Abstract
Many cancers adeptly modulate metabolism to thrive in fluctuating oxygen conditions; however, current tools fail to image metabolic and vascular endpoints at spatial resolutions needed to visualize these adaptations in vivo. We demonstrate a high-resolution intravital microscopy technique to quantify glucose uptake, mitochondrial membrane potential (MMP), and SO2 to characterize the in vivo phentoypes of three distinct murine breast cancer lines. Tetramethyl rhodamine, ethyl ester (TMRE) was thoroughly validated to report on MMP in normal and tumor-bearing mice. Imaging MMP or glucose uptake together with vascular endpoints revealed that metastatic 4T1 tumors maintained increased glucose uptake across all SO2 (“Warburg effect”), and also showed increased MMP relative to normal tissue. Non-metastatic 67NR and 4T07 tumor lines both displayed increased MMP, but comparable glucose uptake, relative to normal tissue. The 4T1 peritumoral areas also showed a significant glycolytic shift relative to the tumor regions. During a hypoxic stress test, 4T1 tumors showed significant increases in MMP with corresponding significant drops in SO2, indicative of intensified mitochondrial metabolism. Conversely, 4T07 and 67NR tumors shifted toward glycolysis during hypoxia. Our findings underscore the importance of imaging metabolic endpoints within the context of a living microenvironment to gain insight into a tumor’s adaptive behavior.
Introduction
Early observations of aerobic glycolysis in cancer led to a persistent view that cancers have defective mitochondrial respiration1. However, many cancer types have now been shown to rely on mitochondrial metabolism in combination with glycolysis to meet the increased energy demands required for proliferation and metastasis2–4. A key indicator of mitochondrial metabolism is the mitochondrial membrane potential (MMP), a transmembrane proton gradient maintained by electron transport5, which is frequently increased (i.e. more negative) in a wide range of cancer types6,7. Proton pumping during electron transport maintains MMP, which, in the presence of oxygen, can be used to produce adenosine triphosphate (ATP)8.
Maintaining increased capacity for both glycolysis and mitochondrial metabolism appears to be critical in helping tumors adapt to environmental stress. In normal tissue, metabolism is directly linked to oxygen availability. Mitochondrial metabolism is preferred during normoxic baseline conditions9. During hypoxia, glycolytic proteins are upregulated and metabolic intermediates are shuttled away from the mitochondria in response to hypoxia-inducible factor 1α (HIF-1α) activity10. In contrast, some tumors can easily switch between anaerobic and aerobic metabolism without regard for oxygen availability. It is well known that many tumors employ high rates of glycolysis during normoxia (i.e. the Warburg effect)11,12. Recent studies also indicate that some aggressive tumor lines heavily utilize mitochondrial metabolism and, unlike primary cells, are able to maintain MMP and mitochondrial metabolism during hypoxia as severe as 0.2-1% O213,14. Hypoxia typically causes a HIF-1a mediated increase in mitochondrial autophagy in an attempt to prolong hypoxic survival10. Surprisingly, hypoxia has been associated with an increase in mitochondrial mass in metastatic murine breast cancer15, and an increase in mitochondrial size mediated by HIF-1α has been shown to prevent mitochondrial apoptosis in colon carcinoma13.
It is no surprise that “adaptable” tumors with high capacity for both glycolytic and mitochondrial metabolism under a range of oxygen conditions are better suited to surviving environmental stress, promoting negative outcomes such as increased migration16 and metastatic propensity14. Recent work also links the adaptable phenotype to metabolic compartmentalization between a tumor and its microenvironment (i.e. the Reverse Warburg Effect)11. In the so-called “Reverse Warburg Effect” (RWE), glycolytic stromal cells excrete lactate, and this micro-environmental “waste” is taken in by cancer cells and used to fuel oxidative phosphorylation (OXPHOS)17. It follows that observing the regional interplay between multiple metabolic and vascular endpoints aids understanding of a tumor’s phenotype.
Considering the importance of glycolysis, MMP, and the oxygen gradients within blood vessels to tumor bioenergetics, there are surprisingly no techniques to image in vivo these three endpoints with a single technology. Commonly used techniques such as cellular metabolic flux analyzers and metabolomics provide comprehensive information about cancer metabolism, but are limited to in vitro assays18 or ex vivo assays19 and neither provides spatial information. There are also multiple in vivo techniques currently available for metabolic imaging. Positron emission tomography (PET) imaging is widely used to measure glucose uptake with the tracer [18F]FDG20, and use of additional radio-labeled probes (e.g. [18F]FMISO) can also enable detection of tissue hypoxia21. The millimeter-scale resolution of PET imaging21,22 prevents it from fully capturing tumor heterogeneity at the microscopic level, however. Similarly, magnetic resonance spectral imaging (MR(S)I) can report on a host of important endpoints related to both mitochondrial metabolism and glycolysis23,24 as well as vasculature25, yet spatial and temporal resolution are limiting22.
Vascular imaging can also be accomplished with a range of magnetic resonance imaging (MRI) techniques20,26. Blood oxygen level dependent (BOLD) MRI reports on oxygenation20,27, dynamic contrast-enhanced (DCE) MRI reports on perfusion and permeability21,28, and dynamic susceptibility contrast (DSC) MRI yields angiogenesis and blood volume assessment29. However, these must be coupled with additional technologies if metabolic endpoints are desired, and resolution may be too poor for some pre-clinical studies20,22.
Optical metabolic imaging has been validated in vivo to report on endpoints such as tumor redox status30–32 and specifically labeled metabolites6,33,34. Optical imaging also allows label-free vascular imaging via endogeneous contrast from hemoglobin35–37. Further, of all the available metabolic imaging techniques, only optical imaging provides the micron-scale resolution necessary to visualize both the heterogeneous metabolic landscape and the aberrant vasculature within small tumors22. Importantly, in vivo optical imaging has not yet been leveraged to perform a comprehensive study measuring glycolysis, mitochondrial metabolism, and small vessel oxygen gradients that influence the overall bioenergetics of a tumor.
We now demonstrate a non-destructive, multi-parametric, intra-vital microscopy technique to image important features of tumor metabolism and vascular physiology at high resolution in small animal models. Glucose uptake is imaged using the well-established indicator 2-[N-(7-nitrobenz-2-oxa-1, 3-diaxol-4-yl) amino]-2-deoxyglucose (2-NBDG) using protocols previously described by our group38,39 and others40–42. Mitochondrial membrane potential (MMP) is imaged with tetramethylrhodamine, ethyl ester (TMRE)43–46. In this manuscript, we thoroughly validate TMRE in normal tissue and tumors to present an optimized method for in vivo mitochondrial membrane potential imaging. Oxygen saturation (SO2) and vessel architecture are quantified by imaging the differential absorption spectra of oxygenated and de-oxygenated hemoglobin, which is an extensively validated method47–52. The relationships between MMP and SO2 and glucose uptake and SO2 were leveraged in our study to characterize the in vivo phenotypes of three murine breast cancer lines- metastatic 4T1 and non-metastatic 67NR and 4T07- that arose from the same parental tumor53,54. Using these well-studied sibling tumor lines with unique metastatic properties allowed us to confirm concordance with previous findings and to add new insights using the distinct capabilities of our technology. This work, incorporating two combinations of two endpoints, represents a critical step toward fully integrated three-endpoint metabolic imaging.
Consistent with previous work, optical microscopy demonstrated that the 4T1 tumors displayed a classic Warburg effect, with increased glucose uptake at all SO2 levels. However, imaging TMRE with our method also enabled the novel finding that 4T1 have hyperpolarized mitochondria relative to normal tissue, suggesting that both mitochondrial metabolism and glycolysis are increased in 4T1 during baseline conditions. On the other hand, 4T07 and 67NR tumors displayed increased mitochondrial membrane potential relative to normal tissue, but comparable levels of glucose uptake, typical of an oxidative phenotype. The increased MMP in all tumor groups was most pronounced at lower oxygen levels, suggesting that low SO2 regions in tumors were associated with increased oxygen-consuming metabolism.
Previous studies have shown that angiogenic vasculature can extend far beyond the tumor border55, recruiting fibroblasts56 and in turn affecting regional metabolism. We saw that the 4T1 peritumoral areas (PAs) had a distinct hypermetabolic phenotype relative to the tumors themselves; this was not observed for 67NR or 4T07 PAs. Specifically, the 4T1 PAs were characterized by angiogenic vasculature, increased glucose uptake, and decreased MMP relative to the neighboring tumors. We hypothesized that increased regional metabolic cooperation would allow 4T1 alone to maintain robust MMP during hypoxia. Indeed, under hypoxic stress, 4T1 tumors showed a significant increase in MMP, with a corresponding significant drop in the SO2, indicative of intensified mitochondrial metabolism. Conversely, 4T07 and 67NR tumors shifted toward a glycolytic phenotype. These findings highlight the unique capability of in vivo metabolic and vascular imaging to provide insight into the microenvironment’s influence on tumor metabolic phenotype.
Results
TMRE responds to established perturbations of mitochondrial membrane potential in vivo
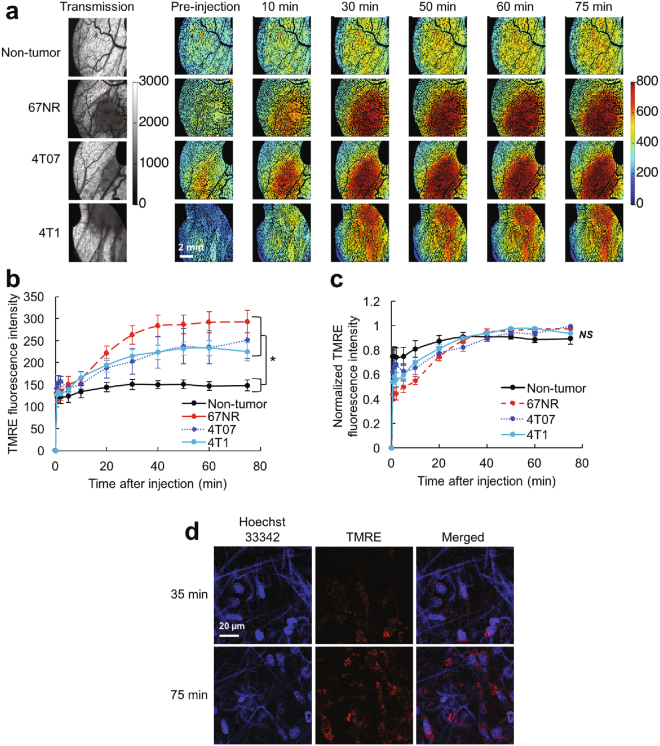
Figures 1 and 2 demonstrate a systematic investigation of TMRE uptake properties and the effects of perturbing mitochondrial membrane potential on TMRE uptake. Fig. 1a shows TMRE imaging in both tumor and non-tumor (N.T.) window chambers, which is quantified into TMRE uptake curves in Fig. 1b. TMRE uptake kinetics were significantly different in all tumor types compared to N.T. windows, due to increased TMRE uptake in the tumor groups (p < 0.05 for 67NR, 4T07, or 4T1 vs. normal). No difference was seen between tumor groups. Normalizing each uptake curve to its respective TMRE peak demonstrates that both tumor and N.T. groups reach a similar uptake plateau by 40 minutes post-injection (Fig. 1c). TMRE uptake is stable from t = 40–75 minutes post-injection in both normal tissue and tumors, and can thus be measured at any point during the stable imaging window. Fig. 1d shows multi-photon imaging of TMRE and Hoechst 33342 (nuclear stain) in a N.T. window chamber at two time points representing the start and end of the stable window. By 35 minutes post-injection, TMRE signal was localized to mitochondrial-sized features surrounding cell nuclei, and this staining pattern persisted until the end of imaging (75 minutes post-injection). Red-channel background fluorescence was negligible at both timepoints, and non-nuclear signal in the blue channel resulted from second harmonic generation of collagen. The known high binding affinity of TMRE [1] and the multiphoton imaging of TMRE’s mitochondrial localization together indicate that TMRE signal results primarily from mitochondrial regions.
Figure 1.
TMRE in vivo uptake kinetics are robust across normal and tumor groups. (a) Representative images of TMRE fluorescence in non-tumor and in 67NR, 4T07, and 4T1 tumor window chambers. Baseline images were acquired prior to TMRE injection. Tumor regions are shown in the transmission images as areas of increased absorption contrast. (b) Mean TMRE uptake kinetics for the non-tumor and tumor groups. (c) Kinetics for a given mouse were normalized to the mouse’s max TMRE fluorescence during the imaging period, and normalized kinetics were then averaged within a group. (d) Multiphoton imaging of TMRE and Hoechst 33342 in a non-tumor window. Images show two fields of view in the same animal. n = 6 mice (all groups). N.T. = Non-tumor. Error bars = SE. *for p < 0.05.
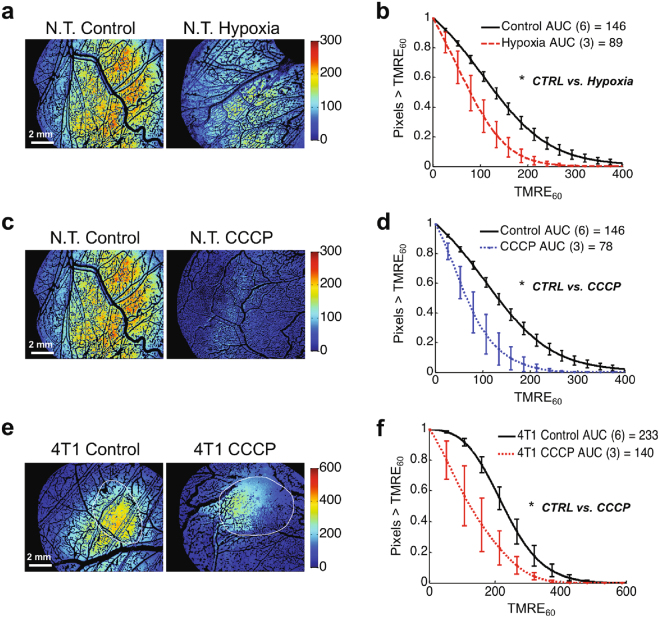
Figure 2.
TMRE responds to established perturbations of mitochondrial membrane potential in vivo in non-tumor and 4T1 tumor windows. Representative images (a) and mean distributions (b) of all TMRE uptake at 60 minutes (TMRE60) pixels for non-tumor mice with control TMRE imaging or TMRE imaging during forced hypoxia (10% inspired O2). Representative images (c) and mean distributions (d) of all TMRE60 pixels for non-tumor mice with control TMRE imaging or TMRE imaging after CCCP pre-treatment. Representative images (e) and mean distributions (f) of all TMRE60 pixels for 4T1 tumor-bearing mice with control TMRE imaging or TMRE imaging after CCCP pre-treatment. Group numbers shown in legend. N.T. = Non-tumor. AUC = area under curve. Error bars = SE. *is p < 0.05.
Three distinct mitochondrial perturbations were tested in non-tumor window chambers. Hypoxia is known to elicit a decrease in mitochondrial metabolism10. Fig. 2a suggests a decrease in TMRE uptake in N.T. windows during hypoxic (10% inspired O2) compared to control (21% inspired O2) conditions. Fig. 2b shows that the distribution of all TMRE60 pixels for the hypoxia group was significantly decreased relative to the control distribution (p < 0.05), as expected. Another group of N.T. window chambers was treated with CCCP, which is known to dissipate mitochondrial membrane potential6, and representative images in Fig. 2c show a qualitative decrease in TMRE uptake in response to CCCP-treatment. Fig. 2d demonstrates that the distribution of all TMRE60 pixels for the CCCP group was significantly decreased relative to control (p < 0.05). Similarly, when 4T1 tumor-bearing window chambers were treated with CCCP, TMRE uptake decreased significantly relative to control (p < 0.05), as shown in the images in Fig. 2e and pixel distribution curves in Fig. 2f. The injection volume and concentration of TMRE were kept consistent across all experiments.
Metabolic and vascular imaging of murine sibling tumor lines of breast cancer
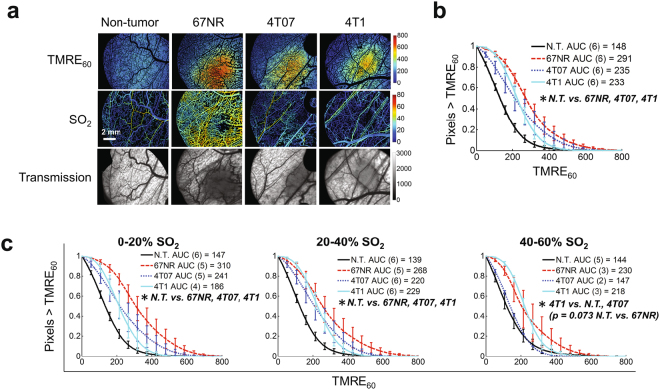
Figure 3 explores the effects of regional SO2 on the distribution of TMRE60 in tumor and N.T. windows. Typical images of TMRE60 and SO2 in Fig. 3a highlight increased TMRE uptake in all tumor types compared to N.T. windows. Transmission images show increased absorption in tumor regions. Fig. 3b shows the distribution of all TMRE60 pixels for each tissue type. TMRE60 was increased in all tumor types relative to N.T. (p < 0.05 N.T. vs. 67NR, 4T07, or 4T1). Fig. 3c takes advantage of the spatial relationships obtained by imaging to show the distribution of TMRE60 at distinct levels of SO2. TMRE60 was increased in tumor relative to N.T. at 0–20% SO2 (all tumor v. N.T. p < 0.05) and 20–40% SO2 (all tumor v. N.T. p < 0.05). At 40–60% SO2, TMRE60 was greater in 4T1 than 4T07 or N.T. (p < 0.05), and greater in 67NR than N.T. (p = 0.073). N.T. and 4T07 were indistinguishable for 40–60% SO2. Oxygen consumption rates were comparable in 67NR and 4T1 cells when measured by a Seahorse mitochondrial assay (Supplementary Fig. S2).
Figure 3.
All tumor types show comparable mitochondrial membrane potential (MMP), and low vascular oxygenation (SO2) enhances differences between tumor and normal MMP. (a) TMRE uptake at 60 minutes (TMRE60) and SO2 in non-tumor and tumor window chambers. Tumor regions are shown in the transmission images as areas of increased absorption contrast. (b) Mean distribution of all TMRE60 pixels for each tissue type. (c) Mean distribution of TMRE60 for each tissue type for distinct levels of regional SO2. Group numbers shown in legend. N.T. = Non-tumor. AUC = area under curve. Error bars = SE. *is p < 0.05.
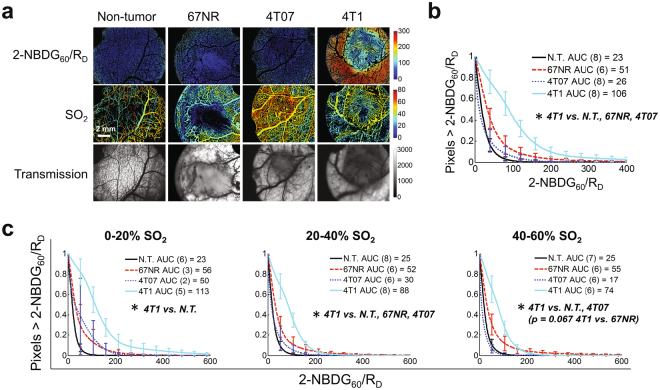
Glucose uptake (2-NBDG60/RD38) was imaged in tumor and N.T. window chambers (Fig. 4a). Fig. 4b shows that the distribution of all 2-NBDG60/RD pixels for 4T1 was dramatically increased relative to all other groups (p < 0.05 4T1 vs. N.T., 67NR, or 4T07). All other comparisons were not significant. Fig. 4c shows that the increased 2-NBDG60/RD in the 4T1 tumors was maintained regardless of SO2 level. 2-NBDG60/RD was increased in 4T1 relative to N.T. at all SO2 (p < 0.05). 2-NBDG60/RD was increased in 4T1 relative to both other tumor lines at 20–40% SO2 (p < 0.05 4T1 v. 67NR or 4T07) and at 40–60% SO2 (4T1 v. 67NR p = 0.067, 4T1 v. 4T07 p < 0.05), but not at 0-20% SO2. Surprisingly, N.T., 67NR, and 4T07 were indistinguishable at all SO2 levels. Results were consistent with a Seahorse assay that showed increased lactate production in 4T1 (Supplementary Fig. S2).
Figure 4.
Glucose uptake is increased in 4T1 regardless of regional oxygenation. (a) Glucose uptake (2-NBDG60/RD) and vascular oxygenation (SO2) in a non-tumor window chamber and non-metastatic (67NR and 4T07) and metastatic (4T1) tumor window chambers. Tumor regions are shown in the transmission images as areas of increased absorption contrast. (b) Mean distribution of all 2-NBDG60/RD pixels for each tissue type. (c) Mean distribution of 2-NBDG60/RD for each tissue type for distinct levels of regional SO2. Group numbers shown in legend. N.T. = Non-tumor. AUC = area under curve. Error bars = SE. *is p < 0.05.
Characterization of the metabolic and vascular landscape in the peritumoral area
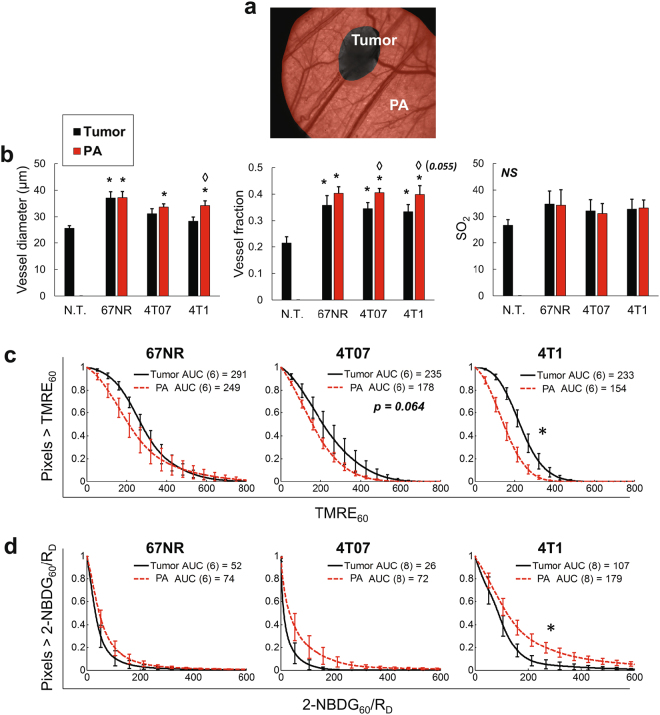
Previous studies have shown that vasculature can be significantly altered in tissue extending well beyond the tumor border55. We segregated each tumor window image into two regions - the tumor and the peritumoral area (PA) - to examine the respective vascular features. As shown in Fig. 5a, transmission images were used to hand-mask tumor regions, and PA was automatically identified as all tissue <5 mm from the tumor57 and >1 mm from the image edge, to avoid artifact. In Fig. 5b, vessel diameter and vessel fraction (the percentage of vascular pixels, i.e. # vascular pixels/# total pixels) in both tumor and PA were consistently differentiated from N.T. Mean SO2 was comparable across groups. The PA of 4T1 and 4T07 (but not 67NR) showed significantly higher vessel fraction compared to the tumor itself (p < 0.05 for 4T07 and p = 0.055 for 4T1). The 4T1 PA also showed a significant increase in vessel diameter relative to the corresponding tumor region (p < 0.05).
Figure 5.
4T1 tumor and peri-tumoral area maintain distinct metabolic and vascular phenotypes. Metabolic and vascular endpoints were quantified for the tumor and peritumoral area (PA) of all tumor types (67NR, 4T07, 4T1). (a) Transmission images were segmented into tumor and peritumoral area (PA) regions. (b) Comparison of mean vascular features in non-tumor tissue and tumor and PA regions of all tumor types. SO2 = vascular oxygenation. (c) TMRE60 in the tumor and PA of all tumor types. (d) 2-NBDG60/RD in the tumor and PA of all tumor types. N.T. = Non-tumor. AUC = area under curve. Error bars = SE. n = 12-14 (b) or as shown in legend (c,d). *is p < 0.05 vs. N.T. (b). ◊ is p < 0.05 tumor vs. PA for same tumor line (b). *is p < 0.05 tumor vs. PA for same tumor line (c,d).
The atypical vascular phenotype of the PAs led us to compare both TMRE60 and 2-NBDG60/RD in tumor and PA regions. In Fig. 5c,d, TMRE60 was significantly decreased and 2-NBDG60/RD was significantly increased in the 4T1 PA relative to the 4T1 tumor (both p < 0.05). 2-NBDG60/RD also showed a borderline increase in the 4T07 PA relative to the 4T07 tumor (p = 0.07). No differences were seen in 67NR tumor and 67NR PA. The PAs were additionally parsed into radial 1 mm regions to determine the effects of distance on vascular and metabolic properties in the PAs, as shown in Supplementary Fig. S3.
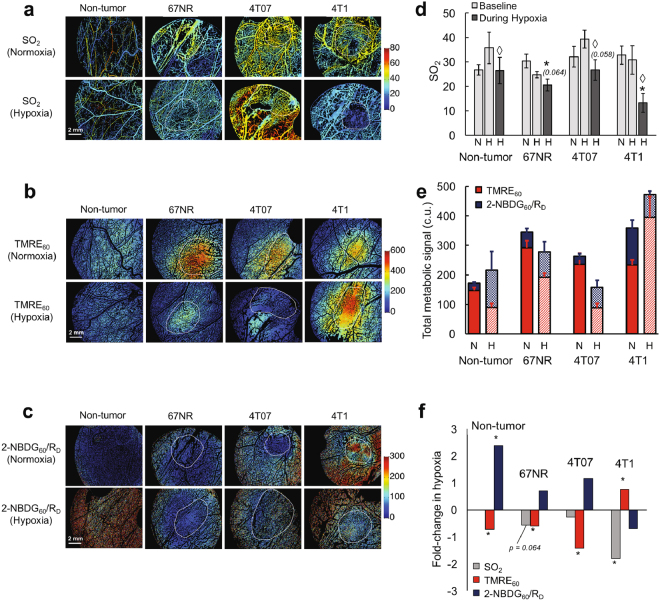
The Effect of Forced Hypoxia on Tumor Metabolism
We next asked whether the metabolic compartmentalization seen in 4T1 tumors and their PAs would correlate with improved ability to maintain mitochondrial metabolism during hypoxia (i.e. Reverse Warburg Effect). Representative images of metabolic endpoints during normoxic baseline conditions (21% inspired O2) and during forced hypoxia (10% inspired O2) are shown in Fig. 6a (SO2), Fig. 6b (TMRE60), and Fig. 6c (2-NBDG60/RD). Note that the changes observed in 4T1 during hypoxia are qualitatively distinct from those seen in all other groups. Mean SO2 for the normoxia and hypoxia groups is shown in Fig. 6d. SO2 was quantified at baseline in mice belonging to both the normoxia and hypoxia groups (shown in light gray). SO2 was also measured during hypoxia, 15 minutes after the induction of hypoxic breathing, in the hypoxia group (shown in dark gray). SO2 decreased in 4T1 (p < 0.05), 4T07 (p = 0.058), and N.T. (p < 0.05) during hypoxia compared to the animal-matched baseline measurements. SO2 decreased in 4T1 (p < 0.05), and to a lesser extent in other groups (p = 0.064 for 67NR), when comparing the hypoxia group (during hypoxia) to the normoxia group. Baseline SO2 was statistically indistinguishable between the normoxia and hypoxia groups for N.T. (p = 0.12), 67NR (p = 0.20), 4T07 (p = 0.33), and 4T1 (p = 0.79).
Figure 6.
Forced hypoxia reveals a switch toward mitochondrial metabolism in 4T1 tumors and toward glycolysis in 67NR and 4T07 tumors and non-tumor tissue. Images of SO2 (%) (a) TMRE60 (b) and 2-NBDG60/RD (c) during normoxic (21% O2) and hypoxic (10% O2) conditions. (d) Mean SO2 for normoxia (N) and hypoxia (H) animal groups. SO2 was measured at baseline (light gray, measured in N and H groups) and during hypoxia (dark gray, measured in H group only). (e) Total metabolic signal (2-NBDG60/RD + TMRE60 fluorescence intensities in calibrated units (c.u.)) during normoxia (N) and hypoxia (H). Red and blue show contributions of TMRE and 2-NBDG, respectively, to the total metabolic signal. (f), Fold-change in mean TMRE60, 2-NBDG60/RD, and SO2 during hypoxia compared to normoxia (fold-change = MeanHYPOXIA/MeanNORMOXIA). Normoxia: n = 6–8 (TMRE60 and 2-NBDG60/RD) and n = 11–14 (SO2). Hypoxia: n = 3 (TMRE60 and 2-NBDG60/RD) and n = 5–6 (SO2). N.T. = Non-tumor. Error bars = SE. Tumor outlines shown in white. *is p < 0.05 vs. normoxsia group (D,F). ◊is p < 0.05 vs. hypoxia group baseline (d).
The total metabolic signal for each group during normoxia and hypoxia is quantified in Fig. 6e, where total metabolic signal is the sum of calibrated 2-NBDG60/RD and TMRE60 fluorescence intensities. Red and blue portions of the bar show contributions of TMRE and 2-NBDG, respectively, to the total metabolic signal, to allow for qualitative visualization of metabolic changes during hypoxia. It is evident that there is a shift towards increased glycolysis in N.T., 4T07 and 67NR tumors while there is an increase in mitochondrial metabolism in the 4T1 tumors under hypoxic stress.
For each endpoint in Fig. 6d and e, the fold-change from normoxia to hypoxia was calculated as fold-change = MeanHYPOXIA/MeanNORMOXIA and shown in Fig. 6f. Significance was established with a two-sided t-test that compared the normoxic and hypoxic groups for each endpoint. N.T., 67NR, and 4T07 all experienced a decrease in TMRE60 (all p < 0.05), and an increase in 2-NBDG60/RD (p < 0.05 for N.T.). 67NR also experienced a borderline decrease in SO2 (p = 0.064). On the other hand, 4T1 experienced a significant increase in TMRE60 and decreases in SO2 (p < 0.05) and 2-NBDG60/RD (p = NS). Changes in TMRE60 and 2-NBDG60/RD were complementary; when one endpoint decreased during hypoxia, the other increased without exception. The full pixel distributions for endpoints (SO2, TMRE60, and 2-NBDG60/RD) are shown for all normoxia and hypoxia groups in Supplementary Fig. S4.
Discussion
Considering the popularity of cancer metabolism for diagnosis, prognosis, and treatment, there is a surprising lack of in vivo metabolic imaging strategies that can be easily incorporated into pre-clinical studies. Current gold standards for in vivo vascular and metabolic imaging, though improving, lack the spatial and temporal resolution needed to examine local tumor heterogeneity22. Metabolomics19 and Seahorse extracellular flux analyzer18 assays provide invaluable information, but are inherently destructive and therefore not amenable to examining the tumor landscape. There is a need for complementary tools that can bridge the gap between multi-parametric ex vivo analysis and low-resolution whole body imaging; in vivo reporters of mitochondrial activity are particularly needed. To address these gaps, we designed a metabolic imaging strategy that incorporates endpoints for glucose uptake (2-NBDG60/RD38), mitochondrial membrane potential (TMRE60), and vascular oxygenation (SO238,39), all imaged using the same technology and in two unique combinations (2-NBDG + SO2, TMRE + SO2).
We first validated TMRE for use in vivo. TMRE reports MMP by accumulating as the charge across the mitochondrion becomes more negative, thus causing an increase in fluorescence intensity58. TMRE was chosen for the study because it has several benefits such as increased mitochondrial binding and rapid equilibration59, which makes it particularly suitable for in vivo studies. The few published studies that use TMRE in vivo46,60 beautifully demonstrate the probe’s utility, but the studies are typically qualitative and focused on other endpoints. Our study expands upon this work by including a recommended TMRE dose, providing TMRE uptake kinetics in both normal and tumor models, and showing that TMRE responds to multiple validated perturbations. Multiphoton imaging of TMRE’s mitochondrial localization indicated that TMRE signal resulted primarily from mitochondrial regions, and administration of hypoxia and CCCP in normal and/or tumor window chambers diminished TMRE uptake, consistent with expectations from literature6,10. Our group also recently demonstrated that TMRE uptake decreased in N.T. window chambers after treatment with 2-deoxyglucose (2-DG)61. 2-DG is a well-known inhibitor of glucose utilization62 which has been shown to cause loss of mitochondrial membrane potential63. In the same study, no change in MMP was seen after administration of glucose61.
Increased MMP in tumor relative to normal tissue was consistent with previous literature that indicates hyperpolarized mitochondria are common across many cancers6,7,64. Regional analysis showed that the trend was driven by tumor regions with low (0–20%) and intermediate (20–40%) SO2 levels, at which tumor and normal tissues were most easily distinguished. Our previous work with window chamber and flank tumor models indicates that an average SO2 of 20–40% is expected in these lines38,65,66. Analysis confirmed that the increased TMRE uptake in tumors relative to non-tumor tissue was not a function of altered vascular properties in the tumor windows. Pearson’s correlation tests revealed that mean TMRE60 was not correlated with vessel fraction (R2 = 0.017, p = 0.55), nor was TMRE60 correlated with vessel diameter (R2 = 0.028, p = 0.43; data not shown). Further, initial uptake kinetics and fluorescence plateau times were observed to be similar between normal and tumor groups, indicating that probe delivery was not impaired in either the tumor or non-tumor group.
Based on previous studies relating increased MMP with aggressiveness3,67–69, we hypothesized that MMP would correlate with metastatic potential in our study (4T1 > 4T07 > 67NR), but MMP was comparable across tumor types. The comparable MMP observed here contrasts with previous studies in the same cell lines that showed that TCA cycle intermediates increased with metastatic potential70 and that 67NR cells had decreased oxygen consumption relative to 4T1 cells2. Our studies did not indicate distinct differences in overall OXPHOS, since MMP and SO2 were consistent across tumor groups and oxygen consumption rates were equally robust in 67NR and 4T1 cells when measured by a Seahorse mitochondrial assay. It is notable that our study measures MMP in vivo, compared with the TCA cycle intermediate study, which was performed in vitro6. Further investigation would be needed to pinpoint the difference between the studies, however, previous work has shown stark differences in the in vitro and in vivo metabolic phenotypes of cell lines including MDA-MB-231 and SiHa71. Further, the Simoes Seahorse study utilized cell media with increased glucose and glutamine concentrations (25 mM glucose and 6 mM glutamine2) compared to our Seahorse study (12.5 mM glucose and 2 mM glutamine), which could have unknown effects on the observed phenotypes.
A validated surrogate of glucose uptake, 2-NBDG, enabled us to test the hypothesis that 4T1 tumors could utilize glycolysis more readily than their non-metastatic counterparts, as previously seen during hypoxia in vitro2. The 4T1 displayed a classic Warburg effect, with increased glucose uptake at all SO2 levels while glucose uptake was consistently low in N.T., 67NR, and 4T07 tumors. Importantly, mean glucose uptake was not sufficient to distinguish between 4T1 and 67NR, but comparing the distributions of glucose uptake did allow for differentiation between these two groups, highlighting the significance of obtaining spatial data. The increased glucose uptake in 4T1 was maintained across all ranges of SO2. Multiple in vivo studies by our lab and others have shown concordant evidence in support of the Warburg effect in 4T12,38.
Previous work has highlighted the peritumoral area (PA) as the site of intensive angiogenesis in human head and neck cancers55, and fibroblasts from the PA have been shown to promote phenotypic changes in tumor cells57. Assessing the PA of each tumor group in our study revealed that abnormal vascular features indeed extended well beyond the tumor boundary. Key features we observed included increased vessel diameter, comparable to what our group observed during spontaneous carcinogenesis in a hamster cheek pouch model72. One notable difference from our hamster study was the increased vessel fraction that we observed here, likely because the tumors in our study were angiogenic, yet too small to have developed avascular or necrotic areas73. Interestingly, vessels in the 4T1 PAs were even more abnormal than in the corresponding subject-matched tumors that they neighbored.
Abnormal vascular features in the PAs prompted further comparison of metabolism in the PA and tumor areas, since angiogenesis has been shown to recruit cancer associated fibroblasts (CAFs)56. It was recently hypothesized that tumors act symbiotically with such fibroblasts to compartmentalize metabolism and decrease competition for resources11. 4T1 tumors have been shown to have higher levels of Wnt7a than 4T07 tumors, which promoted in vivo fibroblast recruitment and activation74. A separate study showed that co-culturing 4T1 cells with CAFs enhanced the growth of 3D tumor clusters75. The RWE has been directly observed in both the primary tumor and lymph node metastases of other metastatic breast cancers76, and increased glycolytic markers in the tumor microenvironment predicted for poor patient survival in clinical breast cancer77. A pre-clinical study of MDA-MB-231 breast cancer demonstrated that simulating the RWE by administering aerobic glycolysis by-products caused increased tumor metastasis compared to control78. In the same study, ex vivo tissue analysis of tumor and adjacent stromal tissue showed a transcriptional shift toward mitochondrial metabolism in the tumor tissue. We observed increased metabolic compartmentalization consistent with the RWE in metastatic 4T1 tumors, since glucose uptake was increased in the PA and MMP was increased in the tumor.
We sought to test the hypothesis that the RWE in 4T1 tumors would allow them to maintain mitochondrial activity during acute hypoxia, since a glycolytic PA could provide fuel for OXPHOS while decreasing competition for oxygen. Surprisingly, MMP was not only maintained, but actually increased in 4T1 tumors during an hour of forced hypoxia without significant change in the steep metabolic gradients between the PA and the tumor (Supplementary Fig. S5). MMP decreased in all other groups over the same period. Importantly, monitoring changes in SO2 and glucose during the hypoxic perturbation gave crucial context for interpreting the changes in MMP. In groups that had increased glucose uptake and decreased MMP during hypoxia (N.T., 67NR, and 4T07) decreases in SO2 were not significant, suggesting diminished oxygen consumption. On the other hand, the increase in MMP in 4T1 correlated with a drastic and significant decrease in SO2, consistent with increased oxygen consumption. Correlation between increased MMP and respiration has been seen during hypoxia in cell studies14. If there was no indication of oxygen consumption in our study as reflected by SO2, a transient increase in MMP could have indicated reverse proton-pumping which has been seen in the progression toward hypoxia-induced necrosis in colorectal cancer cells79. This underscores the importance of measuring multiple metabolic endpoints, as well as concomitant changes in SO2, for appropriate interpretation of metabolic behavior.
A previous study showed that a loss of Bnip-3 protein expression in 4T1 cells enabled them to escape hypoxia-induced apoptosis53. Whereas cleaved caspase-3 (suggestive of apoptosis) increased after 6 hours of hypoxia in 67NR and 4T07 tumors, it decreased in 4T1 tumors during the same time period. During hypoxia, increased HIF-1α is known to upregulate expression of Bnip-3, toward mitochondrial autophagy10. Since Bnip-3 can impair respiration and cause a loss of MMP80, there may be a link between downregulated BNIP3 in 4T1 and maintenance of hypoxic mitochondrial function. A recent study found increased PGC-1α expression in 4T1 cells exposed to hypoxia, and saw that PGC-1α was responsible for increased mitochondrial biogenesis and metabolism15. Optical imaging of the redox ratio of endogenous FAD and NADH fluorescence also detected increased mitochondrial metabolism in 4T1 cells after exposure to hypoxia and increased glycolysis in the 67NR cells, consistent with our results shown in Fig. 681.
Distinct mitochondrial responses to hypoxia were also recently seen in a panel of hepatocellular carcinomas and primary hepatocytes, where particularly aggressive cancer cells, but not primary cells, showed an increase in MMP and oxidative enzymes during hypoxia14. In that study, however, aggressive tumors also showed stark hypoxia-induced increase in glycolytic enzymes, which would be consistent with known HIF-1-dependent metabolic changes10. Other studies have shown that glutamine, and not glucose, is the major carbon source for OXPHOS-driven ATP production in cancer cells even during hypoxia82. Interestingly, an in vitro study showed that succinate dehydrogenase expression increased in 4T1 during hypoxia, but only when glutamine was available2. This finding, along with our observation that 4T1 tumors increased MMP yet decreased glucose uptake during hypoxia, may point to glutamine as an alternate fuel for mitochondrial metabolism during hypoxia in vivo, contrary to in vitro 4T1 behavior that was strongly glycolytic during hypoxia2.
Further study is required to determine the reason why metabolic compartmentalization affects only the 4T1 tumors, while all tumors had comparable vascular phenotypes. Because our study looks at tumors at an early time point (7–10 days), we are likely detecting a metabolic shift that precedes overt vascular changes in 4T1. The finding would not be surprising, since metabolic changes can be attributed to multiple factors which can be either independent from or related to neovascularization. Increased metabolism preceding the recruitment of new vessels in cancer would be consistent with published literature of diverse tumor types83, and pyruvate produced by glycolysis is known to be pro-angiogenic84. Further, studies have seen that dietary restriction can greatly reduce tumor vascularization85, supporting the role of metabolism in vessel growth. On the other hand, the changes may share a common upstream regulator; for example, expression of HIF-1α transcription factor can cause both metabolic and vascular changes86. It should be noted, though, that the glycolytic products lactate and pyruvate have been shown to be necessary for accumulation of HIF-1α87, and this phenomenon has interestingly been shown to affect oxidative but not aerobically glycolytic cells88. The precise relationship between cancer’s metabolic and vascular changes and the timing of each continues to be a subject of much interest, and we hope that our study contributes to the body of knowledge on this topic.
Similarly, while there were clear differences in metabolism that correlated with metastatic potential in this study, additional studies are needed to determine whether these findings can be generalized beyond the 4T1 family to other triple-negative breast cancers (TNBCs) or tumor types with varying metastatic potential. In contrast to the 4T1, an in vitro study of TNBC line MDA-MB-231 showed that the MDA-MB-231 cells maintained high levels of glycolysis through metabolic complementarity with oxidative CAFs89. A separate study showed that circulating tumor cells isolated from in vivo models of MDA-MB-231 and 4T1 had enhanced mitochondrial respiration, with no significant change in glycolysis, relative to the primary tumors15. The enhanced mitochondrial activity mediated through PGC-1α was required for metastatic dissemination. Recently, Neveu, et al., showed that in vitro MDA-MB-231 cells were glycolytic and insensitive to changes in oxygenation; in the same study, they showed that in vivo MDA-MB-231 tumors reduced glycolysis upon exposure to carbogen breathing71. Taken together, these studies indicate that consideration of not only the cell line, but also the experimental model and oxygen status, is crucial for metabolic phenotyping.
Regarding our technique, the following cautions should be considered. As discussed above, the TCA cycle in tumors can be fueled by a host of different carbon sources including glucose (following glycolysis)90, glutamine (following glutaminolysis)90, and fatty acids (following fatty acid oxidation)91. Use of any of these substrates can maintain mitochondrial membrane potential. Though mitochondrial membrane potential captures an important downstream component of mitochondrial metabolism, a limitation of the endpoint is that it cannot distinguish which carbon source is being used in the TCA cycle. Information on metabolic heterogeneity, spatial relationships, and vascular morphology obtained from optical imaging can be coupled with information on metabolic pathway intermediates obtained from metabolomics or magnetic resonance spectral imaging to provide a truly holistic view of a tumor’s metabolic preferences.
Next, the use of an athymic nude mouse model cannot fully replicate the tumor microenvironment seen in an immune competent host. For this preliminary study, athymic mice were chosen so that we could phenotype a more homogeneous tumor cell population without confounding immune factors, while maintaining the presence of peri-tumoral fibroblasts56. Though optical imaging represents an inherent trade-off between resolution and penetration depth, the window chamber has proven an invaluable platform for studying metabolism and angiogenesis in vivo in breast cancer92–98. Tumors grown in this model develop hypoxia47 and interact with the existing host vasculature99. Further, our characterization in this study showed that the peri-tumoral area was characterized by angiogenesis and hyper-metabolism, features which have been seen in ex vivo studies of patient tumors55,77. Since a recent study showed that 4T1 and 4T07 cells have different metabolic properties when grown in high or low density matrix100, further investigation into the exact make-up of the tumor microenvironment in our model will be critical before comparison to other models. In this single-timepoint study we were unable to definitively distinguish between pre-existing and neovascular vessels; in future studies, subtraction of vascular images taken before and after tumor inoculation will enable characterization of each vessel subset. Lastly, for this study it was necessary to image 2-NBDG and TMRE endpoints in separate cohorts of mice to validate our method. Future work will focus on the integration of endpoints for holistic imaging on a single tumor, as well as calibration of both fluorescence endpoints to an objective energy measurement such as ATP production to allow calculation of a standalone “energy budget”. We believe that in vivo imaging of glucose uptake, MMP, and vascular features simultaneously in the same animal will prove useful as a complementary new technique for the study of tumor metabolism.
Materials and Methods
Ethics Statement
All in vivo experiments were conducted according to a protocol approved by Duke University Institutional Animal Care and Use Committee (Protocol A114-15-04).
Murine cancer cell lines
Three murine mammary carcinoma cell lines arising from the same spontaneous murine breast tumor were used in the study53,54,101. 67NR and 4T07 are non-metastatic; 67NR fails to leave the primary site, and 4T07 disseminates cells but cannot form metastatic nodules101. 4T1 are highly metastatic to lung, liver, bone, and brain101. The 4T1 family is typically considered a triple negative breast cancer model (ER-/PR-/HER-)75,81, although nuclear estrogen receptor alpha positivity has been observed in 67NR102. The 4T1 and 4T07 cells were acquired from the American Type Culture Collection, and the 67NR cells were generously provided by Dr. Fred Miller (Karmanos Cancer Institute, Detroit, MI) through Dr. Inna Serganova and Dr. Jason Koucher (Memorial Sloan Kettering Cancer Center, New York, NY). Cell lines were passaged every 2-3 days in RPMI-1640 medium (L-glutamine) with 10% fetal bovine serum (FBS) and 1% antibiotics (Pen Strep). For in vivo injection, cells were prepared in sterile RPMI-1640 containing no FBS nor antibiotics.
Imaging probes
TMRE reports mitochondrial membrane potential by accumulating in proportion to MMP and causing an increase in fluorescence intensity58. TMRE was chosen for the study because its superior mitochondrial binding and rapid equilibration59 are beneficial for in vivo experiments. For in vivo administration, TMRE (Tetramethylrhodamine Ethyl Ester, Life Technologies/ThermoFisher) was diluted to a final concentration of 25 μM in sterile PBS. 2-NBDG (2-(N-(7-Nitrobenz-2-oxa-1,3-diazol-4-yl)Amino)-2-Deoxyglucose, Duke University Small Molecule Facility) was diluted to a final concentration of 6 mM. The total volume of each in vivo injection was 100 μL. The 2-NBDG dose was optimized in a prior publication38. The TMRE dose was chosen to keep the final concentration of TMRE well below 50 nM at the tissue level so that it operates in non-quenching mode and causes the least disturbance to electron transport45. For the current study, an injection of 100 μL of 25 µM TMRE gave a final tissue-level TMRE concentration range of 3.8-13.4 nM in normal tissue and tumors, calculated from tissue-mimicking phantoms (not shown).
Dorsal skin flap window chamber model
Titanium window chambers were surgically implanted on the back of 8-12 week old female athymic nude mice (nu/nu, Duke DLAR Breeding Core, Durham, NC) using an established procedure103. We injected a 50 μL suspension (~1 × 105 cells) of 4T1, 4T07, or 67NR cells into the dorsal skin fold and placed a glass coverslip (dia = 12 mm, No. 2) over the exposed tissue. Tumors were allowed to grow for 5–7 days before imaging. N.T. window chambers received no cell injection. All tumors used for imaging in this study had a tumor volume <150 mm3. All animals were housed in an on-site housing facility with ad libitum access to food and water and standard 12-hour light/dark cycles.
Hyperspectral imaging of metabolic and vascular endpoints
For a 6-hour period prior to imaging, the animals were only provided with water. At the end of 6 hours of fasting, we initially recorded trans-illumination (vascular) images and corresponding background fluorescence images. In addition, a free space trans-illumination image using appropriate neutral density filters was recorded after every imaging session to account for daily variations in light intensity. The animals were administered a 100 μL tail-vein injection of 25 μM TMRE or 6 mM 2-NBDG in sterile PBS, and fluorescence images were captured for 75 minutes. We used a Zeiss Axioskop 2 microscope fitted with an LCTF, previously described in detail50, for all imaging. A 2.5 × objective lens (NA = 0.075) was used to yield a FOV of 9 mm with a resolution of 17.5 μm. Imaging excitation/emission wavelengths were 540 ± 20 nm/590 ± 5 nm for TMRE and 470 nm ± 20 nm/525 nm ± 5 nm for 2-NBDG.
An image acquisition time of 600–800 ms was used for both 2-NBDG and TMRE imaging. All fluorescent images were background fluorescence-subtracted and calibrated for integration time with a Rhodamine B standard solution prior to data analysis or visualization. During baseline (normoxia) measurements, the animals were allowed to breathe 21% oxygen. For the hypoxia group, the animals were subjected to breathing 10% oxygen for 15 minutes prior to imaging and through the end of imaging. Animals were anesthetized under inhaled isoflurane (1–1.5% v/v) in room air or hypoxic gas for the duration of imaging.
Separate cohorts of animals also received treatment with 50 µM CCCP. CCCP (carbonyl cyanide 3-chlorophenylhy-drazone, Sigma Aldrich) was diluted to a final concentration of 50 μM in DMSO. After animals were anesthetized with inhaled isoflurane (1–1.5% v/v) in room air, the window glass was removed and 0.1 mL of CCCP was topically applied to the tissue. The glass was immediately replaced, and imaging began 5 minutes later, following the imaging procedure used for all other groups.
Multiphoton imaging of TMRE in a window chamber
One N.T. mouse was imaged with an Olympus FV1000 Multiphoton microscope, which we have previously described65. Hoechst 33342 (bisBenzimide H33342 trihydrochloride, Cell Signaling Technologies) was diluted to a final concentration of 2 mg/mL in sterile PBS. To visualize nuclei, the mouse received a 100 µL injection of Hoechst 33342 subcutaneously in the window chamber 15 minutes prior to injection of TMRE. TMRE was injected via tail vein following the standard dosing procedure. We used a two-photon excitation wavelength of 900 nm and collection wavelength ranges of 420–460 nm for Hoechst 33342 and 575–630 nm for TMRE.
Calculation of vascular and metabolic parameters
Transmission images were collected in 10 nm increments from 520–620 nm and used to create an image cube (x, y, λ). A modified form of the Beer-Lambert law was fit to the trans-illumination image cube (x, y, λ) to obtain the concentration of the primary absorbers, oxy [HbO2] and deoxy-hemoglobin [dHb], at each pixel47. We then calculated total hemoglobin content, [THb] ([HbO2] + [dHb]), and SO2 ([HbO2]/[THb]) at each pixel. A binary mask was created from the presence or absence of [THb] in the transmission image cube, and used to segment the images into vascular and tissue space, respectively. Other vascular endpoints (length, diameter, tortuosity, area fraction) were quantified from the binary mask with in-house software that was extensively validated elsewhere104. The vessel diameter was calculated at each vessel midpoint, and all diameters within a region of interest were averaged to obtain a mean vessel diameter. The vessel fraction was defined as VF = (#vascular pixels/#total pixels) in the region of interest.
For tumor groups, the data shown corresponds only to pixels within the tumor region and excludes the surrounding tissue. Since increased scattering (due to cellularity105) and increased absorption (due to angiogenesis106) are well-known optical properties of tumors, we used regions of decreased light transmission in the 540 nm white light images to identify tumor tissue. Further, visual inspection and palpation of the tissue side of the window chamber aided clear identification of tumor regions. To avoid bias, hand traced masks were created for each tumor region by viewing the white light (transmission) images only, prior to viewing the corresponding metabolic endpoint images (2-NBDG, TMRE, or SO2). Further demonstration of the masking procedure is provided in Supplementary Fig. S1. Due to low excitation efficiency near the edge of the window chambers, tissue less than 1 mm from the chamber edge was masked using an automated process and excluded from analysis; this process was applied to all groups.
We chose to study TMRE uptake at 60 minutes (TMRE60) to correspond in time to the previously validated glucose uptake endpoint 2-NBDG60/RD (2-NBDG uptake at 60 minutes corrected by a delivery factor38,39). We confirmed that TMRE signal was stable over the imaging period and responsive to known perturbations of MMP (Figs 1 and 2). Pixels in the tissue space of TMRE60 or 2-NBDG60/RD images were used to create a pixel distribution curve (1-cumulative distribution) for each animal, and the individual pixel distribution curves were averaged to create the curves shown (mean ± SE). Area under the curve (AUC) was calculated for each mean pixel distribution curve.
TMRE60 and 2-NBDG60/RD were additionally parsed by SO2. For each TMRE60 or 2-NBDG60/RD image, every tissue pixel in the tumor area was assigned to an SO2 group according to the SO2 of the nearest vascular pixel. In a given image, there were as many as three SO2 bins: 0–20% SO2, 20–40% SO2, and 40–60% SO2. The distribution of TMRE60 or 2-NBDG60/RD pixel intensities within each SO2 group was represented as a pixel distribution curve. Each final curve then represents the mean distribution (±SE) of TMRE60 or 2-NBDG60/RD values in a given SO2 “bin”, for all mice containing image pixels in that SO2 bin.
Statistical analysis
The cohort sizes were based on an expected average change in mitochondrial membrane potential between normal and tumor tissue based on previous literature (N.T. MMP ≈ −140 mV [3], Tumor MMP ≈ −200 to −220 mV [4, 5]). The study was powered to detect a small range of Cohen’s d effect sizes between d = 1.5 and d = 2. These effect sizes correspond to a standard deviation of 52 (for d = 1.5) to a standard deviation of 40 (for d = 2.0). Our data has a standard deviation around 50, which gives an effect size d ≈ 1.6 and minimum sample size n = 6 for each group, assuming normality and group means of 220 and 140, to attain 80% power at a 5% level of significance. Mean metabolic and vascular properties were compared with one-way ANOVA tests of log-transformed data. Tukey-Kramer post-hoc tests were used for all ANOVA. A two-sided t-test was used to compare normoxic and hypoxic conditions for a single endpoint. A paired t-test compared animal-matched tumor and PA vascular properties or animal-matched SO2 at baseline and post-hypoxia.
Whenever reasonable, we used the distribution of all pixels from each image to increase the number of data points for our analysis. For comparisons of pixel distribution curves, we used a repeated measures Kolmogorov–Smirnov test, which does not make an assumption of independence for pixels arising from the same mouse. Empirical p-values were calculated for the Kolmogorov-Smirnov statistic using blocked permutation (n = 1000 random permutations per test), prior to binning data for graphing. Error bars show standard error. P-values are indicated as * for p < 0.05. MATLAB (MathWorks, USA) Statistics Toolbox was used for all tests. One 67NR SO2 was excluded as a statistical outlier (determined by Grubbs test, α = 0.05) and one 4T1 hypoxia SO2 was excluded due to a recorded experimental error; no other data was thrown out.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Electronic supplementary material
Acknowledgements
Thank you to Dr. Fred Miller; Karmanos Cancer Institute, Detroit, MI for the original identification and dissemination of the 67NR cell line. Many thanks to Dr. Jason Koutcher, Dr. Inna Serganova, and Dr. Natalia Kruchevsky at Memorial Sloan Kettering Cancer Center for generously providing and arranging delivery of the 67NR cell line to our lab. Thank you Megan Madonna for helpful discussions during manuscript preparation. We would also like to acknowledge Dr. Greg Palmer and Ken Young for experimental troubleshooting and protocol assistance. This work was supported by generous funding from the Department of Defense Era of Hope Scholar Award (http://cdmrp.army.mil/search.aspx; Award number W81XWH-09-1-0410). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author Contributions
Conception and design of experiments was done by A.F.M., S.S.M., Ni.R. Development of methodology was performed by A.F.M., S.S.M., M.W.D., Ni.R. Acquisition of data by M.L., H.A.M., C.Z., H.L.M., K.A., Na.R. Analysis and interpretation of data by A.F.M., S.S.M., B.T.C., A.E. Writing of the manuscript by A.F.M. with input from all authors. Administrative, technical, or material support provided by A.N.F. Study supervision by M.W.D. and Ni.R.
Competing Interests
Dr. Ramanujam has founded a company called Zenalux Biomedical and she and other team members have developed technologies related to this work where the investigators or Duke may benefit financially if this system is sold commercially.
Footnotes
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-22480-w.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Koppenol WH, Bounds PL, Dang CV. Otto Warburg’s contributions to current concepts of cancer metabolism. Nat Rev Cancer. 2011;11:325–337. doi: 10.1038/nrc3038. [DOI] [PubMed] [Google Scholar]
- 2.Simoes RV, et al. Metabolic plasticity of metastatic breast cancer cells: adaptation to changes in the microenvironment. Neoplasia. 2015;17:671–684. doi: 10.1016/j.neo.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Viale, A., Corti, D. & Draetta, G. F. Tumors and Mitochondrial Respiration: A Neglected Connection. Cancer Res, 10.1158/0008-5472.CAN-15-0491 (2015). [DOI] [PubMed]
- 4.Epstein T, Xu L, Gillies RJ, Gatenby RA. Separation of metabolic supply and demand: aerobic glycolysis as a normal physiological response to fluctuating energetic demands in the membrane. Cancer & metabolism. 2014;2:7. doi: 10.1186/2049-3002-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vowinckel J, Hartl J, Butler R, Ralser M. MitoLoc: A method for the simultaneous quantification of mitochondrial network morphology and membrane potential in single cells. Mitochondrion. 2015;24:77–86. doi: 10.1016/j.mito.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Onoe S, Temma T, Shimizu Y, Ono M, Saji H. Investigation of cyanine dyes for in vivo optical imaging of altered mitochondrial membrane potential in tumors. Cancer medicine. 2014;3:775–786. doi: 10.1002/cam4.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen LB. Mitochondrial membrane potential in living cells. Annual review of cell biology. 1988;4:155–181. doi: 10.1146/annurev.cb.04.110188.001103. [DOI] [PubMed] [Google Scholar]
- 8.Weinberg SE, Chandel NS. Targeting mitochondria metabolism for cancer therapy. Nature chemical biology. 2015;11:9–15. doi: 10.1038/nchembio.1712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heiden MGV, Cantley LC, Thompson CB. Understanding the Warburg Effect: The Metabolic Requirements of Cell Proliferation. Science. 2009;324:1029–1033. doi: 10.1126/science.1160809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Semenza GL. HIF-1: upstream and downstream of cancer metabolism. Curr Opin Genet Dev. 2010;20:51–56. doi: 10.1016/j.gde.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee M, Yoon JH. Metabolic interplay between glycolysis and mitochondrial oxidation: The reverse Warburg effect and its therapeutic implication. World journal of biological chemistry. 2015;6:148–161. doi: 10.4331/wjbc.v6.i3.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Busk M, et al. Aerobic glycolysis in cancers: implications for the usability of oxygen-responsive genes and fluorodeoxyglucose-PET as markers of tissue hypoxia. International journal of cancer. 2008;122:2726–2734. doi: 10.1002/ijc.23449. [DOI] [PubMed] [Google Scholar]
- 13.Chiche J, et al. Hypoxic Enlarged Mitochondria Protect Cancer Cells From Apoptotic Stimuli. J Cell Physiol. 2010;222:648–657. doi: 10.1002/jcp.21984. [DOI] [PubMed] [Google Scholar]
- 14.Li, P. Y. et al. Redox homeostasis protects mitochondria through accelerating ROS conversion to enhance hypoxia resistance in cancer cells. Sci Rep-Uk6, 10.1038/Srep22831 (2016). [DOI] [PMC free article] [PubMed]
- 15.LeBleu VS, et al. PGC-1α mediates mitochondrial biogenesis and oxidative phosphorylation in cancer cells to promote metastasis. Nat Cell Biol. 2014;16:992–1003. doi: 10.1038/ncb3039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Porporato PE, et al. A mitochondrial switch promotes tumor metastasis. Cell reports. 2014;8:754–766. doi: 10.1016/j.celrep.2014.06.043. [DOI] [PubMed] [Google Scholar]
- 17.Pavlides S, et al. The reverse Warburg effect Aerobic glycolysis in cancer associated fibroblasts and the tumor stroma. Cell Cycle. 2009;8:3984–4001. doi: 10.4161/cc.8.23.10238. [DOI] [PubMed] [Google Scholar]
- 18.de Moura MB, Van Houten B. Bioenergetic Analysis of Intact Mammalian Cells Using the Seahorse XF24 Extracellular Flux Analyzer and a Luciferase ATP Assay. Molecular Toxicology Protocols, 2nd Edition. 2014;1105:589–602. doi: 10.1007/978-1-62703-739-6_40. [DOI] [PubMed] [Google Scholar]
- 19.Liu X, Ser Z, Locasale JW. Development and quantitative evaluation of a high-resolution metabolomics technology. Analytical chemistry. 2014;86:2175–2184. doi: 10.1021/ac403845u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James ML, Gambhir SS. A molecular imaging primer: modalities, imaging agents, and applications. Physiological reviews. 2012;92:897–965. doi: 10.1152/physrev.00049.2010. [DOI] [PubMed] [Google Scholar]
- 21.Cho HJ, et al. Noninvasive Multimodality Imaging of the Tumor Microenvironment: Registered Dynamic Magnetic Resonance Imaging and Positron Emission Tomography Studies of a Preclinical Tumor Model of Tumor Hypoxia. Neoplasia. 2009;11:247–U245. doi: 10.1593/neo.81360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ramamonjisoa N, Ackerstaff E. Characterization of the Tumor Microenvironment and Tumor-Stroma Interaction by Non-invasive Preclinical Imaging. Frontiers in oncology. 2017;7:3. doi: 10.3389/fonc.2017.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glunde K, Bhujwalla ZM. Metabolic Tumor Imaging Using Magnetic Resonance Spectroscopy. Semin Oncol. 2011;38:26–41. doi: 10.1053/j.seminoncol.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gillies RJ, Morse DL. In vivo magnetic resonance spectroscopy in cancer. Annu Rev Biomed Eng. 2005;7:287–326. doi: 10.1146/annurev.bioeng.7.060804.100411. [DOI] [PubMed] [Google Scholar]
- 25.Gimi B, et al. Molecular imaging of cancer: Applications of magnetic resonance methods. P Ieee. 2005;93:784–799. doi: 10.1109/JPROC.2005.844266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alonzi R, et al. Antivascular Effects of Neoadjuvant Androgen Deprivation for Prostate Cancer: An In Vivo Human Study Using Susceptibility and Relaxivity Dynamic Mri. Int J Radiat Oncol. 2011;80:721–727. doi: 10.1016/j.ijrobp.2010.02.060. [DOI] [PubMed] [Google Scholar]
- 27.Taylor NJ, et al. BOLD MRI of human tumor oxygenation during carbogen breathing. J Magn Reson Imaging. 2001;14:156–163. doi: 10.1002/jmri.1166. [DOI] [PubMed] [Google Scholar]
- 28.O’Connor JPB, Jackson A, Parker GJM, Jayson GC. DCE-MRI biomarkers in the clinical evaluation of antiangiogenic and vascular disrupting agents. Brit J Cancer. 2007;96:189–195. doi: 10.1038/sj.bjc.6603515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fuss M, et al. Tumor angiogenesis of low-grade astrocytomas measured by dynamic susceptibility contrast-enhanced MRI (DSC-MRI) is predictive of local tumor control after radiation therapy. Int J Radiat Oncol. 2001;51:478–482. doi: 10.1016/S0360-3016(01)01691-1. [DOI] [PubMed] [Google Scholar]
- 30.Skala MC, et al. In vivo multiphoton microscopy of NADH and FAD redox states, fluorescence lifetimes, and cellular morphology in precancerous epithelia. P Natl Acad Sci USA. 2007;104:19494–19499. doi: 10.1073/pnas.0708425104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Walsh AJ, et al. Optical Metabolic Imaging Identifies Glycolytic Levels, Subtypes, and Early-Treatment Response in Breast Cancer. Cancer Research. 2013;73:6164–6174. doi: 10.1158/0008-5472.CAN-13-0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Georgakoudi, I. & Quinn, K. P. Optical Imaging Using Endogenous Contrast to Assess Metabolic State. Annual Review of Biomedical Engineering, Vol 14 14, 351-367, 10.1146/annurev-bioeng-071811-150108 (2012). [DOI] [PubMed]
- 33.Cheng Z, et al. Near-infrared fluorescent deoxyglucose analogue for tumor optical imaging in cell culture and living mice. Bioconjugate chemistry. 2006;17:662–669. doi: 10.1021/bc050345c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nitin N, et al. Molecular imaging of glucose uptake in oral neoplasia following topical application of fluorescently labeled deoxy-glucose. International journal of cancer. 2009;124:2634–2642. doi: 10.1002/ijc.24222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang HF, Maslov K, Stoica G, Wang LHV. Functional photoacoustic microscopy for high-resolution and noninvasive in vivo imaging. Nat Biotechnol. 2006;24:848–851. doi: 10.1038/nbt1220. [DOI] [PubMed] [Google Scholar]
- 36.Vakoc BJ, et al. Three-dimensional microscopy of the tumor microenvironment in vivo using optical frequency domain imaging. Nat Med. 2009;15:1219–U1151. doi: 10.1038/nm.1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hardee ME, Dewhirst MW, Agarwal N, Sorg BS. Novel Imaging Provides New Insights into Mechanisms of Oxygen Transport in Tumors. Curr Mol Med. 2009;9:435–441. doi: 10.2174/156652409788167122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Frees AE, et al. Delivery-corrected imaging of fluorescently-labeled glucose reveals distinct metabolic phenotypes in murine breast cancer. PloS one. 2014;9:e115529. doi: 10.1371/journal.pone.0115529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rajaram N, et al. Delivery rate affects uptake of a fluorescent glucose analog in murine metastatic breast cancer. PloS one. 2013;8:e76524. doi: 10.1371/journal.pone.0076524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sheth RA, Josephson L, Mahmood U. Evaluation and clinically relevant applications of a fluorescent imaging analog to fluorodeoxyglucose positron emission tomography. Journal of biomedical optics. 2009;14:064014. doi: 10.1117/1.3259364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tsytsarev V, et al. In vivo imaging of epileptic activity using 2-NBDG, a fluorescent deoxyglucose analog. J Neurosci Meth. 2012;203:136–140. doi: 10.1016/j.jneumeth.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yao, J. J. et al. Noninvasive Photoacoustic Computed Tomography of Mouse Brain Metabolism In Vivo. Proc Spie8581, 10.1117/12.2005645 (2013). [DOI] [PMC free article] [PubMed]
- 43.Gottlieb E, Vander Heiden MG, Thompson CB. Bcl-x(L) prevents the initial decrease in mitochondrial membrane potential and subsequent reactive oxygen species production during tumor necrosis factor alpha-induced apoptosis. Molecular and cellular biology. 2000;20:5680–5689. doi: 10.1128/MCB.20.15.5680-5689.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Frezza C, et al. Metabolic profiling of hypoxic cells revealed a catabolic signature required for cell survival. PloS one. 2011;6:e24411. doi: 10.1371/journal.pone.0024411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perry, S. W., Norman, J. P., Barbieri, J., Brown, E. B. & Gelbard, H. A. Mitochondrial membrane potential probes and the proton gradient: a practical usage guide. Biotechniques50, 98−+, doi:10.2144/000113610 (2011). [DOI] [PMC free article] [PubMed]
- 46.Xie H, et al. Mitochondrial alterations near amyloid plaques in an Alzheimer’s disease mouse model. The Journal of neuroscience: the official journal of the Society for Neuroscience. 2013;33:17042–17051. doi: 10.1523/JNEUROSCI.1836-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sorg BS, Moeller BJ, Donovan O, Cao Y, Dewhirst MW. Hyperspectral imaging of hemoglobin saturation in tumor microvasculature and tumor hypoxia development. Journal of biomedical optics. 2005;10:44004. doi: 10.1117/1.2003369. [DOI] [PubMed] [Google Scholar]
- 48.Sorg, B. S., Hardee, M. E., Agarwal, N., Moeller, B. J. & Dewhirst, M. W. Spectral imaging facilitates visualization and measurements of unstable and abnormal microvascular oxygen transport in tumors. Journal of biomedical optics 13, 10.1117/1.2837439 (2008). [DOI] [PubMed]
- 49.Palmer, G. M. et al. Quantitative diffuse reflectance and fluorescence spectroscopy: tool to monitor tumor physiology in vivo. Journal of biomedical optics 14, 10.1117/1.3103586 (2009). [DOI] [PMC free article] [PubMed]
- 50.Palmer GM, et al. Optical imaging of tumor hypoxia dynamics. Journal of biomedical optics. 2010;15:066021. doi: 10.1117/1.3523363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brown JQ, et al. Quantitative Optical Spectroscopy: A Robust Tool for Direct Measurement of Breast Cancer Vascular Oxygenation and Total Hemoglobin Content In vivo. Cancer Research. 2009;69:2919–2926. doi: 10.1158/0008-5472.CAN-08-3370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rajaram N, Reesor AF, Mulvey CS, Frees AE, Ramanujam N. Non-invasive, simultaneous quantification of vascular oxygenation and glucose uptake in tissue. PLoS One. 2015;10:e0117132. doi: 10.1371/journal.pone.0117132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Manka D, Spicer Z, Millhorn DE. Bcl-2/adenovirus E1B 19 kDa interacting protein-3 knockdown enables growth of breast cancer metastases in the lung, liver, and bone. Cancer Res. 2005;65:11689–11693. doi: 10.1158/0008-5472.CAN-05-3091. [DOI] [PubMed] [Google Scholar]
- 54.Aslakson CJ, Miller FR. Selective events in the metastatic process defined by analysis of the sequential dissemination of subpopulations of a mouse mammary tumor. Cancer Res. 1992;52:1399–1405. [PubMed] [Google Scholar]
- 55.Zhuang PY, et al. Peritumoral Neuropilin-1 and VEGF receptor-2 expression increases time to recurrence in hepatocellular carcinoma patients undergoing curative hepatectomy. Oncotarget. 2014;5:11121–11132. doi: 10.18632/oncotarget.2553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lindner D. Animal Models and the Tumor Microenvironment: Studies of Tumor-Host Symbiosis. Semin Oncol. 2014;41:146–155. doi: 10.1053/j.seminoncol.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gao MQ, et al. Stromal fibroblasts from the interface zone of human breast carcinomas induce an epithelial-mesenchymal transition-like state in breast cancer cells in vitro. Journal of cell science. 2010;123:3507–3514. doi: 10.1242/jcs.072900. [DOI] [PubMed] [Google Scholar]
- 58.Crowley, L. C., Christensen, M. E. & Waterhouse, N. J. Measuring Mitochondrial Transmembrane Potential by TMRE Staining. Cold Spring Harb Protoc2016, pdbprot087361, 10.1101/pdb.prot087361 (2016). [DOI] [PubMed]
- 59.Scaduto RC, Grotyohann LW. Measurement of mitochondrial membrane potential using fluorescent rhodamine derivatives. Biophys J. 1999;76:469–477. doi: 10.1016/S0006-3495(99)77214-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reif R, et al. In vivo imaging of systemic transport and elimination of xenobiotics and endogenous molecules in mice. Arch Toxicol. 2017;91:1335–1352. doi: 10.1007/s00204-016-1906-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhu, C. G. et al. Near-simultaneous intravital microscopy of glucose uptake and mitochondrial membrane potential, key endpoints that reflect major metabolic axes in cancer. Sci Rep-Uk7, 10.1038/s41598-017-14226-x (2017). [DOI] [PMC free article] [PubMed]
- 62.Pelicano H, Martin DS, Xu RH, Huang P. Glycolysis inhibition for anticancer treatment. Oncogene. 2006;25:4633–4646. doi: 10.1038/sj.onc.1209597. [DOI] [PubMed] [Google Scholar]
- 63.Chen Z, Zhang H, Lu W, Huang P. Role of mitochondria-associated hexokinase II in cancer cell death induced by 3-bromopyruvate. Biochim Biophys Acta. 2009;1787:553–560. doi: 10.1016/j.bbabio.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rudolf R, Mongillo M, Magalhaes PJ, Pozzan T. In vivo monitoring of Ca(2+) uptake into mitochondria of mouse skeletal muscle during contraction. The Journal of cell biology. 2004;166:527–536. doi: 10.1083/jcb.200403102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rajaram, N. et al. Delivery Rate Affects Uptake of a Fluorescent Glucose Analog in Murine Metastatic Breast Cancer. PloS one8, 10.1371/journal.pone.0076524 (2013). [DOI] [PMC free article] [PubMed]
- 66.Rajaram, N., Reesor, A. F., Mulvey, C. S., Frees, A. E. & Ramanujam, N. Non-Invasive, Simultaneous Quantification of Vascular Oxygenation and Glucose Uptake in Tissue. PloS one10, 10.1371/journal.pone.0117132 (2015). [DOI] [PMC free article] [PubMed]
- 67.Heerdt BG, Houston MA, Augenlicht LH. The intrinsic mitochondrial membrane potential of colonic carcinoma cells is linked to the probability of tumor progression. Cancer Res. 2005;65:9861–9867. doi: 10.1158/0008-5472.CAN-05-2444. [DOI] [PubMed] [Google Scholar]
- 68.Houston MA, Augenlicht LH, Heerdt BG. Stable differences in intrinsic mitochondrial membrane potential of tumor cell subpopulations reflect phenotypic heterogeneity. International journal of cell biology. 2011;2011:978583. doi: 10.1155/2011/978583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Viale A, et al. Oncogene ablation-resistant pancreatic cancer cells depend on mitochondrial function. Nature. 2014;514:628–632. doi: 10.1038/nature13611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lu X, Bennet B, Mu E, Rabinowitz J, Kang YB. Metabolomic Changes Accompanying Transformation and Acquisition of Metastatic Potential in a Syngeneic Mouse Mammary Tumor Model. J Biol Chem. 2010;285:9317–9321. doi: 10.1074/jbc.C110.104448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Neveu MA, et al. Multimodality Imaging Identifies Distinct Metabolic Profiles In Vitro and In Vivo. Neoplasia. 2016;18:742–752. doi: 10.1016/j.neo.2016.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wu X, et al. Serum proteomic study on EGFR-TKIs target treatment for patients with NSCLC. OncoTargets and therapy. 2013;6:1481–1491. doi: 10.2147/OTT.S51887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Serganova I, et al. Metabolic imaging: a link between lactate dehydrogenase A, lactate, and tumor phenotype. Clinical cancer research: an official journal of the American Association for Cancer Research. 2011;17:6250–6261. doi: 10.1158/1078-0432.CCR-11-0397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Avgustinova, A. et al. Tumour cell-derived Wnt7a recruits and activates fibroblasts to promote tumour aggressiveness. Nat Commun7, 10.1038/ncomms10305 (2016). [DOI] [PMC free article] [PubMed]
- 75.Takai K, Le A, Weaver VM, Werb Z. Targeting the cancer-associated fibroblasts as a treatment in triple-negative breast cancer. Oncotarget. 2016;7:82889–82901. doi: 10.18632/oncotarget.12658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sotgia F, et al. Mitochondrial metabolism in cancer metastasis Visualizing tumor cell mitochondria and the “reverse Warburg effect” in positive lymph node tissue. Cell Cycle. 2012;11:1445–1454. doi: 10.4161/cc.19841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Witkiewicz AK, et al. Using the “reverse Warburg effect” to identify high-risk breast cancer patients Stromal MCT4 predicts poor clinical outcome in triple-negative breast cancers. Cell Cycle. 2012;11:1108–1117. doi: 10.4161/cc.11.6.19530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bonuccelli G, et al. Ketones and lactate “fuel” tumor growth and metastasis Evidence that epithelial cancer cells use oxidative mitochondrial metabolism. Cell Cycle. 2010;9:3506–3514. doi: 10.4161/cc.9.17.12731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Huang, C. Y., Kuo, W. T., Huang, Y. C., Lee, T. C. & Yu, L. C. H. Resistance to hypoxia-induced necroptosis is conferred by glycolytic pyruvate scavenging of mitochondrial superoxide in colorectal cancer cells. Cell Death & Disease 4, 10.1038/cddis.2013,149 (2013). [DOI] [PMC free article] [PubMed]
- 80.Rikka S, et al. Bnip3 impairs mitochondrial bioenergetics and stimulates mitochondrial turnover. Cell Death Differ. 2011;18:721–731. doi: 10.1038/cdd.2010.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Alhallak K, Rebello LG, Muldoon TJ, Quinn KP, Rajaram N. Optical redox ratio identifies metastatic potential-dependent changes in breast cancer cell metabolism. Biomed. Opt. Express. 2016;7:4364–4374. doi: 10.1364/BOE.7.004364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fan, J. et al. Glutamine-driven oxidative phosphorylation is a major ATP source in transformed mammalian cells in both normoxia and hypoxia. Mol Syst Biol9, 10.1038/Msb.2013.65 (2013). [DOI] [PMC free article] [PubMed]
- 83.Seyfried TN, Flores RE, Poff AM, D’Agostino DP. Cancer as a metabolic disease: implications for novel therapeutics. Carcinogenesis. 2014;35:515–527. doi: 10.1093/carcin/bgt480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lee MS, et al. Angiogenic activity of pyruvic acid in in vivo and in vitro angiogenesis models. Cancer Research. 2001;61:3290–3293. [PubMed] [Google Scholar]
- 85.Mukherjee P, El-Abbadi MM, Kasperzyk JL, Ranes MK, Seyfried TN. Dietary restriction reduces angiogenesis and growth in an orthotopic mouse brain tumour model. Brit J Cancer. 2002;86:1615–1621. doi: 10.1038/sj.bjc.6600298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Masoud GN, Li W. HIF-1 alpha pathway: role, regulation and intervention for cancer therapy. Acta Pharm Sin B. 2015;5:378–389. doi: 10.1016/j.apsb.2015.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Lu HS, Forbes RA, Verma A. Hypoxia-inducible factor 1 activation by aerobic glycolysis implicates the Warburg effect in carcinogenesis. J Biol Chem. 2002;277:23111–23115. doi: 10.1074/jbc.M202487200. [DOI] [PubMed] [Google Scholar]
- 88.De Saedeleer CJ, et al. Lactate activates HIF-1 in oxidative but not in Warburg-phenotype human tumor cells. PloS one. 2012;7:e46571. doi: 10.1371/journal.pone.0046571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Patel BB, et al. Tumor stroma interaction is mediated by monocarboxylate metabolism. Exp Cell Res. 2017;352:20–33. doi: 10.1016/j.yexcr.2017.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lu WQ, Pelicano H, Huang P. Cancer Metabolism: Is Glutamine Sweeter than Glucose? Cancer Cell. 2010;18:199–200. doi: 10.1016/j.ccr.2010.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Carracedo A, Cantley LC, Pandolfi PP. Cancer metabolism: fatty acid oxidation in the limelight. Nat Rev Cancer. 2013;13:227–232. doi: 10.1038/nrc3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Moeller BJ, Cao Y, Li CY, Dewhirst MW. Radiation activates HIF-1 to regulate vascular radiosensitivity in tumors: role of reoxygenation, free radicals, and stress granules. Cancer Cell. 2004;5:429–441. doi: 10.1016/S1535-6108(04)00115-1. [DOI] [PubMed] [Google Scholar]
- 93.Estrella V, et al. Acidity Generated by the Tumor Microenvironment Drives Local Invasion. Cancer Research. 2013;73:1524–1535. doi: 10.1158/0008-5472.CAN-12-2796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Muraoka RS, et al. Blockade of TGF-beta inhibits mammary tumor cell viability, migration, and metastases. J Clin Invest. 2002;109:1551–1559. doi: 10.1172/JCI0215234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dewhirst MW, et al. Arteriolar oxygenation in tumour and subcutaneous arterioles: Effects of inspired air oxygen content. Brit J Cancer. 1996;74:S241–S246. [PMC free article] [PubMed] [Google Scholar]
- 96.Dewhirst MW, et al. Perivascular Oxygen-Tensions in a Transplantable Mammary-Tumor Growing in a Dorsal Flap Window Chamber. Radiat Res. 1992;130:171–182. doi: 10.2307/3578274. [DOI] [PubMed] [Google Scholar]
- 97.Dewhirst MW, et al. Quantification of longitudinal tissue pO2 gradients in window chamber tumours: impact on tumour hypoxia. Br J Cancer. 1999;79:1717–1722. doi: 10.1038/sj.bjc.6690273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Walenta S, et al. Tissue gradients of energy metabolites mirror oxygen tension gradients in a rat mammary carcinoma model. International journal of radiation oncology, biology, physics. 2001;51:840–848. doi: 10.1016/S0360-3016(01)01700-X. [DOI] [PubMed] [Google Scholar]
- 99.Li CY, et al. Initial stages of tumor cell-induced angiogenesis: evaluation via skin window chambers in rodent models. Journal of the National Cancer Institute. 2000;92:143–147. doi: 10.1093/jnci/92.2.143. [DOI] [PubMed] [Google Scholar]
- 100.Morris BA, et al. Collagen Matrix Density Drives the Metabolic Shift in Breast Cancer Cells. Ebiomedicine. 2016;13:146–156. doi: 10.1016/j.ebiom.2016.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Heppner GH, Miller FR, Shekhar PVM. Nontransgenic models of breast cancer. Breast Cancer Research. 2000;2:331–334. doi: 10.1186/bcr77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Johnstone CN, et al. Functional and molecular characterisation of EO771.LMB tumours, a new C57BL/6-mouse-derived model of spontaneously metastatic mammary cancer. Dis Model Mech. 2015;8:237–251. doi: 10.1242/dmm.017830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Palmer GM, et al. In vivo optical molecular imaging and analysis in mice using dorsal window chamber models applied to hypoxia, vasculature and fluorescent reporters. Nat Protoc. 2011;6:1355–1366. doi: 10.1038/nprot.2011.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hu F, Morhard R, Murphy HA, Zhu C, Ramanujam N. Dark field optical imaging reveals vascular changes in an inducible hamster cheek pouch model during carcinogenesis. Biomed Opt Express. 2016;7:3247–3261. doi: 10.1364/BOE.7.003247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Nguyen FT, et al. Intraoperative Evaluation of Breast Tumor Margins with Optical Coherence Tomography. Cancer Research. 2009;69:8790–8796. doi: 10.1158/0008-5472.CAN-08-4340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bargo, P. R. et al. In vivo determination of optical properties of normal and tumor tissue with white light reflectance and an empirical light transport model during endoscopy. Journal of biomedical optics10, 10.1117/1.1921907 (2005). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.