Abstract
Trust in physicians has declined, and surveys of public opinion show a poor level of public trust in physicians. Commodification of health care has been speculated as a plausible driving force. We used cross-national data of 23 countries from the International Social Survey Programme 2011 to quantify health care commodification and study its role in the trust that patients generally place in physicians. A modified health care index was used to quantify health care commodification. There were 34 968 respondents. A question about the level of general trust in physicians and a 4-item “general trust in physicians” scale were used as our major and minor outcomes. The results were that compared with those in the reference countries, the respondents in the health care–commodified countries were approximately half as likely to trust physicians (odds ratio: 0.47, 95% confidence interval [CI]: 0.31-0.72) and scored 1.13 (95% CI: 1.89-0.37) less on the general trust scale. However, trust in physicians in the health care–decommodified countries did not differ from that in the reference countries. In conclusion, health care commodification may play a meaningful role in the deterioration of public trust in physicians.
Keywords: health care commodification, patient trust, multilevel, health care commercialization, surveys and questionnaires, trust, commodification
Background
There are 2 closely related concepts in patient trust—interpersonal trust in a specific physician and general trust in physicians.1 Patient trust in a specific physician is critical for maintaining favorable physician-patient relationship.2 Studies have shown that a higher degree of patient trust in a specific known physician may help patients to raise their self-care ability, to adhere to cancer screening or treatment, and to maintain healthy lifestyles.3-6 More importantly, a higher level of trust in patients’ medical providers is associated with superior patient outcomes such as more favorable long-term glycemic control and higher health-related quality of life, patient satisfaction, and fulfillment of medical needs.7-9 Besides, trust in physicians was also found to be positively associated with better shared decision making.10
Patients’ general trust in physicians theoretically contributes to elicit patients’ interpersonal trust in a specific physician on first acquaintance and to maintain that trust as the relationship develops. As Meyer et al pointed out based on the social theories of Giddens and Luhmann, patients’ general trust and interpersonal trust interact as a complex “web.”11 Empirically, patients’ general trust indeed correlates with trust in one’s physician, satisfaction with care, and better adherence to doctor recommendations.1
Trust is a methodological measurable construct, which showed a variation across countries.12,13 Although general trust in physicians plays a significant role in patient care, a substantial variation of public general trust in physicians was observed across countries and, in recent years, public trust in the medical profession has apparently declined.11,14 Commodification or commercialization of health care has been speculated as a plausible driving force.15 Of the 29 countries in one report, people in the United States had a relatively low level of public general trust in physicians14; the health care system in the United States is well known for its commodification.16-18 According to Mackintosh and Kovalev, health care commodification can be defined by 3 components: financing from individual payment or private insurance, production with the primary aim of cash income or profit, and distribution through the market according to the ability to pay.19 Although Mackintosh and Kovalev actually used the term “commercialization” when defining it, they also use “commodification” interchangeably to represent the same concept.20 In this article, we prefer to use “commodification” to follow the continuity of theories developed by Polanyi,21 Esping-Andersen,22 and Bambra.23 Therefore, it may be worthwhile to explore the relationship between commodification of health care and public general trust in physicians.
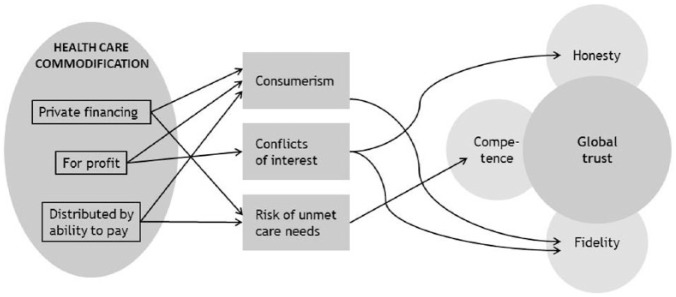
Health care commodification may compromise public general trust in physicians through 3 plausible mechanisms. The first is consumerism, which may transform the physician-patient relationship into a consumer-provider relationship based on self-interest and a market ethic rather than a professional ethic.16,24 According to the “appropriateness-identity-rules” theory of decision making developed by March and Messick, people make “business decisions” or “ethical decisions” on the basis of perceived social context.25-27 The consumer-provider context may lower patient trust in physicians. This mechanism is supported by 2 qualitative studies, which showed that patients without private health insurance waiting for public hospitals saw physicians through an “equity lens,” and did not distrust physicians.28 On the contrary, patients with private health insurance conceived of physicians as self-interested knaves.29 Another quantitative study showed that people with high medical cost burdens (who were prone to view their medical encounters as financial transactions) were less likely to trust their physician.30
The second mechanism is the financial conflicts of interest of medical providers. Financial conflicts of interest may erode patients’ trust in physicians’ fidelity and honesty. A profit-seeking nature of health care commodification may lead people in commodified systems having a greater doubt whether physicians would act for patients’ best interests.24,31 People may doubt whether physicians’ decision making and disclosure of treatment options are beneficent or for profit. Hence, even doctors themselves are increasingly uncomfortable with privatization of health care system because they believe that the chief motivation for private providers is profit but not beneficiary, according to a recent survey on British doctors.32 As health care expenditure increases rapidly, many countries adopt various cost containment strategies. Prospective or risk-sharing payment methods are a typical example. We hypothesized that financial conflicts of interest resulting from cost containment strategies such as prospective risk-sharing payment methods may be larger among more commodified systems than less commodified systems due to potentially stronger profit-seeking motivations in more commodified systems. Patients were shown to feel concern about physicians’ risk-sharing payment methods, especially when doctors can earn more by containing costs.33 More specifically, patients in managed care plans or whose physicians were reimbursed on a capitated basis had lower levels of trust in their physician relative to fee-for-service “indemnity.”34
The third mechanism is risk exposure of unmet health care needs, which was proposed by Cammett et al. Cammett et al revealed that a higher proportion of private health care financing results in lower trust in government, especially in low-income people. People with lower income have higher risk of unmet health care needs, and have negative opinions of health care systems.35 Cammett et al also found that low-income people living in countries with higher proportion of private health care financing (one component of commodification) have even higher risk of unmet health care needs than low-income people living in countries with lower proportion of private health care financing.35 Accordingly, health care commodification may increase the risk of unmet health care needs and reduce trust in physicians, especially for lower income individuals.
Based on the conceptual model proposed by Hall et al, general trust in physician has at least 4 overlapping domains: global trust, honesty, fidelity, and competence.1 Financial conflicts of interest, which are mainly produced by the profit-seeking component of health care commodification, may reduce patients’ trust in physicians’ fidelity and honesty. The conceptual framework of the interrelationship between health care commodification and general trust in physicians is illustrated in Figure 1.
Figure 1.
The conceptual framework to explain how commodification may affect multiple dimension of trust through 3 intermediate factors (consumerism, conflict of interest, and risk of unmet care needs).
In this study, we investigated the factors associated with people’s general trust in physicians and explored the influence of country-level health care commodification on people’s general trust in physicians by using the data of 23 upper-middle to high-income countries from the International Social Survey Programme (ISSP). Although as aforementioned, general trust and interpersonal trust interact as a complex web and thus correlate. They are both equally important. There are 2 reasons why we studied general trust instead of interpersonal trust. First, theoretically or intuitively, commodification is a macro-level construct which might have a greater and more direct influence on general trust than on interpersonal trust. Second, due to data limitations, we could only investigate the relationship between commodification and general trust but not interpersonal trust. Future researches with more rich data contents may help to contribute in this regard.
Methods
Study Design and Data Source
This was a multicountry cross-sectional secondary analysis of the individual survey data of ISSP 2011.36 Country-level data for quantifying health care commodification were obtained from the Organisation for Economic Co-operation and Development (OECD),37 Ministry of Health and Welfare of Taiwan,38 Eurostat,39 European Hospital and Healthcare Federation,40 Pharmaceutical Health Information System,41 and Farsi et al.42
Quantification of Health Care Commodification
We adopted the health care decommodification index developed by Bambra in 2005 to quantify the extent of health care commodification for each country. The index consists of 3 measures: private health expenditure as a percentage of gross domestic product (GDP), private hospital beds as a percentage of total bed stock, and the percentage of the public health care system coverage.43 The 3 measures were selected because they indicate the varied role of the market in a health care system through assessing the financing, provision, and coverage of the private sector.43 The definition of the public health system coverage is “the population receiving a core set of health care goods and services under public programmes . . . (which) refers both to government programmes, generally financed by taxation, and social health insurance, generally financed by payroll taxes.”44
To capture the concept of health care commodification more precisely, we modified this index by excluding expenditures of private social (compulsory) insurance and nonprofit institutions from private health expenditure, and nonprofit hospital beds from private hospital beds. We excluded expenditures of private social insurance because the traditional interpretation of “public” and “private” is not suitable for modern health care systems, which have a complex mix of public and private roles. As the System of Health Accounts 2011 framework proposed, it is preferable to interpret the terms “public” and “private” as “compulsory” and “voluntary” from a perspective of regulation.45
We excluded expenditures and hospital beds of nonprofit institutions because this modification made this index capture the core concept of commodification—profit-seeking—more precisely. The empirical analysis of US hospitals consistently showed that nonprofit hospitals differ in behavior from for-profit hospitals. Nonprofit hospitals have a more propensity to treat less profitable patients,46 and offer relatively unprofitable services.47,48 However, to avoid the suspicion of data manipulation, we also conducted a sensitivity analysis with the original index, and the results remained robust.
According to previous literatures,22,43 we constructed the health care commodification index and the scoring procedure. For each of the first 2 measures, the distribution of the percentages was divided into 3 categories, on the basis of 1 SD from the specific mean, which is adjusted by excluding the extreme outliers (the United States for private for-profit expenditure) when calculating the mean as Bambra’s scoring process.43 We defined the countries with percentage of private for-profit expenditure or beds above 1 SD from the mean as the countries with a high health care commodification level, and assigned a score of 1 to those countries. The countries with a percentage within 1 SD from the specific mean were defined as countries with a medium health care commodification level and were assigned a score of 2. The remaining countries with a percentage below 1 SD from the specific mean were defined as the countries with a low health care commodification level and were assigned a score of 3. Scores of measures 1 and 2 were then summed and multiplied by one-tenth of the percentage of measure 3; the result was defined as the health care index. The final index ranged from 0 to 60, with lower values representing greater health care commodification. Finally, according to each country’s index value, we categorized the countries into 3 types—health care–commodified, reference, and health care–decommodified countries—on the basis of standard deviation (adjusting for outliers) and mean. We believe that with a sufficient number of country observations, having 3 categories can provide more detailed information and allow an opportunity to show a dose response pattern if it exists. Besides, the 3-level categorization has an advantage of comparing our results with previous studies.
Outcomes
Based on the data from ISSP 2011,36 our major outcome was people’s trust in physicians, measured by the item “All things considered, doctors in [your country] can be trusted” on a 5-point Likert scale from strongly agree to strongly disagree.
To ensure a comprehensive measurement of trust in physicians, we used 4 additional items in the ISSP questionnaire (Table 1) to construct a trust scale. These 5 items were literally and conceptually compatible with both a validated 11-item scale (Cronbach’s α = 0.89) and a validated 5-item short version scale (Cronbach’s α = 0.77) by Hall et al.1,49 The Cronbach’s alpha and preliminary exploratory factor analysis were calculated and conducted. Based on the results, one item (“telling patients about mistakes”) was deleted because of its weak item-total correlation (0.20) and low loading factor (0.25). The deletion of this item elevated the Cronbach’s alpha from 0.62 to 0.67. We performed another exploratory factor analysis for our 4-item scale and extracted one factor by using Cattell’s scree test and the interpretability criteria; the second factors accounted for only 10% of the common variance. The loading factors of the 4 items ranged 0.52 to 0.67. To test the construct validity of this scale, we calculated the Pearson correlation with the theoretically related variables, that is, confidence in the health care system, satisfaction with the health care system, with treatment on the previous doctor visit, and with treatment on the previous hospitalization. The results revealed moderate correlation between general trust and the 4 variables (0.40, 0.46, 0.40, and 0.34, respectively, with all P < .001). The final factor-based scale scores ranged 4 to 20 with higher values representing higher trust in physicians.
Table 1.
Items Used to Construct “General Trust in Physician” Scale and the Comparison With Validated Scales.
| Items from the ISSP questionnairea | Items from the scale by Hall et al | Domains of the conceptual model of general trust in physicians |
|---|---|---|
| All things considered, doctors can be trusted. | All in all, you trust doctors completely.b | Global trust |
| Doctors discuss all treatment options with their patients. | Doctors are totally honest in telling their patients about all of the different treatment options available for their conditions. | Honesty |
| The medical skills of doctors are not as good as they should be.c | Doctors are extremely thorough and careful.b | Competence |
| Doctors care more about their earnings than about their patients.c | Doctors in [general] care about their patients’ health just as much or more as their patients do. Sometimes doctors care more about what is convenient for them than about their patients’ medical needs.b |
Fidelity |
| Doctors would tell their patients if they made a mistake during treatment.d | Honesty |
Note. ISSP = International Social Survey Programme.
Measured by 5-point Likert scale with 1 = strongly disagree to 5 = strongly agree; reverse scoring for the negative direction items.
The same items in both the original 11-item scale and the short version 5-item scale.
Negative direction.
Deleted in the final scale.
To explore the influence of health care commodification on the 4 conceptual domains of trust in physicians elaborately, we also used the other 3 items of the trust scale separately as our minor outcomes in addition to our major outcome, global trust.
Study Sample, Explanatory Variables, and Processing of Missing Data
According to a previous study, trust in physicians was associated with some personal characteristics.50 Of the 29 countries with 45 563 respondents, we excluded 6 countries (Bulgaria, Croatia, Lithuania, Philippines, Russian Federation, and South Africa) because of a lack of data required for constructing the health care index. Of the remaining 36 448 respondents from 23 countries, we excluded respondents with missing values of the outcome variables (missing = 765 for the major outcome “trust in physicians”; missing = 4452 for the 4-item scale) or the explanatory variables included in the analysis (missing education = 499, gender = 55, age = 155, and urban or rural residence = 266). We also incorporated occupation and household income into our models. We categorized occupation into medical doctors, other health professionals, and other occupations.
For respondents with missing data on household income and without a partner in paid work living in the same household, we either used personal income as a surrogate or set household income to 0 for respondents not in paid work. If the respondent had a partner in paid work living in the same household, we multiplied his or her personal income by the ratio of average household income to average personal income by gender and country. We categorized household income into 5 country-specific quintiles for cross-national comparison.
The final sample used in analyzing the relationship between health care commodification and one-item ordinal trust outcome included 34 968 respondents; the smallest sample size was 831 in the United Kingdom. The sample used in analyzing the trust scale outcome included 31 412 respondents. All the 23 sample countries were high-income except Chile and Turkey were upper-middle-income in 2011 according to the World Bank classification.
Statistical Analysis
A multilevel cumulative logit model was used to analyze our main ordinal outcome to account for the interdependence of the outcomes within one country owing to unobserved contextual factors. We used the categorized health care index as our main contextual explanatory variable in principle, but also treated the index as a continuous variable to increase the robustness of our results.
For testing the proposed mechanism of risk exposure to unmet health care needs, we also added the interaction terms of the health care index and household income to determine whether the effect size of health care commodification on trust in physicians is larger in individuals with lower incomes. For the aggregated 4- to 20-point scale outcome, a linear multilevel model was applied. All analyses were conducted with SAS software, version 9.4.
Results
Table 2 presents the measures, ranks, and categories of the modified health care index of the 23 countries in the final sample. The well-known commodified countries, the United States and Chile, were categorized as health care–commodified countries. The countries with public health service, such as the United Kingdom and Norway, were categorized as health care–decommodified countries. However, the other 3 Nordic countries (Denmark, Finland, and Sweden) were categorized as reference countries rather than as decommodified countries.
Table 2.
Modified Health Care Index Data (2011).
| Country | Private health expenditurea (% of GDP) | Score 1 | Private for-profit hospital beds (% of total bed stock) | Score 2 | Public health care system coverage (% of population) | Modified health care index score | Rank of level of commodification | Modified health care index categoryb |
|---|---|---|---|---|---|---|---|---|
| United States | 8.3 | 1 | 15.1c | 2 | 31.8 | 9.5 | 1 | Commodified |
| Chile | 2.3 | 2 | 27.5 | 1 | 79.8 | 23.9 | 2 | Commodified |
| Germany | 2.6 | 2 | 29.8 | 1 | 88.9 | 26.7 | 3 | Commodified |
| Poland | 1.9 | 2 | 26.8 | 1 | 96.6 | 29.0 | 4 | Commodified |
| Taiwan | 2.8d | 2 | 26.2d | 1 | 99.9d | 30.0 | 5 | Reference |
| France | 2.6e | 2 | 23.7 | 1 | 99.9 | 30.0 | 6 | Reference |
| Portugal | 3.4 | 1 | 7.6 | 2 | 100.0 | 30.0 | 7 | Reference |
| Switzerland | 3.5 | 1 | 13.1f | 2 | 100.0 | 30.0 | 7 | Reference |
| Slovak Republic | 2.2 | 2 | 16.4g | 2 | 95.2 | 38.1 | 9 | Reference |
| Australia | 2.8e | 2 | 16.6 | 2 | 100.0 | 40.0 | 10 | Reference |
| Denmark | 1.6 | 2 | 2.8 | 2 | 100.0 | 40.0 | 10 | Reference |
| Finland | 2.1 | 2 | 4.9 | 2 | 100.0 | 40.0 | 10 | Reference |
| Israel | 2.7h | 2 | 11.8 | 2 | 100.0 | 40.0 | 10 | Reference |
| Korea | 3.2 | 1 | 0.0 | 3 | 100.0 | 40.0 | 10 | Reference |
| Sweden | 1.7 | 2 | 7.6i | 2 | 100.0 | 40.0 | 10 | Reference |
| Belgium | 2.4 | 2 | 0.0j | 3 | 98.8 | 49.4 | 16 | Reference |
| Turkey | 1.1k | 3 | 18.4 | 2 | 99.5 | 49.8 | 17 | Decommodified |
| Netherlands | 1.5l | 2 | 0.0m | 3 | 99.9 | 50.0 | 18 | Decommodified |
| Czech Republic | 1.1 | 3 | 13.6m | 2 | 100.0 | 50.0 | 19 | Decommodified |
| Japan | 1.8 | 2 | 0.0 | 3 | 100.0 | 50.0 | 19 | Decommodified |
| Norway | 1.4 | 3 | 6.3n | 2 | 100.0 | 50.0 | 19 | Decommodified |
| Slovenia | 1.2 | 3 | 1.1 | 3 | 100.0 | 60.0 | 22 | Decommodified |
| United Kingdoma | 1.2 | 3 | 0.0 | 3 | 100.0 | 60.0 | 22 | Decommodified |
Source. Organisation for Economic Co-operation and Development.24
Note. GDP = gross domestic product.
Excluding expenditures of private social (compulsory) insurance and nonprofit institutions.
Commodified < mean – standard deviation (SD). Reference: between (mean – SD) and (mean + SD). Decommodified > mean + SD.
Data from 2010.
Data from the Ministry of Health and Welfare, Executive Yuan R.O.C. Taiwan.25
Estimated by assuming no private social (compulsory) insurance.
Data from 2001.29
Data of number of hospitals rather than beds, data from 2007.28
Estimated by subtracting private nonprofit institution expenditure of total “current” expenditure from private expenditure of total health expenditure.
Data of number of hospitals rather than beds, from 2012.27
Estimated by assuming no private social (compulsory) insurance and no private nonprofit institution expenditure.
Data from 2007.32
Estimated by multiplying data of total “current” expenditure by the ratio of total expenditure to total current expenditure of other all other countries with available data.
Data from 2009.
Data from Eurostat.26
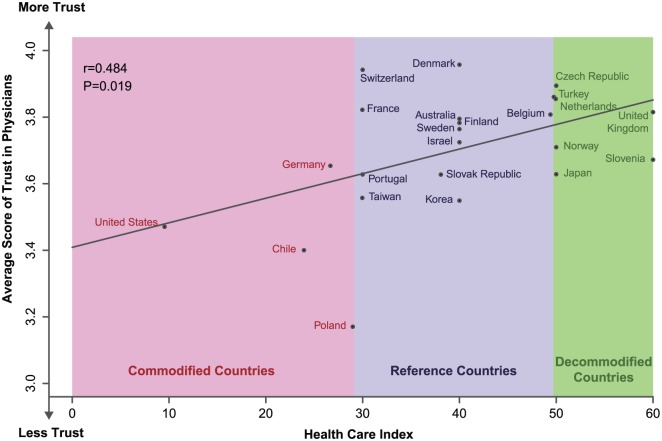
We performed a preliminary analysis with simple regression of the country-averaged scores of ordinal patient trust outcome (strongly disagree = 1 to strongly agree = 5) on the health care index (Figure 2) and calculated a Pearson correlation of 0.484 (P = .019). Countries with a lower health care index level (commodified countries) had lower public trust in physicians. The average score of trust in physicians was significantly higher in decommodified countries (3.8) than in commodified countries (3.4; P = .0035).
Figure 2.
Scatter plot and regression line of average score of patient trust and health care index.
This result suggested a negative impact of health care commodification on public trust in physicians. However, we can see 2 outliers of the United States with extraordinarily low health care index and Poland with extraordinarily low trust levels. Therefore, we also did a sensitivity analysis in the subsequent multilevel model by excluding respondents from the United States and Poland.
The empty multilevel model revealed an intraclass correlation coefficient of 0.057 (P < .001) for the ordinal trust outcome and 0.081 for our trust scale outcome (P < .001), indicating that a significant variation of public trust in physicians was due to contextual factors, although 91.9% to 94.3% of the variations were explained by individual factors. We also verified the proportional odds assumption of using a cumulative logit model; the proportional odds assumption held.
Table 3 presents the results of the adjusted odds ratios (ORs) of having higher trust in physicians regarding the 2 models; the health care index was treated as a categorical or a continuous variable. Compared with those in the reference countries, the respondents in the commodified countries were approximately half as likely to agree with the statement “Doctors in [your country] can be trusted” (OR: 0.47, 95% confidence interval [CI]: 0.31-0.72). Nevertheless, no significant difference was observed for the odds between the respondents in the decommodified countries and in the reference countries (OR: 1.09, 95% CI: 0.78-1.53). To test for the robustness of the results, we treated the health care index as a continuous variable in the model and calculated an OR of 0.84 (95% CI: 0.73-0.98) for a positive response to the statement for a 10-unit decrease in the health care index (more commodified). In the sensitivity analysis excluding respondents from the United States and Poland, the respondents in the commodified countries also were approximately half as likely to trust physicians (OR: 0.59, 95% CI: 0.35-1.01), although it was marginally nonsignificant.
Table 3.
Adjusted OR of Higher Agreement on “Doctors In [Your Country] Can Be Trusted.”
| OR | 95% CI | OR | 95% CI | |
|---|---|---|---|---|
| Health care index | ||||
| 10-unit decrease (more commodified)a | 0.84* | 0.73-0.98 | ||
| Commodified | 0.47** | 0.31-0.72 | ||
| Reference | 1 | |||
| Decommodified | 1.09 | 0.78-1.53 | ||
| Occupation | ||||
| Medical doctor | 2.60*** | 1.80-3.75 | 2.59*** | 1.79-3.75 |
| Other health professional | 1.31* | 1.05-1.62 | 1.31* | 1.05-1.62 |
| Otherb | 1 | 1 | ||
| Household incomec | ||||
| Top quintile | 1.24*** | 1.16-1.34 | 1.24*** | 1.16-1.34 |
| Fourth quintile | 1.13*** | 1.05-1.21 | 1.13*** | 1.05-1.21 |
| Middle quintile | 1 | 1 | ||
| Second quintile | 0.97 | 0.90-1.04 | 0.97 | 0.90-1.04 |
| Bottom quintile | 1.00 | 0.93-1.07 | 1.00 | 0.93-1.07 |
| Missing | 0.92* | 0.84-1.00 | 0.92* | 0.84-1.00 |
| Educationd | ||||
| Upper level tertiarye | 1.21*** | 1.11-1.32 | 1.21*** | 1.11-1.32 |
| Lower level tertiary, first stagef | 1.08* | 1.01-1.16 | 1.08* | 1.01-1.16 |
| Postsecondary, nontertiaryg | 0.96 | 0.89-1.04 | 0.96 | 0.89-1.04 |
| Upper secondaryh | 1 | 1 | ||
| Lower secondaryi | 0.93* | 0.87-0.99 | 0.93* | 0.87-0.99 |
| No formal education or primary school | 0.99 | 0.92-1.07 | 0.99 | 0.92-1.07 |
| Sex | ||||
| Female | 0.87*** | 0.83-0.91 | 0.87*** | 0.83-0.91 |
| Male | 1 | 1 | ||
| Age | ||||
| 15-39 | 1 | 1 | ||
| 40-59 | 1.05 | 1.00-1.11 | 1.05 | 1.00-1.11 |
| 60-100 | 1.69*** | 1.60-1.80 | 1.69*** | 1.60-1.80 |
| Place of living | ||||
| Urban | 1.06* | 1.00-1.11 | 1.06* | 1.00-1.11 |
| Rural | 1 | 1 | ||
Note. OR = odds ratio; CI = confidence interval.
As continuous variable; minimum of 0 representing most commodified; maximum of 60 representing most decommodified.
Including missing value of occupation.
Country-specific quintile.
Categories for international comparison.
Master, Dr.
Also technical schools at a tertiary level.
Other upper secondary programs toward the labor market or technical formation.
Programs that allow entry to university.
Secondary education completed that does not allow entry to university: end of obligatory school but also short programs (less than 2 years).
P< .05. **P < .01. ***P< .001.
Regarding the individual factors, the results showed that medical doctors and other health professionals were more likely to believe that doctors in their country can be trusted compared with people in other occupations (OR: 2.60, 95% CI: 1.80-3.75; OR: 1.31, 95% CI: 1.05-1.62, respectively). People with household incomes in the top 2 quintiles (OR: 1.24, 95% CI: 1.16-1.34; OR: 1.13, 95% CI: 1.05-1.21, respectively), with higher education levels, being male, being older, or living in urban areas, were more likely to trust physicians.
In a model for the interaction of the health care index and household income, we dichotomized the health care index into commodified and reference/decommodified countries according to the results of the previous model for parsimony. The overall interaction effect of the health care index and household income was nonsignificant (P = .36; Figure 3).
Figure 3.
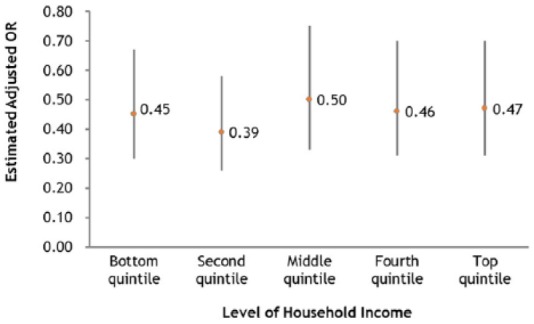
Estimated adjusted odds ratio (OR) of higher trust in physicians for health care–commodified countries compared with reference and decommodified countries conditioning on each level of household income.
Note. The overall interaction effect of health care commodification (dichotomized into commodified and reference/decommodified countries) and household income was nonsignificant (P = .36). Bars represent 95% confidence intervals.
Regarding the 4-item “general trust in physicians” scale, the respondents in the health care–commodified countries scored 1.13 (95% CI: 0.37-1.89) lower than those in the reference countries. The trust scores of people living in the health care–decommodified countries were higher (1.84, 95% CI: –4.43 to 8.10) than those in the reference countries, although the difference did not reach the level of statistical significance.
As for our minor outcomes of the other 3 items of trust scale, respondents in the commodified countries were as predicted less likely to trust physicians’ honesty (OR: 0.65, 95% CI: 0.41-1.03), and more likely to distrust physicians’ competence (OR: 1.60, 95% CI: 1.09-2.35) and fidelity (OR: 1.74, 95% CI: 0.87-3.45), although only the OR of trusting physicians’ competence reached statistical significance.
Discussion
Our study demonstrates that after controlling for the individual determinants of general trust in physicians, people living in health care–commodified countries remained to be significantly less likely to trust physicians than people living in reference countries. In addition, a lower general trust score and less trust in physicians’ honesty, competence, and fidelity observed in health care–commodified countries further support the hypothesis of health care commodification as a possible deteriorating factor to all aspects of public general trust in physicians. Moreover, there was no significant difference in trust in physicians between people living in reference countries and health care–decommodified countries. There are 3 possible explanations. First, the effect of the contextual factor of health care decommodification may reach a “ceiling effect.”51 In other words, health care commodification may not take effect until the level of commodification reaches a threshold; therefore, decommodifying countries with a level of commodification below the threshold may not take effect in elevation of trust level.
Second, not only does the profit-seeking pressure exacerbated by commodification generate financial conflicts of interest, but cost containment pressures made by governments induce conflicts of interest through risk-sharing payment methods such as case payment, capitation, or denial of payment. Because of the expectation of “more is better” created by previous patterns of care,34 patients are typically more concerned about risk-sharing payment methods that might discourage medical use than about methods that might induce unnecessary or even harmful medical demands such as fee-for-service.33 Therefore, financial risk-sharing reimbursement methods may erode patient trust in physicians and offset the “trust protection effect” of decommodification. If there are more tendencies to employ financial risk-sharing reimbursement methods by public health care systems in the decommodified countries due to austerity or other reasons than in the reference countries, the level of public trust in physicians may be indifferent between the decommodified and reference countries. Further researches accounting for the effect of detailed payment systems are encouraged.
Furthermore, although our commodification index was derived from Bambra’s health care decommodification index, the 3 indicators for defining the commodification level of a country may not fully capture the concept of commodification. Therefore, misclassification is likely and may result in underestimation of the differences between countries at different commodification levels. Kawiorska has criticized the adoption of the GDP as a denominator of the “financing” score, and proposed to replace it with “household out-of-pocket payment as a percentage of total current heath expenditure,” as well as to replace the “provision” scores with “the percentage of population reporting difficulties in having their basic medical needs met.”52 After applying their new index as well as the original health care index to the 2012 dataset consisting of data from the 28 member states of the European Union, most (18) of these countries remained at their level of commodification (commodified, reference, and decommodified) as classified by the original health care index (ie, including the measure of private health expenditure as a percentage of GDP); 4 countries altered the level of commodification from decommodified to reference (the original index); 1 country altered from commodified to reference; 4 countries altered from reference to decommodified; and 1 country altered from reference to commodified. No state altered the level of commodification from commodified to decommodified or from decommodified to commodified.52 Therefore, the modification of the health care index by Kawiorska did not alter the result of classification of commodification level much. Because of data limitations, we are not able to reliably test Kawiorska’s alternative measure in our dataset. More efforts are needed to develop more accurate measures and index. Future research with more accurate measures in identifying commodification level of countries may help to contribute in this regard.
We adopted the health care decommodification index developed by Bambra in 2005 to quantify the extent of health care commodification index based on the framework of Esping-Andersen. The health care commodification index later has been adopted in several other studies involving more countries in East Asia and with more recent data. For example, Sam Yu used the data from 2009 and adopted the index to measure the commodification level in 23 countries including the 18 countries studied by Bambra and 5 additional East Asian countries. Kawiorska has also used the data from 2012 and employed the same index to measure health care commodification level in the 28 member states of the European Union. The index yield consistent and reliable results in these studies. The study findings concurred with empirical observations and knowledge, which confirmed the content and construct validity of the index.
Using the modified health care index, Denmark and Finland were classified as reference countries rather than decommodified countries as the results of previous studies43,53 and this study using the original health care index. The reason of this discrepancy is that in the 4 countries—Belgium, Japan, Korea, and the Netherlands—relying on private hospital at the percentage of private beds from 62.3% to 100%, for-profit hospital is forbidden. Therefore, the scores of private for-profit hospital beds of Denmark and Finland were 2 rather than 3 even though their percentages of for-profit beds were relatively low. A recent study that included 28 member states of the European Union also categorized Denmark and Finland as reference countries using the original health care index.52 However, we also used the original health care index to test the robustness of our results, and the results did not change much. Although our modified index captures the profit-seeking aspect of commodification more precisely in theory, further researches are needed to verify its validity. Future research with measures of commodification levels that are more comprehensive may contribute in this regard.
As for the other Nordic country, Sweden, which were classified as a reference country rather than a decommodified country both by the modified and the original health care index, has been classified as a decommodified country by Bambra using the data from 1998, but classified as a reference country by Yu using the data from 2009 and including east Asian countries as our study, and as a reference country by Kawiorska using the data from 2012.52 These results reflect the observation that there has been a trend toward recommodification of health care in Sweden.54
Other limitations should also be noted. First, the sampled countries limited within upper-middle to high-income countries. Second, due to data limitation, we were not able to measure consumerisms and other potential mediators in this study. Future research with better data availability may allow more detailed exploration of the mechanisms. Third, although the negative relationship observed between commodification level of health care and public trust in physicians may suggest a negative influence of health care commodification on public trust in physicians, we cannot rule out the possibility that the observed association may be spurious because of the cross-sectional nature of this study. Lack of temporal sequence and possible unmeasured confounders are 2 limitations. Our study was prone to be confounded by unmeasured contextual confounders such as heterogeneity in culture, developmental stage, and political systems. For example, health care commodification may be just an indicator of a neoliberal ideology of a government, and the ideology causes a comprehensive negative impact on people’s trust in many aspects of public institutes or government-licensed professionals, such as physicians.
Due to data and sample size limitations, an appropriate adjustment of these confounders is not possible for a relatively small sample size of 23 countries. The variation across countries with different commodification levels might be too small to offset the heterogeneity among these countries. This may help to explain why no significant difference was observed between the reference countries and decommodified countries. Empirical analyses based on longitudinal data or comparable countries such as countries with similar health system origins may help to reduce heterogeneity among countries and better identify true effects of health care commodification if sufficient sample sizes can be obtained.
The other limitation is that we did not control general social trust due to lack of suitable data. High level of health care commodification may reflect the free market approaches in the economy of a country, which destroy its social capital including general social trust rather than just trust in physicians. However, as Bambra stated in her study, there were “a number of similarities within the classification of countries between the health care index and that of more conventional labour market centred welfare state typologies,” which means that it may be true that more health care–commodified countries also more generally places with more free market approaches in their economy. However, there were still some exceptions. While Canada, New Zealand, and the United Kingdom were all placed within the more commodified liberal regime, these 3 countries in health care were placed firmly within the decommodified countries. Ireland is another exception. While in the labor market Ireland was placed as the decommodified country, it was classified as reference country with medium commodification score (ie, neither commodified nor decommodified).43
More researches and stronger evidence are still needed to prove a causal relationship leading from health care commodification to a lower level of patient trust. Such a causal relationship may serve as important references in policy making when deciding the role of private financing, the regulation of for-profit providers, and the extent of marketization of a health care system. Potential unintended harmful consequences of commodification should be considered deliberately. For example, a longitudinal cross-regional analysis in Italy showed that an increased percentage of health care dollars allocated on private health care sector was significantly associated with a higher rate of avoidable mortality.55 Other than patients, a British survey showed that two-thirds of doctors were uncomfortable with privatization of the National Health System, and they would like the system to change.32
In conclusion, our study findings illustrate that in addition to the significant role of individual-level characteristics, health care commodification may play a meaningful role in the deterioration of public trust in physicians. Reducing commodification of health care at the country level may help to increase public trust in physicians. However, because of a possible “ceiling effect,” intense health care decommodification does not always guarantee to improved trust in physicians. More research is necessary to investigation factors that might improve or destroy patients’ general trust in physicians.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by National Science Council, Taiwan (grant numbers: 104-2314-B-010-007-MY3 and 106-2314-B-010-026-MY3).
References
- 1. Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37(5):1419-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Arrow KJ. Uncertainty and the welfare economics of medical care. Am Econ Rev. 1963;53(5):941-973. [Google Scholar]
- 3. Bonds DE, Camacho F, Bell RA, Duren-Winfield VT, Anderson RT, Goff DC. The association of patient trust and self-care among patients with diabetes mellitus. BMC Fam Pract. 2004;5:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gupta S, Brenner AT, Ratanawongsa N, Inadomi JM. Patient trust in physician influences colorectal cancer screening in low-income patients. Am J Prev Med. 2014;47(4):417-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jones DE, Carson KA, Bleich SN, Cooper LA. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ Couns. 2012;89(1):57-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nguyen GC, LaVeist TA, Harris ML, Datta LW, Bayless TM, Brant SR. Patient trust-in-physician and race are predictors of adherence to medical management in inflammatory bowel disease. Inflamm Bowel Dis. 2009;15(8):1233-1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee YY, Lin JL. How much does trust really matter? A study of the longitudinal effects of trust and decision-making preferences on diabetic patient outcomes. Patient Educ Couns. 2011;85(3):406-412. [DOI] [PubMed] [Google Scholar]
- 8. Mancuso JM. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs Health Sci. 2010;12(1):94-104. [DOI] [PubMed] [Google Scholar]
- 9. Thom DH, Kravitz RL, Bell RA, Krupat E, Azari R. Patient trust in the physician: relationship to patient requests. Fam Pract. 2002;19(5):476-483. [DOI] [PubMed] [Google Scholar]
- 10. Barton JL, Trupin L, Tonner C, et al. English language proficiency, health literacy, and trust in physician are associated with shared decision making in rheumatoid arthritis. J Rheumatol. 2014;41(7):1290-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Meyer S, Ward P, Coveney J, Rogers W. Trust in the health system: an analysis and extension of the social theories of Giddens and Luhmann. Health Sociol Rev. 2008;17(2):177-186. [Google Scholar]
- 12. Ward PR, Miller E, Pearce AR, Meyer SB. Predictors and extent of institutional trust in government, banks, the media and religious organisations: evidence from cross-sectional surveys in six Asia-Pacific countries. PLoS One. 2016;11(10):e0164096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ward PR, Mamerow L, Meyer SB. Interpersonal trust across six Asia-Pacific countries: testing and extending the “high trust society” and “low trust society” theory. PLoS One. 2014;9(4):e95555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Blendon RJ, Benson JM, Hero JO. Public trust in physicians—U.S. medicine in international perspective. N Engl J Med. 2014;371(17):1570-1572. [DOI] [PubMed] [Google Scholar]
- 15. Mechanic D. Changing medical organization and the erosion of trust. Milbank Q. 1996;74(2):171-189. [PubMed] [Google Scholar]
- 16. Churchill LR. The United States health care system under managed care. How the commodification of health care distorts ethics and threatens equity. Health Care Anal. 1999;7(4):393-411. [DOI] [PubMed] [Google Scholar]
- 17. Havighurst CC. Starr on the corporatization and commodification of health care: the sequel. J Health Polit Policy Law. 2004;29(4-5):947-967; discussion 1005-1019. [DOI] [PubMed] [Google Scholar]
- 18. Reich AD. Selling Our Souls: The Commodification of Hospital Care in the United States. Princeton, NJ: University Press; 2014. [Google Scholar]
- 19. Mackintosh M, Kovalev S. Commercialisation, inequality and transition in health care: the policy challenges in developing and transitional countries. J Int Dev. 2006;18(3):387-391. [Google Scholar]
- 20. Mackintosh M. Commercialisation, inequality and the limits to transition in health care: a Polanyian framework for policy analysis. J Int Dev. 2006;18(3):393-406. [Google Scholar]
- 21. Polanyi K. The Great Transformation: The Political and Economic Origins of Our Time. Boston, MA: Beacon Press; 2007. [Google Scholar]
- 22. Esping-Andersen G. The Three Worlds of Welfare Capitalism. Princeton, NJ: Princeton University Press; 1990. [Google Scholar]
- 23. Bambra C. Cash versus services: “worlds of welfare” and the decommodification of cash benefits and health care services. J Soc Policy. 2005;34(2):195-213. [Google Scholar]
- 24. Pellegrino ED. The commodification of medical and health care: the moral consequences of a paradigm shift from a professional to a market ethic. J Med Philos. 1999;24(3):243-266. [DOI] [PubMed] [Google Scholar]
- 25. March JG. Primer on Decision Making: How Decisions Happen. New York: Free Press; 1994. [Google Scholar]
- 26. Messick DM. Alternative logics for decision making in social settings. J Econ Behav Organ. 1999;39(1):11-28. [Google Scholar]
- 27. Tenbrunsel AE, Messick DM. Sanctioning systems, decision frames, and cooperation. Adm Sci Q. 1999;44(4):684-707. [Google Scholar]
- 28. Ward PR, Rokkas P, Cenko C, et al. “Waiting for” and “waiting in” public and private hospitals: a qualitative study of patient trust in South Australia. BMC Health Serv Res. 2017;17(1):333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ward PR, Rokkas P, Cenko C, et al. A qualitative study of patient (dis)trust in public and private hospitals: the importance of choice and pragmatic acceptance for trust considerations in South Australia. BMC Health Serv Res. 2015;15(1):297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cunningham PJ. High medical cost burdens, patient trust, and perceived quality of care. J Gen Intern Med. 2009;24(3):415-420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Rodwin MA. Conflicts of Interest and the Future of Medicine: the United States, France, and Japan. New York: Oxford University Press; 2011. [Google Scholar]
- 32. O’Dowd A. Doctors’ worry about NHS “privatisation” is growing, says BMA. BMJ. 2016;353:i2232. [DOI] [PubMed] [Google Scholar]
- 33. Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians: effects of choice, continuity, and payment method. J Gen Intern Med. 1998;13(10):681-686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kao AC, Green DC, Zaslavsky AM, Koplan JP, Cleary PD. The relationship between method of physician payment and patient trust. JAMA. 1998;280(19):1708-1714. [DOI] [PubMed] [Google Scholar]
- 35. Cammett M, Lynch J, Bilev G. The influence of private health care financing on citizen trust in government. Perspect Polit. 2015;13(4):938-957. [Google Scholar]
- 36. International Social Survey Programme. Health and Health Care—ISSP 2011. http://www.issp.org/. Published 2013. Accessed December 7, 2014.
- 37. Organisation for Economic Co-operation and Development. OECD health data 2011. http://stats.oecd.org/. Published 2011. Accessed June 6, 2015.
- 38. Ministry of Health Welfare. Executive Yuan R.O.C. Taiwan: https://www.mohw.gov.tw/np-126-2.html. Published 2011. Accessed June 6, 2015. [Google Scholar]
- 39. Eurostat. Hospital beds by hospital ownership. http://ec.europa.eu/eurostat. Published2011. Accessed July 6, 2015.
- 40. European Hospital and Healthcare Federation. The hospitals in the 27 European countries: country profile Sweden. http://www.hope.be/03activities/quality_eu-hospitals/eu_country_profiles/sweden-eu_hospitals-profile.pdf. Published 2012. Accessed June 7, 2015.
- 41. Mazag J. PHIS Hospital Pharma Report: Slovakia. Bratislava, Slovakia: Pharmaceutical Health Information System; 2009. [Google Scholar]
- 42. Farsi M, Filippini M. An analysis of efficiency and productivity in Swiss hospitals. SJES. 2006;142(1):1-37. [Google Scholar]
- 43. Bambra C. Worlds of welfare and the health care discrepancy. Soc Pol Soc. 2005;4(1):31-41. [Google Scholar]
- 44. Organisation for Economic Co-operation and Development. Health Insurance Coverage for a Core Set of Services, 2011, in Health at a Glance 2013. Paris, France: Organisation for Economic Co-operation and Development; 2013. [Google Scholar]
- 45. Organisation for Economic Co-operation and Development Health Division. Guidelines for the implementation of the SHA 2011 framework for accounting health care financing. Paris, France: Organisation for Economic Co-operation and Development; 2014. [Google Scholar]
- 46. Bayindir EE. Hospital ownership type and treatment choices. J Health Econ. 2012;31(2):359-370. [DOI] [PubMed] [Google Scholar]
- 47. Horwitz JR, Nichols A. Rural hospital ownership: medical service provision, market mix, and spillover effects. Health Serv Res. 2011;46(5):1452-1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Horwitz JR. Making profits and providing care: comparing nonprofit, for-profit, and government hospitals. Health Aff. 2005;24(3):790-801. [DOI] [PubMed] [Google Scholar]
- 49. Dugan E, Trachtenberg F, Hall MA. Development of abbreviated measures to assess patient trust in a physician, a health insurer, and the medical profession. BMC Health Serv Res. 2005;5:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Meyer SB, Ward PR, Jiwa M. Does prognosis and socioeconomic status impact on trust in physicians? Interviews with patients with coronary disease in South Australia. BMJ Open. 2012;2:e001389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Everitt BS, Skrondal A. The Cambridge Dictionary of Statistics, Fourth Edition. New York, NY: Cambridge University Press; 2010. [Google Scholar]
- 52. Kawiorska D. Healthcare in the light of the concept of welfare state regimes—comparative analysis of EU member states. Oecon Copernic. 2016;7(2):187. [Google Scholar]
- 53. Yu S. Contribution of health care decommodification index to the analysis of the marginalisation of East Asian countries in comparative welfare studies. Dev Soc. 2012;41(2):253-270. [Google Scholar]
- 54. Farrants K, Bambra C, Nylen L, Kasim A, Burström B, Hunter D. The recommodification of healthcare? A case study of user charges and inequalities in access to healthcare in Sweden 1980-2005. Health Policy . 2017;121(1):42-49. [DOI] [PubMed] [Google Scholar]
- 55. Quercioli C, Messina G, Basu S, McKee M, Nante N, Stuckler D. The effect of healthcare delivery privatisation on avoidable mortality: longitudinal cross-regional results from Italy, 1993-2003. J Epidemiol Community Health. 2013;67(2):132-138. [DOI] [PubMed] [Google Scholar]