Abstract
Objective
To report a diagnosis of hereditary leiomyomatosis and renal cell cancer (HLRCC) syndrome following initial presentation with multiple cutaneous lesions.
Design
Case report.
Design classification
N/A.
Setting
Academic tertiary care center.
Patient(s)
27-year-old nulligravid woman who presented with multiple red-brown lesions on her skin found to have cutaneous and uterine leiomyoma.
Intervention(s)
Biopsy of cutaneous lesions and fertility sparing robot-assisted laparoscopic myomectomy (RALM).
Main outcome measures(s)
Histological assessment of uterine leiomyoma.
Results(s)
Pathologic examination of uterine leiomyoma revealed diffuse atypia and fumarate hydratase loss phenotype concerning for genetic syndrome. Follow-up DNA sequencing via Sanger sequencing confirmed a pathogenetic R2333H mutation consistent with HLRCC.
Conclusion(s)
Consideration of HLRCC on differential diagnosis when patients present with cutaneous nodules and atypical or early onset uterine leiomyoma provides opportunity for early surveillance, family member testing, and more thoughtful surgical planning.
Precis
27-year-old woman with multiple cutaneous lesions is found to have uterine leiomyomas and undergoes robotic myomectomy. Genetic testing of uterine leiomyomas reveals mutation in fumarate hydratase, etiologic in hereditary leiomyomatosis and renal cell cancer (HLRCC).
Keywords: Cutaneous lesions, Fibroids, Leiomyoma, Hereditary leiomyomatosis and renal cell cancer, HLRCC
Highlights
-
•
Atypical skin findings and fibroids warrant consideration of HLRCC on the differential diagnosis.
-
•
Consider similar genetic testing and management as those with Lynch syndrome associated endometrial cancer.
-
•
Pre-operative planning should take HLRCC into consideration when considering tissue containment and removal strategies.
1. Introduction
Hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome is an autosomal dominant disorder caused by a germ line mutation in FH, encoding the Krebs cycle enzyme fumarate hydratase. Mutations in FH have been described in over 100 families worldwide, and various genotype-phenotype relationships have been suggested involving tumor suppression [1]. Uterine leiomyomas are a common gynecologic tumor present in up to 77% of reproductive age women [2]. HLRCC, characterized by multiple cutaneous and uterine leiomyomas, predisposes for aggressive papillary type II renal cell carcinoma and, rarely, leiomyosarcoma (LMS) [3], [4]. This rare genetic condition likely remains undiagnosed in many individuals, as the appearance of cutaneous nodules is often a non-specific and under investigated clinical finding. Herein, we describe a case in which cutaneous lesions in a young woman prompted further evaluation leading to an eventual diagnosis of HLRCC.
2. Case Report
A 27-year-old, nulligravid woman presented to her primary care physician with multiple red-brown, raised maculopapular lesions. She first reported developing these lesions on her back five years prior to presentation. On exam, multiple nodular and non-tender lesions were noted (Fig. 1). Her medical history was significant only for an unrepaired ventricular septal defect. She did not report any surgical history or use of prescription medications. In consultation with a dermatologist, who believed the lesions to be keloids or cysts, a nodule was biopsied. Dermatopathology confirmed cutaneous leiomyomata. During the interval of evaluation and biopsy, she developed new lesions on her arms, chest, and thighs.
Fig. 1.

Photograph of the patients mid back demonstrating multiple, nodular subcutaneous leiomyoma.
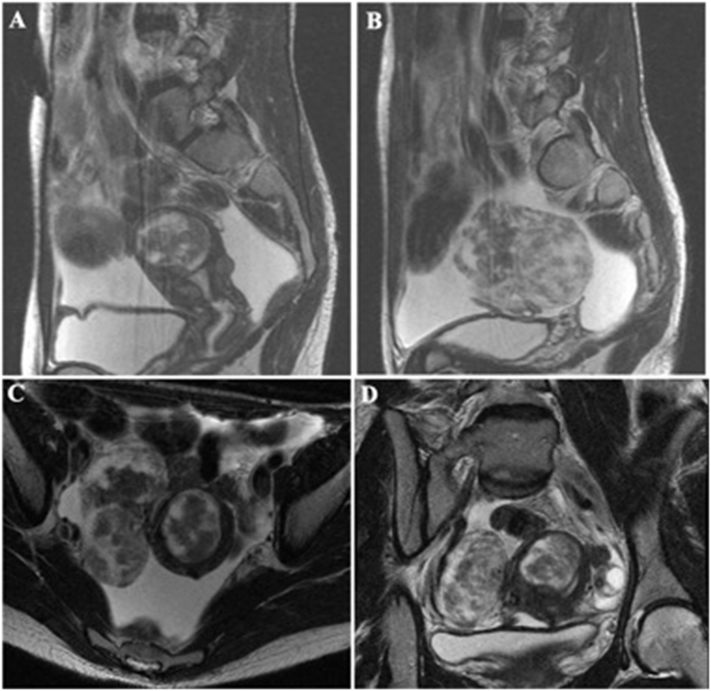
Given clinical suspicion for HLRCC, a more thorough family history revealed a paternal history of renal cell and basal cell carcinoma as well as maternal uterine leiomyoma. As part of her clinical evaluation for HLRCC, kidney function was assessed with serum labs, revealing a creatinine of 0.95 mg/dl and hyperkalemia of 5.4 mmol/L. A renal MRI did not demonstrate any masses. Additionally, a pelvic ultrasound was performed, given an enlarged uterus on pelvic examination. Initial ultrasound demonstrated a fibroid uterus, and due to concern for LMS in HLRCC patients, an MRI was ordered. The MRI identified a subserosal, pedunculated leiomyoma measuring 8.3 cm in diameter and multiple submucosal and intramural leiomyoma, with the largest measuring 4.0 cm (Fig. 2).
Fig. 2.
MRI of abdomen and pelvis with and without contrast: Sagittal T2 images demonstrating a 4 × 4 × 3 cm intramural, fundal fibroid with submucosal component (A) and 8 × 6 × 5 cm heterogeneous, right, subserosal fibroid with broad connection to the uterus (B). Axial T2 image demonstrating both 4 cm intramural and 8 cm right, subserosal fibroids (C). Coronal T2 image demonstrating both 4 cm intramural, fundal and 8 cm right, subserosal fibroid (D).
Given the patient's desire for fertility-sparing surgery and the need to rule out a malignant uterine tumor by histologic diagnosis of presumptive HLRCC, the patient opted for a myomectomy. She underwent a robot-assisted laparoscopic myomectomy (RALM) with resection of four leiomyoma measuring a total of 90 g. Her leiomyoma were removed using uncontained power morcellator, which was considered standard of care at our hospital the time of the operation. Her post-operative course was complicated by a surgical site infection growing Pseudomonas aeruginosa treated with a 14-day course of ofloxacin with complete resolution.
On pathologic examination, the tissue was noted to display diffuse atypia and show nuclear features typically associated with leiomyoma in patients with HLRCC. The patient was referred for genetic testing for mutations in FH. DNA sequence analysis of a peripheral blood sample via Sanger sequencing of FH revealed a heterozygous G > A nucleotide substitution in exon 5, resulting in the replacement of an arginine codon with a histidine codon at amino acid position 233, referred to as R233H at the DNA level (also referred to as R190H in the mutated, truncated protein).
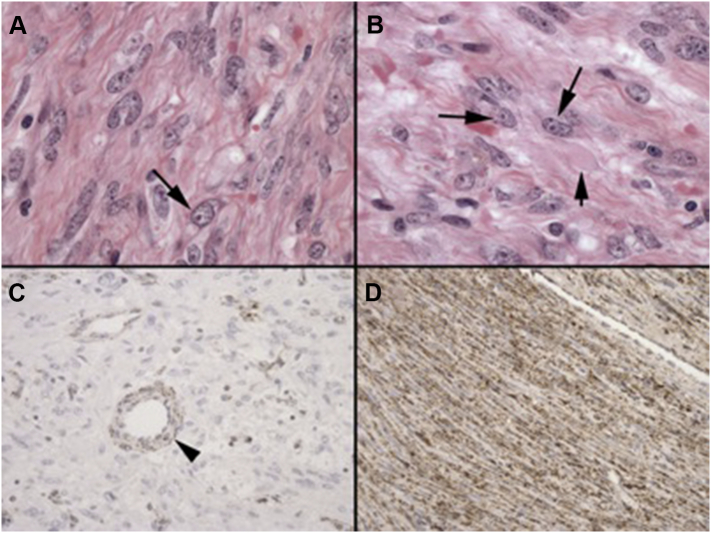
Her uterine leiomyoma were also evaluated for features of HLRCC syndrome. Histopathologic examination by hematoxylin and eosin staining and immunostaining for fumarate hydratase (fumarate hydratase, sc-100743, Santa Cruz Biotechnology, Inc.) revealed a typical “FH loss” phenotype (Fig. 3). Sanger sequencing of uterine leiomyoma was performed using amplified PCR products (QIAamp DNA FFPE Tissue Kit (56404)) with identification of the pathogenetic R233H mutation.
Fig. 3.
Histology of the uterine leiomyomas removed from the subject demonstrating diffuse mild-moderate nuclear atypia and large cherry red nucleoli with distinct clearing of the coarsely granular chromatin around the nucleoli (arrow with long stem) (A, B). Immunohistochemistry with an antibody for fumarate hydratase demonstrated essentially complete loss of protein staining in the neoplastic smooth muscle cells in the subject. Eosinophilic cytoplasmic inclusions (arrow with short stem) and granular cytoplasmic staining reflecting mitochondrial localization were also evident in the non-neoplastic endothelial and vascular smooth muscle cells within the subject's tumor (C). As a positive control, immunohistochemistry was performed on an atypical leiomyomata without the histological phenotype of HLRCC from an unrelated individual, revealing typical granular cytoplasmic staining pattern for fumarate hydratase expression (D).
3. Discussion
While uterine leiomyomas are common, HLRCC is rare, and diagnosing the syndrome is important not only for the affected individual but her entire family. The R233H (or R190H) missense mutation in FH, located on the long arm of chromosome 1 in band q43, is one of many mutations linked to hereditary leiomyomatosis and renal cell cancer (HLRCC). This autosomal dominant disorder results from a defective FH enzyme, which is involved in the Krebs cycle and thus plays a role in cellular metabolism. It is suspected that the inactivated protein, due to a missense mutation, inactivates a highly conserved tumor suppressor, which can lead to benign leiomyomas and aggressive kidney cancer [5], [6]. In a particular patient subset of Finnish descent, FH mutations were also linked to increased risk of early onset uterine leiomyosarcoma [4], [7].
For female patients with a family history of atypical uterine fibroids, early age of onset of fibroids, or a combination of uterine fibroids and cutaneous lesions, genetic testing for a mutation in FH may be an important testing strategy. Furthermore, a positive genetic test for FH may prompt earlier screening for renal cell neoplasms in the patient and family members. Dedicated renal MRI or CT scans with intravenous contrast are recommended for early detection of aggressive renal tumors as their diagnostic accuracy and utility far exceed that of renal ultrasound when there is a high degree of suspicion for renal cancer [8]. Lifetime risk for renal cell cancer in HLRCC patients is estimated to be 15% for men and women [9]. Affected women may have even greater risk for RCC than their affected male family members [8].
Awareness of an HLRCC phenotype and genetic testing for FH can be critical to optimal patient management, especially as morphological identification of HLRCC-associated tumors by histopathology may be inconsistent [10]. We now recognize that uterine leiomyoma with FH mutations have a characteristic microscopic appearance, including prominent enlarged, orangeophilic nucleoli, surrounded by clearing of the nuclear chromatin, usually associated with a recognizable, albeit low level nuclear atypia (slightly enlarged nuclei and slightly coarser chromatin) and sometimes eosinophilic cytoplasmic inclusions. Traditionally, S-(2-succinyl) cysteine (S2C) overexpression using anti-2SC antibodies and appearance of eosinophilic nucleoli have been used as a biomarker for HLRCC-associated tumors [11], [12]. However, the use of anti-FH antibodies has been shown to be a readily available and reliable alternative for HLRCC screening on tissue specimens.
Once a diagnosis is made a careful surveillance and treatment plan should be discussed with the patient. Given that a large percentage of patients with HLRCC are likely of reproductive age, early diagnosis and monitoring allows for a more thoughtful discussion on medical management and fertility sparing surgery. In the case of our patient, she was able to conceive spontaneously one year after her RALM and delivered via cesarean section at 38 weeks. When considering myomectomy, the link between HLRCC and LMS, albeit rare, should give surgeons pause before proceeding with surgical management.
When there is clinical suspicion for occult malignancy, hysterectomy, or en bloc resection of the uterus, is the preferred surgical option. In one study, 89% of women with cutaneous and uterine leiomyomas underwent hysterectomy, of which 57% were under the age of 30 years [8]. Myomectomy allows patients to preserve fertility, and elect for definitive surgery after the completion of childbearing. However, myomectomy also implies acknowledgement by the patient and the surgeon that an occult LMS may be disseminated thus potentially upstaging of occult LMS within the abdomen and pelvis when morcellation is performed [13]. The prevalence of LMS in women undergoing hysterectomy or myomectomy for presumed benign indications is estimated at 0.2% (1 in 458) by the FDA [14]. Contained morcellation has been proposed as a risk reducing strategy in patients opting for myomectomy. However, even when contained morcellation is employed, tissue or dye dissemination has been reported in up to 9.7% of cases [15]. Thus, when considering surgical management, a discussion with the patient regarding the risk of occult malignancy as well as risk reducing strategies is an important part of an informed consent process.
In women with atypical skin findings and fibroids a consideration of HLRCC in the differential diagnosis is warranted. A thorough physical examination and in-depth family history can raise suspicion for this heritable disorder. If palpable cutaneous lesions or renal masses are also present, they should biopsied and analyzed for histopathologic and immunopathologic findings of HLRCC. Finally, gynecologists should consider genetic testing and management for HLRCC in the same manner in which they care for women with endometrial cancer with a diagnosis of Lynch syndrome. When suspicion or knowledge of such a diagnosis is made, pre-operative planning should take this into consideration when considering tissue containment and removal.
Disclosures
RMA, CCM, and EAS are supported by the Agency for Healthcare Research and Quality (AHRQ) (5P50HS023418-02), and Patient-Centered Outcomes Research Institute (PCORI) through COMPARE-UF (Comparing Options for Management: Patient-Centered Results for Uterine Fibroids). ARG is a consultant for Omniguide Holdings, Inc. and for Medicaroid, Inc. No funding was used for this manuscript. The patient in question granted the authors consent to include her history, exam, images, and evaluation in this manuscript.
References
- 1.Schmidt L.S., Linehan W.M. Hereditary leiomyomatosis and renal cell carcinoma. Int. J. Nephrol. Renov. Dis. 2014;7:253–260. doi: 10.2147/IJNRD.S42097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart E.A. Uterine fibroids. Lancet. 2001;357(9252):293–298. doi: 10.1016/S0140-6736(00)03622-9. [DOI] [PubMed] [Google Scholar]
- 3.Launonen V. Inherited susceptibility to uterine leiomyomas and renal cell cancer. Proc. Natl. Acad. Sci. U. S. A. 2001;98(6):3387–3392. doi: 10.1073/pnas.051633798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ylisaukko-oja S.K. Analysis of fumarate hydratase mutations in a population-based series of early onset uterine leiomyosarcoma patients. Int. J. Cancer. 2006;119(2):283–287. doi: 10.1002/ijc.21798. [DOI] [PubMed] [Google Scholar]
- 5.Tomlinson I.P. Germline mutations in FH predispose to dominantly inherited uterine fibroids, skin leiomyomata and papillary renal cell cancer. Nat. Genet. 2002;30(4):406–410. doi: 10.1038/ng849. [DOI] [PubMed] [Google Scholar]
- 6.Costa B. Fumarase tumor suppressor gene and MET oncogene cooperate in upholding transformation and tumorigenesis. FASEB J. 2010;24(8):2680–2688. doi: 10.1096/fj.09-146928. [DOI] [PubMed] [Google Scholar]
- 7.Lehtonen H.J. Increased risk of cancer in patients with fumarate hydratase germline mutation. J. Med. Genet. 2006;43(6):523–526. doi: 10.1136/jmg.2005.036400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toro J.R. Mutations in the fumarate hydratase gene cause hereditary leiomyomatosis and renal cell cancer in families in North America. Am. J. Hum. Genet. 2003;73(1):95–106. doi: 10.1086/376435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Menko F.H. Hereditary leiomyomatosis and renal cell cancer (HLRCC): renal cancer risk, surveillance and treatment. Familial Cancer. 2014 doi: 10.1007/s10689-014-9735-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alsolami S. Current morphologic criteria perform poorly in identifying hereditary leiomyomatosis and renal cell carcinoma syndrome-associated uterine leiomyomas. Int. J. Gynecol. Pathol. 2014;33(6):560–567. doi: 10.1097/PGP.0000000000000091. [DOI] [PubMed] [Google Scholar]
- 11.Bardella C. Aberrant succination of proteins in fumarate hydratase-deficient mice and HLRCC patients is a robust biomarker of mutation status. J. Pathol. 2011;225(1):4–11. doi: 10.1002/path.2932. [DOI] [PubMed] [Google Scholar]
- 12.Merino M.J. The morphologic spectrum of kidney tumors in hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome. Am. J. Surg. Pathol. 2007;31(10):1578–1585. doi: 10.1097/PAS.0b013e31804375b8. [DOI] [PubMed] [Google Scholar]
- 13.Park J.Y. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma. Gynecol. Oncol. 2011;122(2):255–259. doi: 10.1016/j.ygyno.2011.04.021. [DOI] [PubMed] [Google Scholar]
- 14.Administration, U.F.a.D. 2017. UPDATED Laparoscopic Uterine Power Morcellation in Hysterectomy and Myomectomy: FDA Safety Communication. [Google Scholar]
- 15.Cohen S.L. Contained tissue extraction using power morcellation: prospective evaluation of leakage parameters. Am. J. Obstet. Gynecol. 2016;214(2):257.e1–257.e6. doi: 10.1016/j.ajog.2015.08.076. [DOI] [PubMed] [Google Scholar]