Abstract
Cardiac troponins are specific biomarkers of cardiac injury. However, the prognostic usefulness of cardiac troponin in patients with acute ischemic stroke is still controversial. The objective of this meta-analysis was to investigate the association of cardiac troponin elevation with all-cause mortality in patients with acute ischemic stroke. PubMed and Embase databases were searched for relevant studies up to April 31, 2017. All observational studies reporting an association of baseline cardiac troponin-T (cTnT) or troponin-I (cTnI) elevation with all-cause mortality risk in patients with acute ischemic stroke were included. Pooled adjusted risk ratio (RR) and corresponding 95% confidence interval (CI) were obtained using a random effect model. Twelve studies involving 7905 acute ischemic stroke patients met our inclusion criteria. From the overall pooled analysis, patients with elevated cardiac troponin were significantly associated with increased risk of all-cause mortality (RR: 2.53; 95% CI: 1.83–3.50). The prognostic value of cardiac troponin elevation on all-cause mortality risk was stronger (RR: 3.54; 95% CI: 2.09–5.98) during in-hospital stay. Further stratified analysis showed elevated cTnT (RR: 2.36; 95% CI: 1.47–3.77) and cTnI (RR: 2.79; 95% CI: 1.68–4.64) level conferred the similar prognostic value of all-cause mortality. Acute ischemic stroke patients with elevated cTnT or cTnI at baseline independently predicted an increased risk of all-cause mortality. Determination of cardiac troponin on admission may aid in the early death risk stratification in these patients.
Keywords: acute ischemic stroke, all-cause mortality, cardiac troponin, meta-analysis
Introduction
Acute ischemic stroke is caused by permanent brain injury secondary to disruption of blood flow [1]. Approximately 68% of strokes are classified into ischemic stroke [2]. From 2000 to 2010, age-specific acute ischemic stroke hospitalization rates increased for individuals aged 25–64 years in the United States [3]. Ischemic stroke remains the leading cause of disability and second cause of deaths throughout the world [4].Cardiac complications account for the leading cause of mortality in these patients [5]. Therefore, determining the prognosis after acute ischemic stroke is an unmet need.
Cardiac troponin-T (cTnT) and cardiac troponin-I (cTnI) are biochemical markers of cardiac injury [6]. An increase in the serum level of cTnT or cTnI is common in the acute phase of ischemic stroke [7], indicating a close relationship between stroke and cardiac damage. It should be noted that increase in cardiac troponin in acute stroke may be explained by comorbidities in some cases [8]. However, inconsistent results [8–21] have been yielded on the association of elevated cardiac troponin level with all-cause mortality risk in patients with acute ischemic stroke. Moreover, the strength of risk estimates varied significantly across studies. Previously published systematic review [22] did not establish the conclusion that troponin elevation was an independent prognostic factor in acute ischemic stroke patients. So far, prognostic value of cardiac troponin elevation in stroke patients remains conflicting.
The purpose of this meta-analysis was to evaluate the association of baseline cTnT or cTnI elevation with all-cause mortality risk in patients with acute ischemic stroke based on available observational studies.
Materials and methods
Data source and literature search
We conducted this meta-analysis according to the reporting checklist of the Meta-analysis of Observational Studies in Epidemiology [23]. To identify relevant studies, an electronic literature search was conducted in PubMed and Embase databases from their inception to April 2017. The terms searched were a combination of the following keywords: ‘troponin’ AND ‘stroke’ OR ‘cerebrovascular accident’ AND ‘mortality’ OR ‘death’. Included studies were restricted in an English publication. In addition, we also manually searched the bibliographies of all the relevant articles to identify additional studies.
Study selection
Studies included in this meta-analysis should satisfy the following inclusion criteria: (i) participants: patients with acute ischemic stroke; (ii) study design: prospective or retrospective observational studies; (iii) exposure: at least one determination of serum level of cTnT or cTnI on admission; (iv) outcome measure: follow-up all-cause mortality or in-hospital death; and (v) provided multivariate-adjusted risk estimate of all-cause or in-hospital mortality associated with the elevated serum cardiac troponin category. Studies were excluded if: (i) participants included hemorrhagic stroke patients; (ii) not providing mortality outcomes based on troponin values; and (iii) reported unadjusted risk estimate.
Data extraction and quality assessment
From each of the eligible studies, two authors independently extracted the following data: surname of the first author, publication year, region of study performed, study design, sample size, proportion of men, mean age or age range, type of cardiac troponin, cut-off value of cardiac troponin, percentage of abnormal cardiac troponin, follow-up time, number of deaths, maximum adjusted risk estimate, and adjustment for covariates. Any discrepancies between two authors were resolved in the presence of a third reviewer. To perform quality assessment, a maximal 9-star Newcastle–Ottawa Scale (NOS) of cohort studies [24] was applied to assess the methodological quality of each study. According to the NOS score, study awarding 7 or over stars was considered good quality.
Statistical analysis
Meta-analyses were carried out with STATA (version 12.0, Stata, College Station, TX, U.S.A.). Summary risk ratio (RR) with 95% confidence interval (CI) was pooled for patients with elevated serum cardiac troponin compared with undetectable cardiac troponin category. Statistical heterogeneity between studies was evaluated by the I2 statistic and Cochran’s Q test. The I2 > 50% or P<0.10 for Cochran’s Q test was regarded as presence of statistical heterogeneity. In presence of significant heterogeneity, a random effect model was used; otherwise, we selected a fixed-effect model. Subgroup analyses were performed by the type of cardiac troponin measured (cTnT or cTnI), assay of troponin (conventional or high-sensitivity), study design (prospective or retrospective), length of follow-up (in-hospital or follow-up), whether excluded coronary heart disease (CHD)/acute myocardial infarction (AMI) patients (yes or no), whether adjustment for renal dysfunction (yes or no), and NOS (≥7 stars compared with <7 stars). Publication bias was explored by the Egger’s linear regression test [25]. Sensitivity analyses were conducted by excluding any one study at each time to observe the influence of a single study on the pooled summary.
Results
Search results and study characteristics
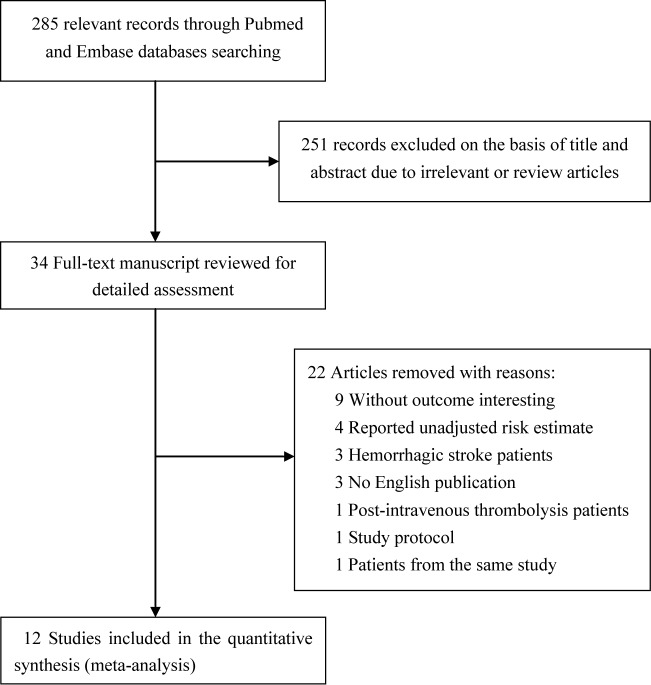
Figure 1 shows the flow diagram for the study selection process. Briefly, a total of 285 records were obtained from the initial electronic search. After screening titles and abstracts, 251 articles were excluded because they were obviously irrelevant or review articles. Two articles [8,26] conducted by Faiz et al. selected the same participants; however, they reported the in-hospital death and follow-up mortality, respectively. After thorough evaluation of the full-text manuscript, 12 studies [8,10–16,18–21] were finally included in this meta-analysis. Table 1 summarizes the baseline clinical and demographic characteristics of the included studies. A total of 7905 acute ischemic stroke patients were included. The sample size of the selected studies ranged from 106 to 1718. Seven studies [10–12,14–16,20] were prospective, whereas five [8,13,18,19,21] were retrospective in nature. Eight studies [8,10–16] were conducted in Europe, two [19,20] in the United States, and two [18,21] in Asia. The percentage of patients with detectable cardiac troponin varied from 10 to 60%. Studied duration ranged from in-hospital stay to 4.4 years. Using the NOS scale, the selected studies were classified into moderate to good quality (Table 3).
Figure 1. Flow diagram of the study selection process.
Table 1. Summary of characteristics of the included studies.
| Author (year) | Region | Study design | Patients (% men) | Age (years) | cTn type/cut-off values | Abnormal cTn (%) | Event number OR/HR (95% CI) | Follow-up duration | Maximum adjusted covariates |
|---|---|---|---|---|---|---|---|---|---|
| Di Angelantonio et al. (2005) [10] | Italy | Prospective study | 330 (51.5) | 57.6 ± 12.9 | cTnI; 0.1 ng/ml | 16.3% | Total deaths: 65; 2.28 (1.42–3.67)* | 144 months | Age and baseline NIHSS score |
| Jensen et al. (2007) [11] | Denmark | Prospective study | 244 (52.5) | 68.7 ± 13.1 | cTnT; 0.03 μg/l | 10% | Total deaths: 36; 3.39 (1.34–8.60) | 19 months | Age, Scandinavian Stroke Scale score, and heart and/or renal failure |
| Jensen et al. (2012) [12] | Denmark | Prospective study | 193 (56.5) | 69.4 ± 12.1 | Hs–cTnT; 14 ng/l | 33.7% | Total deaths: 43; 1.32 (0.62–2.81) | 4.4 years | Age, C-reactive protein, NT-proBNP, prior heart and/or renal failure, and stroke severity |
| Scheitz et al. (2012) [13] | Germany | Retrospective study | 715 (49.8) | 66–84 | cTnT; 0.03 μg/l | 14% | In-hospital deaths: 26; 4.51 (1.93–10.57) | — | Age and stroke severity |
| Hajdinjak et al. (2012) [14] | Slovenia | Prospective cohort study | 106 (58.5) | 70.0 ± 12.1 | cTnT; 0.04 μg/l | 15.1% | In-hospital deaths: 23; 1.8 (1.1–8.4) | — | Age, SBP, DBP, NIHSS score, NT-proBNP, and blood glucose |
| Scheitz et al. (2014) [15] | Germany | Prospective study | 1016 (49.1) | 61–88 | Hs–cTnT; 14 ng/l | 60% | In-hospital deaths: 36; 1.81 (0.80–4.10) | — | Age, gender, prestroke independence, NIHSS score, AF, congestive heart failure, and insular cortex involvement |
| Faiz et al. (2014) [8] | Norway | Retrospective study | 287 (55.1) | 65–83 | Hs–cTnT; 14 ng/l | 54.4% | In-hospital deaths: 17 1.15 (0.17–4.22); total deaths: 88∧; 1.65 (1.04–2.63) | 1.5 years | Age, gender, NIHSS, CHD, cerebrovascular disease, AF, smoking, hypertension, DM, and eGFR |
| Lasek-Bal et al. (2014) [16] | Poland | Prospective study | 1068 (57.0) | 72 ± 11 | Hs–cTnI; 0.014 ng/ml | 9.7% | Total deaths:142 3.05 (1.65–5.65) | 1 month | Age, NIHSS, hypertension, DM, lipid, AF, and CHD |
| Maoz et al. (2015) [18] | Israel | Retrospective study | 212 (56.1) | 73.9 ± 12.9 | Hs–cTnT; 0.03 μg/l | 16.5% | In-hospital deaths: 23; 22.57 (4.4–116.6) | — | Age, ischemic heart disease, creatinine, creatinine clearance, and NIHSS score |
| Peddada et al. (2016) [19] | U.S.A. | Retrospective study | 1145 (55.1) | 65 ± 15 | Hs–cTnI; 0.12 ng/ml | 17.0% | In-hospital deaths: 129; 4.28 (2.40–7.63) | — | Age, gender, smoking, AF, heart failure, hemiplegia, dysphagia, hemorrhagic complication, respiratory failure, renal dysfunction, creatinine, use of oral antiplatelet ot systemic anticoagulation therapy |
| Batal et al. (2016) [20] | U.S.A. | Prospective study | 1718 (50) | 67 ± 15 | cTnI; 0.10 μg/l | 18% | Total deaths: 413; 1.44 (1.10–1.89) | 1.4 years | Age, comorbid factors, stroke etiology, admission SBP, NIHSS score, and creatinine |
| Su et al. (2016) [21] | Taiwan | Retrospective study | 871 (NP) | 72.3 ± 13.6 | cTnI; 0.01 μg/l | 16.8% | In-hospital deaths: 31 5.59 (2.36–13.27) | — | Gender, evidence of clinical deterioration, and NIHSS score |
Abbreviations: AF, atrial fibrillation; BMI, body mass index; CK, creatine kinase; COPD, chronic obstructive pulmonary disease; DBP, diastolic blood pressure; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; HR, hazard ratio; Hs, high-sensitivity; NP, not provided; NIHSS, National Institutes of Health Stroke Scale; SBP, systolic blood pressure. *Combined from each category of troponin I. †Data from Faiz et al. (2014) [26].
Table 3. Subgroup analyses on all-cause mortality.
| Subgroup | Number of studies | Pooled RR | 95% CI | Heterogeneity between studies |
|---|---|---|---|---|
| Study design | ||||
| Prospective | 7 | 1.92 | 1.46–2.53 | P=0.186; I2 = 31.7% |
| Retrospective | 5 | 3.75 | 1.97–7.17 | P=0.186; I2 = 31.7% |
| Region | ||||
| European | 8 | 2.16 | 1.68–2.77 | P=0.354; I2= 9.7% |
| Non-European | 4 | 4.33 | 1.63–11.45 | P<0.001; I2 = 88.5% |
| Type of troponin | ||||
| cTnT | 7 | 2.36 | 1.47–3.77 | P=0.031; I2= 54.7%; |
| cTnI | 5 | 2.79 | 1.68–4.64 | P=0.001; I2= 79.7% |
| Assay of troponin | ||||
| Conventional | 6 | 2.13 | 1.41–3.20 | P=0.027; I2 = 60.3%; |
| High-sensitivity | 6 | 3.00 | 1.83–4.92 | P=0.010; I2 = 64.2% |
| Excluded CHD/AMI patients | ||||
| Yes | 7 | 2.74 | 1.96–3.84 | P=0.061; I2 = 48.0% |
| No | 5 | 2.31 | 1.21–4.41 | P=0.009; I2 = 70.2% |
| Adjusted renal function | ||||
| Yes | 7 | 2.25 | 1.43–3.53 | P=0.002; I2 = 69.9% |
| No | 5 | 2.95 | 2.05–4.25 | P=0.236; I2 = 27.8% |
| NOS | ||||
| ≥7 stars | 6 | 2.45 | 1.55–3.89 | P=0.005; I2 = 70.5% |
| <7 stars | 6 | 3.00 | 1.73–5.21 | P=0.050; I2= 54.8% |
All-cause mortality
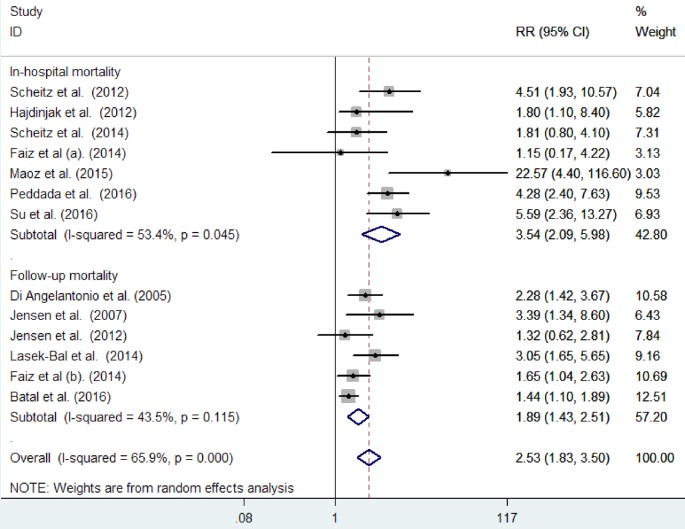
All included studies reported the effect of cardiac troponin elevation on the risk of all-cause mortality in-hospital stay [8,13–15,18,19,21] and at the end of follow-up duration [10–12,16,20]. As shown in Figure 2, significant heterogeneity was detected (I2 = 65.9%; P<0.001) across the studies. Meta-analysis using a random effect model showed that acute ischemic stroke patients with elevated cardiac troponin level significantly increased risk of all-cause mortality (RR: 2.53; 95% CI: 1.83–3.50). Further, pooled RR was 3.54 (95% CI: 2.09–5.98) and 1.89 (95% CI: 1.43–2.51) for in-hospital mortality and follow-up mortality, respectively. Sensitivity analysis by removing a single study by turns indicated that there was no obvious impact of any individual study on the pooled risk estimate (data not shown).
Figure 2. Forest plots showing the association of baseline cardiac troponin elevation with all-cause mortality in patients with acute ischemic stroke.
Subgroup analyses and publication bias
Subgroup analyses suggested that patients with acute ischemic stroke had a higher risk of all-cause mortality in the subgroup of retrospective study, non-European, use of high-sensitivity troponin assays, unadjusted renal function, included CHD, and NOS scores <7 stars (Table 2). Possible publication bias was observed in the overall analysis of all-cause mortality (P=0.046 for the Egger’s test). However, no publication bias was detected according to the results of Egger’s test, P=0.993 in-hospital mortality and P=0.156 in follow-up mortality.
Table 2. Quality assessment of studies included in meta-analysis.
| Study (year) | Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome was not present at the start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Enough follow-up periods (≥1 year) | Adequacy of follow-up of cohorts | Overall NOS |
|---|---|---|---|---|---|---|---|---|---|
| Di Angelantonio et al. (2005) [10] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 8 |
| Jensen et al. (2007) [11] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Jensen et al. (2012) [12] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Scheitz et al. (2012) [13] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Hajdinjak et al. (2012) [14] | ★ | ★ | ★ | ★ | ★ | ★ | 6 | ||
| Scheitz et al. 2014 [15] | ★ | ★ | ★ | ★ | ★ | ★ | 6 | ||
| Faiz et al. (2014) [8] | ★ | ★ | ★ | ★ | ★ | ★ | 6 | ||
| Lasek-Bal et al. (2014) [16] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Maoz et al. (2015) [18] | ★ | ★ | ★ | ★ | ★ | ★ | 6 | ||
| Peddada et al. (2016) [19] | ★ | ★ | ★ | ★ | ★ | ★ | 6 | ||
| Batal et al. (2016) [20] | ★ | ★ | ★ | ★ | ★ | ★ | ★ | 7 | |
| Su et al. (2016) [21] | ★ | ★ | ★ | ★ | ★ | ★ | 6 |
★ denotes a result that satisfies the requirement of the column label.
Discussion
A total of 12 eligible studies with total 7905 acute ischemic stroke patients were identified and analyzed in this meta-analysis. Overall, these selected studies had a moderate-to-good methodological quality. The principal finding of this meta-analysis suggested that acute ischemic stroke patients with cTnT or cTnI elevation were associated with an increased risk for all-cause mortality. Acute ischemic stroke patients with cardiac troponin elevation had a 2.54-times and 89% higher risk of in-hospital deaths and follow-up all-cause mortality, respectively.
The etiology of troponin elevation in acute stroke is not fully understood [27]. Cardiac troponin elevation in the context of acute stroke is associated with the presence of chronic conditions, such as congestive heart failure, impaired renal function [8,13]. Other causes of detectable cardiac troponin include: chronic obstructive pulmonary disease, pulmonary embolism, sepsis, chronic renal failure, and atrial fibrillation [28]. Silent myocardial infarction could have contributed to the poor prognosis of these patients. However, the effects of cardiac troponin elevation on all-cause mortality risk were still statistically significant in pooled studies excluding patients with AMI or pre-existing CHD. Also, elevated cardiac troponin significantly predicted the risk of all-cause mortality despite adjustment for the presence of renal dysfunction. These findings revealed that the prognostic value of abnormal cardiac troponin on mortality was independent of AMI and renal dysfunction. Therefore, troponin elevation in these patients did not seem to be solely a consequence of AMI or renal dysfunction.
Subgroup analysis showed a slight discrepancy in prognostic value between cTnT or cTnI assays. Likewise, similarly prognostic value of cTnI and cTnT has been well established in acute coronary syndrome [29]. In addition, a stronger all-cause mortality risk was found in the subgroup of the retrospective study, in-hospital stay, non-European, and use of high-sensitivity troponin assays. The stronger effect in-hospital mortality may be partly explained by the coincidence of AMI [30].
Increase in troponin was associated with higher mortality in all types of stroke [12,31]. Initial cTnT elevation was a strong predictor of poor outcomes during the acute phase and long-term follow-up [32], even in the absence of acute coronary syndrome [33]. Cardiac troponin elevation also predicted the mortality in patients with intracerebral hemorrhage [34–36]. In spontaneous subarachnoid hemorrhage patients, a well-designed meta-analysis [37] has summarized that cardiac troponin elevation was associated with an increased risk of delayed cerebral ischemia and death.
One possible explanation of troponin elevation in acute ischemic stroke patients may be the coincidence of acute coronary syndrome, triggering a rise in circulating troponin level [38]. Cardiac vulnerability to cerebrogenic stress can be an alternate explanation interpretation of troponin elevation [39,40]. Activation of the sympathoadrenal system may be an important contributor to myocardial damage in acute ischemic stroke patients [41].
This meta-analysis is of clinical relevance to determine the prognostic value of cTnT or cTnI in acute ischemic stroke patients. Given the frequency of abnormal troponin level in the period of acute ischemic stroke patients, routinely determine the level of cardiac troponin in these patients may help identify patients who faced higher risk of post-stroke death. In cases with cardiac troponin increase, one should identify comorbidities associated with cardiac troponin elevation.
Several shortcomings in this meta-analysis should be noted. First, single troponin measurement at baseline may have led to misclassification of patients in each category. Repeated measurements over time can provide more accurate information on the myocardial injury in patients with acute ischemic stroke. Second, lack of adjustment for residual confounding variables may have overestimated the risk estimate of the association between cardiac troponin elevation and mortality. Third, there was a substantial heterogeneity in polling risk summary, mainly due to differences in troponin assays or cut-off values, follow-up duration, and study design. Fourth, potential publication bias could not be excluded because the included studies were limited to English language publications. Finally, the prognostic value of elevated troponin level may be different in various stages or subtypes of ischemic stroke; therefore, the current findings could not generalize all stroke patients.
In conclusion, acute ischemic stroke patients with an elevated baseline cTnT or cTnI level were independently associated with an increased risk of all-cause mortality. Determination of cardiac troponin level should be considered for risk stratification in acute ischemic stroke patients. However, we could not recommend routine troponin measurement on all ischemic stroke patients due to the methodological flaws of the included studies. Further prospective studies are needed to address the prognosis in patients with acute ischemic stroke and concurrent elevated cardiac troponin.
Abbreviations
- AMI
acute myocardial infarction
- CHD
coronary heart disease
- CI
confidence interval
- cTnI
cardiac troponin-I
- cTnT
cardiac troponin-T
- NOS
Newcastle–Ottawa Scale
- RR
risk ratio
Competing interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
This work was supported by the Jiangsu Provincial Key D Special Fund [grant number BE2015666].
Author contribution
Y.C. designed the study, interpreted the results, and finally approved the manuscript. Y.F. and M.J. searched the literature, extracted data, and made the statistical analysis. D.G. and C.M. assessed the study quality. Y.F. drafted the manuscript.
References
- 1.Bevers M.B. and Kimberly W.T. (2017) Critical care management of acute ischemic stroke. Curr. Treat. Opt. Cardiovasc. Med. 19, 41 10.1007/s11936-017-0542-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Krishnamurthi R.V., Feigin V.L., Forouzanfar M.H., Mensah G.A., Connor M., Bennett D.A. et al. (2013) Global and regional burden of first-ever ischaemic and haemorrhagic stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet 1, e259–281 10.1016/S2214-109X(13)70089-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramirez L., Kim-Tenser M.A., Sanossian N., Cen S., Wen G., He S. et al. (2016) Trends in acute ischemic stroke hospitalizations in the United States. J. Am. Heart Assoc. 5, 10.1161/JAHA.116.004026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murray C.J. and Lopez A.D. (2013) Measuring the global burden of disease. N. Engl. J. Med. 369, 448–457 10.1056/NEJMra1201534 [DOI] [PubMed] [Google Scholar]
- 5.Touze E., Varenne O., Chatellier G., Peyrard S., Rothwell P.M. and Mas J.L. (2005) Risk of myocardial infarction and vascular death after transient ischemic attack and ischemic stroke: a systematic review and meta-analysis. Stroke 36, 2748–2755 10.1161/01.STR.0000190118.02275.33 [DOI] [PubMed] [Google Scholar]
- 6.Thygesen K., Alpert J.S., White H.D., Jaffe A.S., Apple F.S. and (2007) Universal definition of myocardial infarction. Circulation 116, 2634–2653 10.1161/CIRCULATIONAHA.107.187397 [DOI] [PubMed] [Google Scholar]
- 7.Eggers K.M. and Lindahl B. (2017) Application of cardiac troponin in cardiovascular diseases other than acute coronary syndrome. Clin. Chem. 63, 223–235 10.1373/clinchem.2016.261495 [DOI] [PubMed] [Google Scholar]
- 8.Faiz K.W., Thommessen B., Einvik G., Brekke P.H., Omland T. and Ronning O.M. (2014) Determinants of high sensitivity cardiac troponin T elevation in acute ischemic stroke. BMC Neurol. 14, 96 10.1186/1471-2377-14-96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James P., Ellis C.J., Whitlock R.M., McNeil A.R., Henley J. and Anderson N.E. (2000) Relation between troponin T concentration and mortality in patients presenting with an acute stroke: observational study. BMJ 320, 1502–1504 10.1136/bmj.320.7248.1502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Angelantonio E., Fiorelli M., Toni D., Sacchetti M.L., Lorenzano S., Falcou A. et al. (2005) Prognostic significance of admission levels of troponin I in patients with acute ischaemic stroke. J. Neurol. Neurosurg. Psychiatry 76, 76–81 10.1136/jnnp.2004.041491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jensen J.K., Kristensen S.R., Bak S., Atar D., Hoilund-Carlsen P.F. and Mickley H. (2007) Frequency and significance of troponin T elevation in acute ischemic stroke. Am. J. Cardiol. 99, 108–112 10.1016/j.amjcard.2006.07.071 [DOI] [PubMed] [Google Scholar]
- 12.Jensen J.K., Ueland T., Aukrust P., Antonsen L., Kristensen S.R., Januzzi J.L. et al. (2012) Highly sensitive troponin T in patients with acute ischemic stroke. Eur. Neurol. 68, 287–293 10.1159/000341340 [DOI] [PubMed] [Google Scholar]
- 13.Scheitz J.F., Endres M., Mochmann H.C., Audebert H.J. and Nolte C.H. (2012) Frequency, determinants and outcome of elevated troponin in acute ischemic stroke patients. Int. J. Cardiol. 157, 239–242 10.1016/j.ijcard.2012.01.055 [DOI] [PubMed] [Google Scholar]
- 14.Hajdinjak E., Klemen P. and Grmec S. (2012) Prognostic value of a single prehospital measurement of N-terminal pro-brain natriuretic peptide and troponin T after acute ischaemic stroke. J. Int. Med. Res. 40, 768–776 10.1177/147323001204000243 [DOI] [PubMed] [Google Scholar]
- 15.Scheitz J.F., Mochmann H.C., Erdur H., Tutuncu S., Haeusler K.G., Grittner U. et al. (2014) Prognostic relevance of cardiac troponin T levels and their dynamic changes measured with a high-sensitivity assay in acute ischaemic stroke: analyses from the TRELAS cohort. Int. J. Cardiol. 177, 886–893 10.1016/j.ijcard.2014.10.036 [DOI] [PubMed] [Google Scholar]
- 16.Lasek-Bal A., Kowalewska-Twardela T., Gasior Z., Warsz-Wianecka A., Haberka M., Puz P. et al. (2014) The significance of troponin elevation for the clinical course and outcome of first-ever ischaemic stroke. Cerebrovasc. Dis. 38, 212–218 10.1159/000365839 [DOI] [PubMed] [Google Scholar]
- 17.Liu X., Chen X., Wang H. and Pan S. (2014) Prognostic significance of admission levels of cardiac indicators in patients with acute ischaemic stroke: prospective observational study. J. Int. Med. Res. 42, 1301–1310 10.1177/0300060514549217 [DOI] [PubMed] [Google Scholar]
- 18.Maoz A., Rosenberg S. and Leker R.R. (2015) Increased high-sensitivity troponin-T levels are associated with mortality after ischemic stroke. J. Mol. Neurosci. 57, 160–165 10.1007/s12031-015-0593-7 [DOI] [PubMed] [Google Scholar]
- 19.Peddada K., Cruz-Flores S., Goldstein L.B., Feen E., Kennedy K.F., Heuring T. et al. (2016) Ischemic stroke with troponin elevation: patient characteristics, resource utilization, and in-hospital outcomes. Cerebrovasc. Dis. 42, 213–223 10.1159/000445526 [DOI] [PubMed] [Google Scholar]
- 20.Batal O., Jentzer J., Balaney B., Kolia N., Hickey G., Dardari Z. et al. (2016) The prognostic significance of troponin I elevation in acute ischemic stroke. J. Crit. Care 31, 41–47 10.1016/j.jcrc.2015.09.018 [DOI] [PubMed] [Google Scholar]
- 21.Su Y.C., Huang K.F., Yang F.Y. and Lin S.K. (2016) Elevation of troponin I in acute ischemic stroke. PeerJ. 4, e1866 10.7717/peerj.1866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kerr G., Ray G., Wu O., Stott D.J. and Langhorne P. (2009) Elevated troponin after stroke: a systematic review. Cerebrovasc. Dis. 28, 220–226 10.1159/000226773 [DOI] [PubMed] [Google Scholar]
- 23.Stroup D.F., Berlin J.A., Morton S.C., Olkin I., Williamson G.D., Rennie D. et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012 10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- 24.Wells G., Shea B., O’Connell D., Peterson J., Welch V., Losos M. et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp [Google Scholar]
- 25.Egger M., Davey Smith G., Schneider M. and Minder C. (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Faiz K.W., Thommessen B., Einvik G., Omland T. and Rønning O.M. (2014) Prognostic value of high-sensitivity cardiac troponin T in acute ischemic stroke. J. Stroke Cerebrovasc. Dis. 23, 241–248 10.1016/j.jstrokecerebrovasdis.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 27.Sonderer J. and Katan Kahles M. (2015) Aetiological blood biomarkers of ischaemic stroke. Swiss Med. Wkly. 145, w14138 [DOI] [PubMed] [Google Scholar]
- 28.Tanindi A. and Cemri M. (2011) Troponin elevation in conditions other than acute coronary syndromes. Vasc. Health Risk Manag. 7, 597–603 10.2147/VHRM.S24509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fleming S.M. and Daly K.M. (2001) Cardiac troponins in suspected acute coronary syndrome: a meta-analysis of published trials. Cardiology 95, 66–73 10.1159/000047348 [DOI] [PubMed] [Google Scholar]
- 30.Anders B., Alonso A., Artemis D., Schafer A., Ebert A., Kablau M. et al. (2013) What does elevated high-sensitive troponin I in stroke patients mean: concomitant acute myocardial infarction or a marker for high-risk patients? Cerebrovasc. Dis. 36, 211–217 10.1159/000353875 [DOI] [PubMed] [Google Scholar]
- 31.Sandhu R., Aronow W.S., Rajdev A., Sukhija R., Amin H., D’Aquila K. et al. (2008) Relation of cardiac troponin I levels with in-hospital mortality in patients with ischemic stroke, intracerebral hemorrhage, and subarachnoid hemorrhage. Am. J. Cardiol. 102, 632–634 10.1016/j.amjcard.2008.04.036 [DOI] [PubMed] [Google Scholar]
- 32.Hjalmarsson C., Bokemark L., Fredriksson S., Antonsson J., Shadman A. and Andersson B. (2012) Can prolonged QTc and cTNT level predict the acute and long-term prognosis of stroke? Int. J. Cardiol. 155, 414–417 10.1016/j.ijcard.2010.10.042 [DOI] [PubMed] [Google Scholar]
- 33.Raza F., Alkhouli M., Sandhu P., Bhatt R. and Bove A.A. (2014) Elevated cardiac troponin in acute stroke without acute coronary syndrome predicts long-term adverse cardiovascular outcomes. Stroke Res. Treatment 2014, 621650 10.1155/2014/621650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Garrett M.C., Komotar R.J., Starke R.M., Doshi D., Otten M.L. and Connolly E.S. (2010) Elevated troponin levels are predictive of mortality in surgical intracerebral hemorrhage patients. Neurocrit. Care 12, 199–203 10.1007/s12028-009-9245-5 [DOI] [PubMed] [Google Scholar]
- 35.Chung P.W., Won Y.S., Kwon Y.J., Choi C.S. and Kim B.M. (2009) Initial troponin level as a predictor of prognosis in patients with intracerebral hemorrhage. J. Korean Neurosurg. Soc. 45, 355–359 10.3340/jkns.2009.45.6.355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hays A. and Diringer M.N. (2006) Elevated troponin levels are associated with higher mortality following intracerebral hemorrhage. Neurology 66, 1330–1334 10.1212/01.wnl.0000210523.22944.9b [DOI] [PubMed] [Google Scholar]
- 37.Zhang L., Wang Z. and Qi S. (2015) Cardiac troponin elevation and outcome after subarachnoid hemorrhage: a systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 24, 2375–2384 10.1016/j.jstrokecerebrovasdis.2015.06.030 [DOI] [PubMed] [Google Scholar]
- 38.Jensen J.K., Atar D. and Mickley H. (2007) Mechanism of troponin elevations in patients with acute ischemic stroke. Am. J. Cardiol. 99, 867–870 10.1016/j.amjcard.2006.10.052 [DOI] [PubMed] [Google Scholar]
- 39.Mannu G.S. (2014) The non-cardiac use and significance of cardiac troponins. Scott. Med. J. 59, 172–178 10.1177/0036933014540090 [DOI] [PubMed] [Google Scholar]
- 40.Ahn S.H., Kim Y.H., Shin C.H., Lee J.S., Kim B.J., Kim Y.J. et al. (2016) Cardiac vulnerability to cerebrogenic stress as a possible cause of troponin elevation in stroke. J. Am. Heart Assoc. 5, 10.1161/JAHA.116.004135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barber M., Morton J.J., Macfarlane P.W., Barlow N., Roditi G. and Stott D.J. (2007) Elevated troponin levels are associated with sympathoadrenal activation in acute ischaemic stroke. Cerebrovasc. Dis. 23, 260–266 10.1159/000098325 [DOI] [PubMed] [Google Scholar]