Abstract
Background
Reduction of low-density lipoprotein cholesterol (LDL-C) is important for patients with a high risk for atherosclerotic events, such as patients with diabetes and other risk factors. Anagliptin was reported to reduce LDL-C for 12 weeks in phase III trials regardless of the use of statins, but it is uncertain whether this effect is common to other dipeptidylpeptidase-4 (DPP-4) inhibitors.
Methods
A multicenter, randomized, open-label, parallel-group trial was conducted to confirm the superiority of anagliptin to sitagliptin in terms of the primary endpoint of reduction of LDL-C for 52 weeks in patients with type 2 diabetes and atherosclerotic vascular lesions, as well as the non-inferiority of anagliptin to sitagliptin in terms of change in hemoglobin A1c (HbA1c). Patients are randomly assigned to receive anagliptin or sitagliptin at a ratio of 1:1, with those in the anagliptin group receiving anagliptin 100 mg orally twice per day and those in the sitagliptin group receiving sitagliptin 50 mg orally once per day. During the trial period, hypoglycemic agents and anti-dyslipidemia drugs should not be added and neither should their dosages be changed. A total sample size of 300 was estimated to provide a power of 0.8 with a two-sided alpha of 0.05 for LDL-C, considering a 30% dropout rate. Pre-specified factors for subgroup analyses are HbA1c, use of DPP-4 inhibitors, sex, body mass index, LDL-C, age, and the presence of treatment for existing ischemic heart disease.
Discussion
If anagliptin were to be shown to reduce LDL-C in patients with type 2 diabetes and atherosclerotic vascular lesions despite pre-existing statin treatment, more intensive cholesterol management would be appropriate.
Trial Registration
Electronic supplementary material
The online version of this article (10.1007/s10557-018-6776-z) contains supplementary material, which is available to authorized users.
Keywords: DPP-4 inhibitors, Low-density lipoprotein cholesterol, Type 2 diabetic patients, Dyslipidemia, Cardiovascular risk
Background
Diabetes mellitus is one of the strongest risk factors for atherosclerotic diseases [1]. In Europe and the USA, myocardial infarction is the direct cause of death in 40–50% of patients with diabetes, and the number of patients with diabetes that die as a direct result of ischemic heart disease is reportedly increasing [2]. In a Finnish study, the rate of incipient myocardial infarction among patients with diabetes was roughly equal to the rate of recurrent myocardial infarction among non-diabetic patients; furthermore, patients with diabetes and prior myocardial infarction demonstrated a greatly increased incidence of myocardial infarction [3]. Although the application of such results to the Japanese population is not straightforward, existing atherosclerotic vascular lesions and diabetes mellitus are undoubtedly major risk factors for further fatal vascular diseases. Therefore, multifactorial intervention, including control of blood glucose, blood pressure, and lipid levels, is crucial for the prevention of vascular disease [4].
Dipeptidylpeptidase-4 (DPP-4) inhibitors enhance the action of glucagon-like peptide 1 (GLP-1), the most physiologically important incretin, and they consequently show various actions, such as the stimulation of glucose-dependent insulin secretion, inhibition of glucagon secretion, inhibition of gastric emptying, and appetite regulation [5]. DPP-4 inhibitors have become standard drugs to improve hemoglobin A1c (HbA1c) levels in patients with diabetes, though improvement of cardiovascular outcomes by adding DPP-4 inhibitors to usual care in diabetic patients with established cardiovascular diseases has not yet been shown [6–8]. Anagliptin is unique among the DPP-4 inhibitors because it was reported to reduce low-density lipoprotein cholesterol (LDL-C) by 9.5 mg/dL over 12 weeks [9] in phase III trials regardless of the use of statins. This effect of anagliptin may not be a “class effect” of DPP-4 inhibitors, because there has been experimental evidence to suggest that anagliptin inhibits the absorption of cholesterol in the small intestine and cholesterol synthesis in the liver, which presumably are involved in the LDL-C-mediated reduction by anagliptin [10].
This LDL-C-lowering effect of anagliptin is particularly relevant to diabetic patients with high cardiovascular risk, but such patients are likely to be excluded from clinical trials for regulatory approval. The aim of the present study is, therefore, to investigate the comparative effects of anagliptin and sitagliptin, which was most frequently prescribed in Japan, on LDL-C in patients with type 2 diabetes with dyslipidemia and atherosclerotic vascular lesions.
Methods
Trial Design
This is a multicenter, randomized, open-label, parallel-group trial to determine the effectiveness of anagliptin versus sitagliptin on reduction in LDL-C in patients with type 2 diabetes and existing atherosclerotic vascular lesions. Patients with type 2 diabetes and existing atherosclerotic vascular lesions under treatment of statin therapy are included. The eligibility criteria are shown in Table 1.
Table 1.
Patient eligibility criteria
| Inclusion criteria | Patients who fulfilled all of the following criteria were included |
|---|---|
| 1 | High-risk (*) patients with type 2 diabetes who are undergoing diet therapy/exercise therapy or are using other hypoglycemic agents in conjunction with diet therapy/exercise therapy |
| 2 | Patients who have been using statins for ≥8 weeks |
| 3 | Patients with LDL-C ≥ 100 mg/gL in ≥ 1 of their previous three measurements after the use of statins |
| 4 | Patients with HbA1c ≥ 6.0% and < 10.5% (if the investigational drug is added on, HbA1c ≥ 7.0% and < 10.5%) |
| 5 | Patients aged ≥ 20 years at the time of consent |
| 6 | Patients who provide written consent to participate in the trial of their own free will based on a sufficient understanding of the trial following an adequate explanation |
| Exclusion criteria | Patients who met any of the following criteria were excluded |
| 1 | Patients with type 1 diabetes |
| 2 | Patients with TG ≥ 400 mg/dL in a past fasting blood sample |
| 3 | Women who are pregnant, potentially pregnant, or lactating |
| 4 | Patients with severe infections, who are scheduled to undergo/have just undergone surgery, or who have serious trauma |
| 5 | Patients with a serum creatinine level ≥ 2.4 mg/dL for men or ≥ 2.0 mg/dL for women |
| 6 | Patients using GLP-1 receptor agonists |
| 7 | Patients considered ineligible for any other reason by a study investigator |
| * High-risk | Defined as the fulfillment of any one of the following criteria |
| 1 | Stenotic lesions or plaques of ≥ 25% of the arterial diameter in past coronary angiography or CT |
| 2 | Coronary artery calcification in past coronary CT |
| 3 | Past history of acute coronary syndrome |
| 4 | Past history of PCI or CABG |
| 5 | Past history of stroke (ischemic cerebral infarction or cerebral hemorrhage) |
| 6 | Past history of TIA |
| 7 | Past history of peripheral artery disease (including aortic lesions) |
| 8 | Past ankle-brachial index ≤ 0.9 |
| 9 | Presence of carotid artery plaque (including max IMT ≥ 1.1 mm) in past carotid duplex |
CABG: coronary artery bypass surgery; CT: computed tomography; GLP-1: glucagon-like peptide-1; HbA1c: hemoglobin A1c; IMT: intima-media thickness; LDL-C: low-density lipoprotein cholesterol; TG: triglyceride; PCI: percutaneous coronary intervention; TIA: transient ischemic attack
Registration, randomization, and data collection are performed using an electronic data capture (EDC) system. Randomization is performed centrally through the EDC system with a stochastic minimization algorithm to balance treatment assignment within and across hospitals, HbA1c (≥ 8.0%, < 8.0%, use of DPP-4 inhibitors prior to trial registration, sex, body mass index (BMI) (≥ 25 kg/m2, < 25 kg/m2), and LDL-C (≥ 130 mg/dL, < 130 mg/dL).
Trial Oversight
The principal investigator, co-principal investigator, and members of the steering committee designed and conducted this study in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan (Table 2). Protocol and consent forms were approved by the institutional review boards at the University of the Ryukyus (No. 731) and each participating center (Table 3) to which important protocol modification and safety information including serious adverse events in this trial are reported. All patients or their legally authorized representatives provide written, informed consent before randomization with investigators. All centers are regularly monitored by steering committee representatives, and the trial is monitored by an independent data and safety monitoring board (Table 2). Auditing this trial is conducted by the audit department of the University of the Ryukyus independently. This trial was registered at Clinicaltrials.gov (NCT02330406).
Table 2.
Study oversight
| Role of study | Name | Institution |
|---|---|---|
| Principal investigator Steering Committee |
Shinichiro Ueda, MD, PhD | Department of Pharmacology and Therapeutics, University of the Ryukyus |
| Co-principal investigator Steering Committee |
Takeshi Morimoto, MD, PhD, MPH | Department of Clinical Epidemiology, Hyogo College of Medicine |
| Steering Committee | Osamu Arasaki, MD | Department of Cardiology, Tomishiro Central Hospital |
| Steering Committee | Koichi Node, MD, PhD | Department of Cardiovascular Medicine, Saga University |
| Steering Committee | Michio Shimabukuro, MD, PhD | Department of Diabetes, Endocrinology and Metabolism, Fukushima Medical University |
| Steering Committee | Takashi Nomiyama, MD, PhD | Department of Endocrinology and Diabetes Mellitus, Fukuoka university, |
| Event Adjudication Committee | Akihiro Tokushige, MD, PhD | Department of Pharmacology and Therapeutics, University of the Ryukyus |
| Event Adjudication Committee | Masahiro Natsuaki, MD, PhD | Department of Cardiovascular Medicine, Saga University |
| Event Adjudication Committee | Tomohiro Asahi, MD, PhD | Department of Cardiology, Naha City Hospital |
| Data Safety Monitoring Board | Keijiro Saku, MD, PhD | General Medical Research Center, Fukuoka University |
| Data Safety Monitoring Board | Tetsunori Saikawa, MD, PhD | Okubo Hospital |
| Data Safety Monitoring Board | Kohei Kaku, MD, PhD | Department of General Internal Medicine 1, Kawasaki Medical School |
| Study statistician | Mio Sakuma, MD, PhD, MPH | Institute for Clinical Effectiveness |
| Study statistician | Takeshi Morimoto, MD, PhD, MPH | Department of Clinical Epidemiology, Hyogo College of Medicine |
| Study secretariat | – | Department of Pharmacology and Therapeutics, University of the Ryukyus |
| Project management | – | Institute for Clinical Effectiveness |
| Data management | – | Institute for Clinical Effectiveness |
| Study advisor | Hisao Ogawa, MD, PhD | National Cerebral and Cardiovascular Center |
Table 3.
Participating centers and investigators
| Center | Investigators |
|---|---|
| Hokko Memorial Clinic | Ichiro Sakuma, MD, PhD |
| Tomishiro Central Hospital | Osamu Arasaki, MD |
| Sunagawa Medical Clinic | Hiroshi Sunagawa, MD |
| Imari Arita Kyoritsu Hospital | Kazuo Matsunaga, MD, PhD |
| Oohama Daiichi Hospital | Ryu Takahashi, MD, PhD |
| Chibana Clinic | Isao Shiroma, MD |
| Northern Okinawa Cardiovascular Center | Kinya Ashida, MD |
| Baba Memorial Hospital | Hajime Yamashita, MD, PhD |
| JR Hiroshima Hospital | Hiroki Teragawa, MD, PhD |
| Kusatsu General Hospital | Atsuyuki Wada, MD, PhD |
| Shonan Hospital | Ken Nakachi, MD, PhD |
| Fukuoka University Hospital | Takashi Nomiyama, MD, PhD |
| Saiseikai Fukuoka General Hospital | Toru Kubota, MD, PhD |
| Urasoe General Hospital | Hiroki Uehara, MD |
| Naha City Hospital | Tomohiro Asahi, MD, PhD |
| Kokura Memorial Hospital | Takashi Morinaga, MD |
| Tokushima University Hospital | Masataka Sata, MD, PhD |
Trial Intervention
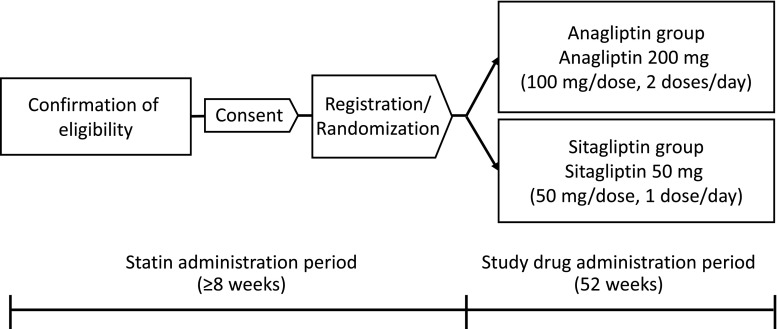
Patients randomly receive anagliptin or sitagliptin at a ratio of 1:1 (Fig. 1). Treatment assignment is not concealed from participants or treating physicians. Patients in the anagliptin group are given anagliptin 100 mg orally twice per day for 52 weeks. If the effects are insufficient, the dose can be increased to 200 mg orally twice per day. Patients in the sitagliptin group are given sitagliptin 50 mg orally once per day for 52 weeks. If the effects are insufficient, the dose can be increased to 100 mg per day. If the patients are using anti-diabetic drugs other than DPP-4 inhibitors at the start of the trial, the study drug is administered concomitantly, and such anti-diabetic drugs are not to be replaced.
Fig. 1.
Study design. After the statin administration period and informed consent is obtained, eligible patients are randomly allocated to the anagliptin group who receive twice a day anagliptin at 200 mg per day and to the sitagliptin group who receive once a day sitagliptin at 50 mg per day for 52 weeks, the study drug treatment period
During the trial period, hypoglycemic agents and anti-dyslipidemia drugs (statins, ezetimibe, anion exchange resins, fibrates, and eicosapentaenoic acid (EPA)) are not to be added, and their dosages are not to be changed. A change in dose of insulin is not considered a change in hypoglycemic agents. Other therapy is determined by the physician in charge.
Changes in the medication use as well as other drugs with possible effects on outcome are prohibited. Our clinical research coordinators regularly monitor participants and their physicians about adherence to the study medication/dose at every visit. If cross-over is found, the patients should be dropped out as per protocol.
Measurements
Through clinical research coordinators or physicians in charge, information on patients is obtained. Clinical characteristics include age, sex, height, waist circumference, body weight, blood pressure, heart rate, past medical history, smoking status, alcohol consumption, drug allergies, and use of concomitant drugs. Blood pressure, heart rate, and compliance with study drug are monitored at 12, 24, 36, and 52 weeks. Height, waist circumference, and body weight were also measured at 52 weeks.
Blood glucose level, red blood cell count, white blood cell count, hemoglobin, hematocrit, platelet count, AST, ALT, γGTP, CK, BUN, and creatinine are measured locally at baseline, 12, 24, 36, and 52 weeks, and LDL-C, HbA1c, total cholesterol (TC), HDL-C, triglycerides (TG), apolipoprotein A1 (Apo-A1), apolipoprotein B (ApoB), apolipoprotein E (ApoE), glycoalbumin, insulin, 1,5-anhydro-D-glucitol (1,5-AG), and C-peptide are measured at the same time periods and analyzed at the core laboratory (SRL Inc., Tokyo, Japan). Small dense LDL, apolipoprotein B48 (ApoB48), high-sensitivity C-reactive protein (hsCRP), interleukin-6 (IL-6), campesterol, sitosterols, lathosterol, and high-molecular-weight adiponectin are measured at baseline and at 52 weeks and analyzed at the same core laboratory. Urine albumin and urine creatinine are also measured at baseline and 52 weeks and analyzed at the same core laboratory. Blood samples are obtained at fasting or at least 4 h after a meal. Follow-up is done at the hospital outpatient clinic or referring clinics.
Other substudies such as changes in the measurement of intima media thickness (IMT), detailed lipoprotein profiling, and fractions of fatty acids are included in the protocol. Substudies that are unplanned at this point should be conducted according to the decision of the Steering Committee. Additional serum samples for this purpose are stored.
Endpoints
The primary endpoint is the change in LDL-C. LDL-C is calculated based on the Friedewald (F) equation. An important secondary endpoint is the change in HbA1c.
Secondary endpoints are changes in the following measurements: fasting blood glucose, fasting insulin, 1,5-AG, C-peptide, TC, TG, HDL-C, non-HDL-C, ApoA1, ApoB, ApoE, ApoB48, small dense LDL, hsCRP, IL-6, campesterol, sitosterols, lathosterol, high-molecular-weight adiponectin, estimated glomerular filtration rate (eGFR), and the urine albumin/creatinine ratio. Secondary endpoints also include progression, lack of change, or remission of microalbuminuria and macroalbuminuria.
Safety outcomes are death and any adverse events systematically reported for 52 weeks, including hypoglycemia, pancreatitis, pancreatic cancer, ileus, and cardiovascular and cerebrovascular events. Safety outcomes are defined in the protocol. Symptoms requiring hospital admission are included, according to the Japanese Ethical Guidelines.
Data Management
The details of data management including data entry, coding, security, and storage, including any related processes to promote data quality, are described in the full protocol and more in the standard operation procedures issued by the data center (Institute of Clinical Effectiveness).
Sample Size and Statistical Analysis
The present trial seeks to confirm that the anagliptin group is significantly superior to the sitagliptin group in terms of the primary endpoint of change in LDL-C after 52 weeks of treatment. Thus, the null hypothesis is that both anagliptin and sitagliptin groups demonstrate equal changes in LDL-C levels, while the alternative hypothesis is that the sitagliptin and anagliptin groups demonstrate different changes in LDL-C.
It was assumed that reductions in LDL-C after 52 weeks would be similar to a previous report that showed that anagliptin provided an LDL-C decrease of 9.5 mg/dL [9], whereas sitagliptin provided a decrease of 0.97 mg/dL [11], with standard deviation (SD) of 21.6 mg/dL for both treatments. With a two-sided alpha of 0.05 and power of 0.8, the sample size was calculated as 102 for each group. Considering a dropout rate of 30%, 300 was set as the total sample size.
This trial was also designed to confirm that the anagliptin group is non-inferior to the sitagliptin group in terms of the important secondary endpoint of the change in HbA1c. The non-inferiority margin of HbA1c was set to 0.3%, which is conventionally used for HbA1c. The null hypothesis is that the 97.5% upper one-sided confidence limit for [change in HbA1c in sitagliptin group − change in HbA1c in anagliptin group] ≥ 0.3, and the alternative hypothesis is that the 97.5% upper one-sided confidence limit for [change in HbA1c in sitagliptin group − change in HbA1c in anagliptin group] < 0.3.
A total sample size of 300 provides a power of 0.8 for HbA1c on the assumption that the SD for HbA1c in the anagliptin group based on a previous clinical trial is 0.91, and the non-inferiority margin is 0.3 with a one-sided alpha of 0.025.
The statistical analysis plan (SAP) will be specified before data analysis. The full analysis set (FAS) includes patients who received allocated treatment and provided assessable outcome data. The safety analysis set (SAS) includes patients who received allocated treatment at least once. The per protocol set (PPS) includes patients who received allocated treatment and for whom planned outcome data as per the protocol are available. The FAS is used for the primary endpoint, and the FAS and PPS are used for the important secondary and other secondary endpoints. The SAS is used for safety outcomes. Categorical variables are expressed as frequencies with percentages, and continuous variables are expressed as means with SDs or medians with interquartile ranges (IQRs). All analyses are conducted under the intention-to-treat principle.
Repeated ANOVA with mixed effect models for repeated measures (MMRM) will be developed to compare the anagliptin and sitagliptin groups in terms of change in LDL-C. In this model, treatment allocation and time are treated as fixed effects and include five variables used in balancing factors at randomization as covariates. The same model without covariates of stratification variables will also be developed for sensitivity analyses. The non-inferiority of the anagliptin group to the sitagliptin group in terms of HbA1c levels will be examined with a non-inferiority margin of 0.3%.
For the changes in other endpoints, a one-sample t test is used for comparisons of the baseline and follow-up values within the group, and two-sample t tests are used for comparisons between groups. The last observation carried forward (LOCF) method is used for missing values.
The number and frequency of categorical safety outcomes will be presented and compared between groups by the chi-squared test or Fisher’s exact test. The means are presented with SDs or medians with IQRs for laboratory parameters, and a one-sample t test is used for comparisons of the baseline and follow-up values within the group, with two-sample t tests used for comparisons between groups. The LOCF method is used for missing values.
Subgroup analyses for the primary and important secondary endpoints will be determined before fixing the SAP. The following pre-specified factors are used for subgroup analyses for the primary and important secondary endpoints: HbA1c (≥ 8.0%, < 8.0%), use of DPP-4 inhibitors prior to trial registration, sex, BMI (≥ 25 kg/m2, < 25 kg/m2), LDL-C (≥ 130 mg/dL, < 130 mg/dL), age (≥ 65 years, < 65 years), and the presence of treatment for existing ischemic heart disease before enrollment (PCI or CABG). The statistical significance of possible treatment effect heterogeneity between subgroups is assessed with interaction terms in repeated ANOVA. Other exploratory analyses are conducted based on the consensus of the Steering Committee. Because of the exploratory nature of these analyses for other than the primary endpoint, no correction for multiplicity is made.
All statistical analyses are performed by a study statistician (Morimoto T) and members of the data center (Institute for Clinical Effectiveness) with the use of JMP 13.1 (SAS Institute Inc., Cary, NC) and SAS 9.4 (SAS Institute Inc., Cary, NC) based on the SAP. All P values are two-sided, and P < 0.05 is considered significant other than for the non-inferiority test for HbA1c, where a one-sided P < 0.025 is considered significant. For baseline data, missing data are not imputed, and data with missing data are analyzed as they are. Because of the short enrollment and follow-up periods and the estimated low risk of adverse events, no interim analyses are planned.
Discussion
This pragmatic, randomized, controlled trial was designed to investigate the comparative effects of two DPP-4 inhibitors, anagliptin and sitagliptin, on plasma levels of LDL-C in type 2 diabetic patients with a high risk for cardiovascular diseases. The lipid-lowering effect of anagliptin was first demonstrated in a phase III trial comparing anagliptin to placebo as a single agent or with concurrent anti-diabetic treatment, such as alpha-glucosidase inhibitors, biguanide, sulfonylurea, or thiazolidine in type 2 diabetic patients for 12 weeks [9]. Anagliptin significantly lowered LDL-C by 5.4 mg/dL and, though it was a before and after comparison, further reduction of LDL-C levels by 9.7 mg/dL compared to those at baseline was observed during the additional observation period extended to 52 weeks. In terms of effects of sitagliptin on lipid metabolism, a similar extended phase III trial showed no significant reduction of LDL-C [11]. Furthermore, a recent meta-analysis including 11 randomized controlled trials showed that sitagliptin alone or in combination with other drugs significantly improved levels of serum TG and HDL-C but had no effects on LDL-C levels with substantial heterogeneities [12]. Although these data suggest that LDL-C-lowering effects of anagliptin seem specific among DPP-4 inhibitors, we should, however, interpret them with great caution because measurement of lipid was not the primary end point in most studies and therefore not well standardized among studies. In addition, there has been no direct comparison between anagliptin and other DPP-4 inhibitors. Possible beneficial effects of anagliptin on lipid metabolism, therefore, should also be demonstrated in a pragmatic trial with a longer observation period that compares it to other DPP-4 inhibitor regarding LDL-C as the primary end point and enrolls more relevant patients, i.e., patients with a high cardiovascular risk with insufficient lipid-lowering despite use of statins. From these points of view, this trial was designed to enroll type 2 diabetic patients with at least one atherosclerotic vascular lesion and LDL-C levels above 100 mg/dL on statin treatment, with an observation period of 52 weeks after randomization. Given that DPP-4 inhibitors are the most frequently prescribed anti-diabetic drugs in Japan, comparing anagliptin to sitagliptin as an active control rather than placebo is more realistic and relevant to clinical practice.
Conclusions
From the points of view discussed above, a pragmatic, unblended, randomized, controlled trial comparing the effects of anagliptin and sitagliptin on plasma LDL-C levels in type 2 diabetic patients with at least one atherosclerotic vascular lesion and insufficient LDL-C lowering despite the use of statins was designed.
Electronic Supplementary Material
(DOCX 30 kb)
Acknowledgments
The authors are indebted to Ms. Makiko Ohtroii, Ms. Ai Sunagawa, Ms. Sachiko Kitamura, Ms. Kaori Yamamoto, Ms. Hirono Saito, and Ms. Saeko Nagano for their data management and Ms. Takako Okumura and for their project management.
Abbreviations
- LDL-C
low-density lipoprotein cholesterol
- HbA1c
hemoglobin A1c
- DPP-4
dipeptidylpeptidase-4
- GLP-1
glucagon-like peptide 1
- EDC system
an electronic data capture system
- BMI
body mass index
- TC
total cholesterol
- HDL-C
high density lipoprotein-cholesterol
- TG
triglycerides
- Apo-A1
apolipoprotein A1
- ApoB
apolipoprotein B
- ApoE
apolipoprotein E
- 1,5-AG
1,5-anhydro-D-glucitol
- ApoB48
apolipoprotein B48
- hsCRP
high-sensitivity C-reactive protein
- IL-6
interleukin-6
- SAP
the statistical analysis plan
- FAS
the full analysis set
- SAS
the safety analysis set
- PPS
the per protocol set
- ANOVA
analysis of variance
- MMRM
mixed effect models for repeated measures
- LOCF
the last observation carried forward
- IMT
intima media thickness
Author Contributions
All authors intellectually contributed to the study protocol development including study design, trial intervention, inclusion and exclusion criteria of patients, and measurement of variables and endpoints. Statistical analysis plan was made by the study statistician.
Funding Information
This study was supported by the Kowa Company, Ltd., and the representative of Kowa participated in the study concept and reviewing the final manuscript, but the study design, operation, data collection, statistical analyses, and drafting of the manuscript were solely conducted by the academic authors.
Compliance with Ethical Standards
Declarations
ᅟ
Ethics Approval and Consent to Participate
Protocol and consent forms were approved by the institutional review boards at the University of the Ryukyus (No. 731) and each participating center. All patients or their legally authorized representatives provided written, informed consent before randomization.
Consent for Publication
Not applicable.
Availability of Data and Material
Not applicable.
Conflict of Interests
Dr. Shinichiro Ueda reports research grants from Bristol-Myers Squibb and Kowa; non-purpose research grants from Bristol-Myers Squibb, Chugai, MSD, Pfizer, and Takeda; lecturer’s fees from Boehringer Ingelheim and MSD. Dr. Michio Shimabukuro reports research grants from AstraZeneca, Ono, and Sanwa Kagaku Kenkyusho; non-purpose research grants from Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Chugai, Eli Lilly, Kowa, Mitsubishi Tanabe, MSD, Novo Nordisk, Ono, Taisho Toyama, and Takeda; lecturer’s fees from Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Chugai, Eli Lilly, Kowa, Mitsubishi Tanabe, Mochida, MSD, Novo Nordisk, Ono, Taisho Toyama, and Takeda; advisory board for Novo Nordisk; sponsored office from Boehringer Ingelheim. Dr. Osamu Arasaki reports lecturer’s fees from Abbott, Astellas, Boehringer Ingelheim, Medtronic, and St. Jude Medical. Dr. Koichi Node reports research grants from Abbott, Actelion, Air Water, Asahi Kasei, Astellas, AstraZeneca, Bayer, Boehringer Ingelheim, Mebix, Mitsubishi Tanabe, Nippon Sigmax, and Teijin; non-purpose research grants from Abbott, Astellas, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Eisai, Eli Lilly, Kissei, Kowa, Kyowa Hakko Kirin, Medtronic, Mitsubishi Tanabe, MSD, Nippon Shinyaku, Novartis, Otsuka, Pfizer, Sanofi, Sanwa Kagaku Kenkyusho, Sumitomo Dainippon, Takeda, and Teijin; lecturer’s fees from Abbott, Actelion, AnGes, Astellas, Astellas Amgen Bio Pharma, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Daiichi Sankyo, Edwards Lifesciences, Eisai, Eli Lilly, Fukuda Denshi, Fukuda Life Tech Kyusyu, Kissei, Kowa, Kyowa Hakko Kirin, Medtronic, Mitsubishi Tanabe, Mochida, MSD, Nippon Kayaku, Nippon Shinyaku, Novartis, Omron, Ono, Otsuka, Pfizer, Roche Diagnostics, Sanofi, Sanwa Kagaku Kenkyusho, Shionogi, Sumitomo Dainippon, Taisho Toyama, Takeda, Teijin, and Toa Eiyo; manuscript fee from Takeda; advisory boards for Astellas, AstraZeneca, Boehringer Ingelheim, Eli Lilly, MSD, Novo Nordisk, Pfizer, Sanofi, Shionogi, and Takeda. Dr. Takashi Nomiyama reports research grants from Eli Lilly, Mitsubishi Tanabe, MSD, and Novartis; lecturer’s fees from Arkray, Astellas, AstraZeneca, Boehringer Ingelheim, Eli Lilly, Johnson & Johnson, Mitsubishi Tanabe, MSD, Novartis, Novo Nordisk, Ono, Sanofi, Sanwa Kagaku Kenkyusho, Sumitomo Dainippon, Taisho Toyama, Takeda, and Terumo. Dr. Takeshi Morimoto reports a research grant from Nexis; lecturer’s fees from AbbVie, AstraZeneca, Daiichi Sankyo, Kyorin, Mitsubishi Tanabe, and Pfizer; manuscript fee from Pfizer; advisory boards for Asahi Kasei, Boston Scientific, and Bristol-Myers Squibb.
Access to Data
The access to the final trial dataset is rigidly restricted to investigators who are authorized by the steering committee and any activity is recorded. There are contractual agreements that limit such access for investigators.
Confidentiality
Confidentiality in the collection of personal information is protected in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects in Japan
Compensation
The compensation to those who suffer death or severe damage requiring hospitalization from trial participation is provided from the clinical trial insurance organized by the trial sponsor (University of the Ryukyus).
Dissemination Policy
Results from this trial are disseminated through publications and conference presentations to participants, healthcare professionals, and the public.
Footnotes
Electronic supplementary material
The online version of this article (10.1007/s10557-018-6776-z) contains supplementary material, which is available to authorized users.
Contributor Information
Shinichiro Ueda, Phone: +81-98-895-1195, Email: blessyou@med.u-ryukyu.ac.jp.
Michio Shimabukuro, Email: mshimabukuro-ur@umin.ac.jp.
Osamu Arasaki, Email: oarasaki@yuuai.or.jp.
Koichi Node, Email: node@cc.saga-u.ac.jp.
Takashi Nomiyama, Email: tnomiyama@fukuoka-u.ac.jp.
Takeshi Morimoto, Email: tm@hyo-med.ac.jp.
References
- 1.Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287(19):2570–2581. doi: 10.1001/jama.287.19.2570. [DOI] [PubMed] [Google Scholar]
- 2.The emerging risk factor collaboration Diabetes mellitus, fasting glucose and risk of cause specific death. N Engl J Med. 2011;364:829–841. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339(4):229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 4.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Pedersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383–393. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 5.Drucker DJ. The biology of incretin hormones. Cell Metab. 2006;3(3):153–165. doi: 10.1016/j.cmet.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369(14):1317–1326. doi: 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 7.White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369(14):1327–1335. doi: 10.1056/NEJMoa1305889. [DOI] [PubMed] [Google Scholar]
- 8.Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, et al. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–242. doi: 10.1056/NEJMoa1501352. [DOI] [PubMed] [Google Scholar]
- 9.Kaku K. Effects of anagliptin on serum lipids in Japanese patients with type 2 diabetes—a pooled analysis of long-term therapy with anagliptin. J Pharmacol Ther. 2012;40:771–784. [Google Scholar]
- 10.Yano W, Inoue N, Ito S, Itou T, Yasumura M, Yoshinaka Y, et al. Mechanism of lipid-lowering action of the dipeptidyl peptidase-4 inhibitor, anagliptin, in low-density lipoprotein receptor-deficient mice. J Diabetes Investig. 2016;(2):155–60. [DOI] [PMC free article] [PubMed]
- 11.The common technical document of sitagliptin 2009 Chapter 2, 301 (in Japanese) http://www.pmda.go.jp/drugs/2009/P200900043/index.html (Accessed on10th of Jan 2018).
- 12.Fan M, Li Y, Zhang S. Effects of sitagliptin on lipid profiles in patients with type 2 diabetes mellitus. A meta-analysis of raaondomized clinical trials. Medicine. 2016;95:e2386. doi: 10.1097/MD.0000000000002386. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 30 kb)