Abstract
Objective:
The study aimed to investigate whether there is any association of anterior knee pain and knee function with chondromalacia stage and patellofemoral alignment in patients with anterior knee pain for over a month and with chondromalacia patellae (CMP) detected by magnetic resonance imaging (MRI).
Materials and Methods:
We reviewed the medical records of 38 patients who underwent a knee MRI examination and were diagnosed with chondromalacia based on the MRI. Knee MRI images were evaluated by a radiologist for chondromalacia staging. Patients were divided into two groups as early stage (stage 1–2) and advanced stage (stage 3–4) chondromalacia. Patients’ demographical data (age, sex, and occupation), clinical features, physical examination findings and patellofemoral pain severity scale, kujala patellofemoral scoring system, and functional index questionnaire scores were obtained from their medical records. Trochlear sulcus angle, sulcus depth, lateral patellofemoral angle, patellar translation, and Insall–Salvati index were measured using the MRI images.
Results:
The mean patient age was higher in the advanced stage CMP group compared to the early stage CMP group (p=0.038). There was no statistically significant difference regarding other demographical data (p>0.05). MRI measurement parameters did not show difference between the groups (p>0.05). Patients in the advanced stage CMP group had higher patellofemoral pain severity score, lower kujala patellofemoral score, and lower functional index questionnaire score compared to the early stage CMP group. The differences were statistically significant (p=0.008, p=0.012, and p=0.026, respectively).
Conclusion:
As chondromalacia stage advances, the symptom severity worsens and knee functions decline; however, MRI measurements do not show difference between early and advanced stage CMP patients.
Keywords: Anterior knee pain, chondromalacia patellae, patellofemoral alignment, kujala
Introduction
Patellofemoral joint pathologies are important causes of knee pain in young patients. Anterior and anterolateral knee pain often suggest patellofemoral joint pathologies particularly chondromalacia patellae (CMP) [1]. Other causes of anterior knee pain include ligament and meniscus injuries, patellofemoral instability, subluxation, patellar tendinopathy, Osgood–Schlatter syndrome, and Sinding-Larsen-Johansen syndrome [2].
In addition to the medical history and physical examination, direct radiograms, ultrasonography, computed tomography, and magnetic resonance imaging (MRI) can help in the diagnosis of anterior knee pain. Furthermore, special tests that are performed during the physical examination can help detect knee pathology to a great extent. Bone pathologies can be detected with direct radiograms. MRI is a valuable tool owing to its high soft tissue contrast, ability to directly visualize joint cartilage, and capacity to obtain images at multiple planes [3, 4]. MRI is used in staging chondromalacia, which is based on the degree of cartilage injury. Grade 1 and 2 chondromalacia can be detected with 66% sensitivity, while grade 3 and 4 chondromalacia can be detected with 85%–100% sensitivity [5].
It is not known if there is any association between the severity of the anterior knee pain and chondromalacia stage detected by MRI in patients with CMP. Elson et al. [6] examined medial tibial plateau and patellar tendon sensitivity and assessed the anterior knee pain with photographic anterior knee pain map in patients incidentally diagnosed with CMP during arthroscopy. However, the researchers did not find any correlation between arthroscopic lesion and anterior knee pain [6]. Atbaşı et al. [7] studied the relationship between anterior knee pain and CMP, Q angle, and patella types in young adult males. They reported that CMP was not frequently observed in MRI images of young adult patients presenting with anterior knee pain and that physical examination findings were more useful in detecting chondromalacia. They used the low sensitivity of MRI in detecting grade 1 chondromalacia.
There is no study in literature, which examines the effect of CMP stage on anterior knee pain severity and knee function. The present study aimed to investigate whether chondromalacia stage and patellofemoral alignment has any association with knee pain severity and function in patients with anterior knee pain.
Materials and Methods
The study was designed as a single-center, retrospective, cross-sectional study. The study was approved by the hospital ethics committee (Issue number: 26.03.2015/45). Written informed consent was obtained from all patients.
Participants
We reviewed Hospital Information System-Radiology Clinic records between November 2014 and January 2015 of outpatients who underwent knee a MRI examination and were diagnosed with chondromalacia. The patients’ age range was 18–55 years. Patients with anterior knee pain for longer than a month and worsening of the anterior knee pain with at least one of the following activities: climbing or descending stairs, squatting, jumping, and prolonged sitting were include in the study. The study exclusion criteria were a history of a major trauma, history of past lower extremity surgery and/or fracture, presence of neuromuscular disease, inflammatory rheumatic disease, epilepsy, dementia, pregnancy, history of intraarticular injection, genu varus-valgus, difference in leg length, and detection of severe ligament, meniscusor bone lesions, Osgood-Schlatter disease, or advanced stage osteoarthritis in MRI.
Thirty-eight patients met the inclusion criteria. Knee MRI images were evaluated by a radiologist for staging of chondromalacia. Based on the chondromalacia stage, patients were categorized into two groups (early stage [stage 1–2] and advanced stage [stage 3–4] chondromalacia groups).
Evaluations
Patients’ demographical data (age, sex, occupation, marital status, educational state, height, and weight), dominant hands, the side with the complaint, duration of anterior knee pain, presence of daily activities that require prolonged flexion of the knee, sports habits, and recent weight gain or loss were recorded. In addition to anterior knee pain, complaints, including swelling, feeling of knee giving way, stiffness, locking at the knee, clicking noise during movements of the knee, crepitation, pain triggered by prolonged sitting, first-step limping, sliding knee cap, and difficulty in squatting were recorded.
Patients’ lower extremity and knee physical examination findings were obtained from the outpatient clinic records. In the knee examination, anterior and posterior drawer tests, McMurray tests, varus-valgus stress tests, patellar compression, patellar tilt, Clarck J sign, and Ober test results were noted as “negative” if they were normal and as “positive” in case of any pathological signs. Additionally, popliteal angle and Q angle measurements and knee flexion test measurements were recorded in degrees; thigh circumference measured from 10 cm proximal of the middle point of the patella was recorded in centimeters. Lower extremity muscle strength was manually evaluated at the hip, knee, and ankle and recorded as “normal” in case of a 5/5 strength and as “reduced” if it was weaker.
Patellofemoral Pain Severity Scale
Patellofemoral pain severity scale is a 10-cm numerical scale. The patient is requested to mark his/her pain level during climbing/descending stairs, squatting, walking, jogging, running/sprinting, participating in a sport, sitting for 20 minutes while knees are at 90° flexion, kneeling on knees, resting, and following an activity. The maximum score is 100 points [8, 9]. In the present study, the evaluation of the patellofemoral pain severity scale was found in medical records. Values between 0 and 10 that are marked by the patients were recorded as scores. As majority of the patients did not participate in a sports activity, they could not sprint. This led to an exclusion of two parameters. Thus, the maximum available score is only 80.
Functional Index Questionnaire
The functional index questionnaire has 8 questions. Each question is answered as either “unable to do” (0 point), “could do with a problem” (1 point), or “could do without problem” (2 points). The maximum score is 16 points [10, 11].
Kujala Patellofemoral Scoring System
This questionnaire evaluates a total of 13 clinical situations, including limping when walking, giving load, walking, squatting, running, jumping, prolonged sitting with knee flexed, pain, swelling, abnormal painful patella movements, and atrophy of thigh and flexion deficiency. It is used to predict the extent of affection of knee functions due to patellofemoral pain. The maximum score is 100 points [12].
Evaluation of MRI Results
Knee MRI examinations of the study participants were evaluated using images archived in the Picture Archiving Communication System (PACS). All MRI scans were performed with the 1.5 Tesla GE Signa Excite MRI device, using superficial knee Q-coil. Scans were performed while patients were supine with their knees at 0 degrees extension. Five different measurements were performed in all patients’ knee MRI images:
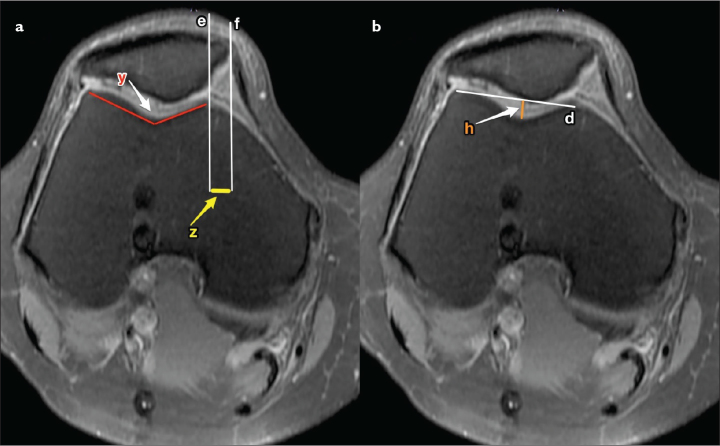
Trochlear sulcus angle: it is the angle between the two lines that connects the deepest point of the trochlea to the anterior medial and lateral femoral condyles [13]. A troch-lear angle greater than 144° was evaluated as trochlear hypoplasia [14] (Figure 1).
Trochlear sulcus depth: it is the distance between the deepest point of the troch-lear sulcus and the line connecting medial and lateral femoral condyles. A sulcus depth lower than 5 mm was accepted as hypoplasia, and a depth lower than 3 mm was accepted as a sign of dysplasia [13] (Figure 1).
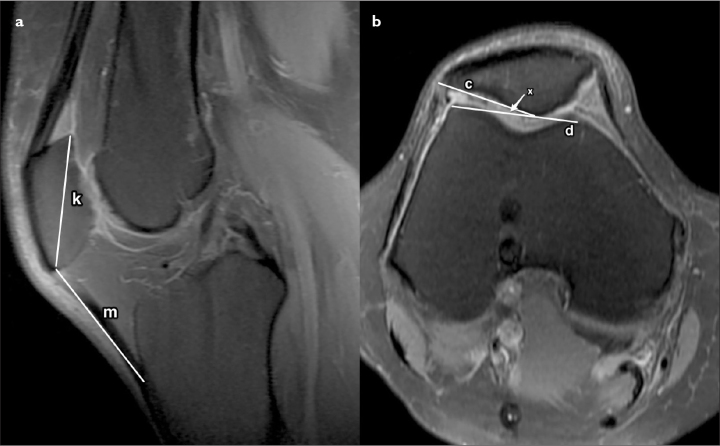
Insall–Salvati index (patellar tendon length / longest diagonal diameter of patella): it is the ratio of patellar tendon length to the longest diagonal diameter of patella. It was measured using the sagittal section where maximum length of patella was visualized (often the section where anterior cruciate ligament can be visualized) [15]. Patellar tendon length was divided by the longest diagonal diameter to calculate the Insall–Salvati index. Values below 1.1 were accepted as patella baja, and values above 1.3 were accepted as patella alta (Figure 2a).
Lateral patellofemoral angle: it is the angle between the line connecting anterior medial and lateral femoral condyles and the line drawn tangential to the lateral patellar facet. This angle is used for the evaluation of patellar tilt and is measured using the axial section corresponding to the middle point of the patella at the sagittal plane [15]. Medial angulation or an angle lower than 8° to the lateral side was evaluated as a sign of abnormal tilt [16] (Figure 2b).
Patellar translation: it is measured to assess patellar subluxation. It is the distance between the vertical line passing from the anterior of medial femoral condyle and the vertical line passing from the medial border of the patella. It is measured using the axial section where the medial border of the patella was at the most medial point. A >2 mm sliding toward the lateral side was evaluated as subluxation [17] (Figure 1).
Figure 1. a, b.
Axial T2-weighted MR images show trochlear sulcus angle, patellar translation, and trochlear sulcus depth measurements
(Trochlear sulcus angle, y: the angle formed between the two lines that connect the deepest point of the trochlea to the highest points of medial and lateral condyles; patellar translation, e: vertical line passing from the anterior of medial femoral condyle, f: vertical line passing from the medial border of the patella, z: the distance between the lines e and f (patellar translation); Trochlear sulcus depth, d: line connecting the anterior points of medial and lateral femoral condyles, h: the distance between the deepest point of the trochlear sulcus and the d line)
Figure 2. a, b.
Sagittal (a) and axial (b) T2-weighted MR images show Insall–Salvati index and lateral patellofemoral angle measurements
(Insall–Salvati Index, k: longest diagonal diameter of patella, m: patellar tendon length; Lateral patellofemoral angle, c: line drawn tangential to the lateral patellar facet, d: line connecting the anterior points of medial and lateral femoral condyles, x: angle value)
Additionally, in all patients, the CMP stage was determined from the MRI images. Patients were categorized in 4 stages based on the MRI staging system that was modified based on the Outerbridge’s arthroscopy staging system [18, 19]. In case cartilage injuries in the medial and patellar facet were at different stages, the highest stage was considered for categorizing the patient.
Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) software version 16., (SPSS Inc.; Chicago, IL, USA) To compare the categorical data in terms of other categorical properties, chi-square and Fisher’s exact tests were used. Any two groups were compared with regard to measurement values using the Mann–Whitney U test. A p value <0.05 was accepted as statistically significant.
Results
Among 38 patients in the study group, 17 patients had stage 3–4 (advanced stage) CMP and 21 had stage 1–2 (early stage) CMP. The mean patient age was significantly higher in the advanced stage CMP group compared to the early stage CMP group (p=0.038). There was no statistically significant difference between the two groups regarding sex, marital status, education level, occupation distribution, and body mass index (p>0.05). Table 1 presents demographical properties of the patients enrolled in the study.
Table 1.
Patient characteristics
| Stage 1–2 CMP (early stage, n=21) | Stage 3–4 CMP (advance stage, n=17) | |
|---|---|---|
| Age (years) | 40 (19–55) | 46 (28–57) |
| Gender | ||
| Female | 16 | 15 |
| Male | 5 | 2 |
| Marital status | ||
| Married | 16 | 14 |
| Single | 5 | 3 |
| Education status | ||
| Primary education | 13 | 7 |
| Secondary education | 5 | 5 |
| University | 3 | 5 |
| Job | ||
| Housewife | 11 | 8 |
| Officer | 2 | 7 |
| Worker | 8 | 2 |
| BMI (kg/m2) | 27.5 (20.1–35.7) | 25.8 (19.4–35.8) |
Data are presented as median (min–max) or number (n); BMI: Body mass index; CMP: chondromalacia patellae
The history of swelling in the knee was significantly different between the advanced (n=8, 47%) and early (n=3, 14%) stage CMP groups (p=0.037). There was no statistically significant difference between the two groups regarding complaints of feeling of knee giving way, knee stiffness, first step limping, sliding of knee cap, locking, clicking sound, crepitation, pain with prolonged sitting, and difficulty in squatting (p>0.05).
In both groups, approximately two-third of the patients had positive Clark and patellar compression test results and one-third had patellar tilt and J sign positivity. Anterior and posterior drawer tests, McMurray tests, varus valgus stress tests, and Ober test results were negative in over 90% of patients in both groups. Muscle strength in all 38 patients was assessed manually. The average measurement in knee flexion test was significantly different between the groups (p=0.038). Twelve patients in advanced stage CMP group (71%) and 15 patients in early stage CMP group (71%) had abnormal Q-angle values indicating pathology. Physical examination findings of the two groups are shown in Table 2.
Table 2.
Physical examination findings of the two groups
| Positive physical examination | Stage 1–2 CMP (early stage, n=21) | Stage 3–4 CMP (advance stage, n=17) | p |
|---|---|---|---|
| Clark | 14 (67) | 11 (65) | 0.899* |
| Patellar compression | 13 (62) | 11 (65) | 0.859* |
| Patellar tilt | 7 (33) | 5 (29) | 0.796* |
| J finding | 6 (29) | 6 (35) | 0.658* |
| Knee flexion measurement | 110 (70–130) | 90 (20–125) | 0.038** |
Data are presented as n (%) or median (min–max); CMP: chondromalacia patellae
Chi square test
Mann–Whitney U test
To evaluate trochlear sulcus dysplasia, trochlear sulcus angle and sulcus depth were measured using MRI images. There was no statistically significant difference between the advanced stage CMP and early stage CMP (p>0.05). However, sulcus angle was above 144°, which is the threshold for trochlear sulcus hypoplasia, in 2 patients with advanced stage CMP (153° and 163°, respectively) and in 1 patient with the early stage CMP group (146°). Regarding the sulcus depth measurement, 2 patients in the advanced stage CMP group had trochlear sulcus dysplasia, and 1 patient in the early stage CMP group had sulcus hypoplasia.
The lateral patellofemoral angle values were not statistically significant different between the two groups (p>0.05). Three patients from the advanced stage CMP group and 1 patient from the early stage CMP group showed medial angulation of the lateral patellofemoral angle. Additionally, although angled laterally, the patellofemoral angle was smaller than 8° in 4 patients with advanced stage CMP and in 6 patients with early stage CMP.
The patellar translation measurements did not show a statistically significant difference between the two groups (p>0.05). Only 2 patients from the advanced stage CMP group had patellar translation values that were consistent with lateral subluxation. There was no patient in the early stage CMP group with a pathological patellar translation value.
The Insall–Salvati index values were also not statistically significant different between the two groups (p>0.05). Patella was in an abnormal position in 70% of patients with advanced stage and early stage CMP (12 and 15 patients, respectively). Table 3 presents the MRI measurement values of the patients.
Table 3.
Comparison of specific measurements made using MRI to determine trochlear dysplasia, patellar subluxation, and patellar placement in groups
| Stage 1–2 CMP (early stage, n=21) | Stage 3–4 CMP (advance stage, n=17) | p | |
|---|---|---|---|
| Sulcus angle | 130 (119–146) | 131.8 (120–163) | 0.240* |
| Sulcus depth (mm) | 6.5 (4.5–8.5) | 6.6 (2–7.8) | 0.640* |
| Lateral patellofemoral angle | 10 (−5–20) | 8.5 (−7–17) | 0.630* |
| Patellar translation (mm) | 3.6 (0.4–7.3) | 3.7 (−6.5–8.3) | 0.480* |
| Insall–Salvati index | 1.2 (0.8–1.4) | 1.2 (0.9–1.5) | 0.410* |
| Patella alta | 6 | 6 | 0.603** |
| Patella baja | 9 | 6 |
Data are presented as median (min–max) or number (n); CMP: chondromalacia patellae
Mann–Whitney U test
chi square test
The patellofemoral pain severity scale score was significantly higher in patients with advanced stage CMP (p = 0.008), whereas the Kujala patellofemoral scores (p=0.012) and functional index questionnaire (p=0.026) were significantly lower when compared to the early stage CMP group. Table 4 shows results from that questionnaire that was applied to assess the level of knee function.
Table 4.
Survey results compared to determine the knee function level of the groups
| Stage 1–2 CMP (early stage, n=21) | Stage 3–4 CMP (advance stage, n=17) | p | |
|---|---|---|---|
| Patellofemoral pain scale (0–80) | 33 (11–57) | 47 (21–69) | 0.008* |
| Kujala patellofemoral score (0–100) | 72 (6–94) | 63.5 (44–82) | 0.012* |
| Functional index survey (0–16) | 9 (6–15) | 8 (3–11) | 0.026* |
Data are presented as median (min–max); CMP: chondromalacia patellae
Mann–Whitney U test
Discussion
Our study demonstrates that the advanced chondromalacia stage is associated with worsened symptom severity and declined knee function. There was no difference between the early and late stage CMP patients regarding their MRI measurement values.
Patellofemoral pain syndrome is a common orthopedic problem that can cause serious disability, and it usually occurs due to CMP. Injury to the patellar cartilage may develop as a result of patellofemoral morphological variations or anatomical incompatibility. This can lead to problems at the joint surface and increase of the mechanical load on the normal joint surface. Therefore, the evaluation of the morphological properties of the patellofemoral joint plays an important role in the diagnosis and treatment of CMP [20]. Although lateral images or tangential images at flexion are recommended for diagnosis, it is difficult to confirm the diagnosis based on these radiograms. The available measurements are inadequate in reflecting the actual patellar alignment, and studies have contradicting results regarding normal measurements of the congruence angles [20, 21]. Arthroscopy is a reliable diagnostic method; however, surgical treatment for CMP is indicated in less than 10% of patients [22]. MRI is the imaging modality that should be chosen for non-interventional diagnosis of CMP [21].
Although literature supports the use of MRI for detecting patellofemoral joint abnormalities, there are not many studies that clearly define and confirm normal and pathological MRI findings in clinical practice. Furthermore, there are only a few studies that examine chondromalacia and patellofemoral joint morphology with MRI [20, 23]. Rubenstein et al. [24] stated that routine clinical MRI images failed to reveal early degenerative changes in the articular cartilage. It is difficult to distinguish small fissure defects in a superficial cartilage injury without arthrography. Studies have shown that routine MRI sequences have high accuracy and precision only in detecting the late-period cartilage lesions [25, 26].
Several studies have investigated the sulcus angle as a risk factor for CMP. However, the relationship between the wide sulcus angle and CMP is not clear [24]. Yang et al. [15] examined 111 patients with anterior knee pain and chronic patellofemoral cartilage lesion who underwent arthroscopy. They reported that patellofemoral cartilage lesions were more frequent if the lateral articular surface was dominant. Additionally, with regard to femoral trochlear morphology, the sulcus depth and relative sulcus depth have shown to be significantly associated with patellofemoral cartilage lesions. Evidence suggests that femoral trochlea with less sulcus depth has a higher risk of patellofemoral cartilage injury [15].
Patellofemoral joint stabilization, which is provided by bone and cartilage, weakens in the presence of trochlear dysplasia. This leads to an increased risk of patellofemoral tracking disorder, instability, dislocation, and ultimately cartilage injury [27]. One study found an association between increased sulcus angle and increased medial and lateral cartilage injury in patients with osteoarthritis. The authors concluded that a wide sulcus accelerated cartilage loss by increasing the pressure on patellofemoral joint surface [28]. Ali et al. [29] compared cases of mild and severe CMP and control group in terms of the degree of patellofemoral incongruence and chondromalacia; they found a difference between severe chondromalacia and non-chondromalacia groups regarding the sulcus angle and trochlear depth. Tuna et al. [20] investigated the relationship between patellofemoral incongruence and the degree of patellofemoral chondromalacia. They found a significant difference between mild and severe chondromalacia groups regarding sulcus angles and trochlear depth. In another study, Endo et al. [30] found equal trochlear depth in axial MRI images of chondromalacia and nonchondromalacia groups.
In our study, we used lateral patellofemoral angle means for the assessment of abnormal patellar tilt. The advanced stage CMP group had an angle of 9.5°, whereas the early stage CMP group had an angle of 10.4°. There was no significant difference between the two groups. Yang et al. [15] showed that patellar tilt or lateral patellar displacement could increase patellofemoral cartilage injury. Tuna et al. [20] found an association of patellar tilt and morphological properties with presence of chondromalacia, but not with the degree.
Patella alta, which is determined using the Insall-Salvati index, is considered a risk factor for CMP [2]. Yang et al. [15] compared patients with anterior knee pain and chronic patellofemoral cartilage lesion who underwent arthroscopy with patients who did not have anterior knee pain, but isolated meniscus rupture. They observed lower frequency of patella alta and baja in the lesion group, while the Insall–Salvati index did not change significantly between the two groups. They concluded that despite variations, these parameters did not have effect on patellofemoral joint injury.
There is conflicting evidence in literature about whether patella alta and baja are associated with cartilage injury [15, 23, 28]. In our study, 31% of all our patients had patella alta and 39% had patella baja. There was no statistically significant difference between early and advanced stage CMP groups regarding the rates of patella alta and baja.
To evaluate the relationship between the chondromalacia stage and severity of pain experienced by patients, patellofemoral pain severity scale scores were used. Patients in the advanced stage CMP group had higher scores. To our knowledge, there are no studies in literature, which examined the relationship between pain severity and disease stage. To evaluate whether knee functions worsen as the disease’s stage advances, we analyzed patients’ scores from the kujala patellofemoral scoring system and functional index questionnaire. Patients in the advanced stage CMP group showed greater decline in their knee functions compared to the early stage CMP group. In literature, only one study prospectively followed up (1–7 years on an average) clinical symptoms in patients who were categorized based on trochlear and patellar cartilage injury in arthroscopy, and found greater functional limitation and more subjective complaints among patients with more severe cartilage injury [6].
There are some limitations of our study. First, there are no clearly defined normal values and methods for MRI measurements. Second, the chondromalacia stage was assessed based on retrospective MRI findings instead of arthroscopy. Third, MRI procedures were not performed during weight-bearing. Also, there was no evaluation of healthy controls in the present study.
In conclusion, the present study indicates that the symptom severity worsens and knee functions decline as the chondromalacia stage advances. However, values obtained from measurements using MRI images were not different between early stage and advanced stage CMP patients. To determine the normal measurement values and their correlation with clinical findings, large-scale prospective studies with control groups are needed.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Katip Çelebi University (Approval number: 2015/45).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - İ.K.A., B.D.M., A.A.; Design - İ.K.A.,B.D.M.; Supervision - İ.K.A., B.D.M.; Resources - E.G., H.K., A.A.; Materials - E.G., H.K., A.A.; Data Collection and/or Processing - İ.K.A., A.A.; Analysis and/or Interpretation - E.G., M.A.; Literature Search -M.A., İ.K.A., H.K.; Writing Manuscript - İ.K.A., E.G., M.A.; Critical Review - İ.K.A., B.D.M., A.A., E.G., M.A., H.K.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Tung GA, Davis LM. The role of magnetic resonance imaging in the evaluation of the soft tissue mass. Crit Rev Diagn Imaging. 1993;34:239–308. [PubMed] [Google Scholar]
- 2.Houghton KM. Review for the generalist: evaluation of anterior knee pain. Pediatr Rheumatol Online J. 2007;5:8. doi: 10.1186/1546-0096-5-8. https://doi.org/10.1186/1546-0096-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly MA. Patellofemoral complications following total knee arthroplasty. Instr Course Lect. 2001;50:403–7. [PubMed] [Google Scholar]
- 4.Ateşalp A. Patellofemoral Eklemin Görüntülenmesi (II. Bölüm) Acta Orthop Traumatol Turc. 1995;29:361–8. [Google Scholar]
- 5.Mattila VM, Weckström M, Leppänen V, Kiuru M, Pihlajamäki H. Sensitivity of MRI for articular cartilage lesions of the patellae. Scand J Surg. 2012;101:56–61. doi: 10.1177/145749691210100111. https://doi.org/10.1177/145749691210100111. [DOI] [PubMed] [Google Scholar]
- 6.Elson DW, Jones S, Caplan N, St Clair Gibson A, Stewart S, Kader DF. Clinically insignificant association between anterior knee pain and patellofemoral lesions which are found incidentally. Knee. 2013;20:471–5. doi: 10.1016/j.knee.2013.02.002. https://doi.org/10.1016/j.knee.2013.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Atbaşı Z, Parlak A, Aytekin A, Kılıç E. The relationship between chondromalacia patella, Q angle and patella type in young male adults with anterior knee pain. Gulhane Med J. 2013;55:89–93. https://doi.org/10.5455/gulhane.39853. [Google Scholar]
- 8.Laprade JA, Culham EG. A self-administered pain severity scale for patellofemoral pain syndrome. Clin Rehabil. 2002;16:780–8. doi: 10.1191/0269215502cr553oa. https://doi.org/10.1191/0269215502cr553oa. [DOI] [PubMed] [Google Scholar]
- 9.Brushøj C, Hölmich P, Nielsen MB, Albrecht-Beste E. Acute patellofemoral pain: aggravating activities, clinical examination, MRI and ultrasound findings. Br J Sports Med. 2008;42:64–7. doi: 10.1136/bjsm.2006.034215. https://doi.org/10.1136/bjsm.2006.034215. [DOI] [PubMed] [Google Scholar]
- 10.Crossley KM, Bennell KL, Cowan SM, Green S. Analysis of outcome measures for persons with patellofemoral pain: which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815–22. doi: 10.1016/s0003-9993(03)00613-0. https://doi.org/10.1016/S0003-9993(03)00613-0. [DOI] [PubMed] [Google Scholar]
- 11.Bennell K, Bartam S, Crossley K, Green S. Outcome measures in patellofemoral pain syndrome: test retest reliability and inter-relationships. Phys Ther Sport. 2000;1:32–41. https://doi.org/10.1054/ptsp.2000.0009. [Google Scholar]
- 12.Kujala UM, Jaakkola LH, Koskinen SK, Taimela S, Hurme M, Nelimarkka O. Scoring of patellofemoral disorders. Arthroscopy. 1993;9:159–63. doi: 10.1016/s0749-8063(05)80366-4. https://doi.org/10.1016/S0749-8063(05)80366-4. [DOI] [PubMed] [Google Scholar]
- 13.Chhabra A, Subhawong TK, Carrino JA. A systematised MRI approach to evaluating the patellofemoral joint. Skeletal Radiol. 2011;40:375–87. doi: 10.1007/s00256-010-0909-1. https://doi.org/10.1007/s00256-010-0909-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salzmann GM, Weber TS, Spang JT, Imhoff AB, Schöttle PB. Comparison of native axial radiographs with axial MR imaging for determination of the trochlear morphology in patients with troch-lear dysplasia. Arch Orthop Trauma Surg. 2010;130:335–40. doi: 10.1007/s00402-009-0912-y. https://doi.org/10.1007/s00402-009-0912-y. [DOI] [PubMed] [Google Scholar]
- 15.Yang B, Tan H, Yang L, Dai G, Guo B. Correlating anatomy and congruence of the patellofemoral joint with cartilage lesions. Orthopedics. 2009;32:20. doi: 10.3928/01477447-20090101-27. https://doi.org/10.3928/01477447-20090101-27. [DOI] [PubMed] [Google Scholar]
- 16.Koskinen SK, Taimela S, Nelimarkka O, Komu M, Kujala UM. Magnetic resonance imaging of patellofemoral relationships. Skeletal Radiol. 1993;22:403–10. doi: 10.1007/BF00538441. https://doi.org/10.1007/BF00538441. [DOI] [PubMed] [Google Scholar]
- 17.McNally EG, Ostlere SJ, Pal C, Phillips A, Reid H, Dodd C. Assessment of patellar maltracking using combined static and dynamic MRI. Eur Radiol. 2000;10:1051–5. doi: 10.1007/s003300000358. https://doi.org/10.1007/s003300000358. [DOI] [PubMed] [Google Scholar]
- 18.Hayes CW, Conway WF. Evaluation of articular cartilage: radiographic and cross- sectional imaging techniques. Radiographics. 1992;12:409–28. doi: 10.1148/radiographics.12.3.1609135. https://doi.org/10.1148/radiographics.12.3.1609135. [DOI] [PubMed] [Google Scholar]
- 19.McCauley TR, Recht MP, Disler DG. Clinical imaging of articular cartilage in the knee. Semin Musculoskelet Radiol. 2001;5:293–304. doi: 10.1055/s-2001-19040. https://doi.org/10.1055/s-2001-19040. [DOI] [PubMed] [Google Scholar]
- 20.Tuna BK, Semiz-Oysu A, Pekar B, Bukte Y, Hayirlioglu A. The association of patellofemoral joint morphology with chondromalacia patella: a quantitative MRI analysis. Clin Imaging. 2014;38:495–8. doi: 10.1016/j.clinimag.2014.01.012. https://doi.org/10.1016/j.clinimag.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 21.Dutton RA, Khadavi MJ, Fredericson M. Patellofemoral Pain. Phys Med Rehabil Clin N Am. 2016;27:31–52. doi: 10.1016/j.pmr.2015.08.002. https://doi.org/10.1016/j.pmr.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Pihlajamäki HK, Kuikka PI, Leppänen VV, Kiuru MJ, Mattila VM. Reliability of clinical findings and magnetic resonance imaging for the diagnosis of chondromalacia patellae. J Bone Joint Surg Am. 2010;92:927–34. doi: 10.2106/JBJS.H.01527. https://doi.org/10.2106/JBJS.H.01527. [DOI] [PubMed] [Google Scholar]
- 23.Kettunen JA, Visuri T, Harilainen A, Sandelin J, Kujala UM. Primary cartilage lesions and outcome among subjects with patellofemoral pain syndrome. Knee Surg Sports Traumatol Arthrosc. 2005;13:131–4. doi: 10.1007/s00167-004-0555-z. https://doi.org/10.1007/s00167-004-0555-z. [DOI] [PubMed] [Google Scholar]
- 24.Rubenstein JD, Li JG, Majumdar S, Henkelman RM. Image resolution and signal- to-noise ratio requirements for MR imaging of degenerative cartilage. AJR Am J Roentgenol. 1997;169:1089–96. doi: 10.2214/ajr.169.4.9308470. https://doi.org/10.2214/ajr.169.4.9308470. [DOI] [PubMed] [Google Scholar]
- 25.Bredella MA, Tirman PF, Peterfy CG, et al. Accuracy of T2-weighted fast spin-echo MR imaging with fat saturation in detecting cartilage defects in the knee: comparison with arthroscopy in 130 patients. AJR Am J Roentgenol. 1999;172:1073–80. doi: 10.2214/ajr.172.4.10587150. https://doi.org/10.2214/ajr.172.4.10587150. [DOI] [PubMed] [Google Scholar]
- 26.Harris JD, Brophy RH, Jia G, et al. Sensitivity of magnetic resonance imaging for detection of patellofemoral articular cartilage defects. Arthroscopy. 2012;28:1728–37. doi: 10.1016/j.arthro.2012.03.018. https://doi.org/10.1016/j.arthro.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 27.Schöttle PB, Fucentese SF, Pfirrmann C, Bereiter H, Romero J. Trochleaplasty for patellar instability due to trochlear dysplasia: A minimum 2-year clinical and radiological follow-up of 19 knees. Acta Orthop. 2005;76:693–8. doi: 10.1080/17453670510041781. https://doi.org/10.1080/17453670510041781. [DOI] [PubMed] [Google Scholar]
- 28.Kalichman L, Zhang Y, Niu J, et al. The association between patellar alignment and patellofemoral joint osteoarthritis features--an MRI study. Rheumatology (Oxford) 2007;46:1303–8. doi: 10.1093/rheumatology/kem095. https://doi.org/10.1093/rheumatology/kem095. [DOI] [PubMed] [Google Scholar]
- 29.Ali SA, Helmer R, Terk MR. Analysis of the patellofemoral region on MRI: association of abnormal trochlear morphology with severe cartilage defects. AJR Am J Roentgenol. 2010;194:721–7. doi: 10.2214/AJR.09.3008. https://doi.org/10.2214/AJR.09.3008. [DOI] [PubMed] [Google Scholar]
- 30.Endo Y, Schweitzer ME, Bordalo-Rodrigues M, Rokito AS, Babb JS. MRI quantitative morphologic analysis of patellofemoral region: lack of correlation with chondromalacia patellae at surgery. AJR Am J Roentgenol. 2007;189:1165–8. doi: 10.2214/AJR.07.2236. https://doi.org/10.2214/AJR.07.2236. [DOI] [PubMed] [Google Scholar]