Abstract
Purpose
Adults and children with intellectual disability (ID) are vulnerable to preventable morbidity and mortality due to poor quality healthcare. While poor quality care has been commonly identified among children with ID, evidence of the patient safety outcomes for this group is lacking and therefore explored in this review.
Data sources
Systematic searches of six electronic bibliographic research databases were undertaken from January 2000 to October 2017, in addition to hand searching.
Study selection
Keywords, subject headings and MeSH terms relating to the experience of iatrogenic harm during hospitalisation for children with ID were used. Potentially relevant articles were screened against the eligibility criteria. Non-English language papers were excluded.
Data extraction
Data regarding: author(s), publication year, country, sample, health service setting, study design, primary focus and main findings related to measures of quality and safety performance were extracted.
Results of data synthesis
Sixteen studies met the inclusion criteria, with three themes emerging: the impact of the assumptions of healthcare workers (HCWs) about the child with ID on care quality and associated safety outcomes; reliance on parental presence during hospitalisation as a protective factor; and the need for HCWs to possess comprehensive understanding of the IDs experienced by children in their care, to scientifically deduce how hospitalisation may compromise their safety, care quality and treatment outcomes.
Conclusion
When HCWs understand and are responsive to children’s individual needs and their ID, they are better placed to adjust care delivery processes to improve care quality and safety during hospitalisation for children with ID.
Keywords: health service, patient perspective, general paediatrics, multidisciplinary team-care, children’s rights
What is already known on this topic?
Approximately 1% to 3% of all children globally have intellectual disability (ID).
Adverse events during hospitalisation are common, occurring in approximately 9.2% to 36.7% of children.
People with ID are admitted to hospital more frequently than their peers, but rates and antecedent factors of adverse events among this population are unknown.
What this study hopes to add?
To minimise adverse events among children with ID, and promote greater equity in care, it is necessary to understand the specific risks associated with care for this population.
The synthesised literature presented shows that when healthcare workers understand the child with ID and how hospitalisation can increase their vulnerability to iatrogenic harm, disparate treatment outcomes can be avoided.
Healthcare workers can improve care quality and optimise treatment outcomes for these children during hospitalisation by engaging with parents/carers when planning care.
Introduction
The provision of a safe, effective and high-quality healthcare is an unalienable human right.1 Poor quality care during hospitalisation is associated with iatrogenic harm and adverse events (AEs)2 3 making it a key global concern.4 The estimated rate of AEs in Organisation for Economic Co-operation and Development countries is 10% of hospitalised adults, which is thought to be conservative.2 5 In the paediatric context, reported rates of AEs for children during hospitalisation vary internationally from 9.2% in Canada,6 14.2% in the UK7 and 36.7% in the USA.8 Children are vulnerable to AEs due to unique iatrogenic risks; for example, in children, drug dosage calculations are weight-based, commonly resulting in medication errors.3
Greater vulnerability to poor quality care during hospitalisation is evident in particular populations.4 People with intellectual disability (ID) have higher rates of preventable, premature mortality than the general population9 10 and experience poorer quality care during hospitalisation.11 12 This represents a clear health inequity for people with ID,9 13 exacerbated by the challenges in identifying and reporting patient safety issues among this population,12 which make it difficult to quantify their incidence of AE.
Children with complex medical needs are reported to experience higher rates of AEs and prolonged admissions during hospitalisation.6 14 For children with ID, the possibility of experiencing iatrogenic harm is compounded by the unique vulnerabilities of children to AEs during hospitalisation,3 14 and the poor care quality experienced by patients with ID.9 11 It is imperative to determine and address the features of hospitalisation that increase the likelihood of children with ID experiencing poor quality care, which manifest as iatrogenic harm and AEs. The vulnerability of children with ID to experience poor quality and less safe care is an ethically and economically significant issue, yet one that is underexamined.
This study aimed to provide a narrative synthesis of published evidence concerning the experience of iatrogenic harm during hospitalisation for children with ID to discern the evidence base and knowledge gaps. The review findings highlight opportunities for policy changes and quality improvement (QI) interventions that could enhance the quality of care delivered to children with ID internationally.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement is an evidence-based approach for reporting in systematic reviews and meta-analyses that was used to guide the reporting of this review.15
Eligibility criteria
Inclusion criteria
Since the 1999 publication of the pivotal work, To Err is Human, patient safety research has intensified in magnitude and scope.2 As such, we searched for publications in English published since 2000 that met the criteria listed below.
Participants
Children (<18 years of age) in hospital as inpatients, aligning with the United Nations definition of child.16 Included publications were required to reference children with ID. This could include either a specific condition known to include ID, such as Down syndrome (DS), or terms that are synonymous with ID such as cognitive impairment, learning disability or developmental disability.13
Intervention
AEs, which could be described using any of the following terms: adverse event, medical error, near miss, adverse incident, unsafe care, patient safety incident or problems with quality of care.
Comparator
Clinical outcomes for children without ID of a care process known to require hospitalisation.
Outcomes
Either clinical outcomes for children with ID of a procedure known to require hospitalisation, self- or family/carer-reported outcomes of such care experiences, or any other terms referring to objective or subjective measures of the quality and safety (Q&S) of inpatient healthcare.
Exclusion criteria
Publications were excluded if they were published prior to 2000, were not available in English, did not focus on patient safety or quality in children who were inpatients and under 18 years or did not include reference to children with ID in the abstract. Publications of the following issues were excluded:
primary care settings
inpatient mental health settings
risks of hospitalisation due to pre-admission patient factors
hospital admissions of <24 hours
effectiveness of surgery without a non-ID comparator
errors in diagnosis of ID or medical negligence
patient/parent satisfaction with healthcare services which did not focus on adverse safety events
case reviews
or rates of hospitalisation and/or healthcare utilisation by children with ID.
Publications that did not include analysis of impacts on care quality and patient safety were excluded. The final exclusion criteria ensured that included publications focused on inpatient care, as short stay contexts present other Q&S concerns that warrant separate research.2
Study identification
A range of text words, synonyms and subject headings for the major foci of this study were used to undertake a systematic search of six electronic databases from January 2000 to October 2017. An initial search was conducted in Medline to refine the search terms (see online supplementary appendix 1 for search terms). The remaining searches were conducted from 3 November to 11 November 2017, involving MEDLINE, EMBASE, CINAHL, PsychInfo, Scopus and Web of Science. Hand searching of reference lists of included publications was also undertaken to ensure that all relevant sources were included for data extraction and synthesis.
bmjpo-2017-000201supp002.pdf (69.8KB, pdf)
Study selection and data extraction
Titles and abstracts were screened, and a copy of the full paper was obtained for relevant articles. The following data were extracted from eligible publications: author(s), publication year, country, sample, health service setting, study design and main focus. Where available, data extraction included main findings related to measures of Q&S performance, such as length of stay, and morbidity and mortality outcomes, as well as any self-reported experiences of AEs or iatrogenic harm, unsafe care or concerns with quality of care.
Assessment of the quality of the studies
The quality of included publications was assessed by the authors using the Quality Assessment Tool for Studies with Diverse Designs.17 Using this tool, the authors assessed the study quality of the included publications using a four-point scale (0–3) against 16 criteria to indicate the quality of each publication and the overall body of evidence. One reviewer (LM) individually assessed all publications and a second reviewer independently assessed a subset of the publications; disagreements were resolved through discussion resulting in substantial agreement (κ=0.75) between reviewers on a random sample of 25% of the papers. Because there were few publications, we did not exclude publications based on the quality assessment. Quality assessment data was used to explore the strength of the available evidence.
Narrative synthesis of key themes of included publications
The findings of included publications were analysed using a narrative synthesis approach, based on the study objectives, to elicit key themes articulated in the literature.18 A narrative approach was necessary to synthesise the heterogeneous qualitative and quantitative findings.19 Overarching descriptions of each publication were tabulated (see online supplementary table S1), then patterns in the data were explored to identify consistent themes across the publications. Regular discussions among the study team helped refine the analysis and enhance study validity.
bmjpo-2017-000201supp001.pdf (523.3KB, pdf)
Results
Title and abstract screening resulted in the identification of 30 publications that fulfilled the inclusion criteria. From these, 11 publications were eligible based on the full text review, with a further five identified from reference list searches. A total of 16 publications were included in the review (see figure 1).
Figure 1.
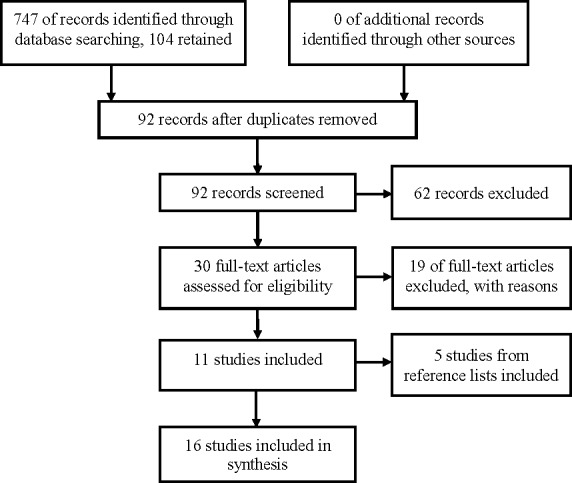
Study selection flowchart.
Characteristics of included studies
A list of included studies, with titles, aims, methodology, participants and main findings with key themes, is displayed in online supplementary table S1. Eleven publications were published since 2010. All were set in specialist paediatric units, and all but one in high-income countries. Seven publications were from the USA, five from the UK, two from The Netherlands, and one each from Canada, India and Japan.
Twelve publications used quantitative methodologies, though no publication specified rates of iatrogenic harm or AEs among children with ID. In eight publications, data were extracted from a single centre, three publications used data from a national database and one was a multicentre study. Four publications used qualitative methods to explore the experience of hospitalisation for children with ID within a specific health service, without comparator populations.
While the study population of interest was all children with ID, 10 publications were specific to children with DS, with the remaining six inclusive of any ID condition. The postoperative experience for children with DS compared with children without DS was described in 10 studies. Of these, six studies related to specifically to cardiac surgery outcomes,20–25 and two considered anaesthetics and/or pain management after surgery.26 27 The remaining two studies looked at surgical intervention for Hirschsprung’s disease, comparing outcomes in children with and without DS.28 29
Two papers reviewed the comparative hospital experience for children with non-specific ID to children without ID. One of these described the post general anaesthetic experience for children with complex special healthcare needs, referencing developmental disorders and DS in the abstract as a factor of interest.26 The final paper investigated the assessment and management of pain in children with and without ID after spinal surgery.30
Study quality
Diverse quality was seen across publications when assessed against the quality criteria17 (see supplementary table S2). Most provided theoretical background to the study, and descriptions of the methods for data collection and analysis. All but one publication relied on opportunistic sampling through a single centre, or retrospective data from existing databases. Subsequently, sample sizes were wide ranging, though study populations were generally well described. Discussion of limitations varied; most gave concise critiques, though two publications lacked any critique of limitations.
bmjpo-2017-000201supp003.pdf (421.2KB, pdf)
Key themes
Three main themes were identified: the impact of HCWs assumptions about the child with ID on care quality and associated safety outcomes; reliance on parental presence during hospitalisation as a protective factor from poor care quality and safety outcomes; and the need for HCWs to understand the child and the ID to know how hospitalisation may compromise their safety, care quality and treatment outcomes. Each theme is described below.
The impact of HCWs assumptions about the child with ID on care quality and associated safety outcomes
Labels, assumptions and stereotyping were described in three publications, which had positive and negative impacts on care provision.31–33 Having a diagnosis or label of an ID can be beneficial for parents to negotiate their child’s care needs with HCWs32 and for early diagnosis to maximise treatment outcomes of comorbidities.21 Assumptions, however, made by HCWs regarding the child’s behaviour, cognitive ability or experience of pain may mean they do not understand the unique needs of each child.31–34 Generalisations regarding analgesic requirements or behaviour led to experiences of poor quality care and adverse outcomes during hospitalisation for the child with ID.26 32
The influence of subtle assumptions and stereotyping of children with ID is highlighted in pain assessment.29 Children with ID had lower pain scores and reduced administration of analgesia than children without ID,26 27 30 34 and two publications suggest that this may be due to HCW’s preconceptions.26 34 Several authors commented their findings challenged long-held beliefs regarding the benefit of surgical interventions to treat comorbidities in children with DS,23–25 28 or effective assessment and management of pain in children with ID.27 30 34
Several publications found that parents identified ready access to healthcare, effective communication between patients and HCWs, and positive treatment outcomes, as being dependent on the assumptions, stereotypes and judgements of HCWs.31–33
Parents/carers consistently reported that assumptions, stereotypes and judgements about their child led to poor care experiences and safety concerns,31 32 compounded by a lack of effective communication.32 33 Four publications found, to some extent, that parents/carers felt HCW judgements about them or their child with ID influenced the quality of care their child received.31–33 35
Reliance on parental presence during hospitalisation as a protective factor from poor care quality
HCWs reliance on parental presence to supervise, protect and advocate for the care of their child was described in four publications31–33 35, and to assist in the assessment of pain in two publications.26 30 HCWs reliance on parents also manifest as an expectation for parents/carers to manage their child’s medical needs and behaviour during hospitalisation.33 35 Parents felt this reliance was frustrating when negotiating their child’s care needs with HCWs.31 32 Aston et al32 identified this tension; HCWs relied on parental presence during hospitalisation only to judge the parent when they provide a lot of detail.32 As one parent said, ’I found as soon as I started to talk and say what James’ meds were, what his seizure activity was, that he was non-verbal, I didn’t stop […] and it was just like all of a sudden ‘well she’s a know-it-all’ and that’s not my intent, my intent was so that people knew James’ (p301).32
To overcome this reliance, parents/carers felt it was important that HCWs listened to them and viewed them as the expert of their child.31 33 35 In knowing more about the child and their ID label by listening to parents, several publications found that HCWs can adapt the hospital environment, such as bed location, and negotiate the child’s care needs, to minimise poor care experiences during hospitalisation.31–33 When HCWs understood the complexities of their child’s medical needs in the context of the current hospitalisation31 33 35 reliance on parental presence could be lessened.
Need for HCWs to understand the child and the ID to know how hospitalisation may compromise their safety, care quality and treatment outcomes
Having specific knowledge about a child’s ID can mean HCWs identify responses or physiological susceptibilities to the hospital environment that impact on treatment outcomes,20 29 30 34 and may have a protective value against poor morbidity and mortality related to treatment.21 23 30 When HCWs apply knowledge of the child with ID and make adjustments to care delivery and the hospital environment during hospitalisation, it may reduce poor quality care and clinical complications.33 For example, understanding of how known immunity issues in DS contributes to postoperative infections was identified in four publications,21 22 28 29 though mitigation strategies were not reported. One publication noted that this susceptibility may have contributed to additional intensive care support in children with DS.21 Another publication suggested that knowledge of DS could be protective, finding children with DS ‘are predisposed to complications and thus warrant more cautious management’ (p181).28
Parents generally perceived ID labels as important for HCWs to know, as the hospital and HCWs then knew something about the needs of their child to ensure quality care.32 33 Two publications reported that HCWs must understand the child with ID and their needs during care planning to optimise the care quality during hospitalisation.31 33 Aston et al22 commented that reducing the vulnerability of children with ID to poor quality care goes beyond educating HCWs, necessitating broader social and hospital system change.32
Discussion
The aim of this research was to synthesise published evidence regarding the experience of iatrogenic harm during hospitalisation for children with ID. Sixteen publications, comprising seven from the US, five from the UK, two from The Netherlands, and one each from Canada, India and Japan, met the inclusion criteria. There is evidence that HCWs stereotype behaviours31–33 and overlook factors associated with ID that predispose the child to poor quality care and harm.22 32
Behaviours of the child with ID during hospitalisation may be interpreted or stereotyped as normal, when they are in fact an expression of pain or discomfort.26 30 Assumptions around the experience of pain or behaviour may result in unnecessary respiratory compromise, admission to intensive care and prolonged hospital admission for the child with ID.29 34 This demonstrates that there are specific aspects of hospitalisation that expose children with ID to harms that are preventable, avoidable and not experienced to the same extent by children without ID.
Implications
An awareness of the child and their ID, or having a label of ID, was seen to be beneficial,32 33 and may even be protective against poor outcomes.21 23 28 30 Several publications noted that children with DS are understood to have compromised immunity,21 22 28 29 which can increase their susceptibility to healthcare-associated infections, compared with children without DS. This is assumed to be the reason children with DS are shown to have more non-cardiac complications postoperatively, such as respiratory illness and surgical site infections.21 22 28 Exploration into care quality factors of hospitalisation that increase infection risk for children with DS would add to the knowledge base for this population.
Inadequate or insufficient measures of pain and pain management were also identified, resulting in respiratory complications or prolonged hospital admission.30 34 While pain management was identified as a particular challenge for this group, only four publications explored this, suggesting evidence to understand the impact of inadequate pain management on treatment outcomes in children with ID is warranted.
Broad assumptions on the utility of safe and equitable care for children with ID were also found.23 24 26 28 This suggests that HCWs infrequently recognise that children with ID have unique care needs during hospitalisation to ensure safe quality of care.31 33 There is evidence of reliance on parental presence to care, advocate and speak for their child31–33 35, and parents were often relied on to assess their child’s pain.26 30 This reliance infers that parents and hospital staff share anxieties about the child with ID being left alone, unprotected, in the hospital environment.31 Exploration into how beliefs and values held by HCW and parents around healthcare Q&S for children with ID influence the experience of care quality is another area of potential future study.
The paucity of research into the hospital experience of iatrogenic harms poses a challenge to reducing health inequities for children with ID. Many papers excluded from this review reported on the frequency of hospitalisations, healthcare utilisation, length of stay and/or complexity of healthcare needs for the child with ID,36–43 but did not report on the influence of healthcare Q&S on these factors. The experience of iatrogenic harms for children with ID in different contexts, such as hospitalisation for Mental Health treatment, primary care and/or outpatient treatment, and day only treatment, is particularly lacking. Furthermore, how the experience of hospitalisation may vary according to severity of ID is not explored in any of the included papers and is an emerging area of interest.44
While individual teams and disciplines have devised various interventions to mitigate the believed perils of hospitalisation, QI interventions and policy changes that are not evidence-informed may ultimately fail to improve, or even possibly worsen, the problems they are designed to address.45 Without a clear picture and scale of the problem, policy-makers and healthcare leaders are ill equipped to mandate change.
Globally, partnerships with consumers to optimise healthcare Q&S, improve patient outcomes and reduce healthcare costs are increasing,2 4 which is strengthened by international recommendations for HCW training in patient engagement.46 The study findings complement this shift, indicating that training HCWs to partner with families of children with ID in planning and implementing their healthcare can have a positive impact on the care quality experience.33 This could be integrated into formal clinical training programme for health professionals, and into standard healthcare organisational training, guidelines and policies. Healthcare organisations can also support Q&S research and interventions that apply principles of experience-based co-design to facilitate HCW partnerships with consumers.47
Limitations
While the study population of interest was all children with ID, 9 of the 12 publications were specific to children with DS. While findings were consistent across the DS and non-DS publications, the emphasis on DS may reduce the generalisability of the findings for all ID conditions. The search strategy may have omitted some relevant publications, particularly due to variations in the definition of ID. For example, publications that referred to children with complex medical conditions but not explicitly ID were excluded from this review. Future reviews in this area could consider search strategies that specify terms for common conditions or syndromes.
A limitation of this review is the exclusion of non-English language studies. However, studies from six countries were included, traversing North America, the UK, Asia and Continental Europe. The identification of consistent themes across studies from these regions indicates that the findings are likely to be generalisable to the experiences of children with ID in hospital across a broad range of contexts.
Conclusion
The published literature indicates that the vulnerability of children with ID increases their likelihood of experiencing poor quality care and iatrogenic harm during hospitalisation, impacting treatment outcomes. By listening to parents to learn about the child and their ID, HCWs and organisations can tailor healthcare delivery and the hospital environment to reduce or mitigate iatrogenic harm and AEs, optimising treatment outcomes. Ensuring HCWs are knowledgeable about the children they care for and their ID is critical to achieving greater equity for this group. Partnering with families of children with ID in planning and implementing their care needs during hospitalisation is therefore important. Embedding patient engagement principles across clinical training programmes, healthcare policy and practice may enable and upskill HCWs to ensure a positive care quality experience for all children during hospitalisation.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge Professor Joanne Travaglia for the suggestion to conduct this review.
Footnotes
Contributors: LM and RHi conceived and designed the study. LM searched the literature, screened abstracts and full-text, extracted the data. All named authors contributed to the thematic data analysis, drafting manuscripts and have approved the final manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.United Nations. Universal declaration of human rights. Geneva, 1948. [Google Scholar]
- 2.National Patient Safety Foundation. Free from harm: accelerating patient safety improvement fifteen years after to err is human. Boston: NPSF, 2015. [Google Scholar]
- 3.Taitz J. Building a culture of safety in pediatrics and child health. Curr Treat Options Pediatr 2015;1:253–61. doi:10.1007/s40746-015-0032-6 [Google Scholar]
- 4.Yu A, Flott K, Chainani N, et al. . Patient safety 2030. London, UK: Imperial Patient Safety Translational Research Centre, 2016. [Google Scholar]
- 5.James JT. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf 2013;9:122–8. doi:10.1097/PTS.0b013e3182948a69 [DOI] [PubMed] [Google Scholar]
- 6.Matlow AG, Baker GR, Flintoft V, et al. . Adverse events among children in Canadian hospitals: the Canadian Paediatric Adverse Events Study. CMAJ 2012;184:E709–18. doi:10.1503/cmaj.112153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chapman SM, Fitzsimons J, Davey N, et al. . Prevalence and severity of patient harm in a sample of UK-hospitalised children detected by the Paediatric Trigger Tool. BMJ Open 2014;4:e005066 doi:10.1136/bmjopen-2014-005066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kirkendall ES, Kloppenborg E, Papp J, et al. . Measuring adverse events and levels of harm in pediatric inpatients with the Global Trigger Tool. Pediatrics 2012;130:e1206–14. doi:10.1542/peds.2012-0179 [DOI] [PubMed] [Google Scholar]
- 9.Heslop P, Blair PS, Fleming P, et al. . The confidential inquiry into premature deaths of people with intellectual disabilities in the UK: a population-based study. Lancet 2014;383:889–95. doi:10.1016/S0140-6736(13)62026-7 [DOI] [PubMed] [Google Scholar]
- 10.Trollor J, Srasuebkul P, Xu H, et al. . Cause of death and potentially avoidable deaths in Australian adults with intellectual disability using retrospective linked data. BMJ Open 2017;7:e013489 doi:10.1136/bmjopen-2016-013489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iacono T, Bigby C, Unsworth C, et al. . A systematic review of hospital experiences of people with intellectual disability. BMC Health Serv Res 2014;14:505 doi:10.1186/s12913-014-0505-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tuffrey-Wijne I, Goulding L, Gordon V, et al. . The challenges in monitoring and preventing patient safety incidents for people with intellectual disabilities in NHS acute hospitals: evidence from a mixed-methods study. BMC Health Serv Res 2014;14:432 doi:10.1186/1472-6963-14-432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ouellette-Kuntz H. Understanding health disparities and inequities faced by individuals with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities 2005;18:113–21. doi:10.1111/j.1468-3148.2005.00240.x [Google Scholar]
- 14.Khan A, Furtak SL, Melvin P, et al. . Parent-reported errors and adverse events in hospitalized children. JAMA Pediatr 2016;170:e154608 doi:10.1001/jamapediatrics.2015.4608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liberati A, Altman DG, Tetzlaff J, et al. . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100 doi:10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.United Nations. United Nations convention on the rights of the child: United Nations, 1990. [Google Scholar]
- 17.Sirriyeh R, Lawton R, Gardner P, et al. . Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract 2012;18:746–52. doi:10.1111/j.1365-2753.2011.01662.x [DOI] [PubMed] [Google Scholar]
- 18.Popay J, Roberts H, Sowden A, et al. . Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods programme. 2006. https://www.researchgate.net/profile/Lisa_Arai/publication/242311393_Guidance_on_the_conduct_of_narrative_synthesis_in_systematic_reviews_a_comparison_of_guidance-led_narrative_synthesis_versus_meta-analysis/links/5532159f0cf2f2a588ad67fd.pdf
- 19.Dixon-Woods M, Agarwal S, Jones D, et al. . Synthesising qualitative and quantitative evidence: a review of possible methods. J Health Serv Res Policy 2005;10:45–53. doi:10.1177/135581960501000110 [DOI] [PubMed] [Google Scholar]
- 20.Atz AM, Hawkins JA, Lu M, et al. . Surgical management of complete atrioventricular septal defect: associations with surgical technique, age, and trisomy 21. J Thorac Cardiovasc Surg 2011;141:1371–9. doi:10.1016/j.jtcvs.2010.08.093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Desai AR, Branco RG, Comitis GA, et al. . Early postoperative outcomes following surgical repair of complete atrioventricular septal defects: is down syndrome a risk factor? Pediatr Crit Care Med 2014;15:35–41. doi:10.1097/PCC.0000000000000004 [DOI] [PubMed] [Google Scholar]
- 22.Furukawa T, Park IS, Yoshikawa T, et al. . Outcome of univentricular repair in patients with Down syndrome. J Thorac Cardiovasc Surg 2013;146:1349–52. doi:10.1016/j.jtcvs.2013.02.017 [DOI] [PubMed] [Google Scholar]
- 23.Fudge JC, Li S, Jaggers J, et al. . Congenital heart surgery outcomes in Down syndrome: analysis of a national clinical database. Pediatrics 2010;126:315–22. doi:10.1542/peds.2009-3245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gupta P, Gossett JM, Rycus PT, et al. . Extracorporeal membrane oxygenation in children with heart disease and down syndrome: a multicenter analysis. Pediatr Cardiol 2014;35:1421–8. doi:10.1007/s00246-014-0945-z [DOI] [PubMed] [Google Scholar]
- 25.Lal PS, Chavan B, Devendran VR, et al. . Surgical outcome of congenital heart disease in Down’s syndrome. Asian Cardiovasc Thorac Ann 2013;21:166–9. doi:10.1177/0218492312450701 [DOI] [PubMed] [Google Scholar]
- 26.Graham RJ, Wachendorf MT, Burns JP, et al. . Successful and safe delivery of anesthesia and perioperative care for children with complex special health care needs. J Clin Anesth 2009;21:165–72. doi:10.1016/j.jclinane.2008.06.033 [DOI] [PubMed] [Google Scholar]
- 27.Valkenburg AJ, van Dijk M, de Leeuw TG, et al. . Anaesthesia and postoperative analgesia in surgical neonates with or without Down’s syndrome: is it really different? Br J Anaesth 2012;108:295–301. doi:10.1093/bja/aer421 [DOI] [PubMed] [Google Scholar]
- 28.Morabito A, Lall A, Gull S, et al. . The impact of Down’s syndrome on the immediate and long-term outcomes of children with Hirschsprung’s disease. Pediatr Surg Int 2006;22:179–81. doi:10.1007/s00383-005-1617-0 [DOI] [PubMed] [Google Scholar]
- 29.Travassos D, van Herwaarden-Lindeboom M, van der Zee DC. Hirschsprung’s disease in children with Down syndrome: a comparative study. Eur J Pediatr Surg 2011;21:220–3. doi:10.1055/s-0031-1271735 [DOI] [PubMed] [Google Scholar]
- 30.Malviya S, Voepel-Lewis T, Tait AR, et al. . Pain management in children with and without cognitive impairment following spine fusion surgery. Paediatr Anaesth 2001;11:453–8. doi:10.1046/j.1460-9592.2001.00686.x [DOI] [PubMed] [Google Scholar]
- 31.Brown FJ, Guvenir J. The experiences of children with learning disablilities, their carers and staff during a hospital admission. Br J Learn Disabil 2009;37:110–5. doi:10.1111/j.1468-3156.2008.00522.x [Google Scholar]
- 32.Aston M, Breau L, MacLeod E. Diagnoses, labels and stereotypes: supporting children with intellectual disabilities in the hospital. J Intellect Disabil 2014;18:291–304. doi:10.1177/1744629514552151 [DOI] [PubMed] [Google Scholar]
- 33.Pratt K, Baird G, Gringras P. Ensuring successful admission to hospital for young people with learning difficulties, autism and challenging behaviour: a continuous quality improvement and change management programme. Child Care Health Dev 2012;38:789–97. doi:10.1111/j.1365-2214.2011.01335.x [DOI] [PubMed] [Google Scholar]
- 34.Van Driest SL, Shah A, Marshall MD, et al. . Opioid use after cardiac surgery in children with Down syndrome. Pediatr Crit Care Med 2013;14:862–8. doi:10.1097/PCC.0b013e31829f5d9d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Croot EJ. The care needs of Pakistani families caring for disabled children: how relevant is cultural competence? Physiotherapy 2012;98:351–6. doi:10.1016/j.physio.2011.05.001 [DOI] [PubMed] [Google Scholar]
- 36.Zachariah P, Ruttenber M, Simões EA. Down syndrome and hospitalizations due to respiratory syncytial virus: a population-based study. J Pediatr 2012;160:827–31. doi:10.1016/j.jpeds.2011.11.004 [DOI] [PubMed] [Google Scholar]
- 37.Williams K, Leonard H, Tursan d’Espaignet E, et al. . Hospitalisations from birth to 5 years in a population cohort of Western Australian children with intellectual disability. Arch Dis Child 2005;90:1243–8. doi:10.1136/adc.2004.062422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.So SA, Urbano RC, Hodapp RM. Hospitalizations of infants and young children with Down syndrome: evidence from inpatient person-records from a statewide administrative database. J Intellect Disabil Res 2007;51(Pt 12):1030–8. doi:10.1111/j.1365-2788.2007.01013.x [DOI] [PubMed] [Google Scholar]
- 39.Nicholson CE. Pediatric critical care for children with congenital neurodevelopmental diagnoses. Pediatr Crit Care Med 2004;5:407–8. doi:10.1097/01.PCC.0000131863.08087.74 [DOI] [PubMed] [Google Scholar]
- 40.Mestrović J, Kardum G, Polić B, et al. . The influence of chronic health conditions on susceptibility to severe acute illness of children treated in PICU. Eur J Pediatr 2006;165:526–9. doi:10.1007/s00431-006-0114-3 [DOI] [PubMed] [Google Scholar]
- 41.Graham RJ, Dumas HM, O’Brien JE, et al. . Congenital neurodevelopmental diagnoses and an intensive care unit: defining a population. Pediatr Crit Care Med 2004;5:321–8. doi:10.1097/01.PCC.0000128892.38431.2B [DOI] [PubMed] [Google Scholar]
- 42.Frid C, Annerén G, Rasmussen F, et al. . Utilization of medical care among children with Down’s syndrome. J Intellect Disabil Res 2002;46(Pt 4):310–7. doi:10.1046/j.1365-2788.2002.00392.x [DOI] [PubMed] [Google Scholar]
- 43.Gallaher MM, Christakis DA, Connell FA. Health care use by children diagnosed as having developmental delay. Arch Pediatr Adolesc Med 2002;156:246–51. doi:10.1001/archpedi.156.3.246 [DOI] [PubMed] [Google Scholar]
- 44.Seliner B, Latal B, Spirig R. When children with profound multiple disabilities are hospitalized: a cross-sectional survey of parental burden of care, quality of life of parents and their hospitalized children, and satisfaction with family-centered care. J Spec Pediatr Nurs 2016;21:147–57. doi:10.1111/jspn.12150 [DOI] [PubMed] [Google Scholar]
- 45.Chalmers I. Trying to do more good than harm in policy and practice: the role of rigorous, transparent, up-to-date evaluations. Ann Am Acad Pol Soc Sci 2003;589:22–40. doi:10.1177/0002716203254762 [Google Scholar]
- 46.World Health Organization. WHO patient safety. Patient safety curriculum guide: multi-professional edition. Geneva: WHO, 2011:272. [Google Scholar]
- 47.Donetto S, Tsianakas V, Robert G. Using Experience-based Co-design (EBCD) to improve the quality of healthcare: mapping where we are now and establishing future directions London: King’s College London, 2014. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2017-000201supp002.pdf (69.8KB, pdf)
bmjpo-2017-000201supp001.pdf (523.3KB, pdf)
bmjpo-2017-000201supp003.pdf (421.2KB, pdf)


