Abstract
Objective
The 2013 ACC/AHA lipid management guidelines recommend high-intensity statins in all patients ≤75 years old with chronic limb-threatening ischemia (CLTI), and moderate-intensity statins in CLTI patients >75 without contraindications or on dialysis, but these recommendations are based primarily on coronary and stroke data. We aimed to validate these guidelines in patients with CLTI. and assess current adherence to these recommendations.
Methods
We identified all patients with CLTI who underwent first time revascularization (endovascular or surgical) at Beth Israel Deaconess Medical Center from 2005 to 2014. Patients were classified as taking high-intensity, moderate-intensity, low-intensity, or no statin postoperatively. Outcomes included death and major adverse limb event (MALE). Propensity scores were calculated for the probability of receiving guideline recommended intensity of statin therapy to account for nonrandom assignment of treatments. Cox regression models were constructed adjusted for the propensity scores and further adjusted for strong potential confounders.
Results
After excluding patients on hemodialysis (n=252), we identified 1,019 limbs from 931 patients with a median follow-up of 380 days. Patients discharged on the recommended statin intensity had higher rates of preoperative statin use, coronary artery disease, chronic kidney disease, stroke, atrial fibrillation, congestive heart failure, and coronary artery bypass grafting, lower smoking rates and were less likely to be ambulatory preoperatively. Overall, only 35% were on the recommended statin dosage: 55% of those >75 years old and 20% of those ≤75. In multivariable analysis including propensity scores where appropriate, discharge on any statin was associated with lower mortality (HR 0.71 [95% Confidence Interval 0.60 – 0.90], P <.01). Discharge on the recommended intensity of statin therapy was associated with lower mortality (HR 0.73 [0.60 – 0.99], P < .05) and lower MALE (HR 0.71 [0.51 – 0.97], P < .05). Patients >75 years old and ≤75 accrued similar benefit. In patients > 75 years old, moderate-intensity statin therapy was associated with lower rates of death and MALE compared to high-intensity therapy, but did not reach statistical significance.
Conclusions
Use of the recommended intensity of statin therapy in compliance with 2013 ACC/AHA lipid management guidelines is associated with significantly improved survival and lower MALE in patients undergoing revascularization for CLTI. Adherence to current guidelines is an appealing target for quality improvement.
Introduction
Peripheral arterial disease (PAD) is the manifestation of atherosclerosis in the extremities. Epidemiologic studies demonstrate that PAD afflicts one in five adults over the age of 65.1,2 Although many patients with PAD are asymptomatic at time of diagnosis, manifestations of the disease range from intermittent claudication to limb-threatening ischemia. Chronic limb-threatening ischemia (CLTI), the infrainguinal equivalent of a myocardial infarction or cerebrovascular accident, is the most devastating form of PAD, and afflicts up to 1% of the population.3 CLTI - defined as ischemia with rest pain, ulceration, or gangrene - carries with it significant morbidity and mortality. Recent studies demonstrate a 30% rate of death or major adverse limb events (MALE) at one year even after successful revascularization.4 Mortality rates remain as high as 25% per year in modern series, with one year amputation rates of 25%.5
Significant advances have been made over the past 20 years in the medical management of atherosclerosis in the coronary and cerebrovascular circulations. Antiplatelet agents, beta blockers, anti-hypertensives, and statin therapy are now mainstays of therapy, supported by a rich evidence base.4–8 In 2013, the American College of Cardiology (ACC) and the American Heart Association (AHA) published an update to their lipid management guidelines. They made two key recommendations: with the exception of patients receiving hemodialysis and those with contraindications or allergies, all patients with CLTI above the age of 75 should be on a moderate-intensity statin, and those under the age of 75 should be on a high-intensity statin.9 These new guidelines were unique in that they replaced targeted blood cholesterol levels with recommended intensity of statin therapy, and their target population was expanded to include patients with PAD. These recommendations are supported by a robust evidence base in patients with atherosclerotic disease in the coronary and cerebrovascular circulations.9 In contrast, there is significantly less evidence for the use of these therapies - especially the intensity of therapy - in patients with peripheral vascular disease. Studies from the Vascular Quality Initiative (VQI) and the REduction of Atherothrombosis for Continued Health (REACH) registries demonstrated an 18% higher rate of survival for PAD patients taking statins compared to those not prescribed statins, but these studies lack any information regarding intensity of therapy.10,11
Unfortunately, despite these guidelines (and likely due at least in part to the dearth of evidence), statins remain underutilized in PAD. A study of Danish registries found that only about half of all patients with PAD were taking a statin, and only 62% of vascular patients in the VQI were prescribed a statin and an antiplatelet agent.11,12 To our knowledge, there are no data on the rate of adherence to these recent guidelines or the relationship between their application and outcomes in a vascular population. Therefore, our goal was to assess the application of the recent ACC/AHA lipid management guidelines to the CLTI population.
Methods
Subjects
We performed a retrospective cohort study of all patients with CLTI who underwent a first time revascularization procedure between 2005–2014 at a single institution. Patients were identified through the review of online booking, institutional Vascular Study Group of New England (VSGNE) data, and billing data.. Patient charts were then reviewed to confirm the procedures performed. Patients on hemodialysis were excluded. The Beth Israel Deaconess Medical Center Institutional Review Board approved this study and waived the need for patient consent due to the retrospective nature of the design.
Statins
Postoperative statin use and intensity were recorded from the discharge medication lists from the index procedure. Statin intensity was classified according to ACC/AHA guidelines, which recommend high-intensity statins in patients with CLTI ≤75 years old, and moderate-intensity in those >75 (Table I). Patients on hemodialysis (n=252) were excluded, as there were no applicable guidelines, and patients on simvastatin 80 mg (n=51) were excluded from the primary analysis as this is no longer a recommended dose and was therefore left out of the guidelines.
Table I.
Intensity of statin therapy, according to 2013 ACC/AHA Guidelines9
| High-Intensity Statin Therapy | Moderate-Intensity Statin Therapy |
Low-Intensity Statin Therapy |
|---|---|---|
|
| ||
| Daily dose lowers LDL–C on average, by approximately ≥50% |
Daily dose lowers LDL–C on average, by approximately 30% to <50% |
Daily dose lowers LDL–C on average, by <30% |
|
| ||
| Atorvastatin 10–20 mg | ||
| Rosuvastatin 5–10 mg | Simvastatin 10 mg | |
| Simvastatin 20–40 mg | Pravastatin 10–20 mg | |
| Atorvastatin 40–80 mg | Pravastatin 40–80 mg | Lovastatin 20 mg |
| Rosuvastatin 20-40 mg | Lovastatin 40 mg | Fluvastatin 20–40 mg |
| Fluvastatin XL 80 mg | Pitavastatin 1 mg | |
| Fluvastatin 40 mg bid | ||
| Pitavastatin 2–4 mg | ||
Outcomes
The primary outcome was death and secondary outcome was major adverse limb event (MALE). MALE included amputation or major re-intervention, defined as creation of a new bypass graft, a jump/interposition graft revision, surgical thrombectomy with or without surgical patch angioplasty, and thrombectomy of an occluded graft or arterial segment using pharmacologic or mechanical thrombolysis. Only major amputations were considered (defined as proximal to the ankle joint). Limb events and interventions were ascertained through chart review, and death was ascertained through chart review and the Social Security Death Index.
To address the problem of repeated measures from treating both limbs independently, if a patient underwent an intervention on one limb and later underwent a contralateral intervention for CLTI, their initial leg was censored at the entry date of the second limb.
Statistical Analysis
We assessed the association between discharge on any statin therapy to no statin therapy, as well as the association between the intensity of statin therapy on the primary and secondary outcomes. Categorical variables were compared using Pearson chi-square and Fisher exact tests. Continuous variables were compared using the Wilcoxon rank-sum test. Univariate survival analysis was carried out with the log-rank test. Cox proportional hazards models were constructed to examine the association between adherence to guidelines and rates of MALE or death.
We constructed a propensity score modeling the odds of receiving treatment with guideline-recommended intensity of statin therapy in a logistic regression model to account for nonrandom assignment to treatment. Covariates were generously introduced into the model, which included age, gender, race, hypertension, renal disease, coronary artery disease, diabetes, chronic obstructive pulmonary disease, smoking, heart failure, stroke, procedure year, indication for procedure (rest pain, ulceration or gangrene), index procedure (endovascular vs open), and preoperative ambulatory status. After computing propensity scores, we assessed covariate balance and overlap of the distributions across treatment groups using the “teffects overlap” and “tebalance” commands in Stata version 14.2. We used Cox proportional hazard regression for our outcome models. The Cox models were adjusted for the propensity scores (entered as a continuous covariate) and to further reduce the potential for residual confounding, the models were also adjusted for potential confounders chosen a priori, based on their plausible confounding effects. A propensity score was not constructed for the analysis of patients on statins compared to those not taking statins, as no score could be constructed that had sufficient overlap.
In a sensitivity analysis, we included the patients on 80 mg of simvastatin, classifying them as high-intensity statin therapy. Since this was a single center study, we also examined the association between intensity of statin therapy and loss to followup to assess for any potential bias in our results.
All statistical analyses were performed using Stata 14.2 (StataCorp, College Station, Tex).
Results
Baseline Characteristics
We identified 1,336 limbs from 1,195 patients. After excluding patients on hemodialysis (n=252) and those on 80 mg of simvastatin (n=51), as well as 14 with missing prescription data, there were 1,019 limbs from 931 patients, with a median follow-up of 380 days (Interquartile Range [IQR] 58–1,113). Baseline characteristics are presented in Table II. Patients on the recommended intensity of statin therapy had significantly more comorbidities compared to those that were not on their recommended intensity, with higher rates of preoperative statin use, coronary artery disease, chronic kidney disease, stroke, atrial fibrillation, congestive heart failure, and coronary artery bypass grafting, and lower rates of smoking rates and preoperative ambulation (all P < .05). However, in the subgroup of patients above the age of 75, there were no differences that reached statistical significance in the baseline characteristics of the patients on recommended intensity of therapy and those that were not.
Table II.
Baseline Characteristics
| ≤75 years old | >75 years old | |||
|---|---|---|---|---|
|
| ||||
| Not on Recommended Statin Intensity (n=464) |
On Recommended Statin Intensity (n=117) |
Not on Recommended Statin Intensity (n=195) |
On Recommended Statin Intensity (n=243) |
|
|
| ||||
| Characteristic | Values are % unless specified | Values are % unless specified | ||
| Age (years), mean (s.d.) | 66 (9.0) | 65 (8.0) | 83 (5.5) | 83 (5.2) |
| Male Gender | 64 | 65 | 51 | 50 |
| White Race | 80 | 79 | 82 | 75 |
| Endovascular Index Procedure | 46 | 47 | 48 | 48 |
| Indication | ||||
| Rest Pain | 24 | 17 | 21 | 21 |
| Ulcer | 49 | 57 | 57 | 53 |
| Gangrene | 27 | 26 | 22 | 27 |
| Preop Antiplatelet | 63 | 76 | 66 | 68 |
| Postop Antiplatelet | 93 | 97 | 91 | 92 |
| Independently Ambulatory | ||||
| Preoperatively | 67 | 67 | 47 | 45 |
| CAD | 42 | 65 | 53 | 52 |
| Hypertension | 83 | 91 | 85 | 85 |
| Diabetes | 77 | 85 | 58 | 64 |
| CKD | 22 | 34 | 25 | 26 |
| Hyperlipidemia | 58 | 74 | 50 | 59 |
| COPD | 11 | 10 | 14 | 15 |
| CABG | 20 | 43 | 23 | 25 |
| Myocardial Infarction | 24 | 40 | 26 | 23 |
| CHF | 21 | 27 | 32 | 35 |
| Atrial Fibrillation | 10 | 13 | 34 | 28 |
| PCI | 16 | 25 | 12 | 14 |
| CVA | 12 | 19 | 12 | 17 |
| Smoking history | 66 | 69 | 53 | 53 |
| Current Smoker | 30 | 27 | 11 | 14 |
(s.d.-standard deviation, CAD-coronary artery disease, CKD-Chronic Kidney Disease, COPD-chronic obstructive pulmonary disease, CABGcoronary artery bypass grafting, CHF-congestive heart failure, PCI-percutaneous coronary intervention, CVA-cerebrovascular accident)
Adherence to Guidelines
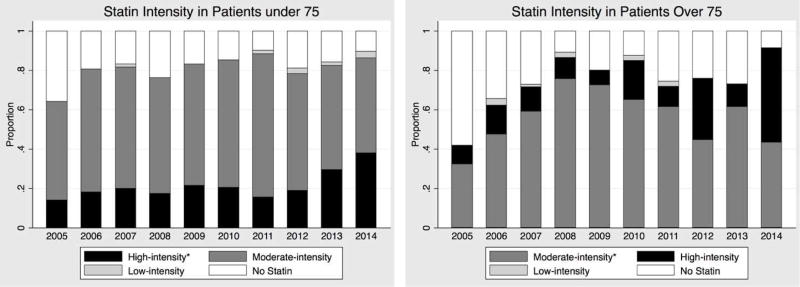
Overall, 77% of the cohort was discharged on a statin, but only 35% were prescribed the intensity of therapy recommended in the 2013 guidelines. Adherence was significantly higher in the cohort of patients above the age of 75, in which 55% were on the recommended intensity, compared to only 20% of those below the age of 75 (Figure I). The use of high-intensity statins in patients under the age of 75 nearly doubled following the introduction of the guidelines in 2013 (18% to 33%). However, use of moderate-intensity statin therapy in those above the age of 75 remained unchanged (56% vs. 53%), likely due to a concomitant doubling of high-intensity statin use from 14% to 29%.
Figure I.
Proportions of patients on various statin intensities, by year. Asterisk (*) indicates the recommended intensity for each population
Univariate Analysis
Postoperative Statin Use Compared to No Statin
On univariate analysis, patients discharged on a statin had significantly higher 5 year survival, with 85% [95% Confidence Interval 82 – 88%] alive at 1 year, 65% [60 – 69%] at 3 years, and 41% [35 – 46%] at 5 years, compared to 82% [76 – 87%], 55% [47 – 62%], and 35% [26 – 43%] for those not on a statin (log-rank P = .02). There was no difference in the rate of MALE (P = .21).
Intensity of Statin Therapy in Accordance with 2013 Lipid Management Guidelines
We also compared those patients on the intensity of statin therapy recommended by the ACC/AHA Guidelines, compared to those not prescribed the recommended intensity or not on statins. Patients on recommended statin intensity had lower 5 year survival, with 84% [80 – 88%] alive at 1 year, 58% [51 – 64%] at 3 years, and 31% at 5 years, compared to 84% [82 – 88%], 65% [60 – 69%], and 43% [38 – 49%] for those not on recommended intensities (log-rank P = .01). There was no statistically significant difference in the rate of MALE (P = .07).
Multivariable Analysis
Postoperative Statin Use Compared to No Statin
After adjustment for age, sex, race, hypertension, diabetes, coronary artery disease, chronic kidney disease, smoking, procedure year and indication, those patients discharged on a statin experienced a 29% lower rate of death (HR 0.71 [95% Confidence Interval 0.60 – 0.90], P < .01) (Table III). This benefit was consistent in the subgroup of patients above the age of 75 and those below 75 years old (P for interaction = 0.54). There was no difference in the rate of MALE (HR 0.81 [0.60 – 1.09], P = .16).
Table III.
Adjusted Hazard Ratios for the comparison of patients discharged on statins versus those who were not
| Adjusted* Outcomes for the Patients on Statins | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Overall | ≤75 years old | >75 years old | ||||
| Outcome: | HR [95% CI] | P | HR [95% CI] | P | HR [95% CI] | P |
| Death | 0.71 [0.56 – 0.90] | 0.01 | 0.65 [0.43 – 0.97] | 0.04 | 0.67 [0.49 – 0.93] | 0.02 |
| MALE | 0.81 [0.60 – 1.09] | 0.16 | 0.91 [0.60 – 1.37] | 0.66 | 0.57 [0.35 – 0.92] | 0.02 |
Adjusted for age, sex, race, hypertension, diabetes, coronary artery disease, chronic kidney disease, smoking, procedure year and indication
Intensity of Statin Therapy in Accordance with 2013 Lipid Management Guidelines
After adding the propensity score to our multivariable model to account for nonrandom assignment of treatment, patients on the intensity of statin therapy recommended by the 2013 Lipid Management Guidelines experienced a 23% lower rate of death compared to other statin intensities (HR 0.77 [0.60 – 0.99], P = .04). The rate of MALE was also significantly lower in the patients on the recommended intensity of statin therapy (HR 0.71 [0.51 – 0.97], P = .03) (Table IV). There was no significant difference in this association between the subgroups of patients above and below 75 years old (P > .1). We also found no difference in this association between patients who underwent endovascular repair compared to those who underwent open surgical bypass.
Table IV.
Adjusted Hazard Ratios for the comparison of patients discharged on the recommended intensity of statin therapy versus those who were not
| Adjusted* Outcomes for the Patients on Recommended Intensity of Statin Therapy | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Overall | ≤75 years old | >75 years old | ||||
| Outcome: | HR [95% CI] | P | HR [95% CI] | P | HR [95% CI] | P |
| Death | 0.77 [0.60 – 0.99] | 0.04 | 0.81 [0.52 – 1.27] | 0.36 | 0.69 [0.49 – 0.96] | 0.03 |
| MALE | 0.71 [0.51 – 0.97] | 0.03 | 0.67 [0.42 – 1.06] | 0.09 | 0.63 [0.39 – 1.03] | 0.07 |
Adjusted for propensity score (continuous) and age, sex, race, hypertension, diabetes, coronary artery disease, chronic kidney disease, smoking, procedure year and indication
High-intensity versus Moderate-intensity in Elderly Patients
High-intensity statins were prescribed to 67 patients above the age of 75 (15%), and moderate-intensity statins were prescribed to 243 (55%). Of those prescribed a high-intensity statin postoperatively, 80% were on a high-intensity preoperatively, 8% were on a moderate-intensity, and 12% were not taking a statin. In unadjusted analysis, patients >75 years old on moderate-intensity statins experienced higher rates of death (log-rank P < .01). After adjustment, there was no statistically significant association between the rates of death and MALE in patients taking the recommended moderate-intensity statins compared to those on high-intensity therapy (death: HR 0.79 [0.49 – 1.26], P = .32; MALE: HR 0.82 [0.41 – 1.64], P = .58) (Table V).
Table V.
Adjusted Hazard Ratios for the comparison of moderate versus high-intensity statin therapy in patients >75 years old
|
Adjusted* Risk for Moderate-Intensity Statin Therapy Compared to High-Intensity | ||
|---|---|---|
| HR [95% CI] | P | |
| Death | 0.79 [0.49 – 1.26] | 0.323 |
| MALE | 0.82 [0.41 – 1.64] | 0.578 |
Adjusted for age, sex, race, hypertension, diabetes, coronary artery disease, chronic kidney disease, smoking, procedure year and indication
Sensitivity Analyses
The primary analysis was re-run after assigning patients on simvastatin 80 mg to the high-intensity therapy group, and there was no difference in any of the observed associations. As this was a single center study, differential loss to followup between treatment arms could bias our results. However, there was no association between loss to followup and intensity of statin therapy (P = .64)
Discussion
Our study demonstrates that statin therapy in accordance with the 2013 ACC/AHA guidelines is associated with significantly lower rates of death and limb events in patients undergoing first-time revascularization for CLTI. Our findings are consistent with prior reports, which document the benefits of statins and the intensity of therapy recommended by the ACC/AHA guidelines in other populations, and validate them in the CLTI population.9
In our study, statin use was associated with lower mortality by almost a third. This is similar to the findings of De Martino et al,11 who showed that patients in the VQI discharged on a statin experienced a 20% decrease in mortality compared to those who were not (HR 0.8 [0.7 – 0.9], P = .01). However, that study was a heterogeneous cohort that included vascular patients undergoing a variety of procedures (lower extremity revascularization, carotid revascularization and aortic aneurysm repair), with comparatively low rates of adequate medical therapy. In 2014, the last year of their study, only 62% of their cohort was on both an antiplatelet agent and a statin. In our study, the rates of statin and antiplatelet use were higher. In 2014, 90% of our patients were on a statin, and 94% were on an antiplatelet agent, and in the entire cohort, 77% were discharged on a statin and 93% on an antiplatelet agent.
Our data demonstrate that although patients benefit from being prescribed a statin, they benefit even more if that statin is the recommended intensity. Patients who were prescribed the guideline-recommended intensity of statin experienced a 23% lower rate of death and 29% lower rate of MALE than those who were not treated in accordance with the guidelines. This is consistent with prior reports in other atherosclerotic disorders, as a substantial body of evidence including randomized, controlled trials demonstrates the importance of statin dose in both cerebrovascular and coronary populations.13–15 Despite rates of medical therapy including statin usage that were higher than many previous studies, event rates in this vulnerable population remain extremely high, with only about a third of the population alive at 5 years. These data suggest that to bridge that gap, clinicians must consider not only if a patient is on a statin, but which statin and at what dose.
The subset of patients above 75 years old represents an important subgroup that has not been well characterized. The ACC/AHA Panel concluded there was adequate evidence to support the use of moderate-intensity statins in this population, but inadequate data to support the use of high-intensity therapy.9 Establishing the most beneficial intensity of therapy in this population is of paramount importance as the population ages. Elderly patients may stand to benefit the most from high-intensity therapy, given their higher burden of comorbid conditions, but conversely may be more likely to discontinue their statin due to intolerance or side effects. Our data demonstrate a trend towards higher rates of death and limb events in elderly patients on high-intensity statins. This could be due to random variation, as our results are not statistically significant, or could be due to other confounding variables we failed to control for. This cohort was a smaller subset, and thus we may have failed to detect a difference due to inadequate power. Those patients may have initially been prescribed higher doses because they are a higher risk cohort, although the fact that patients on moderate-intensity statins actually had higher mortality in unadjusted analysis suggests the opposite conclusion. This population represents an important target for further research.
These data must be interpreted in the context of the study design. We lack detailed records on patient compliance with their prescribed statin therapy or changes in their doses over time, and statin compliance has been as low as 39% in some studies.16,17 Recent efforts such as Get With The Guidelines (GWTG) seek to improve these results, but their success in our population is unknown.18 Further efforts could examine strategies to improve compliance, as well as determine if more intensive statin therapy affects rates of compliance. This is a single center study, and as such these results, and the rates of adherence to guidelines may not be generalizable to the population at large. In addition, we may fail to capture all outcomes that may have occurred elsewhere, and we did not ascertain cause of death. However, this is unlikely to significantly bias our results given our low rate of loss to follow-up (8%), and the lack of association between loss to followup and intensity of statin therapy. Future efforts could include performing similar analyses using nationally representative, multicenter data. It is worth noting that the primary aim of our study was not to assess the adherence to these guidelines, especially prior to their publication, but rather to study the potential impact of their primary goal: treating high risk populations with targeted statin intensities.
Our findings present an important opportunity for multidisciplinary quality improvement. These data support the implementation of the recent guidelines in the CLTI population, but also demonstrate that a substantial gap still exists in their implementation. The CLTI population is a vulnerable cohort which is served by a wide spectrum of clinicians from primary care providers, cardiologists, interventionalists, to vascular surgeons. Educating these diverse physicians about the benefits of following these guidelines represents an important opportunity to improve the care we provide this high risk patient population.
Conclusions
We found that statins are associated with significantly improved overall survival and lower limb events in patients undergoing revascularization for CLTI. Use of the recommended intensity of statin therapy in compliance with 2013 ACC/AHA Lipid Management Guidelines provides important incremental benefit. Although adherence is increasing, 60% of eligible patients in our institution were not on recommended doses even in 2014, an appealing target for future quality improvement projects.
Acknowledgments
Supported by the Harvard-Longwood Research Training in Vascular Surgery NIH T32 Grant 5T32HL007734-22
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Works Cited
- 1.Sigvant B, Wiberg-Hedman K, Bergqvist D, Rolandsson O, Andersson B, Persson E, et al. A population-based study of peripheral arterial disease prevalence with special focus on critical limb ischemia and sex differences. J Vasc Surg. 2007;45(6):1185–91. doi: 10.1016/j.jvs.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 2.Diehm C, Allenberg JR, Pittrow D, Mahn M, Tepohl G, Haberl RL, et al. Mortality and vascular morbidity in older adults with asymptomatic versus symptomatic peripheral artery disease. Circulation. 2009 Nov 24;120(21):2053–61. doi: 10.1161/CIRCULATIONAHA.109.865600. [DOI] [PubMed] [Google Scholar]
- 3.Sigvant B, Lundin F, Wahlberg E, Sigvant B, Wiberg-Hedman K, Bergqvist D, et al. The Risk of Disease Progression in Peripheral Arterial Disease is Higher than Expected: A Meta-Analysis of Mortality and Disease Progression in Peripheral Arterial Disease. Eur J Vasc Endovasc Surg. 2016 Mar;51(3):395–403. doi: 10.1016/j.ejvs.2015.10.022. [DOI] [PubMed] [Google Scholar]
- 4.Conte MS, Pomposelli FB, Clair DG, Geraghty PJ, McKinsey JF, Mills JL, et al. Society for Vascular Surgery practice guidelines for atherosclerotic occlusive disease of the lower extremities: Management of asymptomatic disease and claudication. J Vasc Surg. 2015 Mar;61(3):2S–41S. e1. doi: 10.1016/j.jvs.2014.12.009. [DOI] [PubMed] [Google Scholar]
- 5.Abola MTB, Bhatt DL, Duval S, Cacoub PP, Baumgartner I, Keo H, et al. Fate of individuals with ischemic amputations in the REACH Registry: three-year cardiovascular and limb-related outcomes. Atherosclerosis. 2012 Apr;221(2):527–35. doi: 10.1016/j.atherosclerosis.2012.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Smith SC, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011 Nov 29;124(22):2458–73. doi: 10.1161/CIR.0b013e318235eb4d. [DOI] [PubMed] [Google Scholar]
- 7.Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease. J Am Coll Cardiol. 2016 Mar [Google Scholar]
- 8.MEMBERS WC. Drozda JP, Ferguson TB, Jneid H, Krumholz HM, Nallamothu BK, et al. 2015 ACC/AHA Focused Update of Secondary Prevention Lipid Performance Measures. Circ Cardiovasc Qual Outcomes. 2016 Jan;9(1):68–95. doi: 10.1161/HCQ.0000000000000014. [DOI] [PubMed] [Google Scholar]
- 9.Stone NJ, Robinson J, Lichtenstein AH, Merz CNB, Blum CB, Eckel RH, et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation. 2013 Nov 12; [Google Scholar]
- 10.Kumbhani DJ, Steg PG, Cannon CP, Eagle KA, Smith SC, Goto S, et al. Statin therapy and long-term adverse limb outcomes in patients with peripheral artery disease: insights from the REACH registry. Eur Heart J. 2014 Nov 1;35(41):2864–72. doi: 10.1093/eurheartj/ehu080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Martino RR, Hoel AW, Beck AW, Eldrup-Jorgensen J, Hallett JW, Upchurch GR, et al. Participation in the Vascular Quality Initiative is associated with improved perioperative medication use, which is associated with longer patient survival. J Vasc Surg. 2015 Apr;61(4):1010–9. doi: 10.1016/j.jvs.2014.11.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Subherwal S, Patel MR, Kober L, Peterson ED, Jones WS, Gislason GH, et al. Missed opportunities: despite improvement in use of cardioprotective medications among patients with lower-extremity peripheral artery disease, underuse remains. Circulation. 2012 Sep 11;126(11):1345–54. doi: 10.1161/CIRCULATIONAHA.112.108787. [DOI] [PubMed] [Google Scholar]
- 13.Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, et al. Intensive versus Moderate Lipid Lowering with Statins after Acute Coronary Syndromes. N Engl J Med. 2004 Apr 8;350(15):1495–504. doi: 10.1056/NEJMoa040583. [DOI] [PubMed] [Google Scholar]
- 14.Pedersen TR, Faergeman O, Kastelein JJP, Olsson AG, Tikkanen MJ, Holme I, et al. High-Dose Atorvastatin vs Usual-Dose Simvastatin for Secondary Prevention After Myocardial Infarction<SUBTITLE>The IDEAL Study: A Randomized Controlled Trial</SUBTITLE>. JAMA. 2005 Nov 16;294(19):2437. doi: 10.1001/jama.294.19.2437. [DOI] [PubMed] [Google Scholar]
- 15.Investigators TSP by AR in CL (SPARCL) High-Dose Atorvastatin after Stroke or Transient Ischemic Attack. N Engl J Med. 2006 Aug 10;355(6):549–59. doi: 10.1056/NEJMoa061894. [DOI] [PubMed] [Google Scholar]
- 16.Ford I, Murray H, Packard CJ, Shepherd J, Macfarlane PW, Cobbe SM, et al. Long-term follow-up of the West of Scotland Coronary Prevention Study. N Engl J Med. 2007 Oct 11;357(15):1477–86. doi: 10.1056/NEJMoa065994. [DOI] [PubMed] [Google Scholar]
- 17.Ho PM, Magid DJ, Shetterly SM, Olson KL, Maddox TM, Peterson PN, et al. Medication nonadherence is associated with a broad range of adverse outcomes in patients with coronary artery disease. Am Heart J. 2008 Apr;155(4):772–9. doi: 10.1016/j.ahj.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 18.Heidenreich PA, Lewis WR, LaBresh KA, Schwamm LH, Fonarow GC. Hospital performance recognition with the Get With The Guidelines Program and mortality for acute myocardial infarction and heart failure. Am Heart J. 2009 Oct;158(4):546–53. doi: 10.1016/j.ahj.2009.07.031. [DOI] [PubMed] [Google Scholar]