In the latest issue of Nature Immunology, Piccolo et al.1 elegantly explored the effect of coexisting interferon-γ (IFN-γ) and interleukin 4 (IL-4) antagonistic signals on macrophage transcriptional and epigenetic profiles and, interestingly, identified a plastic cross-talk as opposed to mutually exclusive programs between M1 and M2 polarized macrophages. Their results support the fascinating hypothesis that transcriptional and epigenetic reprogramming overcame genetics to drive the evolution of eukaryotic organisms. A rapid reshaping of chromatin acetylation redirected the expression of hundreds of genes under the control of a few transcription factors in response to two coexisting but opposing signals that indicated inflammation and its resolution simultaneously.
We are currently understanding increasingly more about epigenetics in different areas of biology. Epigenetic changes initially allowed adaptation against external perturbations; they then became the basis of a complex organization that led to a flexible, coordinated and context-dependent expression of a multitude of genes that significantly contributed to the evolution of eukaryotic organisms.2 In other scenarios, the epigenome is what distinguishes humans from a nematode such as Caenorhabditis elegans, in which the genome encodes nearly the same number of genes as the human genome but results in 300 neurons instead of 100 billion.3 Social insects such as bees modulate the same genome by nutritional input to have two phenotypically distinct females, queens and workers, by simply altering the epigenome with royal jelly, which globally inhibits DNA methylation.4
Macrophages are crucial guardians of tissue homeostasis and host defense. Although they are the only innate immune cell type established during embryonic development and maintained in adulthood by longevity and local self-renewal, they possess an extraordinary epigenetic plasticity that allows them to acquire different functional properties to best cope with a variety of external stimuli and coordinate an immune response in all primary pathological settings, ranging from inflammatory conditions to infections, or from tumors to degenerative disorders.5 Macrophage plasticity has been explained by the definition of the M1 and M2 programs, driven by interferon-γ (IFN-γ) and interleukin 4 (IL-4), respectively, which indeed represent two extremes of a broad spectrum of activation states.6 In life, macrophages are exposed to multiple microenvironmental signals that do not induce irreversible differentiation programs, indicating that a better understanding of the inter-conversion between macrophage states when microenvironmental conditions change is a key step to taking full advantage of macrophage pleiotropism.
Via a high-throughput RNA-based sequencing approach, Piccolo and colleagues extensively investigated gene expression programs in mouse bone marrow-derived macrophages after conditioning them with IFN-γ and IL-4, which were individually able to induce the phosphorylation of the key transcription factors STAT1 and STAT6. The results demonstrate that only a fraction of the IFN-γ- and IL-4-induced genes, such as the canonical markers of M1 and M2 polarization-inducible nitric oxide synthase (NOS2) and arginase 1, respectively, were largely inhibited by the antagonistic stimulus, while many others were still inducible after co-stimulation. The main finding is the identification of genomic regions with variable sensitivity to the co-stimulation by mapping genome-wide histone acetylation through chromatin immunoprecipitation coupled with next-generation sequencing. Indeed, the authors found that the 773 IL-4-resistant elements activated by IFN-γ were enriched exclusively for consensus motifs recognized by STAT1 and IRF1, while the 736 IFN-γ-inducible genes required auxiliary transcription factors, such as JUNB and C/EBPβ, for activation and were vulnerable to the inhibitory effects of IL-4. On the other hand, only 317 IL-4-related acetylated regions were resistant to cross-inhibition by INF-γ, and the majority contained the canonical E-box recognized by Myc, while the larger IFN-γ-sensitive group showed the enrichment of the STAT6-binding motif. Phosphorylation of both STAT1 and STAT6 occurred normally when IFN-γ and IL-4 antagonistic signals coexisted, but IFN-γ caused a diminished association of STAT6 with chromatin. The antagonistic effect of IL-4 on IFN-γ-induced histone acetylation was not due to a reduction in the association of STAT1 with its genomic targets, resulting in an overall prevalence of IFN-γ signaling over the IL-4 program.
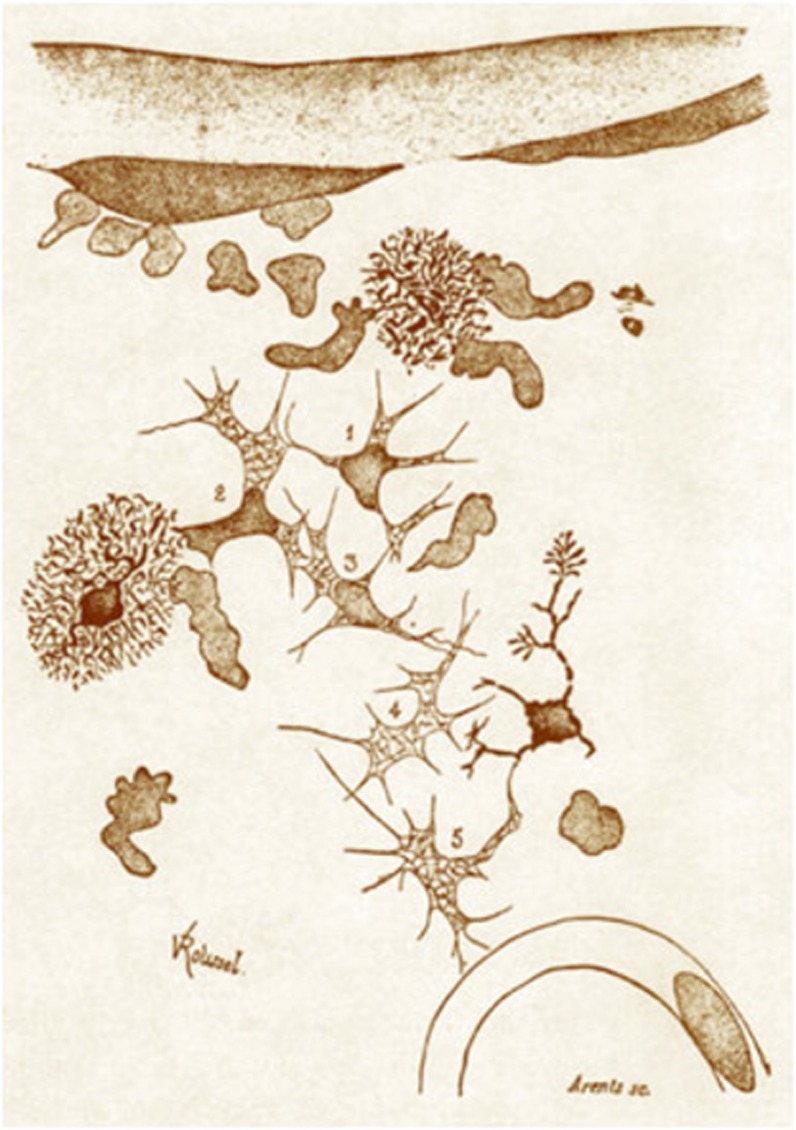
These results suggest that the M1 program is dominant over the M2 program, and M1 inhibits M2 without completely blocking it. Interestingly, the so-called ‘alternative macrophage activation’ is more ancient than the cytotoxic activity of the M1 macrophages, which was first discovered by Elie Metchnikoff in 1882 and is illustrated in Figure 1. Macrophage specialization precedes the development of T and B cells and is based on two ancient mechanisms called ‘the arginine fork in the road’: ornithine and nitric oxide originate from the same amino acid via different enzymatic reactions.8 The former is involved in extracellular matrix formation for organogenesis and subsequent wound healing, while the latter is involved with the primitive function as an endogenous mediator.9 Both processes were under the respective positive and negative control of TGF-β.10 Only in vertebrates did the M1 macrophages acquire the ability to produce a large amount of nitric oxide in response to microbial infection with the synergistic action of LPS and IFN-γ, and M2 macrophages were involved in defense against parasites and allergy under the control of IL-4 and IL-13.9
Figure 1.
The original illustration of a macrophage provided by Elie Metchnikoff who was awarded the Nobel prize in 1908 ‘in recognition of his work on immunity’.7
The power of the IFN-γ-stimulated response is now critical for survival from infection, but the plasticity of macrophages is probably essential to modulate the human response to complex inputs and for the transition from a pro-inflammatory to an anti-inflammatory program during the resolution of inflammation. A fascinating and well-studied example of complex macrophage function is represented by granulomas: a macrophage-driven structure typical of different diseases such as mycobacterial infection, ANCA-associated vasculitis, Crohn’s disease and sarcoidosis, all of which are typically associated with granulomas. M2 plus Th2 are predominant in polyangitis with granulomatosis,11 but in Crohn’s disease and sarcoidosis, a clear M1 plus Th1 profile characterize the granuloma.12, 13 Conversely, different macrophage subsets can be identified under other conditions such as mycobacterial infection. However, rather than a mixed macrophage phenotype as reported in vitro when antagonistic stimuli coexist, distinct differently polarized macrophage subpopulations compete for arginine in succession within a mycobacterial granuloma during the different stages of the disease. In fact, M1 macrophages are prevalent in the intermediate region of a granuloma and in the early stage of the disease, while M2 macrophages are predominant in the peripheral area of a granuloma and in the chronic stage of the disease.14, 15 Nevertheless, we should also note that the in vivo observation does not fully reflect the cell transcriptome and that the M1/M2 discrimination is based only on a limited number of markers. Interestingly, while the role of M1 is not essential to granuloma formation during mycobacterial infection, as shown by the ability of NOS2 knockout mice to form necrotic granulomas,16 M2-like macrophages are thought to have a prominent role. However, IL-4 alone is not able to induce a typical granuloma with multinucleate giant cells,17 while IL-10 depletion results in a mature fibrotic granuloma.18 This evidence suggests the existence of an intricate landscape during infection and immune diseases that involves a complex balance of different cytokines. Although Piccolo’s results warrant translation to a human setting and to specific disease contexts, the data have crucial implications for our understanding of mechanisms of macrophage polarization and potentially for the development of strategies to redirect the immune response toward regulatory pathways during chronic inflammatory conditions. The implication of these observations may reach well beyond conditions such as those that classically manifest with a granuloma. As a paradigm of chronic inflammatory disease, psoriasis and psoriatic arthritis may represent an ideal setting in which modulating macrophage plasticity may lead to therapeutic effects. In skin psoriasis macrophages that share a mixed M1/M2 phenotype are primarily IL-17E (or IL-25)-expressing cells that infiltrate the dermis and can take up a cytokine via endocytosis.19 Remarkably, however, only M2 polarized macrophages express IL-17E receptor in vitro, thus producing inflammatory cytokines.19 Furthermore, it has been recently found that IL-17E can induce M2 macrophage polarization,20 which adds a final piece to the macrophage puzzle.
Footnotes
The authors declare no conflict of interest.
References
- Piccolo V, Curina A, Genua M, Ghisletti S, Simonatto M, Sabo A et al. Opposing macrophage polarization programs show extensive epigenomic and transcriptional cross-talk. Nat Immunol 2017; 18: 530–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maleszka R, Mason PH, Barron AB. Epigenomics and the concept of degeneracy in biological systems. Brief Funct Genom 2014; 13: 191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyko F, Foret S, Kucharski R, Wolf S, Falckenhayn C, Maleszka R. The honey bee epigenomes: differential methylation of brain DNA in queens and workers. PLoS Biol 2010; 8: e1000506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kucharski R, Maleszka J, Foret S, Maleszka R. Nutritional control of reproductive status in honeybees via DNA methylation. Science 2008; 319: 1827–1830. [DOI] [PubMed] [Google Scholar]
- Porta C, Riboldi E, Ippolito A, Sica A. Molecular and epigenetic basis of macrophage polarized activation. Semin Immunol 2015; 27: 237–248. [DOI] [PubMed] [Google Scholar]
- Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity 2014; 41: 14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauber AI. Metchnikoff and the phagocytosis theory. Nat Rev Mol Cell Biol 2003; 4: 897–901. [DOI] [PubMed] [Google Scholar]
- Mills CD. M1 and M2 macrophages: oracles of health and disease. Crit Rev Immunol 2012; 32: 463–488. [DOI] [PubMed] [Google Scholar]
- Dzik JM. Evolutionary roots of arginase expression and regulation. Front Immunol 2014; 5: 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills CD, Kincaid K, Alt JM, Heilman MJ, Hill AM. M-1/M-2 macrophages and the Th1/Th2 paradigm. J Immunol 2000; 164: 6166–6173. [DOI] [PubMed] [Google Scholar]
- de Souza AWS, van Timmeren M, Sanders JS, Stegeman C, Heeringa P, Kallenberg CGM et al. M2 macrophage is the predominant phenotype in airways inflammatory lesions in patients with granulomatosis with polyangiitis. Arthritis Res Ther 2017; 19: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu Y, Yibrehu B, Zabini D, Kuebler WM. Animal models of sarcoidosis. Cell Tissue Res 2017; 367: 651–661. [DOI] [PubMed] [Google Scholar]
- Lissner D, Schumann M, Batra A, Kredel LI, Kuhl AA, Erben U et al. Monocyte and M1 macrophage-induced barrier defect contributes to chronic intestinal inflammation in IBD. Inflamm Bowel Dis 2015; 21: 1297–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattila JT, Ojo OO, Kepka-Lenhart D, Marino S, Kim JH, Eum SY et al. Microenvironments in tuberculous granulomas are delineated by distinct populations of macrophage subsets and expression of nitric oxide synthase and arginase isoforms. J Immunol 2013; 191: 773–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClean CM, Tobin DM. Macrophage form, function, and phenotype in mycobacterial infection: lessons from tuberculosis and other diseases. Pathog Dis 2016; 74 (pii): ftw068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duque-Correa MA, Kuhl AA, Rodriguez PC, Zedler U, Schommer-Leitner S, Rao M et al. Macrophage arginase-1 controls bacterial growth and pathology in hypoxic tuberculosis granulomas. Proc Natl Acad Sci USA 2014; 111: E4024–E4032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helming L, Gordon S. The molecular basis of macrophage fusion. Immunobiology 2007; 212: 785–793. [DOI] [PubMed] [Google Scholar]
- Cyktor JC, Carruthers B, Kominsky RA, Beamer GL, Stromberg P, Turner J. IL-10 inhibits mature fibrotic granuloma formation during Mycobacterium tuberculosis infection. J Immunol 2013; 190: 2778–2790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senra L, Stalder R, Alvarez Martinez D, Chizzolini C, Boehncke WH, Brembilla NC. Keratinocyte-derived IL-17E contributes to inflammation in psoriasis. J Invest Dermatol 2016; 136: 1970–1980. [DOI] [PubMed] [Google Scholar]
- Feng J, Li L, Ou Z, Li Q, Gong B, Zhao Z et al. IL-25 stimulates M2 macrophage polarization and thereby promotes mitochondrial respiratory capacity and lipolysis in adipose tissues against obesity. Cell Mol Immunol 2017; e-pub ahead of print 13 February 2017; doi:10.1038/cmi.2016.71. [DOI] [PMC free article] [PubMed]