Abstract
A growing body of evidence has clearly demonstrated that maternal nutrition can strongly determine the susceptibility to the development of metabolic diseases in offspring. With the increasing prevalence of maternal overweight, obesity, and gestational diabetes mellitus, it yields enormous burden for individual and public health. Interventions during pregnancy have been proven to be challenging, with limited efficacy and low compliance. Resveratrol, as a natural polyphenolic compound, has a wide-range of beneficial properties, including potent antiobesogenic, antiatherosclerotic, and antidiabetic effects. However, the role of maternal resveratrol intake on metabolic health in offspring has not been extensively investigated. Therefore, the aim of this study was to review the effects of maternal resveratrol supplementation on metabolic health in offspring and its potential mechanisms.
Keywords: cardiometabolic health, offspring, pregnancy, Resveratrol consumption
Introduction
The incidence of obesity and diabetes is increasing rapidly, placing a huge economic burden on society [1]. However, the pathogenesis of diabetes has not been fully illustrated. Emerging data show that perinatal nutrition consumption is a pivotal factor determining the susceptibility to metabolic disorders [2–4]. In particular, approximately one in six births is affected by gestational diabetes mellitus (GDM) reported by International Diabetes Federation Atlas in late 2017 [1]. The World Health Organization newly reported that 50% of women of childbearing ages, and 20–25% of pregnant women in Europe were affected by overweight or obesity [5]. As demonstrated by the “Developmental Origins of Health and Disease (DOHaD)” theory [6,7], obese mothers and women with GDM are associated with infant weight z-scores at birth and at 6 months [8], childhood obesity [9], and unhealthy body composition in adult offspring [10,11]. They are more likely to develop insulin resistance [12], type 2 diabetes [13,14] and even early childhood type 1 diabetes [15], and cardiovascular diseases [16] in adulthood.
Interventions for metabolic health during pregnancy are limited
With the increasing prevalence of metabolic diseases during pregnancy, such as maternal obesity and GDM, it yields enormous burden for individual and public health [17]. Preventing obesity, insulin resistance, and type 2 diabetes during pregnancy has pronounced benefits [18]. Lifestyle interventions, including diet and exercise, have been widely used to prevent and treat abnormal metabolism during pregnancy [19]. However, it has proven to be challenging, with limited efficacy and low compliance. One meta-analysis indicated that diet and lifestyle interventions in pregnancy were able to reduce gestational weight gain; however, no effects on composite maternal and fetal outcomes were observed [20]. Poston et al. [21] showed that a behavioral intervention with diet and physical activity in obese mothers was insufficient to reduce the incidence of fetal macrosomia or to prevent GDM occurrence. Han et al. [22] showed that for women with GDM, there were no differences in adverse pregnancy outcomes among several kinds of dietary advice. Flynn et al. [23] showed that the methodological variability in dietary interventions to control gestational weight gain in pregnant women was large, which limited the ability to apply the evidence in clinical practice and develop clinical guidelines. Other management practices, such as medication therapy for GDM, are expensive and with side effects [24]. Therefore, alternative interventions for metabolic health during pregnancy are needed.
Historical perspective of active compounds isolated from plants and herbs
Traditional Chinese Medicine (TCM), as an herbal medicine with a 2000-year-old history, has been widely used to treat diseases in most Asian countries [25]. The safety, efficacy, and mechanisms of most TCM have been clearly demonstrated, and compounds from dietary plants and herbs have been widely used in complementary and alternative medicine [26]. For example, artemisinin, as an important antimalarial drug, is mainly discovered and isolated from sweet wormwood [27]. In addition, approximately 50% of pharmaceutical drugs may be plant derivatives [28]. Salicylic acid, isolated from the willow tree, is the basis of the common drug, aspirin. Atropine, as a muscle relaxant, is isolated from nightshade plants, and morphine is extracted from the opium poppy [29]. In recent years, active compounds isolated from plants and herbs have been discovered, due to its multiple therapeutic capacities [25,30].
Resveratrol and its roles in human health
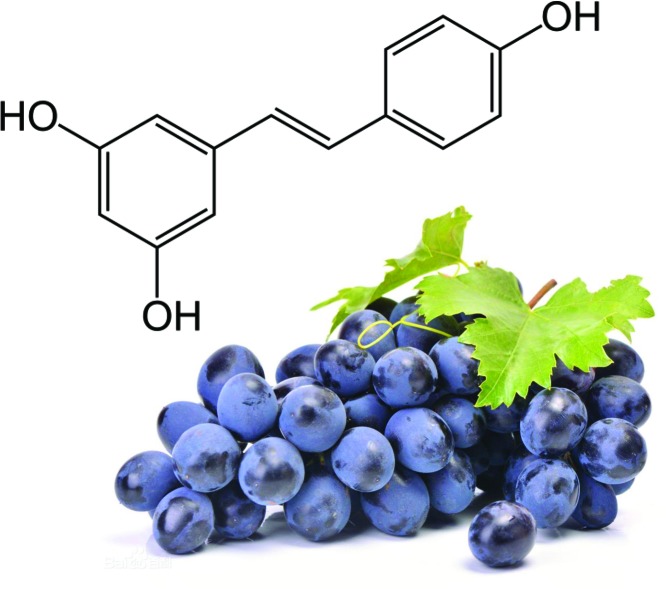
Resveratrol, a polyphenolic compound (3,4′,5-trihydroxystilbene), is mostly isolated from grapes (Figure 1). It also naturally presents in a variety of plant foods such as peanuts and cranberries [31]. It indicates that resveratrol has a variety of beneficial health effects, such as anti-inflammatory [32], antioxidant [33], and anticarcinogenic [34] properties. Resveratrol also can ameliorate metabolic diseases [35], including cardioprotective, antiobesogenic [30], antiatherosclerotic [36], and antidiabetic [37] effects. A systematic analysis of 21 studies found that daily resveratrol consumption (≥300 mg/day) significantly reduced blood pressure, total cholesterol, and plasma glucose in obese subjects, with lower risks of cardiovascular diseases [38]. However, evidence about the effects of maternal resveratrol intake on metabolic health in offspring is limited. Therefore, we aimed to review the effects of maternal resveratrol consumption on metabolic health in offspring and its potential mechanisms underlying these programming effects.
Figure 1. The molecular structure of resveratrol isolated from grapes.
Resveratrol, a polyphenolic compound (3,4′,5-trihydroxystilbene), is mostly present in grapes. Resveratrol has a variety of beneficial health effects and exhibits several biological properties, including its cardioprotective, antiobesogenic, antiatherosclerotic, and antidiabetic effects.
Maternal resveratrol consumption and metabolic health
Evidence from clinical studies in human
The beneficial effects of resveratrol supplementation in humans are widely studied, but the studies about the effects of resveratrol intake during pregnancy on metabolic health in humans are limited. Several studies show that oral resveratrol is well absorbed and rapidly metabolized, without pronounced toxicity [39,40]. One clinical study was conducted to evaluate the metabolic effects of resveratrol in overweight pregnant women. It showed that resveratrol supplement (80 mg) reduced the incidence of GDM and improved the lipid profile and glucose blood level after 60 days [41]. It also showed that both the time and doses of blood pressure control were significantly reduced in preeclampsia patients who received resveratrol supplementation (50 mg each, up to five dosages) [42]. It suggested that maternal resveratrol intake has a beneficial effect in pregnant women. However, the evidence is limited and no information is available about the different effects of resveratrol depending on the dietary intake on pregnant women. Thus, more clinical studies with larger sample size are needed.
Evidence from in vivo and in vitro experiments
Maternal resveratrol consumption and glucose metabolism
Animal experiments showed that maternal resveratrol consumption can improve glucose metabolism in pregnant females, as well as in offspring. Resveratrol supplementation throughout pregnancy was able to decrease maternal body weight, improve glucose tolerance, and increase blood flow volume in uterine artery, with lower triglyceride deposition in liver and decreased placental inflammation in nonhuman primates [43]. Using a genetic mouse model of GDM, it showed that resveratrol intake (10 mg/kg body weight per day) before pregnancy and during pregnancy significantly alleviated hyperglycemia, improved insulin resistance, increased fetal survival, and decreased body weight at birth. They further found that resveratrol enhanced adenosine monophosphate activated protein kinase (AMPK) activation and reduced glucose-6-phosphatase activity in pregnant C57BL/KsJ-Leptin (db/+) mouse, as well as the offspring [44]. Using human samples, Lappas et al. [45] investigated the effects of resveratrol incubation (50, 100, and 200 μmol/l) on insulin resistance and placental inflammation associated with GDM. It showed that resveratrol was able to ameliorate placental inflammation triggered by lipopolysaccharide (LPS), with decreased tumor necrosis factor (TNF), interleukin-6 (IL-6), and interleukin-8 (IL-8) gene expressions in human placentas. Recently, Tran et al. [46] found that treatment with resveratrol (200 μmol/l) significantly reduced the secretion and expression of proinflammatory cytokines, such as IL-6, interleukin-1α (IL-1α), interleukin-1β (IL-1β), IL-8, and monocyte chemoattractantprotein-1 (MCP-1) in human placenta and adipose tissue. It was able to restore the impaired insulin signaling and glucose uptake activity assessed by radio-labeled assay in skeletal muscles obtained from pregnant individuals. Thus, maternal resveratrol intake had a beneficial effect on glucose metabolism in pregnant females and offspring.
Maternal resveratrol consumption and its effects on lipid metabolism
Maternal resveratrol administration (0.2% diet) in pregnant mice increased energy expenditure and insulin sensitivity, which was associated with increased brown adipose activity and the browning of white adipose tissue [47]. Maternal resveratrol consumption (50 mg/l in the drinking water) during pregnancy and lactation reduced body weight, serum leptin level, visceral and subcutaneous adipose tissue weight, with females being more affected in offspring rats, indicating sexually dimorphic impact [48]. Franco et al. [49] also showed that maternal resveratrol intake (30 mg/kg body weight/day) decreased body weight and fat mass in offspring. It was able to reverse hyperleptinemia and improve hypothalamic leptin signaling. Resveratrol administration (100 mg/kg body weight) from embryonic day 3 to 12 prevented the occurrence of oxidative stress and apoptosis in embryos; it further decreased blood cholesterol level by 41.74% and triglyceride level by 60.64% in diabetic dams [50]. Thus, it indicated that maternal resveratrol intake was able to improve lipid metabolism in both dams and offspring.
Maternal resveratrol consumption and its effects on cardiovascular function
Maternal resveratrol supplementation (4 g/kg diet) during pregnancy and lactation alleviated the development of hypertension in adult offspring, with improved nitric oxide bioavailability in spontaneously hypertensive rats [51]. However, Moraloglu et al. [52] found that resveratrol intake (20 mg/kg per day) during the whole pregnancy did not decrease blood pressure, and did not result in a significant response in blood flows and placental pathology parameters in pregnant rats. Resveratrol consumption (4 g/kg diet) improved cardiac recovery from ischemia/reperfusion injury and attenuated superoxide levels in both male and female rat offspring exposed to prenatal hypoxia [53]. This variability in findings could be caused by variations in the different doses of resveratrol intake or the length of study duration. Thus, it suggests that the efficacy of distinct doses is needed to be evaluated and the best dosing should be determined in further studies. The relevant evidence of maternal resveratrol intake and metabolic health in both pregnant females and offspring are summarized in Table 1.
Table 1. Relevant studies about maternal resveratrol intake and metabolic health in offspring.
| Resveratrol consumption | Intervention period | Species | Beneficial effects on pregnant females | Beneficial effects on offspring | Potential mechanism | References |
|---|---|---|---|---|---|---|
| A Western-style diet supplemented with 0.37% resveratrol | Throughout pregnancy | Nonhuman primates | - Resulted in maternal weight loss and improved glucose tolerance | - Fetal pancreatic mass was enlarged by 42% | May be driven by an eNOS-dependent mechanism | Roberts et al. [43] |
| - Increased uterine artery volume blood flow | - A 12-fold increase in proliferation | |||||
| - Decreased placental inflammation and liver triglyceride deposition | ||||||
| Oral gavage with resveratrol (10 mg/kg body weight per day) | Four weeks before pregnancy and during pregnancy | A genetic GDM model: C57BL/KsJ-Leptin (db/+) mouse | - Improved glucose metabolism, insulin tolerance, and reproductive outcome of the pregnant db/+ females | - Increased fetal survival and decreased body weight | - Enhanced AMPK activation | Yao et al. [44] |
| - Reduced production and activity of G6Pase | ||||||
| 50, 100, and 200 μmol/l resveratrol incubation | 6- and/or 24-h incubation | Human placenta | - Quenched inflammation induced by LPS | NA | - SIRT1 possessed anti-inflammatory actions | Lappas et al. [45] |
| 200 μmol/l resveratrol incubation | 20-h incubation | Human placenta, adipose tissue, and skeletal muscle | - Reduced the expression and secretion of pro-inflammatory cytokines IL-6, IL-1α, IL-1β, IL-8, and MCP-1 in human placenta and omental and subcutaneous adipose tissue | NA | - Restored the impaired insulin signaling pathway and insulin-mediated glucose uptake in human skeletal muscle | Tran et al. [46] |
| A high-fat diet with or without 0.2% (w/w) resveratrol | During pregnancy and lactation | C57BL/6 J mice | - Protected dams against body weight gain and fat accumulation | - Increased energy expenditure and insulin sensitivity | - Increased phosphorylated AMPKα levels, Sirt1, PRDM16, and other thermogenic genes protein contents | Zou et al. [47] |
| - Reduced the concentrations of triglycerides and insulin | - Enhanced white adipose tissue browning | |||||
| Resveratrol (50 mg/l) in drinking water | During pregnancy and lactation | Wistar rats | - No difference in body weight at the end of lactation | - Reduced body weight, leptin, VAT and SCAT, with females being more affected | - Decreased fatty acid synthase expression in VAT | Ros et al. [48] |
| - An antiadipogenic effect | ||||||
| Resveratrol (30 mg/kg body weight/day) | 8 weeks before mating and throughout gestation and lactation | Wistar rats | NA | - Decreased body weight, subcutaneous and visceral fat mass, and adiposity | - Increased p-STAT3 content in the hypothalamus | Franco et al. [49] |
| Resveratrol (100 mg/kg body weight) was administered by gavage feeding | 10 days (from day E3 to E12) | Sprague Dawley rats | - Decreased lipid accumulation including cholesterol by 41.74% and triglyceride by 60.64% and increased HDL in diabetic dams | - Prevented both oxidative stress and apoptosis in embryos | - Stimulation of the extrinsic and intrinsic pathway | Singh et al. [50] |
| - May attenuate the expression of HMG-CoA reductase | ||||||
| Resveratrol-supplemented diet (4 g/kg diet) | From gestational day 0.5 until postnatal day 21 | Spontaneously hypertensive rat | - Had no effect on blood flow patterns in the maternal uterine arteries | - Mitigated the development of hypertension in adult offspring | - Improved nitric oxide bioavailability | Care et al. [51] |
| 20 mg/kg per day and twice daily | During the whole pregnancy | Wistar albino rats | - Did not decrease blood pressure | NA | NA | Moraloglu et al. [52] |
| - No changes in blood flows and placental pathology parameters | ||||||
| Resveratrol supplementation (4 g/kg diet) | For 9 weeks following weaning | Sprague–Dawley rats | NA | - Improved cardiac recovery from ischemia/reperfusion injury | - Unclear, without AMPK–ACC signaling activation | Shah et al. [53] |
| - Attenuated superoxide levels |
Abbreviations: ACC, acetyl-CoA carboxylase; AMPK, adenosine monophosphate activated protein kinase; E, embryonic; eNOS, endothelial nitric oxide synthase; G6Pase, glucose-6-phosphatase; GDM:, gestational diabetes mellitus; HDL, high-density lipoprotein; HMG-CoA, hydroxy-3-methyl-glutaryl (HMG)-CoA reductase; IL-1α, interleukin-1α; IL-1β, interleukin-1β; IL-6, interleukin-6; IL-8, interleukin-8; LPS, lipopolysaccharide; MCP-1, monocyte chemoattractantprotein-1; NA, not available; PRDM16, PR domain containing 16; p-STAT3, phosphorylated-signal transducer and activator of transcription 3; SCAT, subcutaneous adipose tissue; SIRT, sirtuin; VAT, visceral adipose tissue.
Possible harmful effects of resveratrol
In addition to the above beneficial effects of resveratrol, detrimental effects of resveratrol should also be considered. Studies that reported possible harmful effects of resveratrol are limited. Roebrts et al. [43] found that, in stark contrast with the other seemingly beneficial effects to the placenta and developing fetus, a dramatic increase in fetal pancreatic mass and exocrine proliferation, independent of an increase in islet mass, following maternal resveratrol supplementation in nonhuman primates which is clinically concerning. Klink et al. [54] showed that resveratrol was associated with significantly worse survival with LAPC-4 (the human CaP cell line) tumors and caution should be advised in using resveratrol for patients. Further studies about other possible harmful effects of resveratrol should be conducted.
Potential mechanisms of maternal resveratrol consumption and metabolic health in offspring
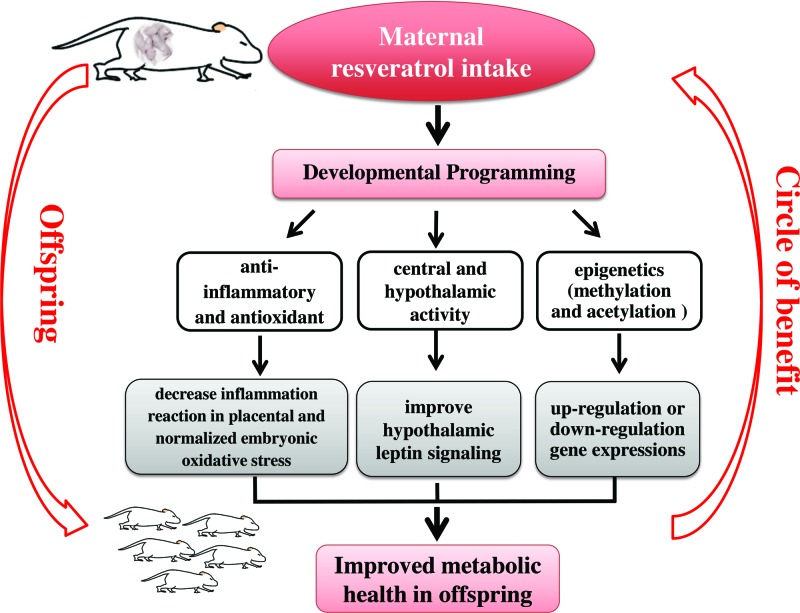
Taken together, the above studies suggest that maternal resveratrol intake protects against hyperglycemia, insulin resistance, dyslipidemia, and cardiac function in pregnant females, as well as their offspring. However, the molecular mechanisms are not clearly elaborated. It is speculated that “developmental programming” may be the underlying mechanism that can elucidate maternal nutrition and metabolic health in offspring [55]. Several potential points can explain the beneficial effects of maternal resveratrol consumption on offspring, which are summarized in Figure 2. First, resveratrol can decrease inflammation reaction in placental and normalize embryonic oxidative stress level [43], due to its anti-inflammatory [32], antioxidant [33] properties. Second, it can reverse hyperleptinemia and improve hypothalamic leptin signaling in offspring [49]. Another possible mechanism is epigenetic modification [56]. Our previous studies showed that epigenetics can link early life nutrition and cardiometabolic health in later life [57–60]. It demonstrated that resveratrol was able to modulate histone H3 on lysine 9 (H3K9) methylation and acetylation in the zygotic pronuclei [61]. Gestational resveratrol exposure induced breast cancer-1 (BRCA-1) promoter hypermethylation and reduced BRCA-1 expression in mammary tissue of rat offspring [62]. However, whether the role of maternal resveratrol consumption on the offspring is due to adaptive responses to improved glucose and lipid metabolism in mothers, or is the direct result of resveratrol transfer through the placenta or the mother’s milk is still unclear. There have been no reports, however, on whether resveratrol crosses the placental barrier. One study showed that as a polyphenol, administration of resveratrol has vasodilator effect on isolated human umbilical vein in vitro [63]. Jang et al. [64] showed that resveratrol is beneficial against diabetes-induced embryonic malformation, we therefore might cautiously assume that it does cross the placental barrier. Thus, further studies focusing on this point and the molecular mechanisms in depth are warranted.
Figure 2. Maternal resveratrol consumption and its beneficial effects on metabolic health in offspring.
It is speculated that “Developmental Programming” is the underlying mechanism because it can link maternal nutrition and metabolic health in offspring. Several potential points could explain the beneficial effects of maternal resveratrol consumption on offspring. First, resveratrol can decrease inflammation reaction in placental and normalized embryonic oxidative stress level, due to its anti-inflammatory and antioxidant properties. Second, it was able to improve hypothalamic leptin signaling in offspring with central nervous system regulation. Another possible mechanism is epigenetic modification, including methylation and acetylation, thus regulate gene expressions.
Conclusions
In summary, pregnancy period is the critical time window of offspring/embryo growth and development. Perinatal nutrition consumption can determine the susceptibility of developing metabolic diseases in adulthood. Interventions during pregnancy are challenging, with limited efficacy and low compliance. Our review suggests that maternal resveratrol consumption during pregnancy has beneficial effects on metabolic health in both pregnant females and offspring. More importantly, the safe and easy implementation of resveratrol consumption has been widely accepted. A broad understanding of the role of resveratrol supplementation during pregnancy can provide critical hints for the early prevention and treatment of metabolic diseases during pregnancy, and thus ensure a healthier future for the mothers and offspring.
Abbreviations
- AMPK
adenosine monophosphate activated protein kinase
- BRCA-1
breast cancer-1
- GDM
gestational diabetes mellitus
- IL
interleukin
- LPS
lipopolysaccharide
- MCP-1
monocyte chemoattractantprotein-1
- TCM
Traditional Chinese Medicine
- TNF
tumor necrosis factor
Author Contribution
S.Z. and Q.Y.F. collected data, synthesized data, and wrote the manuscript. J.C. and J.Z. reviewed and edited the manuscript. J.Z. contributed to the design of this review.
Funding
This study was sponsored by Beijing Municipal Natural Science Foundation (No. 7184252), the Fund for Fostering Young Scholars of Peking University Health Science Center (No. BMU2017PY008), China Scholarship Council of the Ministry of Education (No. 201506210378), and Postgraduate Student Innovation Fund in Peking Union Medical College (No. 2013-1002-33). The funders had no role in study design, data collection and analysis, or preparation of the manuscript.
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
References
- 1. International Diabetes Federation. (2017) IDF diabetes atlas, 8th edn www.diabetesatlas.org.
- 2.Pinhas-Hamiel O. and Zeitler P. (2005) The global spread of type 2 diabetes mellitus in children and adolescents. J. Pediatr. 146, 693–700 10.1016/j.jpeds.2004.12.042 [DOI] [PubMed] [Google Scholar]
- 3.Rando O.J. and Simmons R.A. (2015) I’m eating for two: parental dietary effects on offspring metabolism. Cell 161, 93–105 10.1016/j.cell.2015.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel N., Pasupathy D. and Poston L. (2015) Determining the consequences of maternal obesity for offspring health. Exp. Physiol. 100, 1421–1428 10.1113/EP085132 [DOI] [PubMed] [Google Scholar]
- 5.Organization, W.H. (2016) Obesity and overweight, http://www.who.int/gho/ncd/risk_factors/overweight/en/ [Google Scholar]
- 6.Wallack L. and Thornburg K. (2016) Developmental origins, epigenetics, and equity: moving upstream. Matern. Child Health J. 20, 935–940 10.1007/s10995-016-1970-8 [DOI] [PubMed] [Google Scholar]
- 7.Baird J., Jacob C., Barker M., Fall C.H., Hanson M., Harvey N.C. et al. (2017) Developmental origins of health and disease: A lifecourse approach to the prevention of non-communicable diseases. Healthcare 5, 1–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Patel N., Hellmuth C., Uhl O., Godfrey K., Briley A., Welsh P. et al. (2017) Cord metabolic profiles in obese pregnant women; insights into offspring growth and body composition. J. Clin. Endocrinol. Metab., 103, 346–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hillier T.A., Pedula K.L., Schmidt M.M., Mullen J.A., Charles M.A. and Pettitt D.J. (2007) Childhood obesity and metabolic imprinting: The ongoing effects of maternal hyperglycemia. Diabetes Care 30, 2287–2292 10.2337/dc06-2361 [DOI] [PubMed] [Google Scholar]
- 10.Kaseva N., Vaarasmaki M., Matinolli H.M., Sipola-Leppanen M., Tikanmaki M., Heinonen K. et al. (2017) Pre-pregnancy overweight or obesity and gestational diabetes as predictors of body composition in offspring twenty years later-evidence from two birth cohort studies. Int. J. Obesit 10.1038/ijo.2017.277, [DOI] [PubMed] [Google Scholar]
- 11.Kubo A., Ferrara A., Windham G.C., Greenspan L.C., Deardorff J., Hiatt R.A. et al. (2014) Maternal hyperglycemia during pregnancy predicts adiposity of the offspring. Diabetes Care 37, 2996–3002 10.2337/dc14-1438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bozkurt L., Gobl C.S., Rami-Merhar B., Winhofer Y., Baumgartner-Parzer S., Schober E. et al. (2016) The cross-link between adipokines, insulin resistance and obesity in offspring of diabetic pregnancies. Hormone Res. Paediatrics 86, 300–308 10.1159/000448076 [DOI] [PubMed] [Google Scholar]
- 13.American Diabetes Association (2018) Management of diabetes in pregnancy: standards of medical care in diabetes-2018. Diabetes Care 41, S137–S143 10.2337/dc18-S013 [DOI] [PubMed] [Google Scholar]
- 14.Dabelea D., Hanson R.L., Lindsay R.S., Pettitt D.J., Imperatore G., Gabir M.M. et al. (2000) Intrauterine exposure to diabetes conveys risks for type 2 diabetes and obesity: a study of discordant sibships. Diabetes 49, 2208–2211 10.2337/diabetes.49.12.2208 [DOI] [PubMed] [Google Scholar]
- 15.Lindell N., Carlsson A., Josefsson A. and Samuelsson U. (2018) Maternal obesity as a risk factor for early childhood type 1 diabetes: a nationwide, prospective, population-based case-control study. Diabetologia 61, 130–137 10.1007/s00125-017-4481-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Di Bernardo S., Mivelaz Y., Epure A.M., Vial Y., Simeoni U., Bovet P. et al. (2017) Assessing the consequences of gestational diabetes mellitus on offspring’s cardiovascular health: Mysweetheart cohort study protocol, switzerland. BMJ Open 7, e016972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevens G.A., Singh G.M., Lu Y., Danaei G., Lin J.K., Finucane M.M. et al. (2012) National, regional, and global trends in adult overweight and obesity prevalences. Population Health Metrics 10, 22 10.1186/1478-7954-10-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ohno M.S., Sparks T.N., Cheng Y.W. and Caughey A.B. (2011) Treating mild gestational diabetes mellitus: A cost-effectiveness analysis. Am. J. Obstet. Gynecol. 205, 282.e281–287.e281 10.1016/j.ajog.2011.06.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chuang C.H., Weisman C.S., Hillemeier M.M., Schwarz E.B., Camacho F.T. and Dyer A.M. (2010) Pregnancy intention and health behaviors: Results from the central pennsylvania women’s health study cohort. Matern. Child Health J. 14, 501–510 10.1007/s10995-009-0453-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rogozinska E., Marlin N., Jackson L., Rayanagoudar G., Ruifrok A.E., Dodds J. et al. (2017) Effects of antenatal diet and physical activity on maternal and fetal outcomes: individual patient data meta-analysis and health economic evaluation. Health Technol. Assess. 21, 1–158 10.3310/hta21410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poston L., Bell R., Croker H., Flynn A.C., Godfrey K.M., Goff L. et al. (2015) Effect of a behavioural intervention in obese pregnant women (the upbeat study): a multicentre, randomised controlled trial. Lancet Diabetes Endocrinol. 3, 767–777 10.1016/S2213-8587(15)00227-2 [DOI] [PubMed] [Google Scholar]
- 22.Han S., Middleton P., Shepherd E., Van Ryswyk E. and Crowther C.A. (2017) Different types of dietary advice for women with gestational diabetes mellitus. Cochrane Database Syst. Rev. 2, Cd009275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Flynn A.C., Dalrymple K., Barr S., Poston L., Goff L.M., Rogozinska E. et al. (2016) Dietary interventions in overweight and obese pregnant women: a systematic review of the content, delivery, and outcomes of randomized controlled trials. Nutr. Rev. 74, 312–328 10.1093/nutrit/nuw005 [DOI] [PubMed] [Google Scholar]
- 24.Barrett H.L., Dekker Nitert M., Conwell L.S. and Callaway L.K. (2014) Probiotics for preventing gestational diabetes. Cochrane Database Syst. Rev. 2 Cd009951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hao P.P., Jiang F., Chen Y.G., Yang J., Zhang K., Zhang M.X. et al. (2015) Traditional chinese medication for cardiovascular disease. Nat. Rev. Cardiol. 12, 115–122 10.1038/nrcardio.2014.177 [DOI] [PubMed] [Google Scholar]
- 26.Hao P., Jiang F., Cheng J., Ma L., Zhang Y. and Zhao Y. (2017) Traditional chinese medicine for cardiovascular disease: Evidence and potential mechanisms. J. Am. Coll. Cardiol. 69, 2952–2966 10.1016/j.jacc.2017.04.041 [DOI] [PubMed] [Google Scholar]
- 27.Kong L.Y. and Tan R.X. (2015) Artemisinin, a miracle of traditional chinese medicine. Nat. Prod. Rep. 32, 1617–1621 10.1039/C5NP00133A [DOI] [PubMed] [Google Scholar]
- 28.Koehn F.E. and Carter G.T. (2005) The evolving role of natural products in drug discovery. Nat. Rev. Drug Discovery 4, 206–220 10.1038/nrd1657 [DOI] [PubMed] [Google Scholar]
- 29.Fabricant D.S. and Farnsworth N.R. (2001) The value of plants used in traditional medicine for drug discovery. Environ. Health Perspect. 109, 69–75 10.1289/ehp.01109s169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Martel J., Ojcius D.M., Chang C.J., Lin C.S., Lu C.C., Ko Y.F. et al. (2017) Anti-obesogenic and antidiabetic effects of plants and mushrooms. Nat. Rev. Endocrinology 13, 149–160 10.1038/nrendo.2016.142 [DOI] [PubMed] [Google Scholar]
- 31.Nabavi S.F., Li H., Daglia M. and Nabavi S.M (2014) Resveratrol and stroke: from chemistry to medicine. Curr. Neurovasc. Res. 11, 390–397 10.2174/1567202611666140912114833 [DOI] [PubMed] [Google Scholar]
- 32.Oliveira A.L.B., Monteiro V.V.S., Navegantes-Lima K.C., Reis J.F., Gomes R.S., Rodrigues D.V.S. et al. (2017) Resveratrol role in autoimmune disease-a mini-review. Nutrients 9, 1–22, 10.3390/nu9121306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Truong V.L., Jun M. and Jeong W.S. (2017) Role of resveratrol in regulation of cellular defense systems against oxidative stress. Biofactors, 44, 36–49 [DOI] [PubMed] [Google Scholar]
- 34.Farzaei M.H., Bahramsoltani R. and Rahimi R. (2016) Phytochemicals as adjunctive with conventional anticancer therapies. Curr. Pharm. Des. 22, 4201–4218 10.2174/1381612822666160601100823 [DOI] [PubMed] [Google Scholar]
- 35.Park S.J., Ahmad F., Philp A., Baar K., Williams T., Luo H. et al. (2012) Resveratrol ameliorates aging-related metabolic phenotypes by inhibiting camp phosphodiesterases. Cell 148, 421–433 10.1016/j.cell.2012.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fan E., Zhang L., Jiang S. and Bai Y. (2008) Beneficial effects of resveratrol on atherosclerosis. J. Med. Food 11, 610–614 10.1089/jmf.2007.0091 [DOI] [PubMed] [Google Scholar]
- 37.Zhu X., Wu C., Qiu S., Yuan X. and Li L. (2017) Effects of resveratrol on glucose control and insulin sensitivity in subjects with type 2 diabetes: Systematic review and meta-analysis. Nutr. Metab. 14, 60 10.1186/s12986-017-0217-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang H., Chen G., Liao D., Zhu Y., Pu R. and Xue X. (2016) The effects of resveratrol intervention on risk markers of cardiovascular health in overweight and obese subjects: A pooled analysis of randomized controlled trials. Obesity Rev. 17, 1329–1340 10.1111/obr.12458 [DOI] [PubMed] [Google Scholar]
- 39.Cottart C.H., Nivet-Antoine V., Laguillier-Morizot C. and Beaudeux J.L. (2010) Resveratrol bioavailability and toxicity in humans. Mol. Nutr. Food Res. 54, 7–16 10.1002/mnfr.200900437 [DOI] [PubMed] [Google Scholar]
- 40.Singh C.K., Kumar A., Lavoie H.A., Dipette D.J. and Singh U.S. (2013) Diabetic complications in pregnancy: is resveratrol a solution? Exp. Biol. Med. 238, 482–490 10.1177/1535370212473704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Malvasi A., Kosmas I., Mynbaev O.A., Sparic R., Gustapane S., Guido M. et al. (2017) Can trans resveratrol plus d-chiro-inositol and myo-inositol improve maternal metabolic profile in overweight pregnant patients? Clin. Ther. 168, e240–e247 [DOI] [PubMed] [Google Scholar]
- 42.Ding J., Kang Y., Fan Y. and Chen Q. (2017) Efficacy of resveratrol to supplement oral nifedipine treatment in pregnancy-induced preeclampsia. Endocr. Connect. 6, 595–600 10.1530/EC-17-0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roberts V.H., Pound L.D., Thorn S.R., Gillingham M.B., Thornburg K.L., Friedman J.E. et al. (2014) Beneficial and cautionary outcomes of resveratrol supplementation in pregnant nonhuman primates. FASEB J. 28, 2466–2477 10.1096/fj.13-245472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yao L., Wan J., Li H., Ding J., Wang Y., Wang X. et al. (2015) Resveratrol relieves gestational diabetes mellitus in mice through activating ampk. Reprod. Biol. Endocrinol. 13, 118 10.1186/s12958-015-0114-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lappas M., Mitton A., Lim R., Barker G., Riley C. and Permezel M. (2011) Sirt1 is a novel regulator of key pathways of human labor. Biol. Reprod. 84, 167–178 10.1095/biolreprod.110.086983 [DOI] [PubMed] [Google Scholar]
- 46.Tran H.T., Liong S., Lim R., Barker G. and Lappas M. (2017) Resveratrol ameliorates the chemical and microbial induction of inflammation and insulin resistance in human placenta, adipose tissue and skeletal muscle. PLoS One 12, e0173373 10.1371/journal.pone.0173373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zou T., Chen D., Yang Q., Wang B., Zhu M.J., Nathanielsz P.W. et al. (2017) Resveratrol supplementation of high-fat diet-fed pregnant mice promotes brown and beige adipocyte development and prevents obesity in male offspring. J. Physiol. 595, 1547–1562 10.1113/JP273478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ros P., Diaz F., Freire-Regatillo A., Argente-Arizon P., Barrios V., Argente J. et al. (2017) Resveratrol intake during pregnancy and lactation modulates the early metabolic effects of maternal nutrition differently in male and female offspring. Endocrinology, 59, 810–825, 10.1210/en.2017-00610, [DOI] [PubMed] [Google Scholar]
- 49.Franco J.G., Dias-Rocha C.P., Fernandes T.P., Albuquerque Maia L., Lisboa P.C., Moura E.G. et al. (2016) Resveratrol treatment rescues hyperleptinemia and improves hypothalamic leptin signaling programmed by maternal high-fat diet in rats. Eur. J. Nutr. 55, 601–610 10.1007/s00394-015-0880-7 [DOI] [PubMed] [Google Scholar]
- 50.Singh C.K., Kumar A., Hitchcock D.B., Fan D., Goodwin R., LaVoie H.A. et al. (2011) Resveratrol prevents embryonic oxidative stress and apoptosis associated with diabetic embryopathy and improves glucose and lipid profile of diabetic dam. Mol. Nutr. Food Res. 55, 1186–1196 10.1002/mnfr.201000457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Care A.S., Sung M.M., Panahi S., Gragasin F.S., Dyck J.R., Davidge S.T. et al. (2016) Perinatal resveratrol supplementation to spontaneously hypertensive rat dams mitigates the development of hypertension in adult offspring. Hypertension 67, 1038–1044 10.1161/HYPERTENSIONAHA.115.06793 [DOI] [PubMed] [Google Scholar]
- 52.Moraloglu O., Engin-Ustun Y., Tonguc E., Var T., Tapisiz O.L., Ergun H. et al. (2012) The effect of resveratrol on blood pressure in a rat model of preeclampsia. J. Matern. Fetal Neonatal Med. 25, 845–848 10.3109/14767058.2011.599081 [DOI] [PubMed] [Google Scholar]
- 53.Shah A., Reyes L.M., Morton J.S., Fung D., Schneider J. and Davidge S.T. (2016) Effect of resveratrol on metabolic and cardiovascular function in male and female adult offspring exposed to prenatal hypoxia and a high-fat diet. J. Physiol. 594, 1465–1482 10.1113/JP271133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Klink J.C., Tewari A.K., Masko E.M., Antonelli J., Febbo P.G., Cohen P. et al. (2013) Resveratrol worsens survival in scid mice with prostate cancer xenografts in a cell-line specific manner, through paradoxical effects on oncogenic pathways. Prostate 73, 754–762 10.1002/pros.22619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Costa-Silva J.H., Simoes-Alves A.C. and Fernandes M.P. (2016) Developmental origins of cardiometabolic diseases: Role of the maternal diet. Front. Physiol. 7, 504 10.3389/fphys.2016.00504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Estampador A.C. and Franks P.W. (2014) Genetic and epigenetic catalysts in early-life programming of adult cardiometabolic disorders. Diabetes Metab. Syndr. Obes. 7, 575–586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zheng J., Xiao X., Zhang Q. and Yu M. (2014) DNA methylation: the pivotal interaction between early-life nutrition and glucose metabolism in later life. Br. J. Nutr. 112, 1850–1857 10.1017/S0007114514002827 [DOI] [PubMed] [Google Scholar]
- 58.Zheng J., Xiao X., Zhang Q., Wang T., Yu M. and Xu J. (2017) Maternal low-protein diet modulates glucose metabolism and hepatic micrornas expression in the early life of offspring dagger. Nutrients 9, 1–14, 10.3390/nu9030205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zheng J., Zhang Q., Mul J.D., Yu M., Xu J., Qi C. et al. (2016) Maternal high-calorie diet is associated with altered hepatic microrna expression and impaired metabolic health in offspring at weaning age. Endocrine 54, 70–80 10.1007/s12020-016-0959-9 [DOI] [PubMed] [Google Scholar]
- 60.Xiao X. and Zheng J. (2014) Micrornas: Crucial modulators of fetal epigenetic programming in nutrition and glucose metabolism. Chin. Med. J. 127, 3521–3523 [PubMed] [Google Scholar]
- 61.Adamkova K., Yi Y.J., Petr J., Zalmanova T., Hoskova K., Jelinkova P. et al. (2017) Sirt1-dependent modulation of methylation and acetylation of histone h3 on lysine 9 (h3k9) in the zygotic pronuclei improves porcine embryo development. J. Anim. Sci. Biotechnol. 8, 83 10.1186/s40104-017-0214-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Papoutsis A.J., Selmin O.I., Borg J.L. and Romagnolo D.F. (2015) Gestational exposure to the ahr agonist 2,3,7,8-tetrachlorodibenzo-p-dioxin induces brca-1 promoter hypermethylation and reduces brca-1 expression in mammary tissue of rat offspring: Preventive effects of resveratrol. Mol. Carcinog. 54, 261–269 10.1002/mc.22095 [DOI] [PubMed] [Google Scholar]
- 63.Protic D., Beleslin-Cokic B., Spremovic-Radenovic S., Radunovic N., Heinle H., Scepanovic R. et al. (2014) The different effects of resveratrol and naringenin on isolated human umbilical vein: The role of atp-sensitive k(+) channels. Phytother. Res. 28, 1412–1418 10.1002/ptr.5145 [DOI] [PubMed] [Google Scholar]
- 64.Jang J.Y., Park D., Shin S., Jeon J.H., Choi B.I., Joo S.S. et al. (2008) Antiteratogenic effect of resveratrol in mice exposed in utero to 2,3,7,8-tetrachlorodibenzo-p-dioxin. Eur. J. Pharmacol. 591, 280–283 10.1016/j.ejphar.2008.05.033 [DOI] [PubMed] [Google Scholar]