effectively.
Limitations
From a methodologic perspective, 1 limitation is that the articles needed to be written in English to be included. Also, despite numerous attempts, we had to exclude 8 additional studies (8/35 = 22% originally pulled for review) because the authors failed to report means and SDs and did not reply to data requests. The lack of knowledge related to preinjury biomechanics in individuals included in this review may limit the ability to clearly describe the effect of ACLR versus the underlying biomechanical patterns that may have put these individuals at risk for primary ACL injury. In addition, the lack of information about sex-specific alterations in landing patterns after ACLR may have limited both the effect sizes and the homogeneity of findings presented in this review. Much of the work focused on initial ACL injury prevention has been directed toward female athletes, with little evidence regarding male athletes. The failure of the included studies to compare male and female participants represents a significant limitation in the ACLR literature, which should be addressed in future studies. Similarly, we were unable to provide recommendations on the effect that graft type has on landing strategies, which should also be considered a limitation in the postreconstruction literature and a focus moving forward. Lastly, published data are lacking on transverse-plane kinematics in patients with ACLR, which creates an area for future investigation.
CONCLUSIONS
Unique compensatory movement profiles after ACLR include reduced knee-extension moments and decreased vGRF in the injured limb, which have not been identified as risk factors for initial ACL injury. These compensations were present in the ACLR limb despite surgical intervention and therapeutic rehabilitation, suggesting that the current standard of care does not address these deficiencies. Aberrant hip kinematics associated with initial ACL injury may contribute to abnormal movement profiles after ACLR; however, no clinically meaningful differences were observed. Future researchers should focus on prospective investigations to identify biomechanical risk factors in patients with ACLR, including stratification by sex and graft type.
Supplementary Material
SUPPLEMENTAL MATERIAL
Supplemental Table. Description of study characteristics and methodological quality
Found at DOI: http://dx.doi.org/10.4085/1062-6050-334-16.S1
REFERENCES
- 1. Myklebust G, Maehlum S, Engebretsen L, Strand T, Solheim E. . Registration of cruciate ligament injuries in Norwegian top level team handball. A prospective study covering two seasons. Scand J Med Sci Sports. 1997; 7 5: 289– 292. [DOI] [PubMed] [Google Scholar]
- 2. Myklebust G, Maehlum S, Holm I, Bahr R. . A prospective cohort study of anterior cruciate ligament injuries in elite Norwegian team handball. Scand J Med Sci Sports. 1998; 8 3: 149– 153. [DOI] [PubMed] [Google Scholar]
- 3. Griffin LY, Albohm MJ, Arendt EA, et al. Understanding and preventing noncontact anterior cruciate ligament injuries: a review of the Hunt Valley II meeting, January 2005. Am J Sports Med. 2006; 34 9: 1512– 1532. [DOI] [PubMed] [Google Scholar]
- 4. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005; 33 4: 492– 501. [DOI] [PubMed] [Google Scholar]
- 5. Boden BP, Dean GS, Feagin JA Jr, Garrett WE Jr.. Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000; 23 6: 573– 578. [DOI] [PubMed] [Google Scholar]
- 6. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007; 35 3: 359– 367. [DOI] [PubMed] [Google Scholar]
- 7. Hewett TE, Myer GD, Ford KR. . Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. Am J Sports Med. 2006; 34 2: 299– 311. [DOI] [PubMed] [Google Scholar]
- 8. Yu B, Garrett WE. . Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007; 41 suppl 1: i47– i51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Decker MJ, Torry MR, Wyland DJ, Sterett WI, Richard Steadman J. . Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech (Bristol, Avon). 2003; 18 7: 662– 669. [DOI] [PubMed] [Google Scholar]
- 10. Colby S, Francisco A, Yu B, Kirkendall D, Finch M, Garrett W Jr.. Electromyographic and kinematic analysis of cutting maneuvers. Implications for anterior cruciate ligament injury. Am J Sports Med. 2000; 28 2: 234– 240. [DOI] [PubMed] [Google Scholar]
- 11. Beaulieu ML, Oh YK, Bedi A, Ashton-Miller JA, Wojtys EM. . Does limited internal femoral rotation increase peak anterior cruciate ligament strain during a simulated pivot landing? Am J Sports Med. 2014; 42 12: 2955– 2963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, Slauterbeck JL. . Combined knee loading states that generate high anterior cruciate ligament forces. J Orthop Res. 1995; 13 6: 930– 935. [DOI] [PubMed] [Google Scholar]
- 13. Shin CS, Chaudhari AM, Andriacchi TP. . Valgus plus internal rotation moments increase anterior cruciate ligament strain more than either alone. Med Sci Sports Exerc. 2011; 43 8: 1484– 1491. [DOI] [PubMed] [Google Scholar]
- 14. Powers CM. . The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010; 40 2: 42– 51. [DOI] [PubMed] [Google Scholar]
- 15. Fox AS, Bonacci J, McLean SG, Spittle M, Saunders N. . What is normal? Female lower limb kinematic profiles during athletic tasks used to examine anterior cruciate ligament injury risk: a systematic review. Sports Med. 2014; 44 6: 815– 832. [DOI] [PubMed] [Google Scholar]
- 16. McLean SG, Huang X, van den Bogert AJ. . Association between lower extremity posture at contact and peak knee valgus moment during sidestepping: implications for ACL injury. Clin Biomech (Bristol, Avon). 2005; 20 8: 863– 870. [DOI] [PubMed] [Google Scholar]
- 17. Myer GD, Ford KR, Di Stasi SL, Foss KD, Micheli LJ, Hewett TE. . High knee abduction moments are common risk factors for patellofemoral pain (PFP) and anterior cruciate ligament (ACL) injury in girls: is PFP itself a predictor for subsequent ACL injury? Br J Sports Med. 2015; 49 2: 118– 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Frank B, Bell DR, Norcross MF, Blackburn JT, Goerger BM, Padua DA. . Trunk and hip biomechanics influence anterior cruciate loading mechanisms in physically active participants. Am J Sports Med. 2013; 41 11: 2676– 2683. [DOI] [PubMed] [Google Scholar]
- 19. Myer GD, Ford KR, Brent JL, Hewett TE. . Differential neuromuscular training effects on ACL injury risk factors in “high-risk” versus “low-risk” athletes. BMC Musculoskelet Disord. 2007; 8: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Myer GD, Ford KR, Hewett TE. . Rationale and clinical techniques for anterior cruciate ligament injury prevention among female athletes. J Athl Train. 2004; 39 4: 352– 364. [PMC free article] [PubMed] [Google Scholar]
- 21. DiStefano LJ, Blackburn JT, Marshall SW, Guskiewicz KM, Garrett WE, Padua DA. . Effects of an age-specific anterior cruciate ligament injury prevention program on lower extremity biomechanics in children. Am J Sports Med. 2011; 39 5: 949– 957. [DOI] [PubMed] [Google Scholar]
- 22. Hewett TE, Myer GD, Ford KR. . Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J Knee Surg. 2005; 18 1: 82– 88. [DOI] [PubMed] [Google Scholar]
- 23. Padua DA, Distefano LJ. . Sagittal plane knee biomechanics and vertical ground reaction forces are modified following ACL injury prevention programs: a systematic review. Sports Health. 2009; 1 2: 165– 173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Alentorn-Geli E, Myer GD, Silvers HJ, et al. Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. Knee Surg Sports Traumatol Arthrosc. 2009; 17 8: 859– 879. [DOI] [PubMed] [Google Scholar]
- 25. Shultz SJ, Schmitz RJ, Nguyen AD. . Research retreat IV: ACL injuries—the gender bias: April 3–5, 2008 Greensboro, NC. J Athl Train. 2008; 43 5: 530– 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ardern CL, Webster KE, Taylor NF, Feller JA. . Return to sport following anterior cruciate ligament reconstruction surgery: a systematic review and meta-analysis of the state of play. Br J Sports Med. 2011; 45 7: 596– 606. [DOI] [PubMed] [Google Scholar]
- 27. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. . Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012; 22 2: 116– 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Paterno MV, Schmitt LC, Ford KR, et al. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010; 38 10: 1968– 1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A. 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007; 35 4: 564– 574. [DOI] [PubMed] [Google Scholar]
- 30. Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: a prospective MOON cohort study. Am J Sports Med. 2007; 35 7: 1131– 1134. [DOI] [PubMed] [Google Scholar]
- 31. Downs SH, Black N. . The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998; 52 6: 377– 384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hart HF, Culvenor AG, Collins NJ, et al. Knee kinematics and joint moments during gait following anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Br J Sports Med. 2016; 50 10: 597– 612. [DOI] [PubMed] [Google Scholar]
- 33. Cohen J. . Statistical Power Analysis for Behavioral Sciences. New York, NY: Academic Press; 1977. [Google Scholar]
- 34. Webster KE, Wotherspoon S, Feller JA, McClelland JA. . The effect of anterior cruciate ligament graft orientation on rotational knee kinematics. Knee Surg Sports Traumatol Arthrosc. 2013; 21 9: 2113– 2120. [DOI] [PubMed] [Google Scholar]
- 35. Gokeler A, Hof AL, Arnold MP, Dijkstra PU, Postema K, Otten E. . Abnormal landing strategies after ACL reconstruction. Scand J Med Sci Sports. 2010; 20 1: e12– e19. [DOI] [PubMed] [Google Scholar]
- 36. Bell DR, Blackburn JT, Hackney AC, Marshall SW, Beutler AI, Padua DA. . Jump-landing biomechanics and knee-laxity change across the menstrual cycle in women with anterior cruciate ligament reconstruction. J Athl Train. 2014; 49 2: 154– 162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bell DR, Smith MD, Pennuto AP, Stiffler MR, Olson ME. . Jump-landing mechanics after anterior cruciate ligament reconstruction: a landing error scoring system study. J Athl Train. 2014; 49 4: 435– 441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kuenze CM, Foot N, Saliba SA, Hart JM. . Drop-landing performance and knee-extension strength after anterior cruciate ligament reconstruction. J Athl Train. 2015; 50 6: 596– 602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Hewett TE. . Effects of sex on compensatory landing strategies upon return to sport after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2011; 41 8: 553– 559. [DOI] [PubMed] [Google Scholar]
- 40. Myer GD, Martin L Jr, Ford KR, et al. No association of time from surgery with functional deficits in athletes after anterior cruciate ligament reconstruction: evidence for objective return-to-sport criteria. Am J Sports Med. 2012; 40 10: 2256– 2263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chouliaras V, Ristanis S, Moraiti C, Tzimas V, Stergiou N, Georgoulis AD. . Anterior cruciate ligament reconstruction with a quadrupled hamstrings tendon autograft does not restore tibial rotation to normative levels during landing from a jump and subsequent pivoting. J Sports Med Phys Fitness. 2009; 49 1: 64– 70. [PubMed] [Google Scholar]
- 42. Lam MH, Fong DT, Yung PS, Ho EP, Fung KY, Chan KM. . Knee rotational stability during pivoting movement is restored after anatomic double-bundle anterior cruciate ligament reconstruction. Am J Sports Med. 2011; 39 5: 1032– 1038. [DOI] [PubMed] [Google Scholar]
- 43. Misonoo G, Kanamori A, Ida H, Miyakawa S, Ochiai N. . Evaluation of tibial rotational stability of single-bundle vs. anatomical double-bundle anterior cruciate ligament reconstruction during a high-demand activity—a quasi-randomized trial. Knee. 2012; 19 2: 87– 93. [DOI] [PubMed] [Google Scholar]
- 44. Ristanis S, Stergiou N, Patras K, Tsepis E, Moraiti C, Georgoulis AD. . Follow-up evaluation 2 years after ACL reconstruction with bone-patellar tendon-bone graft shows that excessive tibial rotation persists. Clin J Sport Med. 2006; 16 2: 111– 116. [DOI] [PubMed] [Google Scholar]
- 45. Ristanis S, Stergiou N, Patras K, Vasiliadis HS, Giakas G, Georgoulis AD. . Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy. 2005; 21 11: 1323– 1329. [DOI] [PubMed] [Google Scholar]
- 46. Rudroff T. . Functional capability is enhanced with semitendinosus than patellar tendon ACL repair. Med Sci Sports Exerc. 2003; 35 9: 1486– 1492. [DOI] [PubMed] [Google Scholar]
- 47. Zampeli F, Ntoulia A, Giotis D, et al. The PCL index is correlated with the control of rotational kinematics that is achieved after anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2014; 42 3: 665– 674. [DOI] [PubMed] [Google Scholar]
- 48. Zampeli F, Pappas E, Giotis D, Hantes ME, Georgoulis AD. . Kinematic predictors of subjective outcome after anterior cruciate ligament reconstruction: an in vivo motion analysis study. Knee Surg Sports Traumatol Arthrosc. 2012; 20 4: 785– 792. [DOI] [PubMed] [Google Scholar]
- 49. Dai B, Butler RJ, Garrett WE, Queen RM. . Using ground reaction force to predict knee kinetic asymmetry following anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2014; 24 6: 974– 981. [DOI] [PubMed] [Google Scholar]
- 50. Decker MJ, Torry MR, Noonan TJ, Riviere A, Sterett WI. . Landing adaptations after ACL reconstruction. Med Sci Sports Exerc. 2002; 34 9: 1408– 1413. [DOI] [PubMed] [Google Scholar]
- 51. Delahunt E, Prendiville A, Sweeney L, et al. Hip and knee joint kinematics during a diagonal jump landing in anterior cruciate ligament reconstructed females. J Electromyogr Kinesiol. 2012; 22 4: 598– 606. [DOI] [PubMed] [Google Scholar]
- 52. Delahunt E, Sweeney L, Chawke M, et al. Lower limb kinematic alterations during drop vertical jumps in female athletes who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012; 30 1: 72– 78. [DOI] [PubMed] [Google Scholar]
- 53. Ernst GP, Saliba E, Diduch DR, Hurwitz SR, Ball DW. . Lower-extremity compensations following anterior cruciate ligament reconstruction. Phys Ther. 2000; 80 3: 251– 260. [PubMed] [Google Scholar]
- 54. Giotis D, Zampeli F, Pappas E, Mitsionis G, Papadopoulos P, Georgoulis AD. . Effects of knee bracing on tibial rotation during high loading activities in anterior cruciate ligament-reconstructed knees. Arthroscopy. 2013; 29 10: 1644– 1652. [DOI] [PubMed] [Google Scholar]
- 55. Goerger BM, Marshall SW, Beutler AI, Blackburn JT, Wilckens JH, Padua DA. . Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: the JUMP-ACL study. Br J Sports Med. 2014; 49 3: 188– 195. [DOI] [PubMed] [Google Scholar]
- 56. Miranda DL, Fadale PD, Hulstyn MJ, Shalvoy RM, Machan JT, Fleming BC. . Knee biomechanics during a jump-cut maneuver: effects of sex and ACL surgery. Med Sci Sports Exerc. 2013; 45 5: 942– 951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Mohammadi F, Salavati M, Akhbari B, Mazaheri M, Mohsen Mir S, Etemadi Y. . Comparison of functional outcome measures after ACL reconstruction in competitive soccer players: a randomized trial. J Bone Joint Surg Am. 2013; 95 14: 1271– 1277. [DOI] [PubMed] [Google Scholar]
- 58. Nyland J, Klein S, Caborn DN. . Lower extremity compensatory neuromuscular and biomechanical adaptations 2 to 11 years after anterior cruciate ligament reconstruction. Arthroscopy. 2010; 26 9: 1212– 1225. [DOI] [PubMed] [Google Scholar]
- 59. Nyland J, Mauser N, Caborn DN. . Sports involvement following ACL reconstruction is related to lower extremity neuromuscular adaptations, subjective knee function and health locus of control. Knee Surg Sports Traumatol Arthrosc. 2013; 21 9: 2019– 2028. [DOI] [PubMed] [Google Scholar]
- 60. Ortiz A, Olson S, Libby CL, et al. Landing mechanics between noninjured women and women with anterior cruciate ligament reconstruction during 2 jump tasks. Am J Sports Med. 2008; 36 1: 149– 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Orishimo KF, Kremenic IJ, Mullaney MJ, McHugh MP, Nicholas SJ. . Adaptations in single-leg hop biomechanics following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010; 18 11: 1587– 1593. [DOI] [PubMed] [Google Scholar]
- 62. Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE. . Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clin J Sport Med. 2007; 17 4: 258– 262. [DOI] [PubMed] [Google Scholar]
- 63. Sato K, Maeda A, Takano Y, Matsuse H, Ida H, Shiba N. . Relationship between static anterior laxity using the KT-1000 and dynamic tibial rotation during motion in patients with anatomical anterior cruciate ligament reconstruction. Kurume Med J. 2013; 60 1: 1– 6. [DOI] [PubMed] [Google Scholar]
- 64. Tsai LC, McLean S, Colletti PM, Powers CM. . Greater muscle co-contraction results in increased tibiofemoral compressive forces in females who have undergone anterior cruciate ligament reconstruction. J Orthop Res. 2012; 30 12: 2007– 2014. [DOI] [PubMed] [Google Scholar]
- 65. Tsai LC, Powers CM. . Increased hip and knee flexion during landing decreases tibiofemoral compressive forces in women who have undergone anterior cruciate ligament reconstruction. Am J Sports Med. 2013; 41 2: 423– 429. [DOI] [PubMed] [Google Scholar]
- 66. Vairo GL, Myers JB, Sell TC, Fu FH, Harner CD, Lephart SM. . Neuromuscular and biomechanical landing performance subsequent to ipsilateral semitendinosus and gracilis autograft anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2008; 16 1: 2– 14. [DOI] [PubMed] [Google Scholar]
- 67. Webster KE, Santamaria LJ, McClelland JA, Feller JA. . Effect of fatigue on landing biomechanics after anterior cruciate ligament reconstruction surgery. Med Sci Sports Exerc. 2012; 44 5: 910– 916. [DOI] [PubMed] [Google Scholar]
- 68. Giotis D, Zampeli F, Pappas E, Mitsionis G, Papadopoulos P, Georgoulis AD. Effects of knee bracing on tibial rotation during high loading activities in anterior cruciate ligament-reconstructed knees. Arthroscopy. 2013; 29 10: 1644– 1652. [DOI] [PubMed] [Google Scholar]
- 69. Hooper DM, Morrissey MC, Drechsler WI, Clark NC, Coutts FJ, McAuliffe TB. . Gait analysis 6 and 12 months after anterior cruciate ligament reconstruction surgery. Clin Orthop Relat Res. 2002; 403: 168– 178. [DOI] [PubMed] [Google Scholar]
- 70. Lewek M, Rudolph K, Axe M, Snyder-Mackler L. . The effect of insufficient quadriceps strength on gait after anterior cruciate ligament reconstruction. Clin Biomech (Bristol, Avon). 2002; 17 1: 56– 63. [DOI] [PubMed] [Google Scholar]
- 71. Hall M, Stevermer CA, Gillette JC. . Gait analysis post anterior cruciate ligament reconstruction: knee osteoarthritis perspective. Gait Posture. 2012; 36 1: 56– 60. [DOI] [PubMed] [Google Scholar]
- 72. Lepley AS, Gribble PA, Thomas AC, Tevald MA, Sohn DH, Pietrosimone BG. . Longitudinal evaluation of stair walking biomechanics in patients with ACL injury. Med Sci Sports Exerc. 2016; 48 1: 7– 15. [DOI] [PubMed] [Google Scholar]
- 73. Andriacchi TP, Mündermann A, Smith RL, Alexander EJ, Dyrby CO, Koo S. . A framework for the in vivo pathomechanics of osteoarthritis at the knee. Ann Biomed Eng. 2004; 32 3: 447– 457. [DOI] [PubMed] [Google Scholar]
- 74. Ingersoll CD, Grindstaff TL, Pietrosimone BG, Hart JM. . Neuromuscular consequences of anterior cruciate ligament injury. Clin Sports Med. 2008; 27 3: 383– 404, vii. [DOI] [PubMed] [Google Scholar]
- 75. Sturnieks DL, Besier TF, Mills PM, et al. Knee joint biomechanics following arthroscopic partial meniscectomy. J Orthop Res. 2008; 26 8: 1075– 1080. [DOI] [PubMed] [Google Scholar]
- 76. Myer GD, Ford KR, Khoury J, Hewett TE. . Three-dimensional motion analysis validation of a clinic-based nomogram designed to identify high ACL injury risk in female athletes. Phys Sportsmed. 2011; 39 1: 19– 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Myer GD, Ford KR, Khoury J, Succop P, Hewett TE. . Biomechanics laboratory-based prediction algorithm to identify female athletes with high knee loads that increase risk of ACL injury. Br J Sports Med. 2011; 45 4: 245– 252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Yeow CH, Lee PV, Goh JC. . An investigation of lower extremity energy dissipation strategies during single-leg and double-leg landing based on sagittal and frontal plane biomechanics. Hum Mov Sci. 2011; 30 3: 624– 635. [DOI] [PubMed] [Google Scholar]
- 79. Ford KR, Myer GD, Hewett TE. . Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003; 35 10: 1745– 1750. [DOI] [PubMed] [Google Scholar]
- 80. Arendt E, Dick R. . Knee injury patterns among men and women in collegiate basketball and soccer. NCAA data and review of literature. Am J Sports Med. 1995; 23 6: 694– 701. [DOI] [PubMed] [Google Scholar]
- 81. Di Stasi S, Myer GD, Hewett TE. . Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013; 43 11: 777– 792, A1–A11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Benjaminse A, Gokeler A, Dowling AV, et al. Optimization of the anterior cruciate ligament injury prevention paradigm: novel feedback techniques to enhance motor learning and reduce injury risk. J Orthop Sports Phys Ther. 2015; 45 3: 170– 182. [DOI] [PubMed] [Google Scholar]
- 83. Ericksen HM, Gribble PA, Pfile KR, Pietrosimone BG. . Different modes of feedback and peak vertical ground reaction force during jump landing: a systematic review. J Athl Train. 2013; 48 5: 685– 695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Ericksen HM, Thomas AC, Gribble PA, Armstrong C, Rice M, Pietrosimone B. . Jump-landing biomechanics following a 4-week real-time feedback intervention and retention. Clin Biomech (Bristol, Avon). 2016; 32: 85– 91. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.