Summary
This is a case report of intracardiac foreign bodies that gained access to the heart by migration from a peripheral vein. The case report describes the diagnostic findings on cardiac imaging and summarizes different approaches to management.
Learning points:
Appearance of embolized cardiac missiles with reverberation and acoustic shadowing.
Role of different imaging modalities in the diagnosis of intracardiac foreign bodies.
Indications for surgical or transcatheter retrieval.
Keywords: bullet, pulmonary embolism, cardiac embolization
Background
Intracardiac foreign bodies can be encountered through different mechanisms; for example, embolized material from a peripheral vein as in fractured catheter or foreign bodies acquired by direct penetrating injuries to the heart. This case highlights the use of complementary imaging modalities.
Case report
A 28-year-old male was admitted with shotgun injury following attempted robbery. On examination, he was cardiovascularly stable, with shot entry wounds to the neck, left arm and left armpit, causing damage to the left axillary vein. The precordium was externally intact.
Investigations
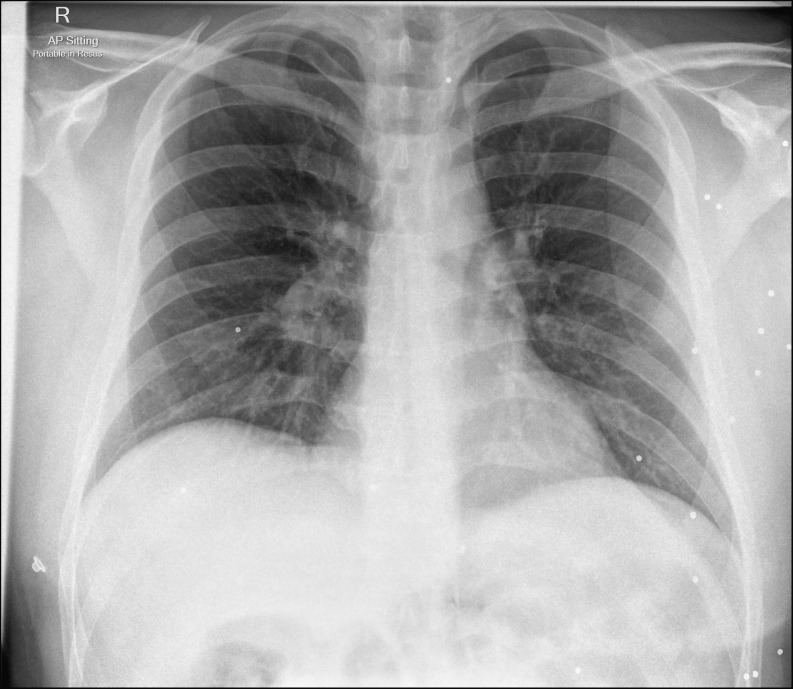
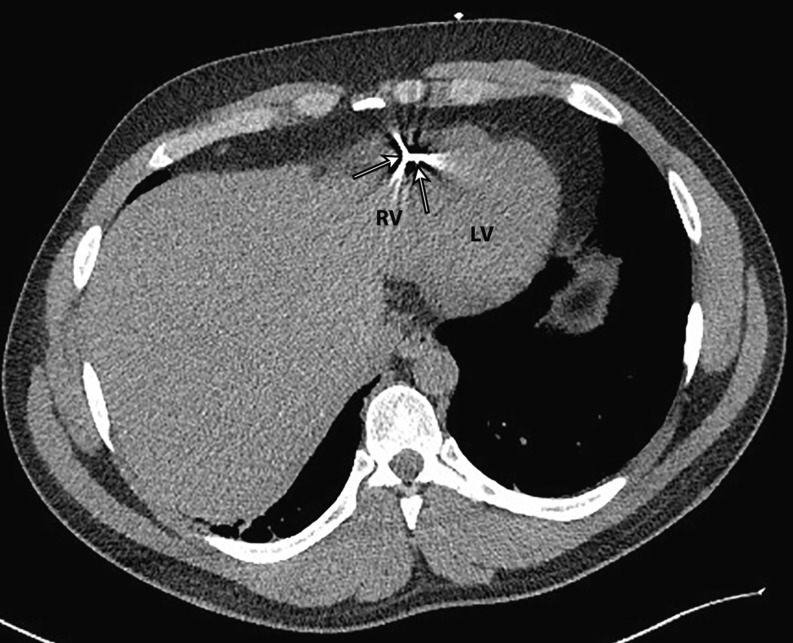
Chest radiography revealed multiple pellets in his chest (Fig. 1). CT scanning demonstrated two intracardiac pellets within the right ventricle (Fig. 2).
Figure 1.
Chest radiograph demonstrating multiple shotgun pellets, predominantly in left hemithorax and axilla.
Figure 2.
Transaxial CT slice demonstrating pellets in the right ventricle (arrowed). Characteristic blooming artefacts are seen. LV, left ventricle; RV, right ventricle.
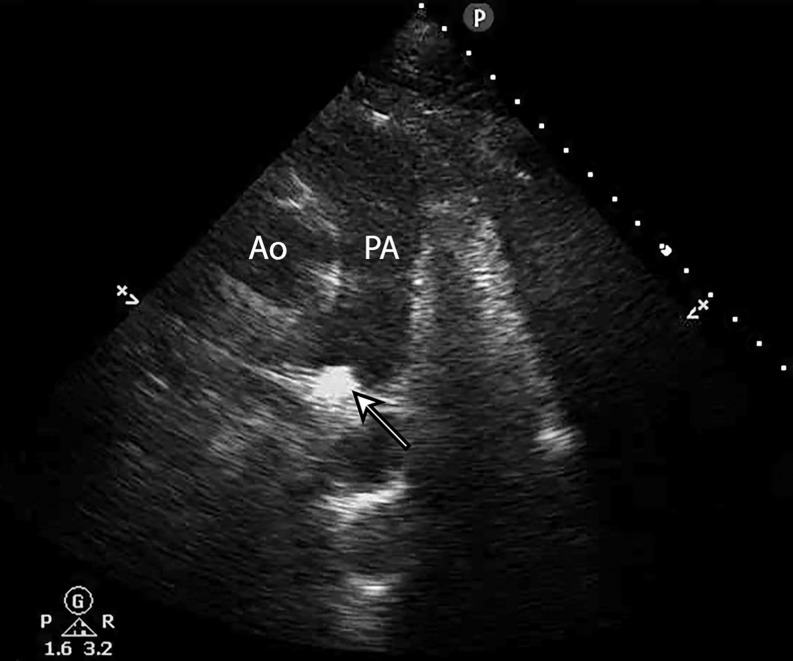
Transthoracic echocardiography performed shortly after CT showed an echogenic pellet within the right ventricle below the tricuspid annular plane (Video 1). The other pellet apparent on CT had migrated to the pulmonary artery bifurcation (Fig. 3, Videos 2 and 3).
Figure 3.
Modified parasternal short axis view of shotgun pellet in the pulmonary artery bifurcation, with typical hyperechoic appearance with acoustic shadowing under the pellet. Ao, aorta; PA, pulmonary artery.
Apical four-chamber view of pellet in the right ventricular cavity. View Video 1 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-17-0073/video-1.
Download Video 1 (281.6KB, mp4)
Modified parasternal short axis view of shotgun pellet at the pulmonary artery bifurcation. View Video 2 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-17-0073/video-2.
Download Video 2 (371.7KB, mp4)
Zoomed-in view of pellet from modified parasternal short axis view. View Video 3 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-17-0073/video-3.
Download Video 3 (213.7KB, mp4)
Serial CT chest and echocardiography were performed at 24 and 48 h. There was no evidence of thrombosis, infection, perforation or further movement of the emboli.
With no entry wounds on the precordium, it was clear that the shot had embolized from a peripheral vein entry point, likely the left axillary vein.
Treatment and outcome
Following multidisciplinary discussion, including cardiologists, surgeons and radiologists, the patient was managed conservatively, following interval imaging and antibiotic cover. The intravascular pellets were felt to be too small to significantly compromise patient haemodynamics (even if migrating to a more distal point within the pulmonary tree), and the risk of local or systemic complications was deemed to be low. Recovery was uneventful.
Discussion
Missiles such as shotgun pellets can gain access to the heart via direct penetrating injuries or vascular migration (1, 2).
Patients with direct cardiac trauma often present in extremis. Other reported complications include pericarditis, pulmonary or systemic embolization, arrhythmia, local infection, in situ clot formation or rarely local erosion into neighbouring bronchi or intracardiac shunts (3, 4).
Although plain radiography and tomographic imaging are useful, the most accurate modality to localise intracardiac missiles, and plan further management, is echocardiography (5). The hyperechoic appearance of the pellets with acoustic shadowing is characteristic of missile embolism.
Management options should be individualized depending on the size, intracardiac location and risk of infection or systemic embolization and may include surgical extraction or transcatheter retrieval (6, 7). In this case, conservative management was successfully employed, as the risk of infection, clinical sequelae or systemic embolization was deemed to be low.
A useful approach to guide the choice of management is as follows (8):
Symptomatic foreign bodies with infection, arrhythmia or neurological sequelae should be removed irrespective of their location.
Missiles with on-going adverse haemodynamic effects, e.g. intracardiac shunting or significant valvular complications should be removed.
Asymptomatic foreign bodies diagnosed immediately after the injury with an associated risk of infection, systemic embolization or erosion should be removed.
Asymptomatic foreign bodies without associated risks or diagnosed late after the injury may be treated conservatively, particularly if they are completely embedded in the myocardium or in the pericardium and pericardial space.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this case report.
Funding
This work did not receive any specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Patient consent
Written informed consent has been obtained from the patient for publication of the article and accompanying images.
Author contribution statement
The two authors were involved in the image acquisition and follow-up.
References
- 1.Symbas PN, Picone AL, Hatcher CR, Vlasis-Hale SE. Cardiac missiles. A review of the literature and personal experience. Annals of Surgery 1990. 211 639–647. [PMC free article] [PubMed] [Google Scholar]
- 2.Michelassi F, Pietrabissa A, Ferrari M, Mosca F, Vargish T, Moosa HH. Bullet emboli to the systemic and venous circulation. Surgery 1990. 107 239–245. [PubMed] [Google Scholar]
- 3.Lundy JB, Johnson EK, Seery JM, Pham T, Frizzi JD, Chasen AB. Conservative management of retained cardiac missiles: case report and literature review. Journal of Surgical Education 2009. 66 228–235. ( 10.1016/j.jsurg.2009.04.002) [DOI] [PubMed] [Google Scholar]
- 4.Elsner D. Images in cardiology. Penetrating heart injury from Second World War. Heart 2001. 86 323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amsel BJ, Van der Mast M, De Bock L, van Haasen R, Beeckman C. The importance of two-dimensional echocardiography in the location of a bullet embolus to the right ventricle. Annals of Thoracic Surgery 1988. 46 102–103. ( 10.1016/S0003-4975(10)65865-1) [DOI] [PubMed] [Google Scholar]
- 6.Gandhi SK, Marts BC, Mistry BM, Brown JW, Durham RM, Mazuski JE. Selective management of embolized intracardiac missiles. Annals of Thoracic Surgery 1996. 62 290–292. ( 10.1016/0003-4975(96)00097-5) [DOI] [PubMed] [Google Scholar]
- 7.Shannon JJ, Vo NM, Stanton PE, Jr, Dimler M. Peripheral arterial missile embolization: a case report and 22-year literature review. Journal of Vascular Surgery 1987. 5 773–778. ( 10.1016/0741-5214(87)90169-8) [DOI] [PubMed] [Google Scholar]
- 8.Actis Dato GM, Arslanian A, Di Marzio P, Filosso PL, Ruffini E. Posttraumatic and iatrogenic foreign bodies in the heart: report of fourteen cases and review of the literature. Journal of Thoracic and Cardiovascular Surgery 2003. 126 408–414. ( 10.1016/S0022-5223(03)00399-4) [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Apical four-chamber view of pellet in the right ventricular cavity. View Video 1 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-17-0073/video-1.
Download Video 1 (281.6KB, mp4)
Modified parasternal short axis view of shotgun pellet at the pulmonary artery bifurcation. View Video 2 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-17-0073/video-2.
Download Video 2 (371.7KB, mp4)
Zoomed-in view of pellet from modified parasternal short axis view. View Video 3 at http://movie-usa.glencoesoftware.com/video/10.1530/ERP-17-0073/video-3.
Download Video 3 (213.7KB, mp4)



 This work is licensed under a
This work is licensed under a