Abstract
Objective
Caregivers of psychiatrically impaired children experience considerable parenting stress. However, no research has evaluated parenting stress within the context of pediatric bipolar spectrum disorders (BPSD). Thus, the aim of this investigation was to identify predictors and moderators of stress among caregivers in the Longitudinal Assessment of Manic Symptoms (LAMS) study.
Method
Participants included 640 children and their caregivers in the LAMS cohort. Children had a mean age of 9.4±1.9 years (68% male, 23% BPSD); parents had a mean age of 36.5±8.3 years (84% mothers).
Results
Children with BPSD had more service utilization, psychiatric diagnoses, mood and anxiety symptoms, and functional impairment, but fewer disruptive behavior disorders. Caregivers of children with BPSD were more likely than caregivers of children without BPSD to have a partner, elevated depressive symptoms, antisocial tendencies, and parenting stress (Cohen’s d=.49). For the whole sample, higher child IQ, mania, anxiety, disruptive behavior, and caregiver depression predicted increased parenting stress; maternal conduct disorder predicted lower stress. Child anxiety and disruptive behavior were associated with elevated caregiver stress only for non-BPSD children.
Conclusions
Caregivers of children with BPSD experience significant burden and thus require specialized, family-focused interventions. As stress was also elevated, to a lesser degree, among depressed caregivers of children with higher IQ, mania, anxiety, and disruptive behavior, these families may need additional supports as well. Though parents with conduct/antisocial problems evidenced lower stress, these difficulties should be monitored. Thus, parenting stress should be evaluated and addressed in the treatment of childhood mental health problems, especially BPSD.
Keywords: parenting stress, bipolar spectrum disorders, children and adolescents, predictors and moderators, Longitudinal Assessment of Manic Symptoms (LAMS) Study
Parenting can be challenging, even among typically developing, well-adjusted children. However, raising children with medical, developmental, or psychiatric problems is exceptionally difficult, as these children often have special needs that can interfere with both individual and family functioning. Parenting stress refers to the demands, responsibilities, difficulties, physiological reactions, and psychological consequences of caring for a child (Brannan, Heflinger, & Bickman, 1997; Deater-Deckard, 2004). Previous research has examined parenting stress within the context of children’s chronic medical conditions (Cousino & Hazen, 2013) and developmental disabilities (Hayes & Waston, 2013). Most mental health research that has investigated parenting burden has focused on caregivers of adults with serious mental illness (Pompili et al., 2014). Only a handful of studies have examined parenting stress associated with pediatric psychiatric disorders, and even fewer have focused on caregivers of children with bipolar spectrum disorders (BPSD). However, such research can offer important insights for improving existing interventions and identifying families who may require additional support.
Characteristics of Children with BPSD
BPSD include bipolar I and II, cyclothymic disorders, and other specified/unspecified bipolar and related disorders (American Psychiatric Association, 2013). Hallmark symptoms of BPSD include irritability and/or euphoria with increased energy, decreased need for sleep, cognitive changes (e.g., distractibility, grandiosity), and behavioral disturbances (e.g., increase in goal-directed activity, excessive involvement in pleasurable activities with high potential for painful consequences). Depressive episodes, characterized by anhedonia and/or sadness/irritability with associated symptoms (e.g., insomnia/hypersomnia, feelings of worthlessness/guilt, thoughts of death/suicide) are also common in BPSD.
BPSD affects approximately 1–2% of children and adolescents (Van Meter, Moreira, & Youngstrom, 2011). These youth often present with: mixed mood states, rapid mood fluctuations, and psychiatric comorbidity (Axelson et al., 2006; Birmaher et al., 2009a; Geller, Tillman, Bolhofner, & Zimerman, 2008); impairment of global functioning (Axelson et al., 2006), psychosocial adjustment (Goldstein et al., 2009), and family functioning (Keenan-Miller, Peris, Axelson, Kowatch, & Miklowitz, 2012); poor quality of life (Freeman et al., 2009); and suicidality (Hauser, Galling, & Correll, 2013). In addition, BPSD has been considered the fourth leading cause of youth disability worldwide (Gore et al., 2011). Thus, these children and families often require extensive treatment to manage chronic impairing symptoms and associated difficulties (Evans-Lacko, Spencer, Logan, & Riley, 2010; Rizzo et al., 2007).
Families of Children with BPSD
Development of BPSD results from the interaction of genetic and environmental factors (Youngstrom & Algorta, 2014), and BPSD is among the most heritable of psychiatric disorders (Mick & Farone, 2009). Offspring of parents with BPSD are at heightened risk for developing mental health problems, especially BPSD and other mood disorders (Birmaher et al., 2009b; Mesman, Nolen, Reichart, Wals, & Hillegers, 2013). Furthermore, it is common for biological parents and relatives of children with BPSD to also have BPSD and other psychiatric conditions (Arnold et al., 2012; Brotman et al., 2007; Geller et al., 2006).
Although genetics plays an important role, familial transmission of BPSD may also be influenced by family functioning (Algorta, Van Meter, & Youngstrom, 2015). Families of children at risk and who actually have BPSD show dysfunctional interactions, including high levels of: conflict (Barron et al., 2014; Belardinelli et al., 2008; Chang, Blasey, Ketter, & Steiner, 2001; Ferreira et al., 2013; Nader et al., 2013); control (Ferreira et al., 2013; Nader et al., 2013); aggression (Keenan-Miller et al., 2012); quarreling (Schenkel, West, Harral, Patel, & Pavuluri, 2008); forceful punishment (Schenkel et al., 2008); parental tension (Nader et al., 2013); and negative expressed emotion (Nader et al., 2013). These families also demonstrate low levels of: warmth, affection, and intimacy (Schenkel et al., 2008); cohesion (Belardinelli et al., 2008; Chang et al., 2001; Ferreira et al., 2013; Nader et al., 2013); expressiveness (Barron et al., 2014; Belardinelli et al., 2008); organization (Barron et al., 2014; Belardinelli et al., 2008; Chang et al., 2001; Ferreira et al., 2013; Nader et al., 2013); intellectual-cultural orientation (Barron et al., 2014; Belardinelli et al., 2008; Ferreira et al., 2013); active-recreational orientation (Barron et al., 2014; Belardinelli et al., 2008; Ferreira et al., 2013); moral-religious emphasis (Ferreira et al., 2013); and positive expressed emotion (Nader et al., 2013). In addition, worse longitudinal course of BPSD is predicted by impaired family characteristics, such as: low maternal warmth (Geller et al., 2008); chronic stress in family, romantic, and peer relationships (Kim, Miklowitz, Biuckians, & Mullen, 2007; Siegel et al., 2015); frequency and severity of independent family stressful life events (Kim et al., 2007); low levels of cohesion and adaptability (Sullivan, Judd, Axelson, & Miklowitz, 2012); and high levels of conflict (Sullivan et al., 2012). Interestingly, one study found a small but significant indirect pathway from parental mood disorder to childhood BPSD via increased family conflict (Du Rocher Schudlich, Youngstrom, Calabrese, & Findling, 2008). Thus, functional deficits are evident in families when a parent and/or a child has BPSD, which can impact onset and course of the disorder, further supporting the role of both genetics and environmental factors in the familial transmission of BPSD.
Parenting Stress among Caregivers of Children with Psychiatric Impairment
Given the chronic and impairing nature of BPSD and associated familial problems, parents of these children, regardless of their own psychiatric history, experience a significant amount of stress, which can influence their parenting abilities and family functioning. Objective factors related to the parent (e.g., balancing work and family) and child (e.g., problematic behavior), subjective parent factors (e.g., parents’ emotional experience related to the child or parenting), and characteristics of the parent-child relationship (e.g., quality of interactions) contribute to parenting stress (Brannan et al., 1997; Abidin, 1992). Thus, as a result of stigmatization and the time, energy, and coordination involved in caring for a psychiatrically impaired child, parents experience considerable stress, diminished interpersonal/family relationships, financial pressure of treatment costs and reduced ability to work, compromised self-care, impaired parenting ability, and strained emotional/physical well-being (Hellander, Sisson, & Fristad, 2003; Mendenhall & Mount, 2011; Nadkarni & Fristad, 2012).
While the relationship between parenting stress and childhood psychopathology appears to be transactional (Mackler et al., 2015; Stone, Mares, Otten, Engels, & Janssens, 2016), and thus the directionality of effects is not well understood, several predictors of caregiver burden have been identified, including: children’s symptom severity, functional impairment, and type of mental illness; and parents’ age, race/ethnicity, psychiatric history, and perceived amount of social support (Mendenhall & Mount, 2011). Specifically, parenting stress is more pronounced if caregivers are older (Schoeder & Remer, 2007), Caucasian (McCabe, Yeh, Lau, Garland, & Hough, 2003), psychiatrically impaired (Angold et al., 1998), with attention-deficit/hyperactivity disorder (ADHD) symptoms (Algorta et al., 2014; Wiener, Biondic, Grimbos, & Herbert, 2016), depressive symptoms (Theule, Wiener, Tannock, & Jenkins, 2013), or lower perceived social support (Schoeder & Remer, 2007). Child characteristic predictors of parenting stress include greater functional impairment (Angold et al., 1998), more severe psychiatric symptoms (Angold et al., 1998; Yatchmenoff et al., 1998), increased Tourette’s disorder symptoms (Schoeder & Remer, 2007; Stewart, Greene, Lessov-Schlaggar, Church, & Schlaggar, 2015), externalizing behaviors (Algorta et al., 2014; Anderson, 2008; Bussing et al., 2003a; Bussing et al., 2003b; Mackler et al., 2015; McDonald, Gregoire, Poertner, & Early, 1997; Stone et al., 2016; Theule et al., 2013; Tzang, Change, & Liu, 2009; Vaughan, Feinn, Bernard, Brereton, & Kaufman, 2013), and high rates of internalizing symptoms (Bussing et al., 2003a; Bussing et al. 2003b; Deater-Deckard, 2004; Stone et al., 2016; Vaughan et al., 2013).
Few investigations have identified moderators of parenting stress, although this is a potentially important area given results from the sparse extant literature. For example, one study reported that while parenting stress was significantly higher in mothers of children with ADHD compared to mothers of children without ADHD, this difference became non-significant when mothers’ own ADHD symptoms were 1SD above the pooled sample mean (Algorta et al., 2014)—i.e., mothers with ADHD found parenting stressful regardless of whether the child had ADHD. Thus, disorganization within the family appeared stressful whether the source was maternal or child ADHD symptoms. These results suggest that screening for both child and parental psychopathology may identify families that require additional supports. Moderation findings such as these have valuable treatment and clinical implications.
Despite growing literature on predictors and moderators of stress among caregivers of children with psychiatric diagnoses, no studies have focused specifically on BPSD, even with high rates of parenting stress apparent in this population (Hellander et al., 2003; Fristad et al., 2012; Nadkarni & Fristad, 2012). Study of predictors and moderators can elucidate variables associated with stress and identify subgroups that may be more vulnerable to stress, and such information can help inform improved interventions. For example, Evidence-Based Treatments (EBTs) for BPSD largely seek to improve children’s mood dysregulation by targeting not only child coping, but also parent and family functioning via psychoeducation, communication, problem solving, affect regulation, self-care, and advocacy skills (Fristad & MacPherson, 2014). Interestingly, parental psychopathology predicts increased mood severity in children if parents have low, but not average or high, coping skills (Peters, Henry, & West, 2014). In addition, while poor child functioning has been implicated as a treatment moderator for pediatric BPSD (MacPherson, Algorta, Mendenhall, Fields, & Fristad, 2014), parent and family variables also moderate treatment outcomes. Specifically, moderators include elevated parent depression (Weinstein, Henry, Katz, Peters, & West, 2015), low income (Weinstein et al., 2015), elevated negative expressed emotion (Miklowitz et al., 2009), and increased conflict (Sullivan et al., 2012), with more impaired children and families generally benefitting most from EBTs for BPSD. Finally, parent and family constructs can mediate improvements in child mood symptoms and functioning in response to EBTs. These factors include: parents’ positive beliefs about treatment (Mendenhall, Fristad, & Early, 2009), parents’ ability to access high quality services for children (Mendenhall et al., 2009), and the use of effective parenting and coping skills, family flexibility, and positive reframing of problems (MacPherson, Weinstein, Henry, & West, 2016). Thus, identification of variables associated with impaired parent coping and/or negative family processes, such as parenting stress, can indicate families that may require more specialized interventions, treatment targets, and mechanisms for enhancing and tailoring EBTs.
Purpose of Current Study
Given limited research on pediatric BPSD and parenting stress, the current study used secondary data analyses to explore characteristics of children with and without BPSD and their caregivers, and to identify predictors and moderators of caregiver stress. Based on prior research, it was expected that children with BPSD, as compared to those with other psychiatric diagnoses, would have a more extensive treatment history, greater number of psychiatric diagnoses, increased internalizing and externalizing symptoms, and worse functional impairment. Caregivers of children with BPSD, as compared to those of children without BPSD, were hypothesized to have more severe mood symptoms, greater parenting stress, and higher rates of psychiatric problems. Regarding predictors, we hypothesized that parenting stress would be more pronounced among caregivers if they were older, had mental health problems, or had a child with exacerbated symptoms, greater functional impairment, and/or a greater number of disorders. Exploratory analyses examined moderators of parenting stress between caregivers of children with BPSD and those of children without BPSD. Limited prior research on this topic precluded development of directional hypotheses.
Method
Participants and Procedures
The current study performed secondary analyses on baseline data from the Longitudinal Assessment of Manic Symptoms (LAMS) study (11/14/2005-11/28/2008), which enrolled 621 children with elevated symptoms of mania (ESM+) and 86 psychiatric controls without elevated symptoms of mania (ESM-). LAMS study participants and methodology have been described previously (Findling et al., 2010; Horwitz et al., 2010); the sample included 707 children ages 6–12 years (M=9.4±1.9, 67.6% male) presenting for initial assessment at nine outpatient psychiatric clinics affiliated with four Midwestern universities. Only one child per household could participate. One parent/guardian was selected as the primary informant. Most primary caregivers self-identified as biological mothers (82%) or biological fathers (5%). However, 13% of primary caregivers reported a different relationship to the child (i.e., adoptive mothers/fathers, step mothers/fathers, grandparents, other family members, legal guardians). Under-representation of some caregiver categories precluded comparison across caregiver groups. Only baseline data from families with a caregiver Parent Stress Survey (PSS; Sisson & Fristad, 2001) and complete child information were used in the current investigation (N=640), as the PSS was the primary outcome of interest. This subsample did not differ significantly on any demographic or clinical variables from the complete LAMS sample. University Institutional Review Boards oversaw and approved all study procedures.
Measures
Demographics
Parents/guardians provided demographic information about children (age, sex, race) and themselves (age, race, health insurance status as proxy for socioeconomic status, education, employment, income, marital status, family structure). Children’s medication usage and hospitalization history was captured on the parent-report version of the Services Assessment of Children and Adolescents (SACA; Hoagwood et al., 2000). Children’s intellectual capacity was measured via the Wechsler Abbreviated Scale of Intelligence, which has well-established reliability and validity (WASI; Wechsler, 1999).
Diagnostic Assessment
Children and caregivers were administered the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Episode with additional depression and manic symptom items derived from the Washington University in St. Louis Kiddie Schedule for Affective Disorders (K-SADS-PL-W; Geller et al., 2001; Kaufman et al., 1997). This semi-structured interview assesses current and lifetime psychiatric symptoms and diagnoses according to DSM-IV criteria. All diagnoses were reviewed by a licensed child psychiatrist or psychologist. The K-SADS-PL-W demonstrated good inter-rater reliability in the current study (k=0.82).
DSM-IV diagnostic criteria were used in the LAMS study. The criteria for bipolar disorder not otherwise specified (BP-NOS) followed the same criteria used in the Course and Outcome of Bipolar Youth study (COBY; Axelson et al., 2006). BP-NOS was operationalized by: a) elated mood plus two associated symptoms of mania (e.g., grandiosity, decreased need for sleep, pressured speech, racing thoughts, increased goal-directed activity, etc.), or irritable mood plus three associated symptoms of mania; b) change in the child's level of functioning (increase or decrease); c) symptoms must be present for a total of at least four hours within a 24-hour period; and d) the participant must have had at least four episodes of four hours duration or a total of four days of the above-noted symptom intensity in his/her lifetime.
Child Symptom Severity
Children’s manic symptoms were measured via the Young Mania Rating Scale (YMRS; Young, Biggs, Ziegler, & Meyer, 1978). The YMRS is an 11-item, clinician-rated interview conducted with both children and caregivers. Items use a 0–4 or 0–8 scale. Total scores range from 0–60; higher scores indicate greater severity. Validity and reliability have been established with both adults and children. When used with children, the YMRS total score demonstrated adequate internal consistency (α=.75 in the present sample) (see also Youngstrom, Danielson, Findling, Gracious, & Calabrese, 2002). In the LAMS sample, unfiltered administration (i.e., regardless of whether symptoms occurred within a mood episode) of YMRS achieved good discriminative validity when classifying BPSD versus other disorders (Yee et al., 2015).
Children’s manic symptoms were also measured via the Parent General Behavior Inventory-10 Item Mania Scale (PGBI-10M; Youngstrom, Frazier, Demeter, Calabrese, & Findling, 2008). The 10-item PGBI-10M is a parent rating of child symptoms using a 0–3 scale. Total scores range from 0–30; higher scores indicate greater severity. The PGBI-10M utilizes 10 items from the 73-item Parent General Behavior Inventory (PGBI; Youngstrom, Findling, Danielson, & Calabrese, 2001; Youngstrom et al., 2008) that best discriminate bipolar disorder from other diagnoses. It has excellent internal consistency (α=.89 in the present sample), discriminative validity, and diagnostic efficiency (Youngstrom et al., 2008).
Children’s depressive symptoms were measured via the Children’s Depression Rating Scale-Revised (CDRS-R; Poznanski et al., 1984). The CDRS-R is a 17-item, clinician-rated interview conducted with both children and caregivers. Items use either a 1–5 or 1–7 scale. Total scores range from 17–113; higher scores indicate greater severity. The CDRS-R total score has adequate inter-rater reliability (r=.86), test-retest reliability (r=.81), and validity (Poznanski et al., 1984). In the LAMS sample, unfiltered administration of CDRS-R achieved moderate to good discriminative validity when classifying depressive disorders versus other disorders (Yee et al., 2015), with an alpha of .66 in the present sample.
Parents reported on their children’s anxiety symptoms via the Screen for Child Anxiety Related Emotional Disorders-Parent Version (SCARED-P; Birmaher et al., 1997). Forty-one items are scored on a 0–2 scale. Total scores range from 0–82; higher scores indicate greater severity. SCARED-P scores have shown good internal consistency (α=0.90), test-retest reliability (r=.86), discriminative validity (between anxiety and other disorders and within anxiety disorders), and moderate parent-child agreement (Birmaher et al., 1999; Birmaher et al., 1997), with alpha = .95 in the present sample.
Child Functioning
Functional impairment was evaluated via the clinician-rated Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983). Total scores on this clinical rating scale range from 1 (severe impairment) to 100 (superior functioning).
Maternal Psychopathology
Caregivers provided information regarding maternal psychopathology, using the Family History Screen (FHS; Weissman et al., 2000). The clinician-administered FHS collects information on 15 psychiatric disorders and suicidality. It has adequate sensitivity, specificity, and test-retest reliability. Validity is best demonstrated for major depression, anxiety disorders, substance dependence, and suicide attempts (Weissman et al., 2000). As the items are causal indicators, internal consistency reliability is not conceptually appropriate (Streiner, Norman, & Cairney, 2015); the scores have demonstrated criterion validity in the present cohort (Fristad et al., 2012).
Caregiver Mood Severity
Caregivers reported on their own symptoms of hypomania and depression on the 73-item, self-report General Behavior Inventory (GBI; Depue et al., 1987). Items use a 0–3 scale; higher scores indicate greater severity. The depression scale is comprised of 46 items and the hypomania scale of 28 items. The GBI scores have consistently shown good diagnostic efficiency (Depue, Krauss, Spoont, & Arbisi, 1989; Pendergast et al., 2014), and alpha of .92 and .94 for the scales in the present sample.
Caregiver Parenting Stress
The Parent Stress Survey (PSS; Sisson & Fristad, 2001) is a 25-item self-report questionnaire that assesses parent/caregiver stress related to raising a psychiatrically impaired child. Each item has a yes/no response to document occurrence of event, followed by a Likert-type scale, with response choices ranging from 0 (not at all stressful) to 4 (very stressful), to measure severity of stress. Total score is the item sum, which ranges from 0 (no stress) to 100 (high stress). Scores show good internal consistency (α=.84 in the present sample) and are sensitive to differences in parenting stress across child diagnostic groups (Fristad et al., 2012). Example items from the PSS include: “Pressure from work because of absence due to your child’s illness” and “Walking on eggshells around your child to avoid rages.”
Analyses
Chi-square and independent samples t-tests compared descriptive statistics between children with (n=149) and without BPSD (n=491) and their caregivers. In the current study, the BPSD group included children with bipolar I disorder (n=66), bipolar II disorder (n=3), cyclothymia (n=10), and BP-NOS (n=69; now called other specified/unspecified bipolar and related disorders; American Psychiatric Association, 2013).
We used standard definitions of predictors and moderators (Kraemer et al., 2002). Complete data were necessary for initial selection of predictors. A complete data set with a pool of 38 candidate predictors of parenting stress, including variables related to demographics, medical history, comorbidity, and general functioning (listed in Tables 1 and 2), was passed to L1-regularized logistic regression (Least Absolute Shrinkage and Selection Operator: LASSO) to prevent overfitting models and to support parsimony in predictor selection. LASSO was conducted through the “glmnet” package in R (James, Witten, Hastie, & Tibshirani, 2013).
Table 1.
LAMS Study Child Characteristics at Baseline
| Variables | Non-BPSD n=491 |
BPSD n=149 |
Statistic t or χ2 |
|---|---|---|---|
| Demographics | |||
| Age, (M±SD) | 9.28±1.86 | 9.83±2.07 | −3.07** |
| Gender, Male, n(%) | 351(72) | 85(57) | 10.98** |
| Race, White, n(%) | 310(63) | 103(69) | 1.79 |
| IQ, (M±SD) | 98.39±15.92 | 96.29±16.94 | 1.39 |
| Number of Baseline Diagnoses, (M±SD) | 2.36±1.25 | 2.91±1.26 | −4.75*** |
| Number of Baseline Medications, (M±SD) | .94±.98 | 1.42±1.24 | −4.93*** |
| Ever Hospitalized, yes, n(%) | 23(5) | 33(22) | 43.66*** |
| Baseline Medications, yes, n(%) | 295(60) | 109(73) | 8.39** |
| Functioning | |||
| CGAS, (M±SD) | 55.79±10.36 | 51.21±9.49 | 4.82*** |
| Symptom Severity | |||
| YMRS Mania, (M±SD) | 14.17±7.54 | 25.45±8.96 | −15.30*** |
| PGBI-10 Mania, (M±SD) | 16.42±6.25 | 18.42±5.52 | −3.50*** |
| CDRS-R Depression, (M±SD) | 33.74±10.40 | 39.17±11.00 | −5.50*** |
| SCARED-P Anxiety, (M±SD) | 17.44±13.98 | 20.62±12.86 | −2.47** |
| Current Diagnoses | |||
| Any Depressive Disorders, yes, n(%)1 | 108(22) | 0(0) | −- |
| Any Disruptive Behavior Disorders, yes, n(%) | 263(54) | 65(44) | 4.52** |
| Any Psychotic Disorder, yes, n(%) | 13(3) | 3(2) | .189 |
| Any Anxiety Disorder, yes, n(%) | 156(32) | 47(32) | .003 |
| Any Elimination Disorder, yes, n(%) | 86(18) | 37(25) | 3.94* |
| Any ADHD, yes, n(%) | 382(78) | 109(73) | 1.38 |
| Any Pervasive Developmental Disorders, yes, n(%) | 36(7) | 4(3) | 3.46 |
| Any Posttraumatic Stress Disorder, yes, n(%) | 9(2) | 4(3) | .099 |
| Family Structure | |||
| Any Siblings of Proband, yes, n(%) | 442(92) | 136(93) | .151 |
| Full Biological Siblings, (M±SD) | .94±1.10 | 1.04±1.10 | −.973 |
| Half-Biological Siblings, (M±SD) | .76±1.24 | .84±1.11 | −.607 |
| Step-Siblings, (M±SD) | .14±.66 | .07±.30 | 1.18 |
Note. LAMS = Longitudinal Assessment of Manic Symptoms; BPSD = Bipolar Spectrum Disorders; IQ = Intellectual Quotient; CGAS = Children’s Global Assessment Scale; YMRS = Young Mania Rating Scale; PGBI-10M = Parent General Behavior Inventory-10 Item Mania Scale; CDRS-R = Children’s Depression Rating Scale-Revised; SCARED-P = Screen for Child Anxiety Related Emotional Disorders-Parent Version; ADHD = Attention-Deficit/Hyperactivity Disorder.
p<.05;
p<.01;
p<.001.
If children received a diagnosis of BPSD, their prior depressive diagnoses were not recorded as a current diagnosis.
Table 2.
LAMS Study Caregiver and Family Characteristics at Baseline
| Variables | Non-BPSD n=491 |
BPSD n=149 |
Statistic t or χ2 |
|---|---|---|---|
| Demographics | |||
| Age, (M±SD) | 36.66±8.73 | 36.97±6.92 | .880 |
| Medicaid Status, yes, n(%) | 260(53) | 73(49) | .718 |
| Education, Attended High School, n(%) | 484(99) | 145(97) | 1.07 |
| Employed, yes, n(%) | 293(60) | 85(57) | .326 |
| Income, <$20,000, n(%) | 238(49) | 72(48) | .001 |
| Marital Status, Single vs Other, n(%) | 117(24) | 23(15) | 4.71* |
| Maternal Psychopathology | |||
| Total Number of Diagnoses, (M±SD) | 2.56±2.79 | 2.98±3.12 | −1.57 |
| Lifetime Mania, yes, n(%) | 41(9) | 30(22) | 15.58*** |
| Lifetime Depression, yes, n(%) | 256(52) | 66(45) | 6.51* |
| Lifetime ADHD, yes, n(%) | 62(13) | 20(13) | .065 |
| Lifetime Psychosis, yes, n(%) | 29(6) | 12(8) | .879 |
| Number of Anxiety Disorders, (M±SD) | 1.00±1.52 | 1.04±1.55 | −.311 |
| Lifetime Alcohol Dependence, yes, n(%) | 65(13) | 16(11) | .646 |
| Lifetime Drug Dependence, yes, n(%) | 62(13) | 16(11) | .381 |
| Lifetime Conduct Disorder, yes, n(%) | 119(24) | 42(28) | .948 |
| Lifetime Antisocial Personality Disorder, yes, n(%) | 89(18) | 43(29) | 8.04** |
| Caregiver Psychopathology | |||
| GBI Depression, (M±SD) | 31.40±27.27 | 36.14±30.57 | −1.80 |
| GBI Hypomania, (M±SD) | 15.07±14.60 | 17.51±16.67 | −1.72 |
| Caregiver Parenting Stress | |||
| Parent Stress Survey, (M±SD) | 18.31±12.64 | 24.34±14.10 | −4.97*** |
Note. LAMS = Longitudinal Assessment of Manic Symptoms; BPSD = Bipolar Spectrum Disorders; ADHD = Attention-Deficit/Hyperactivity Disorder; GBI = General Behavior Inventory.
p<.05;
p<.01;
p<.001.
The final list of predictors was then entered in a single model combining child and caregiver information. A multiple regression model tested the main effect and interaction term for each candidate predictor × caregiver group (BPSD vs. non-BPSD; Aiken & West, 1991; Cohen, Cohen, West, & Aiken, 2003). Continuous variables were centered on the sample mean. Given the sample size, power was >.80 to detect even small effects: the critical effect size would be f2=.012 for pcrit<.05, .017 for p<.017, and .025 for p<.00125 (using a Bonferroni correction; Faul, Erdfelder, Buchner, & Lang, 2009). Testing interactions necessarily involves a large number of predictors. To balance concerns about Type I error, we interpreted interactions that produced at least “small” effects in Cohen’s convention (f2~.02 is small, .15 medium, .35 large), which also would survive a Bonferroni or False Discovery Rate (FDR) correction. However, we also listed p<.05 interactions as “hypothesis generating” findings for future study and replication. When a significant and potentially meaningful (f2>.02) two-way interaction indicated significant differences in slopes between groups, simple slope analyses were conducted using the Preacher approach (Preacher, Currant & Bauer, 2006) and effect displays (Fox, 2003).
Results
Characteristics of Children with vs. without BPSD and their Caregivers
Within this predominantly male sample, compared to children without BPSD, children with BPSD had: a greater number of baseline psychiatric diagnoses and medications; higher lifetime hospitalization rates; more severe symptoms of mania, depression, and anxiety; worse global functioning; higher rates of elimination disorders; and lower rates of disruptive disorders (see Table 1).
Primary informants/caregivers of children with BPSD were less likely to be single but endorsed higher rates of parenting stress than caregivers of children without BPSD (Cohen’s d=.49; see Table 2). In addition, caregivers of children with BPSD reported more severe mania and depression, and higher rates of antisocial personality disorder than did caregivers of children without BPSD. Age of caregivers did not differ between BPSD- and non-BPSD groups.
Predictors of Stress for Caregivers Regardless of Child BPSD
We used a shrinkage method (LASSO) splitting the sample into a training set and a test set, to select relevant variables related to parenting stress. Of the original 38 candidate predictors, the estimated coefficients of 20 were shrunken toward zero and finally excluded from the model. We then evaluated for the presence of influential cases and outliers. After close inspection of different diagnostic indices, a single case with a studentized residual of 5.09 was removed from the final sample.
Regarding child characteristics, higher IQ, more severe symptoms of mania (YMRS) and anxiety (SCARED-P), and presence of any disruptive behavior disorder were associated with increased caregiver stress (see Table 3). In terms of caregiver characteristics, higher depressive symptoms (GBI) were associated with increased caregiver stress; maternal lifetime presence of conduct disorder was associated with lower stress levels.
Table 3.
Predictors and Moderators of Parenting Stress in the LAMS Cohort
| Adj. R2 | B | 95% CI | |
|---|---|---|---|
|
|
|||
| .38*** | |||
| Constant | 15.74 | 13.29, 18.19 | |
| Child Characteristics | |||
| Age | .36 | −.15, .86 | |
| Race, White | 1.75 | −.57, 4.06 | |
| IQ | .06 | .002, .13 | |
| Number of Baseline Diagnoses | −.32 | −1.40, .75 | |
| Number of Baseline Medications | .85 | −.18, 1.87 | |
| Ever Hospitalized, yes | 3.69 | −.70, 8.08 | |
| YMRS Mania | .19 | .05, .33 | |
| CDRS-R Depression | .09 | −.02, .20 | |
| SCARED-P Anxiety | .18 | .10, .26 | |
| Any Disruptive Behavior Disorders | 3.36 | 1.13, 5.59 | |
| Any Pervasive Developmental Disorders | −1.64 | −5.38, 2.09 | |
| Any Elimination Disorders | 2.72 | −.06, 5.51 | |
| Caregiver Characteristics | |||
| Medicaid Status, yes | 1.01 | −1.19, 3.21 | |
| GBI Depression | .18 | .13, .22 | |
| Maternal Psychopathology | |||
| Number of Anxiety Disorders | .48 | −.22, 1.18 | |
| Lifetime ADHD | 2.60 | −.34, 5.55 | |
| Lifetime Conduct Disorder | −2.65 | −5.07, −.23 | |
| Caregiver Group (CG; BPSD vs. Non-BPSD Child) | 3.88 | −1.28, 9.03 | |
| CG*Age | .09 | −.95, 1.12 | |
| CG*Race, White | −2.44 | −7.24, 2.36 | |
| CG*IQ | .11 | −.02, .24 | |
| CG*Number of Baseline Diagnoses | 1.71 | −.82, 4.25 | |
| CG*Number of Baseline Medications | .98 | −.87, 2.82 | |
| CG*Ever Hospitalized, yes | 1.64 | −4.67, 7.96 | |
| CG*YMRS Mania | .05 | −.20, .30 | |
| CG*CDRS-R Depression | .03 | −.18, .24 | |
| CG*SCARED-P Anxiety | −.18 | −.35, −.02 | |
| CG*Any Disruptive Behavior Disorders | −5.47 | −10.76, −.18 | |
| CG*Any Pervasive Developmental Disorders | −5.13 | −16.85, 6.59 | |
| CG*Any Elimination Disorders | −4.03 | −9.71, 1.65 | |
| CG*Medicaid Status, yes | 2.38 | −2.14, 6.89 | |
| CG*GBI Depression | −.02 | −.09, .06 | |
| CG*Number of Anxiety Disorders | −.25 | −.71, 1.22 | |
| CG*Lifetime ADHD | −4.11 | −10.28, 2.06 | |
| CG*Lifetime Conduct Disorder | −.29 | −5.33, 4.75 | |
F(35, 603) = 12.01, p<.00001.
Note. BPSD = Bipolar Spectrum Disorders; IQ = Intellectual Quotient; YMRS = Young Mania Rating Scale; CDRS-R = Children’s Depression Rating Scale-Revised; SCARED-P = Screen for Child Anxiety Related Emotional Disorders-Parent Version; CG = Caregiver Group; CI = Confidence Interval. Values in bold text reflect statistically significant (p<.05) findings.
p<.001
Moderators of Stress for Caregivers of Children with vs. without BPSD
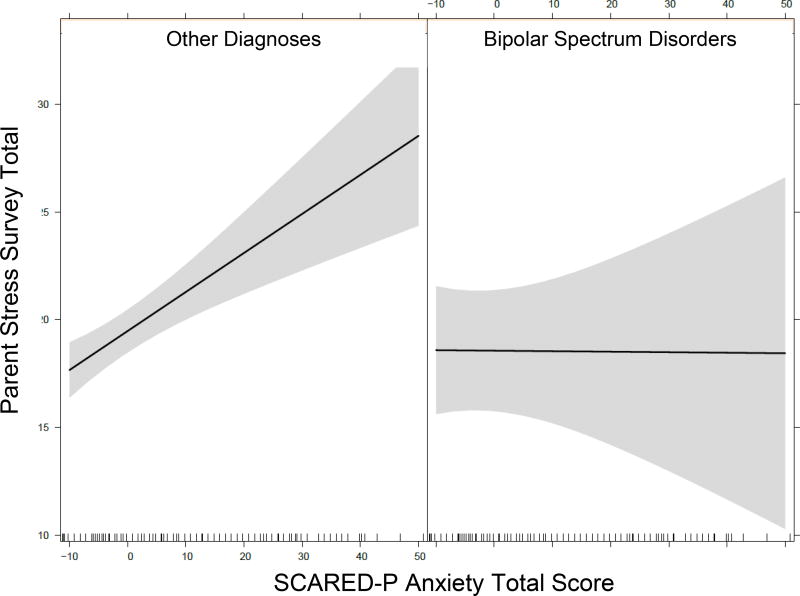
When considering caregiver group (CG) in the model, there were two significant interaction effects. First, caregivers of children with BPSD differed from those without BPSD in the level of association between caregiver stress and child anxiety symptoms (CG*SCARED-P b=−.17, 95% CI [−.35, − .02]; see Figure 1). Specifically, SCARED-P scores were positively associated with caregiver parenting stress in the non-BPSD group (b=.18, SE=.04, t=4.39, p<.0001) but not in the BPSD group (b=−.002, SE=.07, t=−0.03, p>.95).
Figure 1.
Increasing child anxiety predicts increasing stress in parents of youths without BPSD (left panel), but not among those with BPSD (right panel). SCARED-P = Screen for Child Anxiety Related Emotional Disorders-Parent Version. SCARED-P (x-axis) was centered on the pooled sample mean.
Caregiver groups also differed in the level of association between caregiver stress and the presence of any child disruptive behavior disorder (CG*any DBD b=−5.47, 95% CI [-10.76, −.18]). The estimated mean of caregivers’ stress levels was significantly higher for those with children with versus without any disruptive behavior disorder (b=21.10, 95% CI [19.75, 22.46] vs. b=17.74, 95% CI [16.11, 19.36]) in the non-BPSD group, but not in the BPSD group (b=17.53, 95% CI [13.26, 21.80] vs. b=19.64, 95% CI [16.67, 22.60]).
Discussion
The current investigation explored demographic and clinical correlates among caregivers and children impacted by pediatric BPSD, and identified characteristics associated with, and those that were moderators of, parenting stress. This study is significant in that it: offers empirical evidence about predictors and moderators of parenting stress, the first focused on pediatric BPSD to date, an understudied group; highlights the tense environment that caregivers of children affected by pediatric BPSD endure; presents a detailed picture of characteristics of strained caregivers; and underscores the need for careful evaluation of parenting stress before treatment initiation, to inform selection of additional and tailored interventions.
In this young sample comprised predominantly of boys, children with BPSD had more service utilization, psychiatric diagnoses, mood and anxiety symptoms, and functional impairment, but fewer disruptive behavior disorders. Caregivers of children with BPSD were more likely than caregivers of children without BPSD to have a partner. They also reported elevated parenting stress, mood symptoms, and antisocial tendencies. Higher child IQ, mania, anxiety, and disruptive behavior, and caregiver depression, predicted increased parenting stress; maternal conduct disorder was associated with lower stress levels. Regarding moderators, child anxiety and disruptive behavior were associated with increased caregiver stress only in the non-BPSD group.
Characteristics of Children with vs. without BPSD and their Caregivers
Consistent with prior research, children with BPSD presented with considerable mood and anxiety symptoms, psychiatric comorbidity, and functional impairment (Axelson et al., 2006; Birmaher et al., 2009a; Geller et al., 2008) and required more extensive treatment than children without BPSD (Evans-Lacko et al., 2010; Rizzo et al., 2007). In addition, children with BPSD presented with fewer disruptive disorders, which is likely is a function of the ESM+ sample; those that did not have BPSD most commonly had ADHD (76.1%) and/or a disruptive behavior disorder (51.1%; Findling et al. 2010).
Caregivers of children with BPSD were less likely to be single. They also reported more parenting stress, and had higher rates of mania, depression, and antisocial personality disorder. Prior research suggests that caregivers of children with BPSD often have a partner and experience considerable stress, given the demands of caring for an impaired child (Fristad et al., 2012; Hellander et al., 2003; Nadkarni & Fristad, 2012). However, in the current study presence of a partner was associated with higher stress, potentially resulting from marital discord, which is common among caregivers raising children with psychiatric impairment (Mendenhall & Mount, 2011). In addition, couples may feel as though they should be able to manage their children’s difficulties, compared to single parents, and feel hopeless or ashamed when neither caregiver can calm or ameliorate their children’s dysregulation. The finding that caregivers (mostly biological relatives in this sample) of children with BPSD presented with higher rates of mood symptoms/disorders and other comorbidities is also consistent with prior research (Brotman et al., 2007; Geller et al., 2006), which may be due to heritability of the disorder (Mick & Faraone, 2009), familial environmental contagion and family functioning deficits (Du Rocher et al., 2008), or parental depression as a result of managing a child with BPSD, though these relationships were not specifically examined.
Predictors of Stress for Caregivers Regardless of Child BPSD
As expected, child mania and anxiety symptoms, and presence of any disruptive behavior disorder, were associated with increased caregiver stress (e.g., Anderson, 2008; Bussing et al. 2003a; Bussing et al., 2003b; Deater-Deckard, 2004; Stone et al., 2016; Vaughan et al., 2013). These problem areas likely exacerbate parenting stress in different ways. For example, child manic euphoria and irritability may induce caregiver strain if parents have to coordinate various mental health appointments and monitor children’s mood symptoms, medication compliance, sleep schedule, and safety. Alternatively, child anxiety may increase stress when parents are forced to appease avoidant or reassurance-seeking behaviors, while child disruptive behavior may interfere with caregiver functioning when parents have to troubleshoot difficulties at school, mediate sibling arguments, and resolve other conflicts.
Interestingly, higher child IQ was also associated with increased caregiver stress. Thus, intelligent children may be more cunning adversaries in family conflict (e.g. more manipulative and argumentative). Alternatively, brighter children may be easily bored and thus require extra stimulation, which can be challenging for parents to provide. Or, parents of intelligent, high-achieving children may also be high-achieving and successful (e.g., heritability for IQ is moderate), and put greater pressure on themselves and their children to excel, exacerbating stress. For example, parenting stress is associated with parental perfectionism (Lee, Schoppe-Sulivan, & Kamp Dush, 2012) and use of more controlling strategies regarding children’s academics (Rogers, Wiener, Marton, & Tannock, 2009), which may impair parent-child relations and exacerbate familial stress among high-achieving children (Qin, Rak, Rana, & Donnellan, 2012). As caregivers of children with greater cognitive abilities likely have higher expectations, they may become increasing discouraged and overwhelmed when their intelligent and capable child succumbs to emotional and behavioral dysregulation, does not perform the way he/she otherwise might, and experiences unexpected social problems. The discrepancy of the loss may feel even greater to these parents, whose children otherwise display tremendous potential.
Regarding caregiver characteristics, parents with psychiatric problems experienced greater stress, consistent with prior research (Algorta et al., 2014; Angold et al., 1998). Specifically, caregiver depressive symptoms correlated with parenting stress. Impairing depressive symptoms can make daily tasks challenging, especially raising a child with mental health problems. Parental depression has been strongly linked to parenting stress in both clinical (Theule et al., 2013) and normative samples (Nam, Wikoff, & Sherraden, 2015). Thus, the added burden of caring for a psychiatrically impaired child on top of managing one’s own depression would certainly exacerbate caregiver stress. Conversely, depressive symptoms may reflect demoralization and burn out from high levels of parenting stress; directionality of findings is unknown in these correlational data.
Finally, lifetime presence of maternal conduct disorder was associated with lower levels of stress. Conduct/antisocial problems are characterized by disregard for societal rules and feelings/rights of others, lower levels of empathy, and less adherence to duty (American Psychiatric Association, 2013). Mothers with these traits may not have as vested an interest in being an effective parent or in having the child meet social norms, and thus may not experience stress surrounding this role. Indeed, research suggests mothers who exhibit antisocial behavior display more abuse, hostility, and maltreatment in the home, potentially generating more familial stress as opposed to experiencing increased stress levels themselves (Kim-Cohen, Caspi, Rutter, Tomas, & Moffitt, 2006).
Moderators of Stress for Caregivers of Children with vs. without BPSD
Regarding moderators, child anxiety and disruptive behavior were associated with increased caregiver stress only in the non-BPSD group. Thus, caregivers of children with BPSD reported the highest levels of parenting stress, and the child’s BPSD appeared to trump any effect of comorbid anxiety and DBD. On the other hand, parents of children without BPSD, lacking the stress of child BPSD, may have been more influenced by child anxiety and disruptive behavior. A further possible explanation is the higher rate of disruptive symptoms in those without BPSD, making it a stronger impact on parental stress. Indeed, for some families, anxiety or disruptive behavior may have been the only stressor from the child.
Given the chronic and impairing nature of pediatric BPSD (Axelson et al., 2006; Birmaher et al., 2009a; Freeman et al., 2009; Geller et al., 2008; Goldstein et al., 2009; Hauser et al., 2013; Keenan-Miller et al., 2012), which requires careful monitoring and extensive treatment (Evans-Lacko et al., 2010; Rizzo et al., 2007), and thus impacts the entire family system, it is not surprising that parenting stress was highest among caregivers of children with BPSD. While child anxiety and disruptive behavior were only associated with increased parenting stress among caregivers of children without BPSD, this may be a function of the BPSD subsample, for which comorbidity was the rule rather than the exception (Findling et al., 2010). Nevertheless, these results suggest that caregivers of children with anxiety and disruptive behavior also endure elevated parenting stress, though not to the extent experienced by caregivers of children with BPSD. These findings are consistent with prior work documenting high levels of parenting stress among children with internalizing (Bussing et al., 2003a; Bussing et al. 2003b; Deater-Deckard, 2004; Stone et al., 2016; Vaughan et al., 2013) and externalizing problems (Algorta et al., 2014; Anderson, 2008; Bussing et al., 2003a; Bussing et al., 2003b; Mackler et al., 2015; McDonald et al., 1997; Stone et al., 2016; Theule et al., 2013; Tzang et al., 2009; Vaughan et al., 2013), and intuitively make sense, as caregiver management of avoidant behaviors in anxiety and aggressive/defiant behaviors in disruptive disorders is likely to exacerbate caregiver strain.
Interestingly, improvements in parent factors and family functioning, including and related to parenting stress, have been implicated as mediators of treatment effects for children with BPSD (MacPherson et al., 2016; Mendenhall et al., 2009), anxiety (Schleider et al., 2015; Wood, McLeod, Piacentini, & Sigman, 2009), and disruptive behavior (Forehand, Lafko, Parent, & Burt, 2014). Such parent and family variables have also been found to predict and moderate treatment effects. While more impaired children and families tend to benefit most from EBTs for BPSD (MacPherson et al., 2014; Miklowitz et al., 2009; Weinstein et al., 2015) and disruptive behavior (Gardner, Hutchings, Bywater, & Whitaker, 2010), caregiver stress is generally predictive of worse treatment outcomes for anxiety (Compton et al., 2014; Crawford & Manassis, 2001), though treatments with active parental involvement are highly effective for anxious children (Manassis et al., 2014). Thus, families of children with anxiety, disruptive behavior, or especially BPSD, experience considerable stress and may require more structured and intensive interventions with high levels of parental involvement to experience benefit. In turn, improving stress or other parent-focused constructs may facilitate children’s response to EBTs.
Limitations and Future Directions
This study benefits from having several strengths, including the use of a large sample of outpatient mental health services utilizers and examination of a variety of variables potentially associated with pediatric BPSD and parenting stress. Nevertheless, several limitations related to the sample and study design, independent of outcome measurement, should be noted. First, participants were mainly children with elevated symptoms of mania and their caregivers presenting for initial outpatient psychiatric assessment. Thus, findings may not extend to families of children with different diagnostic profiles (e.g., intellectual disability) or to a non-treatment-seeking population. Given lack of a non-clinical control, it is possible that parenting stress was overestimated, and analyses did not account for clustering within the clinics. In addition, only baseline data from the LAMS study were analyzed, and some children in the non-BPSD group may have converted to BPSD at a later age. Thus, trajectory of stress and predictors/moderators of these constructs over time were not evaluated. Also, other important variables found to be associated with stress, such as social support (Schoeder & Remer, 2007), the presence of psychopathology in all family members, or genetic factors were not measured in the current study. In addition, caregiver IQ and executive functioning likely influence parenting stress, though these constructs were not specifically assessed. Finally, stress levels may have been especially high at the time of the evaluation, as many of the families were seen prior to initiating treatment for their children’s problems. Thus, findings may differ within a less acute sample.
Future studies based on longitudinal analyses would offer insight regarding the trajectory of stress in relation to established and emerging psychopathology, and associated predictors/moderators over time. Additional work should measure other variables previously found or hypothesized to be related to stress, and use such information to refine and improve current EBTs.
Clinical Implications and Conclusions
This study suggests that caregivers of children affected by pediatric BPSD experience increased burden compared to caregivers of children with other diagnoses. Children with BPSD are significantly impaired and require more involved treatment than children with most other mental health problems. In addition, their caregivers experience more stress and psychiatric impairment than caregivers of children with non-BPSD disorders; thus, they may require additional support and family-focused interventions.
Depressed caregivers of children with higher IQ, more severe mania and anxiety symptoms, and disruptive behavior seem to experience increased stress regardless of child BPSD, and thus likely require more help compared to families unaffected by these characteristics. Though parents with conduct/antisocial problems evidenced lower stress, these difficulties could be associated with poor parenting resources and thus should be monitored closely.
Caregivers of children with BPSD may also experience parenting stress differently than caregivers of children without BPSD: child anxiety symptoms and disruptive behavior were more strongly associated with higher parenting stress among caregivers of children without versus with BPSD. Thus, consistent with existing practice parameters, findings highlight the importance of comprehensive assessment evaluating multiple child, parent, and family factors contributing to the onset and maintenance of mental health problems in youth prior to intervention selection. Parenting stress in particular should be carefully evaluated and addressed in assessment and treatment of pediatric BPSD, anxiety, and disruptive disorders, as these caregivers experience the highest stress levels, especially caregivers of children with BPSD, and thus may require more support, services, and specialized, family-focused interventions.
Acknowledgments
Support for this manuscript was provided by the National Institute of Mental Health: R01 MH073801, R01-MH073967, R01-MH073953, and R01-MH073816.
Potential conflicts of interest: Dr. Youngstrom has consulted about psychological assessment with Otsuka, Lundbeck, Janssen, Western Psychological Services, and Pearson. Dr. Arnold has received research funding from Curemark, Forest, Lilly, Neuropharm, Novartis, Noven, Shire, Supernus, and Young Living (as well as NIH and Autism Speaks) and has consulted with or been on advisory boards for Arbor, Gowlings, Ironshore, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Roche, Seaside Therapeutics, Sigma Tau, Shire, Tris Pharma, and Waypoint and received travel support from Noven. Dr. Frazier has received federal funding or research support from, acted as a consultant to, received travel support from, and/or received a speaker’s honorarium from the Cole Family Research Fund, Simons Foundation, Ingalls Foundation, Forest Laboratories, Ecoeos, IntegraGen, Kugona LLC, Shire Development, Bristol-Myers Squibb, National Institutes of Health, and the Brain and Behavior Research Foundation. Dr. Birmaher receives royalties from American Psychiatric Publishing, Random House, UpToDate, and Lippincott Williams & Wilkins. Dr. Findling receives or has received research support, acted as a consultant and/or served on a speaker’s bureau for Alcobra, American Academy of Child & Adolescent Psychiatry, American Physician Institute, American Psychiatric Press, Bracket, CogCubed, Cognition Group, Coronado Biosciences, Dana Foundation, Elsevier, Forest, Guilford Press, Ironshore, Johns Hopkins University Press, Jubilant Clinsys, KemPharm, Lundbeck, Merck, NIH, Neurim, Novartis, Otsuka, Oxford University Press, Pfizer, Physicians Postgraduate Press, Purdue, Rhodes Pharmaceuticals, Roche, Sage, Shire, Sunovion, Supernus Pharmaceuticals, Teva, Transcept Pharmaceuticals, Tris, Validus, and WebMD. Dr. Fristad receives royalties from American Psychiatric Press, Guilford Press and Child & Family Psychological Services as well as honoraria from Physicians’ Post-Graduate Press. Drs. Algorta, MacPherson, Taylor, and Horwitz, and Ms. Belt, have no conflicts to report.
Contributor Information
Guillermo Perez Algorta, Lancaster University.
Heather A. MacPherson, Harvard University
Eric A. Youngstrom, University of North Carolina at Chapel Hill
Caroline C. Belt, The Ohio State University
L. Eugene Arnold, The Ohio State University Wexner Medical Center.
Thomas W. Frazier, Cleveland Clinic
H. Gerry Taylor, Case Western Reserve University and Rainbow Babies & Children’s Hospital.
Boris Birmaher, University of Pittsburgh Medical Center.
Sarah McCue Horwitz, New York University School of Medicine.
Robert L. Findling, Johns Hopkins University/Kennedy Krieger Institute
Mary A. Fristad, The Ohio State University Wexner Medical Center
References
- Abidin RR. The determinants of parenting behavior. Journal of Clinical Child Psychology. 1992;21:407–412. [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications, Inc.; 1991. [Google Scholar]
- Algorta GP, Kragh CA, Arnold LE, Molina BSG, Hinshaw SP, Swanson JM, Jensen PS. Maternal ADHD symptoms, personality, and parenting stress: Differences between mothers of children with ADHD and mothers of comparison children. Journal of Attention Disorders. 2014 doi: 10.1177/1087054714561290. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Algorta GP, Van Meter A, Youngstrom EA. The Apple and the Tree: What Family and Offspring Studies of Bipolar Disorder Show About Mechanisms of Risk and Prevention. In: Yildiz A, Nemeroff C, Ruiz P, editors. Bipolar Disorder: Millennium Update. New York, NY: Oxford University Press; 2015. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- Anderson LS. Predictors of parenting stress in a diverse sample of parents of early adolescents in high-risk communities. Nursing Research. 2008;57:340–350. doi: 10.1097/01.NNR.0000313502.92227.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Messer SC, Stangl D, Farmer EMZ, Costello EJ, Burns BJ. Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health. 1998;88:75–80. doi: 10.2105/ajph.88.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold LE, Mount K, Frazier TW, Demeter C, Youngstrom EA, Fristad MA, Axelson DA. Pediatric bipolar disorder and ADHD: Family history comparison in the LAMS clinical sample. Journal of Affective Disorders. 2012;10:382–389. doi: 10.1016/j.jad.2012.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelson D, Birmaher B, Strober M, Gill MK, Valeri S, Chiappetta L, Keller M. Phenomenology of children and adolescents with bipolar spectrum disorders. Archives of General Psychiatry. 2006;63:1139–1148. doi: 10.1001/archpsyc.63.10.1139. [DOI] [PubMed] [Google Scholar]
- Barron E, Sharma A, Le Couteur J, Rushton S, Close A, Kelly T, Le Couteur A. Family environment of bipolar families: A UK study. Journal of Affective Disorders. 2014;152–154:522–525. doi: 10.1016/j.jad.2013.08.016. [DOI] [PubMed] [Google Scholar]
- Belardinelli C, Hatch JP, Olvera RL, Fonseca M, Caetano SC, Nicoletti M, Soares JC. Family environment patterns in families with bipolar children. Journal of Affective Disorders. 2008;107:299–305. doi: 10.1016/j.jad.2007.08.011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Goldstein B, Strober M, Gill MK, Hunt J, Keller M. Four-year longitudinal course of children and adolescents with bipolar spectrum disorders: The Course and Outcome of Bipolar Youth (COBY) study. American Journal of Psychiatry. 2009a;166:795–804. doi: 10.1176/appi.ajp.2009.08101569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Axelson D, Monk K, Kalas C, Goldstein B, Hickey MB, Brent D. Lifetime psychiatric disorders in school-aged offspring of parents with bipolar disorder: The Pittsburgh Bipolar Offspring Study. Archives of General Psychiatry. 2009b;66:287–296. doi: 10.1001/archgenpsychiatry.2008.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1230–1236. doi: 10.1097/00004583-199910000-00011. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM. The Screen for Child Anxiety Related Emotional Disorders (SCARED): Scale construction and psychometric characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:545–553. doi: 10.1097/00004583-199704000-00018. [DOI] [PubMed] [Google Scholar]
- Brannan AM, Heflinger CA, Bickman L. The Caregiver Strain Questionnaire: Measuring the impact of the family living with a child with serious emotional problems. Journal of Emotional and Behavioral Disorders. 1997;5:212–222. [Google Scholar]
- Brotman MA, Kassem L, Reising MM, Guyer AE, Dickstein DP, Rich BA, Leibenluft E. Parental diagnoses in youth with narrow phenotype bipolar disorder or severe mood dysregulation. American Journal of Psychiatry. 2007;164:1238–1241. doi: 10.1176/appi.ajp.2007.06101619. [DOI] [PubMed] [Google Scholar]
- Bussing R, Gary FA, Mason DM, Leon CE, Sinha K, Garvan CW. Child temperament, ADHD, and caregiver strain: Exploring relationships in an epidemiologic sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2003a;42:184–192. doi: 10.1097/00004583-200302000-00012. [DOI] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Gary FA, Mason DA, Leon CE, Sinha K, Garvan CW. Social networks, caregiver strain, and utilization of mental health services among elementary school students at high risk for ADHD. Journal of the American Academy of Child and Adolescent Psychiatry. 2003b;42:842–850. doi: 10.1097/01.CHI.0000046876.27264.BF. [DOI] [PubMed] [Google Scholar]
- Chang KD, Blasey C, Ketter TA, Steiner H. Family environment of children and adolescents with bipolar parents. Bipolar Disorders. 2001;3:73–78. doi: 10.1034/j.1399-5618.2001.030205.x. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Lawrence Erlbaum Associates, Inc.; 2003. [Google Scholar]
- Compton SN, Peris TS, Almirall D, Birmaher B, Sherrill J, Kendall PC, Albano AM. Predictors and moderators of treatment response in childhood anxiety disorders: Results from the CAMS trial. Journal of Consulting and Clinical Psychology. 2014;82:212–224. doi: 10.1037/a0035458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cousino MK, Hazen RA. Parenting stress among caregivers of children with chronic illness: A systematic review. Journal of Pediatric Psychology. 2013;38:809–828. doi: 10.1093/jpepsy/jst049. [DOI] [PubMed] [Google Scholar]
- Crawford AM, Manassis K. Familial predictors of treatment outcome in childhood anxiety disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:1182–1189. doi: 10.1097/00004583-200110000-00012. [DOI] [PubMed] [Google Scholar]
- Deater-Deckard K. Parenting stress. New Haven, CT: Yale University Press; 2004. [Google Scholar]
- Depue RA. General Behavior Inventory Assessment Manual. Minneapolis, MN: University of Minnesota; 1987. [Google Scholar]
- Depue RA, Krauss S, Spoont MR, Arbisi B. General Behavior Inventory identification of unipolar and bipolar affective conditions in a non-clinical university population. Journal of Abnormal Psychology. 1989;98:117–126. doi: 10.1037//0021-843x.98.2.117. [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Youngstrom EA, Calabrese JR, Findling R. The role of family functioning in bipolar disorder in families. Journal of Child Abnormal Psychology. 2008;36:849–863. doi: 10.1007/s10802-008-9217-9. [DOI] [PubMed] [Google Scholar]
- Evans-Lacko SE, Spencer CS, Logan JE, Riley AW. Patterns and predictors of restrictive health care use by youths with bipolar disorder. Administration and Policy in Mental Health. 2010;37:379–387. doi: 10.1007/s10488-009-0248-5. [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behavior Research Methods. 2009;41:1149–1160. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- Ferreira GS, Moreira CRL, Kleinman A, Nader ECGP, Gomes BC, Teixeira AMA, Caetano SC. Dysfunctional family environment in affected versus unaffected offspring of parents with bipolar disorder. Australian and New Zealand Journal of Psychiatry. 2013;47:1051–1057. doi: 10.1177/0004867413506754. [DOI] [PubMed] [Google Scholar]
- Findling RL, Youngstrom EA, Fristad MA, Birmaher B, Kowatch RA, Arnold LE, Horwitz SM. Characteristics of children with elevated symptoms of mania: The Longitudinal Assessment of Manic Symptoms (LAMS) study. Journal of Clinical Psychiatry. 2010;71:1664–1672. doi: 10.4088/JCP.09m05859yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forehand R, Lafko N, Parent J, Burt KB. Is parenting the mediator of change in behavioral parent training for externalizing problems of youth? Clinical Psychology Review. 2014;34:608–619. doi: 10.1016/j.cpr.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox J. Effect displays in R for generalised linear models. Journal of Statistical Software. 2003;8:1–27. [Google Scholar]
- Freeman AJ, Youngstrom EA, Michalak E, Siegel R, Meyers OI, Findling RL. Quality of life in pediatric bipolar disorder. Pediatrics. 2009;123:e446–e452. doi: 10.1542/peds.2008-0841. [DOI] [PubMed] [Google Scholar]
- Fristad MA, Frazier TW, Youngstrom EA, Mount K, Fields BW, Demeter C, Findling RL. What differentiates children visiting outpatient mental health services with bipolar spectrum disorder from children with other psychiatric diagnoses? Bipolar Disorders. 2012;14:497–506. doi: 10.1111/j.1399-5618.2012.01034.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fristad MA, MacPherson HA. Evidence-based psychosocial treatments for child and adolescent bipolar spectrum disorders. Journal of Clinical Child and Adolescent Psychology. 2014;43:339–355. doi: 10.1080/15374416.2013.822309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardner F, Hutchings J, Bywater T, Whitaker C. Who benefits and how does it work? Moderators and mediators of outcome in an effectiveness trial of a parenting intervention. Journal of Clinical Child and Adolescent Psychology. 2010;39:568–580. doi: 10.1080/15374416.2010.486315. [DOI] [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B. Child bipolar I disorder: Prospective continuity with adult bipolar I disorder; Characteristics of second and third episodes; Predictors of 8-year outcome. Archives of General Psychiatry. 2008;65:1125–1133. doi: 10.1001/archpsyc.65.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geller B, Tillman R, Bolhofner K, Zimerman B, Strauss NA, Kaufman P. Controlled, blindly rated, direct-interview family study of a prepubertal and early-adolescent bipolar I disorder phenotype: Morbid risk, age at onset, and comorbidity. Archives of General Psychiatry. 2006;63:1130–1138. doi: 10.1001/archpsyc.63.10.1130. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL, DelBello MP, Soutullo C. Reliability of the Wahsington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS) mania and rapid cycling sections. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:450–455. doi: 10.1097/00004583-200104000-00014. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Birmaher B, Axelson D, Goldstein BI, Gill MK, Esposito-Smythers C, Keller M. Psychosocial functioning among bipolar youth. Journal of Affective Disorders. 2009;114:174–183. doi: 10.1016/j.jad.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gore FM, Bloem PJ, Patton GC, Ferguson J, Joseph V, Coffey C, Mathers CD. Global burden of disease in young people aged 10–24 years: a systematic analysis. The Lancet. 2011;377(9783):2093–2102. doi: 10.1016/S0140-6736(11)60512-6. [DOI] [PubMed] [Google Scholar]
- Hauser M, Galling B, Correll CU. Suicidal ideation and suicide attempts in children and adolescents with bipolar disorder: A systematic review of prevalence and incidence rates, correlates, and targeted interventions. Bipolar Disorders. 2013;15:507–523. doi: 10.1111/bdi.12094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SA, Watson SL. The impact of parenting stress: A meta-analysis of studies comparing the experience of parenting stress in parents of children with and without autism spectrum disorder. Journal of Autism and Developmental Disorders. 2013;43:629–642. doi: 10.1007/s10803-012-1604-y. [DOI] [PubMed] [Google Scholar]
- Hellander M, Sisson DP, Fristad MA. Internet support for parents of children with early-onset bipolar disorder. In: Geller B, Del Bello M, editors. Child and early adolescent bipolar disorder: Theory, Assessment, and Treatment. New York, NY: Guilford Publications, Inc.; 2003. pp. 314–329. [Google Scholar]
- Hoagwood K, Horwitz S, Stiffman A, Weisz J, Bean D, Rae D, Leaf P. Concordance between parent reports of children’s mental health services and service records: The Services Assessment for Children and Adolescents (SACA) Journal of Child and Family Studies. 2000;9:315–331. [Google Scholar]
- Horwitz SM, Demeter CA, Pagano ME, Youngstrom EA, Fristad MA, Arnold LE, Findling RL. Longitudinal Assessment of Manic Aymptoms (LAMS) study: Background, design, and initial screening results. Journal of Clinical Psychiatry. 2010;71:1511–1517. doi: 10.4088/JCP.09m05835yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James G, Witten D, Hastie T, Tibshirani R. An introduction to statistical learning. Vol. 112. New York, NY: Springer; 2013. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Ryan N. Schedule of Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (KSADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Keenan-Miller D, Peris T, Axelson D, Kowatch RA, Miklowitz DJ. Family functioning, social impairment, and symptoms among adolescents with bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:1085–1094. doi: 10.1016/j.jaac.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim EY, Miklowitz DJ, Biuckians A, Mullen K. Life stress and the course of early-onset bipolar disorder. Journal of Affective Disorders. 2007;99:37–44. doi: 10.1016/j.jad.2006.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Rutter M, Tomás MP, Moffitt TE. The caregiving environments provided to children by depressed mothers with or without antisocial personality. American Journal of Psychiatry. 2006;163:1009–1018. doi: 10.1176/ajp.2006.163.6.1009. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Lee MA, Schoppe-Sullivan SJ, Kamp Dush CM. Parenting perfectionism and parental adjustment. Personality and Individual Differences. 2012;52:454–457. doi: 10.1016/j.paid.2011.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manassis K, Lee TC, Bennett K, Zhao XY, Mendlowitz S, Duda S, Wood JJ. Types of parental involvement in CBT with anxious youth: A preliminary meta-analysis. Journal of Consulting and Clinical Psychology. 2014;82:1163–1172. doi: 10.1037/a0036969. [DOI] [PubMed] [Google Scholar]
- Mackler JS, Kelleher RT, Shanahan L, Calkins SD, Keane SP, O’Brien M. Parenting stress, parental reactions, and externalizing behavior from ages 4 to 10. Journal of Marriage and Family. 2015;77:388–406. doi: 10.1111/jomf.12163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson HA, Algorta GP, Mendenhall AN, Fields BW, Fristad MA. Predictors and moderators in the randomized trial of multi-family psychoeducational psychotherapy for childhood mood disorders. Journal of Clinical Child and Adolescent Psychology. 2014;43:459–472. doi: 10.1080/15374416.2013.807735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacPherson HA, Weinstein SM, Henry DB, West AE. Mediators in the randomized trial of Child- and Family-Focused Cognitive-Behavioral Therapy for pediatric bipolar disorder. Behaviour Research and Therapy. 2016;85:60–71. doi: 10.1016/j.brat.2016.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe KM, Yeh M, Lau A, Garland A, Hough R. Racial/ethnic differences in caregiver strain and perceived social support among parents of youth with emotional and behavioral problems. Mental Health Services Research. 2003;5:137–147. doi: 10.1023/a:1024439317884. [DOI] [PubMed] [Google Scholar]
- McDonald TP, Gregoire TK, Poertner J, Early TJ. Building a model of family caregiving for children with emotional disorders. Journal of Emotional and Behavioral Disorders. 1997;5:138–148. [Google Scholar]
- Mendenhall AN, Fristad MA, Early TJ. Factors influencing service utilization and mood symptom severity in children with mood disorders: Effects of multifamily psychoeducation groups (MFPGs) Journal of Consulting and Clinical Psychology. 2009;77:463–473. doi: 10.1037/a0014527. [DOI] [PubMed] [Google Scholar]
- Mendenhall AN, Mount K. Parents of children with mental illness: Exploring the caregiver experience and caregiver-focused interventions. Families in Society: The Journal of Contemporary Social Services. 2011;92:183–190. [Google Scholar]
- Mesman E, Nolen WA, Reichart CG, Wals M, Hillegers MH. The Dutch bipolar offspring study: 12-year follow-up. American Journal of Psychiatry. 2013;170:542–549. doi: 10.1176/appi.ajp.2012.12030401. [DOI] [PubMed] [Google Scholar]
- Mick E, Faraone SV. Family and genetic association studies of bipolar disorder in children. Child and Adolescent Psychiatric Clinics of North America. 2009;18:441–453. doi: 10.1016/j.chc.2008.11.008. [DOI] [PubMed] [Google Scholar]
- Miklowitz DJ, Axelson DA, George EL, Taylor DO, Schneck CD, Sullivan AE, Birmaher B. Expressed emotion moderates the effects of family-focused treatment for bipolar adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:643–651. doi: 10.1097/CHI.0b013e3181a0ab9d. [DOI] [PubMed] [Google Scholar]
- Nader EG, Kleinman A, Gomes BC, Bruscagin C, dos Santos B, Nicoletti M, Caetano SC. Negative expressed emotion best discriminates families with bipolar disorder children. Journal of Affective Disorders. 2013;148:418–423. doi: 10.1016/j.jad.2012.11.017. [DOI] [PubMed] [Google Scholar]
- Nam Y, Wikoff N, Sherraden M. Racial and ethnic differences in parenting stress: Evidence from a statewide sample of new mothers. Journal of Child and Family Studies. 2015;24:278–288. [Google Scholar]
- Nadkarni RB, Fristad MA. Stress and support for parents of youth with bipolar disorder. The Israel Journal of Psychiatry and Related Sciences. 2012;49:104–110. [PMC free article] [PubMed] [Google Scholar]
- Pendergast LL, Youngstrom EA, Merkitch KG, Moore KA, Black C, Abramson L, Alloy LB. Differentiating bipolar disorder from unipolar depression and ADHD: The utility of the General Behavior Inventory. Psychological Assessment. 2014;26:195–206. doi: 10.1037/a0035138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters AT, Henry DB, West AE. Caregiver characteristics and symptoms of pediatric bipolar disorder. Journal of Family Studies. 2014;24:1469–1480. [Google Scholar]
- Pompili M, Harnic D, Gonda X, Forte A, Dominici G, Innamorati M, Girardi P. Impact of living with bipolar patients: Making sense of caregivers’ burden. World Journal of Psychiatry. 2014;4:1–12. doi: 10.5498/wjp.v4.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poznanski EO, Grossman JA, Buchsbaum Y, Banegas M, Freeman L, Gibbons R. Preliminary studies of the reliability and validity of the Children's Depression Rating Scale. Journal of the American Academy of Child Psychiatry. 1984;23:191–197. doi: 10.1097/00004583-198403000-00011. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interaction effects in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Qin DB, Rak E, Rana M, Donnellan MB. Parent-child relations and psychological adjustment among high-achieving Chinese and European American adolescents. Journal of Adolescence. 2012;35:863–873. doi: 10.1016/j.adolescence.2011.12.004. [DOI] [PubMed] [Google Scholar]
- Rizzo CJ, Esposito-Smythers C, Swenson L, Birmaher B, Ryan N, Strober M, Keller M. Factors associated with mental health service utilization among bipolar youth. Bipolar Disorders. 2007;9:839–850. doi: 10.1111/j.1399-5618.2007.00439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers MA, Wiener J, Marton I, Tannock R. Supportive and controlling parental involvement as predictors of children’s academic achievement: Relations to children’s ADHD symptoms and parenting stress. School Mental Health. 2009;1:89–102. [Google Scholar]
- Schenkel LS, West AE, Harral EM, Patel NB, Pavuluri MN. Parent-child interactions in pediatric bipolar disorder. Journal of Clinical Psychology. 2008;64:422–437. doi: 10.1002/jclp.20470. [DOI] [PubMed] [Google Scholar]
- Schleider JL, Ginsburg GS, Keeton CP, Weisz JR, Birmaher B, Kendall PC, Walkup JT. Parental psychopathology and treatment outcome for anxious youth: Roles of family functioning and caregiver strain. Journal of Consulting and Clinical Psychology. 2015;83:213–224. doi: 10.1037/a0037935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoeder CE, Remer R. Perceived social support and caregiver strain in caregivers of children with Tourette’s disorder. Journal of Child and Family Studies. 2007;16:888–901. [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, Aluwahlia S. A Children's Global Assessment Scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Siegel RS, Hoeppner B, Yen S, Stout RL, Weinstock LM, Keller MB. Longitudinal associations between interpersonal relationship functioning and mood episode severity in youth with bipolar disorder. Journal of Nervous and Mental Disease. 2015;203:1–11. doi: 10.1097/NMD.0000000000000261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sisson DP, Fristad MA. A survey of stress and support for parents of children with early-onset bipolar disorder. Bipolar Disorders. 2001;3:58. [Google Scholar]
- Stewart SB, Greene DJ, Lessov-Schlaggar CN, Church JA, Schlaggar BL. Clinical correlates of parenting stress in children with Tourette syndrome and typically developing children. Journal of Pediatrics. 2015;166:1297–1302. doi: 10.1016/j.jpeds.2015.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone LL, Mares SHW, Otten R, Engels RCME, Janssens JMAM. The co-development of parenting stress and childhood internalizing and externalizing problems. Journal of Psychopathology and Behavioral Assessment. 2016;38:76–86. doi: 10.1007/s10862-015-9500-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streiner DL, Norman GR, Cairney J. Health Measurement Scales: A Practical Guide to their Development and Use. 5. New York, NY: Oxford University Press; 2015. [Google Scholar]
- Sullivan AE, Judd CM, Axelson DA, Miklowitz DJ. Family functioning and the course of adolescent bipolar disorder. Behavior Therapy. 2012;43:837–847. doi: 10.1016/j.beth.2012.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theule J, Wiener J, Tannock R, Jenkins JM. Parenting stress in families of children with ADHD: A meta-analysis. Journal of Emotional and Behavioral Disorders. 2013;21:3–17. [Google Scholar]
- Tzang R, Change Y, Liu S. The association between children’s ADHD subtype and parenting stress and parental symptoms. International Journal of Psychiatry in Clinical Practice. 2009;13:318–325. doi: 10.3109/13651500903094567. [DOI] [PubMed] [Google Scholar]
- Van Meter AR, Moreira AL, Youngstrom EA. Meta-analysis of epidemiologic studies of pediatric bipolar disorder. Journal of Clinical Psychiatry. 2011;72:1250–1256. doi: 10.4088/JCP.10m06290. [DOI] [PubMed] [Google Scholar]
- Vaughan EL, Feinn R, Bernard S, Brereton M, Kaufman JS. Relationships between child emotional and behavioral symptoms and caregiver strain and parenting stress. Journal of Family Issues. 2013;34:534–556. doi: 10.1177/0192513X12440949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Abbreviated Intelligence Scale. San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- Weinstein SM, Henry DB, Katz AC, Peters AT, West AE. Treatment moderators of child- and family-focused cognitive-behavioral therapy for pediatric bipolar disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2015;54:116–125. doi: 10.1016/j.jaac.2014.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Breif screening for family psychiatric history: The Family History Screen. Archives of General Psychiatry. 2000;57:675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- Wiener J, Biondic D, Grimbos T, Herbert M. Parenting stress of parents of adolescents with attention-deficit hyperactivity disorder. Journal of Abnormal Child Psychology. 2016;44:561–574. doi: 10.1007/s10802-015-0050-7. [DOI] [PubMed] [Google Scholar]
- Wood JJ, McLeod BD, Piacentini JC, Sigman M. One-year follow-up of family versus child CBT for anxiety disorders: Exploring the roles of child age and parental intrusiveness. Child Psychiatry and Human Development. 2009;40:301–316. doi: 10.1007/s10578-009-0127-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yatchmenoff DK, Koren PE, Friesen BJ, Gordon LJ, Kinney RF. Enrichment and stress and families caring for a child with a serious emotional disorder. Journal of Child and Family Studies. 1998;7:129–145. [Google Scholar]
- Yee AM, Algorta GP, Youngstrom EA, Findling RL, Birmaher B, Fristad MA the LAMS Group. Unfiltered administration of the YMRS and CDRS-R in a clinical sample of children. Journal of Clinical Child and Adolescent Psychology. 2015;44:992–1007. doi: 10.1080/15374416.2014.915548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity, and sensitivity. British Journal of Psychiatry. 1978;133:429–435. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Algorta GP. Bipolar disorder. In: Mash E, Barkley R, editors. Child psychopathology. 3. New York, NY: Guilford Press; 2014. [Google Scholar]
- Youngstrom EA, Danielson CK, Findling RL, Gracious BL, Calabrese JR. Factor structure of the Young Mania Rating Scale for use with youths ages 5 to 17 years. Journal of Clinical Child and Adolescent Psychology. 2002;31:567–572. doi: 10.1207/S15374424JCCP3104_15. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Findling RL, Danielson CK, Calabrese JR. Discriminative validity of parent report of hypomanic and depressive symptoms on the General Behavior Inventory. Psychological Assessment. 2001;13:267–276. [PubMed] [Google Scholar]
- Youngstrom EA, Frazier TW, Demeter C, Calabrese JR, Findling RL. Developing a 10-item mania scale from the Parent General Behavior Inventory for children and adolescents. Journal of Clinical Psychiatry. 2008;69:831–839. doi: 10.4088/jcp.v69n0517. [DOI] [PMC free article] [PubMed] [Google Scholar]