Abstract
Objective
Disorders in sex development (DSD) can be treated well medically, but families will encounter many psychosocial challenges. Promoting counselling to facilitate acceptance and coping is important yet equality of access is unknown. This study investigated the modalities of psychosocial care provided in centres of DSD care.
Methods
An international survey conducted among 93 providers of psychosocial care, identified through clinical networks, registries and professional forums.
Results
Forty-six respondents from 22 different countries filled out the survey (49%). Most respondents (78%) were based in hospital-based expert teams. Referrals came from paediatric endocrinologists (76%), gynaecologists (39%) and paediatric urologists (37%). Psychological counselling was most frequently given to parents (74%), followed by children (39%), adolescents (37%) and adults (11%) and was most frequently focused on coping and acceptance of DSD (54%), education (52%), the atypical body (39%) and genital (41%), decisions on genital surgery (33%), complications with sexual intercourse (29%), disclosure (28%) and acceptance of infertility (11%). Respondents most frequently observed DSD related confusion about gender (54%), acceptance of cross gender behaviour (50%), anxiety (43%) and sadness and depression (38%).
Conclusions
Most psychosocial care is provided to parents. It is assumed that parental support is important as acceptance is conditional to become affectionate caretakers. Although it may be more difficult for youngsters to communicate about their condition and treatment, providing opportunity to bring up issues that are important for them, is imperative. Clinicians and parents should be aware that parental and patients’ interests may not correspond completely. Psychosocial management should also include transition and adult care.
Keywords: Clinical networks, Disorders of sex development, Multidisciplinary team, Rare diseases, Psychosocial care
What is known about the subject.
Diagnosis of DSD has a great psychological impact on patients and their parents.
Coping with DSD comprises coping with intersexuality, atypical genital appearance and function, infertility, gender atypicality in behavior and sexual orientation and misunderstandings about the condition.
Guidelines for clinical care endorse counseling, but support and advocacy groups point out that services are sparsely provided.
What this study adds.
This survey on the service offered by providers of psychosocial care revealed a focus on parental support
Issues regarding sexual functioning with genital atypicality, infertility and inability to meet some social expectations receive little attention
An extension to the needs of adolescents and adults is discussed
Introduction
Disorders in sex development (DSD)) refer to a group of congenital conditions characterised by incongruence in the chromosomal, gonadal and anatomical sex.1 2 In children with atypically developed external genitalia, DSD will be mostly identified at birth. In children born with genitalia that have a typical male or female appearance, DSD will be identified later in life, in most cases because of an atypical development in puberty.
Most types of DSD do not involve life-threatening diseases, and pathology can be treated well. Identification of DSD, however, can be a traumatic experience.3 In children born with atypical genitalia, it may be necessary to postpone assignment of gender until a (preliminary) diagnosis has been reached. For parents, the delay in establishing a fundamental component of the child’s identity can be an extremely stressful event. The findings of the diagnostic procedures will require additional demands. By sharing results, professionals and parents can discuss the infant's gender and surgical options. Some parents prefer to delay gender assignment and/or surgical decision making, but deciding to delay is also an active decision. In addition, parents need to decide on disclosure of their child’s condition to family and friends. Such demands can be extremely distressing, particularly in case parents do not immediately comprehend the child’s condition and lack overview of the consequences of decisions.3–9 Identification of DSD later in life is often preceded by worries related to an atypical development in puberty, such as a delay of puberty, cease of continuation or development of bodily changes of the other gender. Such changes are puzzling and may lead to sadness, disgust of the own body, shame and social fear. In adolescents, it can be shocking to learn that they have been born with DSD; they may have fundamental doubts about oneself and experience themselves differently than before. Parents may undergo similar feelings raising doubts and uncertainty about the child’s future opportunities. Often, time is needed to accommodate the self-concept to the recent medical findings.9–11
Coping with DSD, at any stage in life, remains challenging. Most individuals with DSD have to cope with atypical genitalia and subinfertility or infertility. Due to a wider social unawareness of DSD and misunderstandings, individuals with DSD may be confronted with insensitive reactions and social stigmatisation. Children, adolescents and adults with DSD may prefer atypical or cross-gender role behaviour and activities; sometimes they are criticised for these preferences. The atypical appearance of the body and genitalia requires self-confidence to enter romantic relationships. Young people need to build confidence in exploring their sexual self before they will be able to make necessary adjustments in love making.9–15 In communities, cultures or religions that expect procreation, individuals who are subinfertile or infertile will be less valued as spouses. Being unmarried may involve an unfavourable social position.16
In meeting these challenges, many individuals with DSD and their parents need help.3–18 Basic thought for medical and psychosocial care is that the individual with DSD will be accepted and will have optimal chances for self-actualisation and for social participation in childhood, adolescence and adulthood. Against a backdrop of variation across countries, providers and professional roles, we wanted to understand how psychosocial care for these individuals happens. Therefore, a survey, developed to examine practice and understand research priorities, was distributed to psychosocial caregivers working in centres that deliver specialist care for children and adults with DSD.
Materials and methods
Design
Web-based survey among psychosocial caregivers with expertise in DSD.
Participants
Professional caregivers involved in psychosocial care for individuals with DSD were included. Names and email addresses of 93 potential respondents were obtained from multiple sources related to DSD, including from a previous survey19 held among paediatric endocrinologists who were registered clinical users of the I-DSD Registry or members of DSDnet,20 21 from the European Network for Psychosocial Studies in Intersex/Diverse Sex Development (EuroPsi22) and from the Pediatric Psychology Network (PPN23).
Measure
The survey consisted of 63 questions with preset answer categories on professional training, working setting, collaboration with other professionals, patients, types of professional activities and a few open-ended questions that asked the respondents to share their ideas regarding good psychosocial practice for individuals with DSD and expertise that should be developed in the future. The survey took about 20 min to complete. For some questions only one response could be given, other questions allowed for multiple responses.
Procedure
The survey was open between 23 September and 23 December 2015. Personalised emails with a reference link to the survey were sent to all potential participants; non-responders received two reminders. Collected data were automatically stored in a database file and made ready for statistical analysis. The database was protected by password and only accessible for researchers.
Statistical analyses
All categorical data were analysed by descriptive statistics, cross-tabulation and χ2 test using IBM SPSS V.22. Qualitative data were analysed by text analysis, conducted by two researchers.
Results
Response rate and respondents’ characteristics
Forty-six respondents from 22 countries completed the survey (response rate 49%). Respondents were based in Europe and adjacent Mediterranean countries (88%), North and South America (10%) and Asia (2%). They were trained in psychiatry (n=3), psychology (n=27), as nurse specialists (n=6), social workers (n=3), religious workers (n=3) and teachers (n=2). All respondents had obtained at least a bachelor’s degree, 54% had completed advanced or postgraduate training and obtained registrations in professional or governmental registries. Most respondents (76%) had attended a specific course, training or a conference on DSD in the past 3 years, and 56% were involved in training courses on DSD.
Almost all respondents (87%) indicated they were working in or collaborating with a team of professionals specialised in DSD care. Most respondents were based in hospital-based expert teams (78%), 22% of respondents were working in other clinics, centres or private practices and collaborated with medical doctors with expertise in DSD working in other hospitals and 15% of respondents were working in both settings. Compared with non-hospital based respondents, hospital-based respondents were available at short notice (χ2=11.276, df=2 p=0.004). In addition to psychosocial care, 50% of respondents reported involvement in DSD-related research (see table 1 for details of respondents’ characteristics).
Table 1.
Respondents’ characteristics
| Location | Europe | 80% |
| Mediterranean area outside Europe | 8% | |
| North and South America | 10% | |
| Asia | 2% | |
| Education | Bachelor’s degree | 100% |
| Master’s degree | 32% | |
| Postgraduate/advanced training | 54% | |
| Registration in national registry | 67% | |
| Supplementary training on DSD | 76% | |
| Membership professional association | 58% | |
| Clinical setting | Hospital-based DSD team | 78% |
| Non-hospital based—referrals from DSD-specialised clinicians | 22% | |
| Hospital and non-hospital based | 15% |
Involvement in clinical care
Referrals for psychosocial counselling came from paediatric endocrinologists (76%), gynaecologists (39%), paediatric urologists (37%), paediatricians (37%), endocrinologists (30%) and clinical geneticists (28%). Approximately 20% of referrals came from other disciplines (eg, neonatologists and paediatric surgeons).
Professional activities
Most counselling was provided to parents (74%), followed by counselling of children (39%), adolescents (37%) and adults (11%) (see figure 1).
Figure 1.
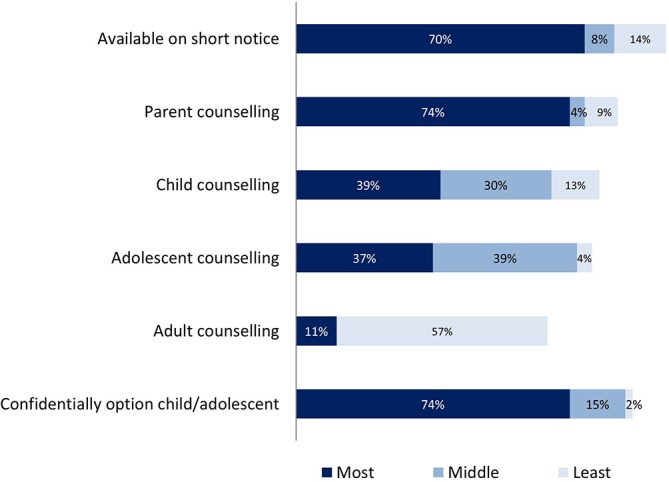
Involvement in clinical care.
Care focused on patients diagnosed with 46,XX DSD (74%), 46,XY DSD (59%) and chromosomal DSD (59%), but care for patients born with an atypical development of the genitalia—not related to DSD (59%)—and patients born with severe anatomic anomalies of the abdomen such as malformations of the urinary tract and cloacal malformations (54%) were also reported. Patients with Turner and Klinefelter syndromes were least frequently referred (41% and 52% of referrals, respectively).
Psychosocial counselling primarily focused on coping and acceptance of DSD, education on psychological aspects of DSD, information on disclosure among family and friends and on coping and acceptance of infertility is represented in figure 2.
Figure 2.
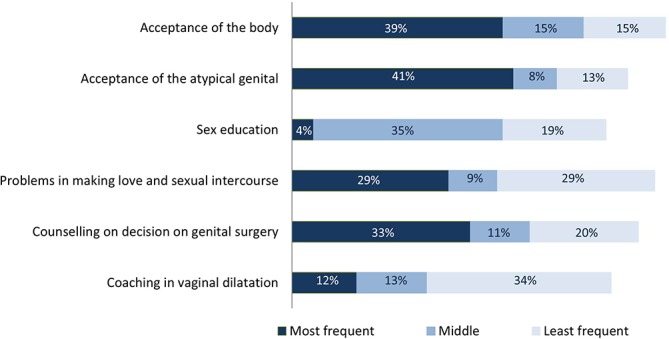
Counselling activities.
Respondents were asked about frequency of utilised resources of information. The the most common included web-based resources (50%), information leaflets (37%) and books (30%). Information on support groups was provided more often (56%) than group facilitation (17%). Fifty-six per cent of respondents reported at least one support group active in their country, but 32% respondents were not aware about a national support group (12% had not responded).
Respondents were asked to report the emotional problems related to DSD they most frequently observed among referred individuals (see figure 3).
Figure 3.
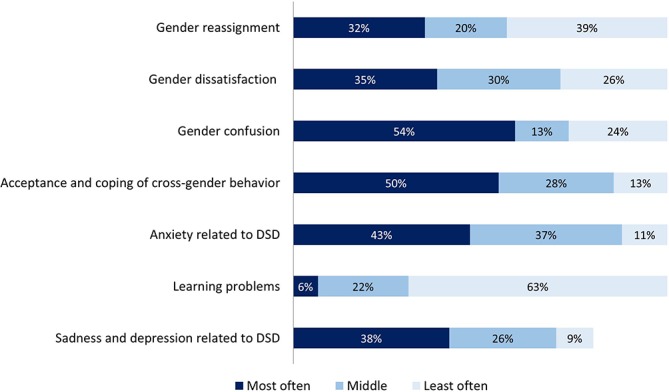
Types of adjustment problems in DSD.
Most psychosocial caregivers collaborated with a psychiatry department, a psychiatrist or were trained in psychiatry (76%). Only seven respondents indicated they did not do so, and another four respondents had not completed this question. From a list of 19 services in psychosocial management, respondents were asked to prioritise five services they valued most. We observed high agreement regarding prioritised services: individual counselling and therapy (19%), helping individuals and parents in making decisions (19%), promoting resilience (19%), preventive group work (15%) and their professional contribution to the multidisciplinary team (28%).
Consultation was also provided regarding acceptance of the atypical body and genitalia, counselling regarding decision making on genital surgery and sexual intercourse. Coaching in vaginal dilation and sex education were least requested (see figure 4). Only 33% of the providers of psychosocial care collaborated with a sex therapist or were trained as a sex therapist themselves.
Figure 4.
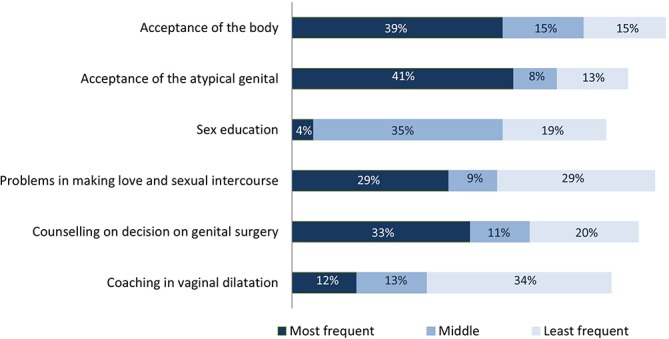
Provided care regarding body atypicality and sexuality.
Furthermore, participants indicated that long-term case management could be improved as well as communication between the members of their own team.
Discussion
The consensus statement1 2 made clear that standardisation is conditional for future development of clinical management in DSD. Related guideline documents promote an integrated, interdisciplinary healthcare team that includes qualified mental health providers.2 24 In the process to develop standards, several surveys among professionals have been conducted.19 25–27 From the survey, we learnt that professionals working in psychosocial care are less well organised than medical professionals and there is variation within disciplines, training and clinical settings. Most respondents were based in hospital-based expert teams. Those who were not hospital based, collaborated with medical professionals specialised in DSD care. Since most referrals were generated from paediatric endocrinologists, it is reassuring to note well-established collaboration between psychosocial providers and medical specialty teams exist. Most hospital-based psychosocial caregivers were available at short notice. Availability without delay is important; identification of DSD can be a shocking experience for the parents3 as well as the adolescent who is able to comprehend the implications of the diagnosis. The diagnosis, often difficult to understand well immediately, will raise many questions and uncertainties. Availability of professional counselling with minimal delay will be helpful for patients or parents to regain grip and will restore confidence in the situation.
The majority of responders provided psychosocial care to parents. Particularly in the first period after diagnosis, parents will need counselling to comprehend and cope with the condition. By supporting parents well in this first intensive period, parents will likely become able to support their own child. Confidential counselling for children and adolescents is valued since children and youth may experience difficulties to discuss delicate matters regarding gender, identity and sexuality with their parents.
Counselling was focused on providing information in helping to understand DSD and its implications, coping and acceptance and information on disclosure. Most activities were focused on patients with 46,XX, 46,XY and chromosomal DSD, but consultation was also provided to parents and children with other rare anomalies of the genitalia and abdomen.
Children with Turner and Klinefelter syndromes were least frequently seen. As these syndromes are most prevalent among all types of DSD, with prevalence of 1:4500 (Turner syndrome28) and 1:500 (Klinefelter syndrome29), it seems likely that children and adolescents with these syndromes and their parents more often will be referred to other psychosocial caregivers with expertise in the neurocognitive problems more frequently observed in these children.
Confusion about gender and coping with cross-gender role behaviour were frequently reported resulting in emotional problems and challenges. Additionally, DSD-related anxiety and depression were also frequently seen in services. Regarding the high frequency of gender dissatisfaction, collaboration with a psychiatrist is recommended. Only a minority of the respondents collaborated with a sex therapist. Most consultations on this issue were on coping with the atypical genitalia and decision making on genital surgery, but colleagues were also consulted for questions regarding sexual functioning. Collaboration with a sex therapist, and development of expertise on sexual issues among psychosocial caregivers in DSD, is important.
This survey has several shortcomings. As psychosocial caregivers are not organised well, many respondents were traced by email addresses obtained from a survey carried out among paediatric endocrinologists who were registered clinical users of the I-DSD Registry or members of DSDnet. By this strategy, we selected providers of psychosocial care who collaborate with paediatricians and who are working in specialised teams. We may have invited the vast majority of the available colleagues, but we may have not identified an important number of psychosocial caregivers who are only involved in adult care or psychosocial caregivers who do not wish to collaborate with medical professionals. Despite repeated requests to complete the survey, half of all colleagues did not respond. Language of the survey was English. Non-respondents may have had insufficient knowledge of the language to respond to the questionnaire. Consequently, our findings may not be representative. Furthermore, respondents were able to skip questions while responding to the survey. Consequently, we were left with incomplete surveys. Despite providing free text or narrative space, few respondents provided feedback about their service, education or research needs.
The survey among professionals from different nations worldwide who are involved in psychosocial care is original and provides a platform for growth. It is well recognised that individuals with DSD and their parents face many psychological and psychosocial challenges in life, and psychosocial consultation is valued highly, both by clinicians and by members from support groups.1–18 As DSD are rare conditions, the number of colleagues with expertise in providing psychosocial care is limited; publications on content of psychosocial care, such as themes in counselling and type of interventions, are scarce.9 15 17 Our survey revealed a large variety between providers’ training, background and position in the DSD team; standardisation in the development of psychosocial care only recently came under attention.15 Nevertheless, we observed high agreement among respondents in priority of services in psychosocial management. Combined with research publications,9 15 17 we think that this survey can be the start for development of standards of psychosocial care in DSD.
A few respondents also provided consultation to adults. Adults with DSD may have less access for psychosocial care than children, adolescents and their parents. Sexual dysfunctions and sadness regarding infertility are frequently reported.30–37 In the past 25 years, adults with DSD became organised in support groups. These groups became very successful in ending the isolated position of individuals with DSD and raising awareness that necessary changes in medical practice are possible. These groups also became successful in setting the agenda for improvement of clinical practice. However, members of support groups cannot and should not fulfil the role of the professional caretaker.
Medical professionals are working hard to develop standards of care for individuals with DSD. Availability for psychosocial care should be included. From this survey, we learnt that psychosocial care is focused on parental help, for children and adolescents. We assume that psychosocial management should also include adult care. Sexual problems, confusion about gender or gender dysphoria are probably more frequently seen in late adolescence and early adulthood. The providers of help for DSD were all mainly based in paediatric service, and we think children will benefit from collaboration with gynaecology and urology. A greater focus for acceptance of the atypical genitalia, sex education, how to discuss sexual issues with your child (parents) and with your lover (patients) in combination with reinforcement of coping capacities and resilience is needed. Professionals in psychosocial care should be trained in discussing sexological issues.
Acknowledgments
The authors would like to thank all professionals in psychosocial care who have been willing to fill out the survey and share their experiences, knowledge and ideas with us.
Footnotes
Contributors: AD designed the study, including development of the first draft of the questionnaire; distributed the questionnaire to the surveyed clinicians; and received and collected the responses; analysed and interpreted the data; drafted the initial manuscript; and approved the final manuscript as submitted. GGF, AK, JB, CS, MR and VI reviewed and revised the first draft of the questionnaire. GGF compiled the survey into a web-based tool (Google forms). GGF and AK reviewed and revised the first draft of the initial manuscript. GGF, AK, JB, CS, AN, MR, VI, AE, AJ, MK and OH reviewed and approved the final manuscript as submitted. SFA initiated the project and provided overall supervision of the study from conception to completion; reviewed and revised the initial questionnaire and manuscript; approved the final manuscript as submitted; and acts as the guarantor.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: We do not wish to share data originating from our database in order to protect the anonymity of subjects included in this survey. Permission has not been obtained to share data widely with other investigators and would require individual content/assent.
References
- 1. Hughes IA, Houk C, Ahmed SF, et al. Consensus statement on management of intersex disorders. Arch Dis Child 2006;91:554–63. doi:10.1136/adc.2006.098319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lee PA, Nordenström A, Houk CP, et al. Global Disorders of sex development Update since 2006: perceptions, approach and care. Horm Res Paediatr 2016;85:158–80. doi:10.1159/000442975 [DOI] [PubMed] [Google Scholar]
- 3. Pasterski V, Mastroyannopoulou K, Wright D, et al. Predictors of posttraumatic stress in parents of children diagnosed with a disorder of sex development. Arch Sex Behav 2014;43:369–75. doi:10.1007/s10508-013-0196-8 [DOI] [PubMed] [Google Scholar]
- 4. Sanders C, Carter B, Goodacre L. Searching for harmony: parents' narratives about their child's genital ambiguity and reconstructive genital surgeries in childhood. J Adv Nurs 2011;67:2220–30. doi:10.1111/j.1365-2648.2011.05617.x [DOI] [PubMed] [Google Scholar]
- 5. Sanders C, Carter B, Goodacre L. Parents need to protect: influences, risks and tensions for parents of prepubertal children born with ambiguous genitalia. J Clin Nurs 2012;21(21-22):3315–23. doi:10.1111/j.1365-2702.2012.04109.x [DOI] [PubMed] [Google Scholar]
- 6. Wisniewski AB, Sandberg DE. Parenting children with disorders of sex development (DSD): A Developmental Perspective Beyond gender. Horm Metab Res 2015;47:375 doi:10.1055/s-0034-1398561 [DOI] [PubMed] [Google Scholar]
- 7. Siminoff LA, Sandberg DE. Promoting shared Decision making in disorders of sex development (DSD): Decision aids and support tools. Horm Metab Res 2015;47:335–9. doi:10.1055/s-0035-1545302 [DOI] [PubMed] [Google Scholar]
- 8. Wolfe-Christensen C, Wisniewski AB, Mullins AJ, et al. Changes in levels of parental distress after their child with atypical genitalia undergoes genitoplasty. J Pediatr Urol 2017;13:e1-32.e6:32.e1–32.e6. doi:10.1016/j.jpurol.2016.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bennecke E, Werner-Rosen K, Thyen U, et al. Subjective need for psychological support (PsySupp) in parents of children and adolescents with disorders of sex development (dsd). Eur J Pediatr 2015;174:1287–97. doi:10.1007/s00431-015-2530-8 [DOI] [PubMed] [Google Scholar]
- 10. Sandberg DE, Gardner M, Callens N, et al. The DSD-TRN Advocacy Advisory Network, and Accord Alliance. Interdisciplinary care in disorders/differences of sex development (DSD): The psychosocial component of the DSD-Translational research network. Am J Med Genet C Semin Med Genet 2017;175:279–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liao LM, Tacconelli E, Wood D, et al. Adolescent girls with disorders of sex development: A needs analysis of transitional care. J Pediatr Urol 2010;6:609–13. doi:10.1016/j.jpurol.2010.07.006 [DOI] [PubMed] [Google Scholar]
- 12. Callens N, De Cuypere G, De Sutter P, et al. An update on surgical and non-surgical treatments for vaginal hypoplasia. Hum Reprod Update 2014;20 801:775–801. doi:10.1093/humupd/dmu024 [DOI] [PubMed] [Google Scholar]
- 13. Meyer-Bahlburg HF, Baratz Dalke K, Berenbaum SA, et al. Gender assignment, reassignment and outcome in disorders of sex development: update of the 2005 Consensus Conference. Horm Res Paediatr 2016;85:112–8. doi:10.1159/000442386 [DOI] [PubMed] [Google Scholar]
- 14. Nokoff NJ, Palmer B, Mullins AJ, et al. Prospective assessment of cosmesis before and after genital surgery. J Pediatr Urol 2016;5131:30279–0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wisniewski AB. Psychosocial implications of disorders of sex development treatment for parents. Curr Opin Urol 2017;27:11–13. doi:10.1097/MOU.0000000000000344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ediati A, Juniarto AZ, Birnie E, et al. Body image and sexuality in Indonesian adults with a disorder of sex development (DSD). J Sex Res 2015;52:15–29. doi:10.1080/00224499.2013.816260 [DOI] [PubMed] [Google Scholar]
- 17. Rolston AM, Gardner M, Vilain E, et al. Parental Reports of Stigma Associated with Child's Disorder of Sex Development. Int J Endocrinol 2015;2015:1–15. doi:10.1155/2015/980121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Neve-Enthoven NG, Callens N, van Kuyk M, et al. Psychosocial well-being in dutch adults with disorders of sex development. J Psychosom Res 2016;83:57–64. doi:10.1016/j.jpsychores.2016.03.005 [DOI] [PubMed] [Google Scholar]
- 19. Kyriakou A, Dessens A, Bryce J, et al. Current models of care for disorders of sex development - results from an International survey of specialist centres. Orphanet J Rare Dis 2016;11:155 doi:10.1186/s13023-016-0534-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. European Society for Paediatric Endocrinology (ESPE). https://www.eurospe.org/DSDworkinggroup.
- 21.DSDnet. www.dsdnet.eu
- 22.EuroPsi. www.europsi.org
- 23.Pediatric Psychology Network. www.bps.org.uk/networks-andcommunities/member-microsite/dcp-faculty-children-young-people-and-theirfamilies/paediatric-psychology-network and www.pediatrischepsychologie.nl
- 24. Ahmed SF, Achermann JC, Arlt W, et al. Society for Endocrinology UK guidance on the initial evaluation of an infant or an adolescent with a suspected disorder of sex development (Revised 2015). Clin Endocrinol 2016;84:771–88. doi:10.1111/cen.12857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pasterski V, Prentice P, Hughes IA. Consequences of the Chicago consensus on disorders of sex development (DSD): current practices in Europe. Arch Dis Child 2010;95:618–23. doi:10.1136/adc.2009.163840 [DOI] [PubMed] [Google Scholar]
- 26. Josso N, Audi L, Shaw G. Regional variations in the management of testicular or ovotesticular disorders of sex development. Sex Dev 2011;5:225–34. doi:10.1159/000334263 [DOI] [PubMed] [Google Scholar]
- 27. Rolston AM, Gardner M, van Leeuwen K, et al. Disorders of sex development (DSD): Clinical service delivery in the United States. Am J Med Genet C Semin Med Genet 2017;175:268–78. doi:10.1002/ajmg.c.31558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Prevalence Klinefelter syndrome worldwide. https://ghr.nlm.nih.gov/condition/klinefelter-syndrome#statistics.
- 29.Prevalence Turner syndrome worldwide. https://ghr.nlm.nih.gov/condition/turner-syndrome#statistics.
- 30. Krege S, Walz KH, Hauffa BP, et al. Long-term follow-up of female patients with congenital adrenal hyperplasia from 21-hydroxylase deficiency, with special emphasis on the results of vaginoplasty. BJU Int 2000;86:253–8. doi:10.1046/j.1464-410x.2000.00789.x [DOI] [PubMed] [Google Scholar]
- 31. Minto CL, Liao KL, Conway GS, et al. Sexual function in women with complete androgen insensitivity syndrome. Fertil Steril 2003;80:157–64. doi:10.1016/S0015-0282(03)00501-6 [DOI] [PubMed] [Google Scholar]
- 32. Minto CL, Liao LM, Woodhouse CR, et al. The effect of clitoral surgery on sexual outcome in individuals who have intersex conditions with ambiguous genitalia: a cross-sectional study. Lancet 2003;361:1252–7. doi:10.1016/S0140-6736(03)12980-7 [DOI] [PubMed] [Google Scholar]
- 33. Schonbucher V, Schweizer K, Richter-Appelt H. Sexual quality of life of individuals with disorders of sex development and a 46,XY karyotype: a review of international research. J Sex Marital Ther 2010;36:193–215. doi:10.1080/00926231003719574 [DOI] [PubMed] [Google Scholar]
- 34. Nordenström A, Frisén L, Falhammar H, et al. Sexual function and surgical outcome in women with congenital adrenal hyperplasia due to CYP21A2 deficiency: clinical perspective and the patients' perception. J Clin Endocrinol Metab 2010;95:3633–40. doi:10.1210/jc.2009-2639 [DOI] [PubMed] [Google Scholar]
- 35. Kleinemeier E, Jürgensen M, Lux A, et al. Psychological adjustment and sexual development of adolescents with disorders of sex development. J Adolesc Health 2010;47:463–71. [DOI] [PubMed] [Google Scholar]
- 36. van der Zwan YG, Janssen EH, Callens N, et al. Dutch Study Group on DSD. Severity of virilization is associated with cosmetic appearance and sexual function in women with congenital adrenal hyperplasia: a cross-sectional study. J Sex Med 2013;10:866–75. doi:10.1111/jsm.12028 [DOI] [PubMed] [Google Scholar]
- 37. van der Zwan YG, Callens N, van Kuppenveld J, et al. Long-term outcomes in males with disorders of sex development. J Urol 2013;190 42:1038-42. [DOI] [PubMed] [Google Scholar]


