Abstract
Background
The epidemiology of heart failure (HF) is changing. This study aims to describe questions that arise during the routine care of heart failure (HF) patients that are unanswered by the current literature and describe how the type and focus of these questions has changed over time.
Methods
Investigators from the NHLBI-sponsored Heart Failure Apprentice Network collected and categorized questions from 5 academic hospitals over 12 months. A total of 174 unanswered questions were collected and analyzed.
Results
As compared to 2004, there were more unanswered questions about “whether” to use therapies and fewer about “how” to use therapies. There were fewer questions about what therapeutic targets, therapy adjustment and combination therapies. There were more questions about whether or how to stop therapies and how to add therapies back. Newly prominent topics, not observed in 2004, including novel therapeutics, refractory ventricular tachycardia, right heart failure and nutrition/frailty accounted for 24% of questions.
Conclusions
As compared to 2004, there are fewer unanswered questions about how to use, adjust and combine therapies. There were more unanswered questions about whether and how to stop therapies. Almost 25% of unanswered questions dealt with topics indicative of more advanced disease, not observed in 2004.
Keywords: Heart failure, Epidemiology, Evidence based medicine, Treatment
Introduction
Cardiology is fortunate to have randomized trials and robust guidelines to inform the management of patients with heart failure (HF). However, questions often arise in practice for which there is little or no literature to support one management strategy over another. Such questions are termed “unanswered.” In 2004, Shah and Stevenson fist described a series of these unanswered questions for patients with HF(1). At that time, most questions focused on how to use therapies and the most common question topics included: diuretic strategies, potassium management and the use of neurohormonal therapies.
Since then, many of these questions have been answered but others have arisen to take their place (2–5). Driven in large part by aging demographics and prolonged duration of HF(6), the unanswered questions facing today’s HF cardiologist are different. The primary aim of this study is to describe the unanswered questions that arise during the routine care of HF patients and describe how the type and focus of these questions has changed over time.
Methods
The study was designed and carried out by the Heart Failure Apprentice Network (HFAN), within the National Heart Lung and Blood Institute’s Heart Failure Clinical Research Network.(7) Fellows and junior faculty attendings prospectively identified patients with acute decompensated heart failure (ADHF) at 5 academic medical centers. During daily rounds with the attending HF cardiologist, questions or topics for which the existing HF literature was undecided or silent were recorded as “unanswered questions” by the team. Baseline patient characteristics were also recorded for each patient from whom an unanswered question was identified. Both unanswered questions and patient data were combined and analyzed across sites in a de-identified fashion. This study was either approved or exempted by each center’s IRB. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, North Carolina).
Results
Patients
This study collected data from 134 patients between October 2015 and September 2016. The baseline characteristics are compared to patients in the 2004 unanswered questions study in Table 1 (1). Similar to the 2004, the median age was approximately 60 years, over 60% of patients were male and over 70% were white. Beta blocker use was not measured in the prior study but 45% of the patients in the current study were not on a beta-blocker (35% of HFrEF and 10% of HFpEF patients). Eight-two percent of patients in the current study were not on ACEi/ARB therapy (58% of HFrEF and 24% of HFpEF patients). Almost 40% of patients in the current study required more than 240mg of furosemide/day. Similar to 2004, all patients were derived from academic, referral HF populations.
Table 1.
Comparison of Baseline Characteristics and Comparison to 2004 Study
| 2004 Unanswered Questions Study | Current Unanswered Questions Study | |
|---|---|---|
| N (%) | 57 | 134 |
| Sites Included | 1 | 5 |
| Demographics | ||
| Age | 61 (48, 68) | 62.5 (52, 73) |
| Male (%) | 74 | 64 |
| White (%) | 79 | 72 |
| Heart Failure Characteristics | ||
| Non-Ischemic Etiology (%) | 41 | 69 |
| Likely Transplant/VAD Candidate (%) | – | 23 |
| NYHA 4 (%) | 75 | 42.5 |
| Ejection Fraction (%) | 20 (15, 30) | 30 (20, 45) |
| Days Since Last Hospitalization (days) | 9 (5.5, 15) | 50 (18, 108) |
| Length of Stay (days) | – | 7.5 (4, 15) |
| Vital Signs/Physical Exam | ||
| Systolic Blood Pressure (mmHg) | 110 (90,120) | 113 (100, 128) |
| Diastolic Blood Pressure (mmHg) | 70 (60, 80) | 68 (60, 78) |
| Heart Rate (bmp) | 80 (71, 92.5) | 82 (72, 96) |
| Jugular Venous Pressure (cmH20) | 15 (11, 20) | 13 (10, 15) |
| Laboratory Values | ||
| Sodium (mg/dl) | 138 (133, 141) | 138 (132, 140) |
| Potassium (mg/dl) | 4.1 (3.7, 4.4) | 4.2 (3.8, 4.6) |
| Blood Urea Nitrogen (mg/dl) | 30 (18, 49) | 27 (18, 44.5) |
| Creatinine (mg/dl) | 1.5 (1.1, 2.1) | 1.36 (1.02, 1.99) |
| NT-proBNP (pg/ml)* | – | 4989 (1842, 10250) |
| BNP (pg/ml)* | – | 772 (484, 1182) |
| Medication Doses | ||
| Beta Blocker Total Daily Dose (mg)† | – | 25 (0, 50) |
| N (%) On no Beta Blocker therapy | – | 45 (34) |
| ACEi/ARB Total Daily Dose (mg)‡ | 18.75 (0, 75) | 0 (0, 5) |
| N (%) On no ACEi/ARB therapy | – | 82 (61) |
| Diuretic Total Daily Dose (mg)§ | – | 80 (20, 240) |
| N(%) on >240mg/d Furosemide | – | 37 (28) |
– Indicates that the data was not collected in the 2004 study
NT pro-BNP 22.4% missing, BNP 88.8% missing
Metoprolol equivalents
Lisinopril equivalents
Furosemide equivalents
ACEi: Angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; BNP: B-type natriuretic peptide; NYHA: New York Heart Association; VAD: ventricular assist device
Unanswered Question Type
Of the 174 refractory questions that were collected, 88 (51%) questions addressed “whether” to use a therapy (Group 1) and 86 (49%) questions addressed “how” to use a therapy (Group 2) (Figure 1). As compared to 2004, the spilt between question type was more symmetric. There were more Group 1“whether” questions and fewer Group 2 “how” questions. Among the 88 Group 1 questions, there were similar rates of questions regarding medical, device, surgical and catheter-based therapies as compared to 2004. There was also a new category of Group 1 questions that focused on whether to stop therapy that was not observed in 2004 and accounted for 6% of Group 1 questions. Among the 86 Group 2 questions, there were fewer questions about therapeutic targets and therapy adjustments (17% from 33% of Group 2 questions) and fewer questions how to identify best doses and combine therapies (36% from 63% of Group 2 questions). There were also two new categories of Group 2 questions observed. These focused on how to stop therapy and how to add back therapy. Together, these two new categories comprised 35% of Group 2 questions.
Figure 1.
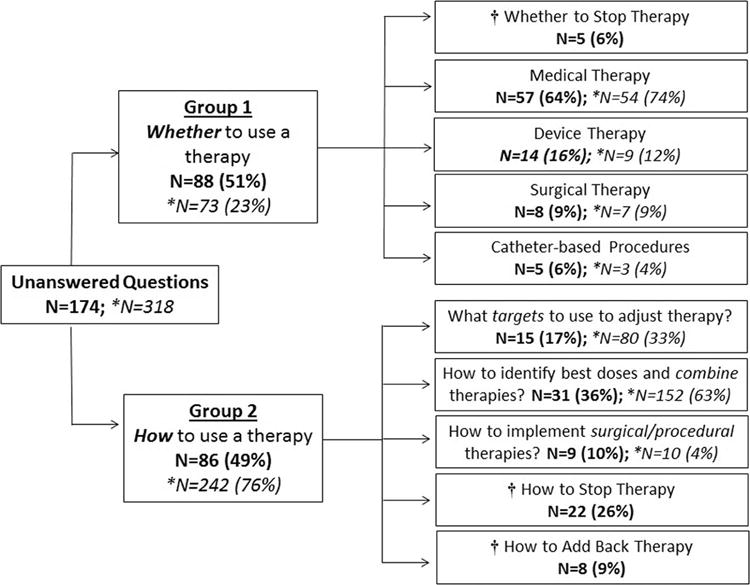
This figure shows the classification of the 174 unanswered questions that were collected. Questions were first classified as either Group 1 “whether” questions or Group 2 “how” questions. Next, the questions were classified by category within their respective groups. The frequencies of the current questions are compared to the 2004 unanswered question analysis.
*Indicates data from the 2004 Unanswered Questions Analysis
†Indicates a new question type, not prominent in 2004
Unanswered Question Topics
The 10 most common unanswered question topics are displayed in Figure 2. A complete list of all 174 unanswered questions can be found in the supplementary material. Questions related to the use of standard HF therapy (ACEi/ARB and beta-blockers) remained the most common topic, though less dominant than in 2004. New topics, not previously in the top 10 list included: the use of novel therapeutics (ivabradine and sacubitril/valsartan), the management of refractory ventricular tachycardia (VT), right heart failure management and nutrition/frailty.
Figure 2.
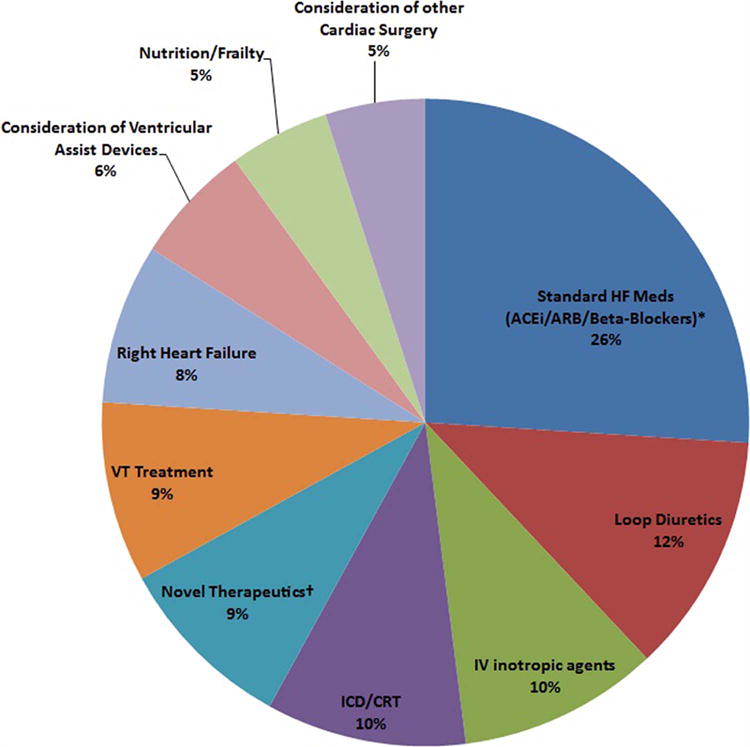
This figure shows the 10 topics that account for 130 of 174 (75%) unanswered questions. The most common question topic was the use of standard therapies, similar to the 2004 unanswered questions analysis. New topics, not previously observed in the 2004 analysis included: the use of novel therapeutics (ivabradine and sacubitril/valsartan), the management of refractory ventricular tachycardia (VT), right heart failure management and nutrition/frailty.
*Standard Heart Failure Medications include: Angiotensin converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARB) and Beta-Blockers
†Novel Therapeutics include: Sacubitril/Valsartan and Ivabradine
CRT: Cardiac resynchronization therapy; HF: heart failure; ICD: Implanted cardiac defibrillator; IV: intravenous; VT: ventricular tachycardia
In 2004, many of the unanswered questions about standard therapies (ACEi/ARB and betablockers) and loop diuretics dealt with how to optimally use, combine and adjust these therapies. In contrast, this study found unanswered questions about whether and how to stop standard therapy, particularly in the setting of concurrent inotropic infusions, and how to add back standard therapies, after an episode of acute decompensation. In addition, this study found a number of answered questions about how to optimally use ivabradine and sacubitril/valsartan. Most questions dealt with how to combine these novel drugs with other therapies and how to use them in patients with marginal hemodynamics. Refractory ventricular tachycardia generated a number of unanswered questions focused on the utility of various therapeutics, the role of imaging and the management of VT in patients with ventricular assist devices. Right heart failure was also newly prominent with unanswered questions pertaining to optimal diuresis strategies, and the appropriateness of advanced therapies in patients with concurrent or predominate right sided HF. Finally, we found a number of new unanswered questions about the assessment and prognostic implications of frailty and how to best manage it with various nutritional therapies.
Discussion
Despite impressive advances in medical and device therapy for HF in recent decades, we report on 174 questions, currently unanswered by the literature. These questions can be used to help guide future research. In addition, we report on how the type and topic of these unanswered questions has changed since 2004. We found an increased number of questions about whether and how to withdraw standard therapies and an increased number of questions about how to reinitiate them. These new question types reflect both the progress of the past decade and a half as well as the more advanced and complex nature of contemporary HF.
This study also found new question topics not previously prominent in 2004. The first of these was the use of novel therapeutics, specifically ivabradine and sacubitril/valsartan. Similar in nature to the type of ACEi/ARB and beta-blocker question seen in 2004, these unanswered questions focused on about how to optimally use, adjust and combine ivabradine and sacubitril/valsartan with other therapies in acute HF setting. The PRIME HF (initiation of ivabradine at discharge)(8), PIONEER-HF study (use of sacubitril/valsartan in inpatients)(9), and LIFE study (upcoming NHLBI Heart Failure Network study examining sacubitril/valsartan in inpatient Class IV inpatients) will hopefully provide guidance.
Refractory VT management was also newly prominent. In 2016, while this study was being conducted, Sapp et al. published the VANISH study which demonstrated the benefit of ablation over escalation of antiarrhythmic therapy in patients with ischemic cardiomyopathy (10). In addition, there has been some work examining the feasibility and utility of VT ablation in patients with VADs (11), but its role remains unclear.
This study also found unanswered questions about right sided HF, specifically “optimal diuretic strategy” questions, reminiscent of those for left sided HF seen in 2004. At present, while some advocate the use of higher dose aldosterone antagonist diuretics (12) and the use of phosphodiesterase type 5 inhibitors to augment diuresis (13), more work is needed to determine therapeutic targets and optimal strategies for these patients.
Finally, as the HF population ages, it is not surprising that issues of frailty and nutrition have become more common. Prior work has suggested that perhaps the best method for assessing frailty should depend upon the therapy being considered (14), but this remains open to debate. Moreover, while we know poor nutrition and frailty are associated with worse outcomes (15, 16), it is unclear how helpful nutritional supplements are in rectifying these issues.
Limitations
The findings of this study are unique to the patient populations from which they were derived, namely patients hospitalized with ADHF at academic referral centers, and are not necessarily representative of the ADHF patient population at large. These results should be interpreted with the clear understanding that the questions are derived from a younger, predominately HFrEF, referral population and that this aspect may impact the study’s findings.
Conclusion
In conclusion, the demographics and epidemiology of HF is changing and we are now caring for an older, sicker population that is less able to tolerate even low doses of drugs proven to decrease morbidity and mortality. While much progress has been made to answer pervious unanswered questions, clinicians now must wrestle with the challenges posed by more advanced disease. Contemporary unanswered questions include new question types such as whether and how to stop or add back standard therapies and well as new question topics such as how to use novel therapeutics in sicker patient populations, how to manage worsening VT, how to manage right sided heart failure and how to assess and address frailty.
Acknowledgments
The authors wish to thank Dr. Margaret Redfield, Dr. Victor Devila-Roman, Dr. W.H. Wilson Tang and Dr. Michael Felker for their support for this project and continued mentorship within the Heart Failure Apprentice Network.
Grants
This work was sponsored by the NHLBI’s Heart Failure Network training grant.
Abbreviations
- HF
heart failure
- HFrEF
heart failure with reduced ejection fraction
- HFpEF
heart failure with preserved ejection fraction
- ACEi
angiotensin converting enzyme inhibitor
- ARB
angiotensin II receptor blocker
- NHLBI
National Heart Lung and Blood Institute
- HFAN
Heart Failure Apprentice Network
- ADHF
acute decompensated heart failure
- VAD
ventricular assist device
- VT
ventricular tachycardia
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
The authors have no relevant disclosures.
References
- 1.Shah MR, Stevenson LW. Searching for evidence: Refractory questions in advanced heart failure. J Card Fail. 2004;10(3):210–8. doi: 10.1016/j.cardfail.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 2.Felker GM, Lee KL, Bull DA, Redfield MM, Stevenson LW, Goldsmith SR, et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med. 2011;364(9):797–805. doi: 10.1056/NEJMoa1005419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bart BA, Goldsmith SR, Lee KL, Givertz MM, O’Connor CM, Bull DA, et al. Ultrafiltration in decompensated heart failure with cardiorenal syndrome. N Engl J Med. 2012;367(24):2296–304. doi: 10.1056/NEJMoa1210357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen HH, Anstrom KJ, Givertz MM, Stevenson LW, Semigran MJ, Goldsmith SR, et al. Low-dose dopamine or low-dose nesiritide in acute heart failure with renal dysfunction: the ROSE acute heart failure randomized trial. JAMA. 2013;310(23):2533–43. doi: 10.1001/jama.2013.282190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wan SH, Stevens SR, Borlaug BA, Anstrom KJ, Deswal A, Felker GM, et al. Differential Response to Low-Dose Dopamine or Low-Dose Nesiritide in Acute Heart Failure With Reduced or Preserved Ejection Fraction: Results From the ROSE AHF Trial (Renal Optimization Strategies Evaluation in Acute Heart Failure) Circ Heart Fail. 2016;9(8) doi: 10.1161/CIRCHEARTFAILURE.115.002593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.CDC. Heart Failure Fact Sheet 2016. [Available from: http://www.cdc.gov/dhdsp/data_statistics/fact_sheets/fs_heart_failure.htm.
- 7.Lala A, Mentz RJ. A call for collaboration: the evolving heart failure apprenticeship network. J Am Coll Cardiol. 2015;65(21):2348–51. doi: 10.1016/j.jacc.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 8.Figueroa JF, Tsugawa Y, Zheng J, Orav EJ, Jha AK. Association between the Value- Based Purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214. doi: 10.1136/bmj.i2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.comParIson Of Sacubitril/valsartaN Versus Enalapril on Effect on ntpRo-bnp in Patients Stabilized From an Acute Heart Failure Episode (PIONEER-HF) ClinicalTrials.gov. 2016 doi: 10.1016/j.ahj.2018.01.004. [Available from: https://clinicaltrials.gov/ct2/show/NCT02554890. [DOI] [PubMed]
- 10.Sapp JL, Wells GA, Parkash R, Stevenson WG, Blier L, Sarrazin JF, et al. Ventricular Tachycardia Ablation versus Escalation of Antiarrhythmic Drugs. N Engl J Med. 2016;375(2):111–21. doi: 10.1056/NEJMoa1513614. [DOI] [PubMed] [Google Scholar]
- 11.Sacher F, Reichlin T, Zado ES, Field ME, Viles-Gonzalez JF, Peichl P, et al. Characteristics of ventricular tachycardia ablation in patients with continuous flow left ventricular assist devices. Circ Arrhythm Electrophysiol. 2015;8(3):592–7. doi: 10.1161/CIRCEP.114.002394. [DOI] [PubMed] [Google Scholar]
- 12.Vazir A. The use of diuretics in acute heart failure: Evidence based therapy? World Journal of Cardiovascular Diseases. 2013 [Google Scholar]
- 13.Berez PB. The successful use of phosphodiesterase type 5 inhibitors to treat the syndrome of cor pulmonale and prerenal azotemia with diuresis of anasarca (CorPRADA) South Med J. 2010;103(2):116–20. doi: 10.1097/SMJ.0b013e3181c98b82. [DOI] [PubMed] [Google Scholar]
- 14.Uchmanowicz I, Loboz-Rudnicka M, Szelag P, Jankowska-Polanska B, Loboz-Grudzien K. Frailty in heart failure. Curr Heart Fail Rep. 2014;11(3):266–73. doi: 10.1007/s11897-014-0198-4. [DOI] [PubMed] [Google Scholar]
- 15.Harkness K, Heckman GA, McKelvie RS. The older patient with heart failure: high risk for frailty and cognitive impairment. Expert Rev Cardiovasc Ther. 2012;10(6):779–95. doi: 10.1586/erc.12.49. [DOI] [PubMed] [Google Scholar]
- 16.Jha SR, Ha HS, Hickman LD, Hannu M, Davidson PM, Macdonald PS, et al. Frailty in advanced heart failure: a systematic review. Heart Fail Rev. 2015;20(5):553–60. doi: 10.1007/s10741-015-9493-8. [DOI] [PubMed] [Google Scholar]


