Abstract
This study aimed to investigate the effect of double oscillation exercise combined with elastic band exercise on the strength and thickness ratio of the scapular stabilizing muscles in healthy young individuals. A total of 30 subjects (17 male, 13 female) were randomly assigned to an elastic band exercise group (EBG) (n = 15) or an elastic band plus double oscillation exercise group (EB-DOG) (n = 15). A total of 28 subjects completed the experiment and evaluation. Patients in the EBG performed the elastic band exercise for shoulder flexion, extension, abduction, adduction, horizontal abduction/adduction, and internal/external rotation for 30 minutes/session, five times/week, for four weeks. Patients in the EB-DOG performed the elastic band exercise for 15 minutes and the double oscillation exercise in three planes of motion (frontal, sagittal, and transverse), using a Bodyblade® for 15 minutes/session, five times/week, for four weeks. Shoulder muscle strength was assessed using a manual muscle test device during maximal voluntary isometric contraction (MVIC), while the thicknesses of the scapular stabilizing muscles were assessed using rehabilitative ultrasound imaging both at rest and during MVIC. Both groups had significant effects on shoulder muscle strength, however, there was no significant difference between the two groups for change value of shoulder muscle strength (Bonferroni correction p < 0.005). Significant differences were observed in the group × time interactions for horizontal abduction, external rotation, and protraction. There was a statistically significant improvement in thickness ratio of LT and SA in the EB-DOG and no significant difference was founded in EBG (Bonferroni correction p < 0.006). In comparison between the two groups, EB-DOG showed a significant change in the thickness ratio of LT compared to EBG. In addition, significant differences were observed for the group × time interactions for the thickness ratio of the LT (F = 12.177, P = 0.002; Bonferroni correction p < 0.006). The double oscillation exercise combined with elastic band exercise more effectively increased the thickness of the shoulder stabilizing muscles compared with the resistance exercise alone.
Key points.
The double oscillation plus elastic band exercises significantly affected the thickness ratio of the shoulder stabilizing muscles.
The combination of resistance and oscillation exercises may be more effective on structural changes of the shoulder stabilizing muscles than resistance exercise alone.
Double oscillation exercises in the upper limb are effective in improving shoulder stability.
Key words: Shoulder stabilizer, rotator cuff, oscillation exercises, upper extremity, muscle strength, ultrasonography
Introduction
The shoulder complex is a region of frequent movement. For this reason, it is vulnerable to structural changes and can be easily injured (Lippitt and Matsen, 1993). Muscle imbalances can cause structural changes and movement deficits. Muscle balance signifies that the antagonist and agonist muscles surrounding a joint have reciprocal and balanced strength, endurance, and power (Kang et al., 2014). Strengthening exercises are effective for functional recovery and are a common therapeutic approach to improve muscle balance (Magarey and Jones, 2003).
The shoulder complex consists of prime movers such as the upper trapezius (UT), pectoralis major (PM), and middle deltoid (MD), and these muscles are often targeted in training programs to increase muscle power and hypertrophy (Kolber et al., 2009). However, the scapular stabilizing muscles, including the lower trapezius (LT), serratus anterior (SA), supraspinatus (SS), infraspinatus (IS), and the rhomboid muscle (RM), have been found to have impaired balance with respect to the glenohumeral prime movers in patients with subacromial impingement syndrome (Chester et al., 2010). Scapular stabilizing muscles assist in keeping the glenohumeral joint in place and play an important role in glenohumeral motion and dynamic stability of the shoulder joint (Hess, 2000).
Resistance exercise is the most common and effective exercise for strengthening the shoulder stabilizing muscles (Cardoso de Souza et al., 2009). A Thera-Band® or dumbbells that increase muscle strength through increasing external force are often used for resistance exercise (Andersen et al., 2010). The Bodyblade® has been used as a double oscillation device to evaluate and train muscle power, coordination, endurance, strength, intensity, and stabilization in athletes and the general population (Available at: https://www.bodyblade.com/pages/ physical-effects). Moreover, the vibration that is generated through the oscillation exercise is effective in improving muscle strength and endurance (Luo et al., 2005; Verschueren et al., 2004). Previous studies have shown that double-oscillation exercises using the Bodyblade® have a significant effect on activation of the UT, LT, and SA scapular muscles, rather than resistance exercises using cuff weights or the Thera-Band® (Lister et al., 2007). However, another previous study reported that 8 weeks of oscillation exercises had no significant effect on muscle strength improvement in the control or elastic band groups (Sugimoto and Blanpied, 2006). The effects of oscillation exercises are still unclear, and randomized controlled trial studies with oscillation exercises are scarce.
Most previous studies have reported the effects of upper limb training, including oscillation exercises, through electromyographic studies (Arora et al., 2013; Hallal et al., 2011; Lister et al., 2007). However, measurements of muscle morphology, such as muscle thickness, or a cross-sectional area measurement during a contraction or a task, are considered an indirect measure of muscle function (Teyhen and Koppenhaver, 2011). Rehabilitative ultrasound imaging measurements of the thickness of scapular stabilizing muscles (Schneebeli et al., 2014; Talbott and Witt, 2014) and shoulder prime movers (Bhansing et al., 2015; O’Sullivan et al., 2009) by physical therapists are considered reliable assessments. Although ultrasound imaging is an important measure to assess shoulder muscle function, there has been a lack of research to date on the effect of structural changes to muscle using oscillation exercises.
Therefore, the aim of this study was to investigate the effects of upper body double oscillation exercises on scapular stabilizing muscle strength and thickness ratio. Our hypothesis was that oscillation exercises, in combination with general resistance exercises, may have a greater effect on the strength and the thickness ratio of shoulder stabilizing muscles than resistance exercise alone. In addition, we aimed to demonstrate the effect of applying oscillation exercises to a general shoulder resistance exercise, and suggest a more effective method for shoulder strengthening training.
Methods
Participants
Thirty healthy staff members (15 men and 15 women) from Myongji Choonhey Rehabilitation Hospital in Seoul, Republic of Korea, volunteered to participate in this study. The inclusion criteria were: (1) no history of shoulder surgery or a recurring shoulder problem; (2) no acute shoulder injury; and (3) no history of participating in any formal upper body or shoulder strengthening exercise program during the previous 6 months. Two participants (one man, one woman) failed to complete the study because they participated in < 80% of the sessions. The average age, weight, and height of the participants were 29.29 ± 3.40 years, 65.32 ± 10.64 kg, and 167.93 ± 7.02 cm, respectively. The general characteristics of the participants are described in Table 1. The study protocol was approved by the institutional review board of Sahmyook University (SYUIRB2015-124) in Seoul and the World Health Organization International Clinical Trials Registry Platform (KCT0001904). The participants provided written informed consent after receiving verbal and written information about the study.
Table 1.
General characteristics of the participants. Values are means (±SD).
| EBG | EB-DOG | p | |
|---|---|---|---|
| Sex (M/F) | 8/6 | 9/5 | .704 |
| Age (years) | 29.0 (3.6) | 29.6 (3.3) | .665 |
| Height (m) | 1.68 (.08) | 1.68 (.06) | .915 |
| Weight (kg) | 64.9 (9.8) | 65.8 (11.8) | .882 |
| BMI (kg·m2) | 21.8 (1.9) | 22.1 (3.0) | .754 |
EBG: elastic band exercise group; EB-DOG: elastic band plus double oscillation exercise; M: male; F: female; BMI: body mass index; SD: standard deviation.
Measurements: Shoulder muscle strength
The participants’ shoulders were examined for flexion, extension, abduction, adduction, horizontal abduction/adduction, internal/external rotation, and protraction, using a handheld dynamometer (Roy et al., 2009). The maximal voluntary isometric contraction (MVIC) of the shoulder muscles on each participant’s dominant side was measured using a manual muscle tester (model 11001163; Lafayette Instruments, Leicis, England). The dominant arm was determined through a questionnaire consisting of questions such as “Which hand do you prefer to use for this activity?” and “Do you ever use your other hand for this activity?” The participants were positioned in the sitting, prone, or supine position for the measurements, and stability was provided using the measurer to isolate the joint motion. Measurement positions and descriptions of each muscle are depicted in Table 2. The participants performed one practice trial and three test trials in each of the three test positions. Each trial consisted of a 3-second MVIC, and a 30-second rest period was provided between trials. The average MVIC of the three trials was used as the criterion measure. The examiners and participants were blinded to the test results during the strength testing. Shoulder strength was evaluated before and after the intervention. To minimize the effect of post-training fatigue, the post-test was performed three days after the training.
Table 2.
Conditions for measuring shoulder joint muscle strength using a hand held dynamometer.
| MVIC task | Posture | Limb posture | Dynamometer position |
|---|---|---|---|
| Flexion | Seated | 0° shoulder flexion, 0° abduction, elbow slightly bent, forearm in neutral |
Distal lateral humerus supracondylar crest |
| Extension | Seated | 0eatedulder flexion, 0t abduction, 0° elbow flexion, forearm in neutral |
Above the olecranon |
| Abduction | Seated | 90atedoulder abduction, elbow slightly bent, forearm in pronation |
Distal lateral humerus supracondylar crest |
| Adduction | Seated | 0eatedulder flexion, 0t abduction, 0° elbow flexion, forearm in pronation |
Distal medial humerus supracondylar crest |
| Horizontal abduction | Prone | 90° shoulder abduction, elbow slightly bent, forearm in pronation |
Above the olecranon |
| Horizontal adduction | Supine | 90° shoulder abduction, elbow slightly bent, forearm in pronation |
Distal lateral humerus |
| Internal rotation | Seated | 45° shoulder flexion, 135° elbow flexion | Styloid process of the ulna |
| External rotation | Seated | 45° shoulder flexion, 135° elbow flexion | Styloid process of the ulna |
| Protraction | Seated | 90° shoulder flexion, elbow full extension | 2nd~3rd proximal interphalanges |
MVIC: maximal voluntary isometric contraction.
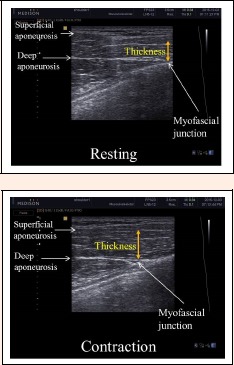
Shoulder prime mover and stabilizing muscle thickness ratio
The thickness of the shoulder prime movers (UT, PM, and MD) and stabilizers (LT, SA, SS, IS, and RM) were measured using real-time B-mode ultrasonography (MYSONO US, Samsung Medicine, Seoul, Korea) with a 7.5-MHz linear transducer. Muscle thickness was measured at rest and during MVIC, and the resistance position and direction were determined using the method defined in the manual muscle test, according to the action of each muscle. Muscle thickness was measured 3 times at rest and 3 times during MVIC, and the average thickness value and thickness ratio were calculated. The formula that was used to obtain standardized thickness ratios is shown below.
The participants were positioned in the prone, side-lying, sitting, or standing position for ultrasound imaging of each shoulder muscle. The measurement positions, the transducer position, and the descriptions of ultrasound images for each muscle are described in Table 3. The muscle thickness of UT (O'Sullivan et al., 2009), PM (Abe et al., 2000; Yasuda et al., 2010), and MD (Bhansing et al., 2015) was measured as a shoulder prime mover, and the muscle thickness of LT (O'Sullivan et al., 2007), SA (Talbott and Witt, 2013), SS (Schneebeli et al., 2014), IS (Koppenhaver et al., 2015), and RM (Jeong et al., 2016) was measured as a shoulder stabilizing muscle. The measured ultrasound image of each muscle corresponds with Figures 1 to 8. When measuring muscle strength and muscle thickness, measurements were obtained after a sufficient rest period between each measurement in order to minimize the potential effect of muscle fatigue.
Table 3.
The measurement position and method for scapular stabilizing and shoulder large muscles.
| Posture | Transducer position | Image | |
|---|---|---|---|
| Upper trapezius | Prone | Spinous process at the level of C6 | Triangular shaped medial portion of the muscle |
| Lower trapezius | Prone | Spinous process at the level of T8 | Medial portions of the muscle belly |
| Serratus anterior | Side-lying | Superior to the peak convexity of the most distal rib | Between the superior and inferior echogenic fascial lines |
| Supraspinatus | Seated | Center of the supraspinous fossa | 2cm from the angle formed by the superior muscular fascia of the supraspinatus |
| Infraspinatus | Seated | Center of the infraspinous fossa | 2cm from the angle formed by the superior muscular fascia of the infraspinatus |
| Rhomboid major | Seated | Center of two lines: the middle of the line from T2 to the root of the scapular spine and the middle of the line from T5 to the scapular inferior angle | Vertical length between the inferior echogenic fascial line of the trapezius and the superior line of the posterior serratus |
| Pectoralis major | Stood | Between third and fourth of costa under the clavicle midpoint | Between the subcutaneous adipose tissue–muscle interface and the muscle–bone interface |
| Middle deltoid | Seated | Superior surface of the acromion process of the scapula | Quarter of the distance from acromion to the lateral epicondyle |
Side-lying: Side-lying with shoulder supported in 90° flexion
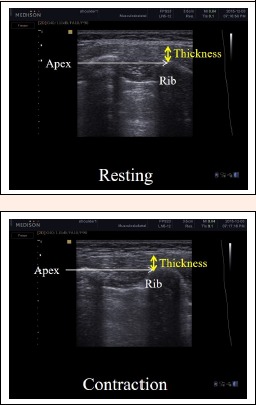
Figure 1.
Ultrasound images of the right upper trapezius muscle at the level of C6 at rest and during MVIC. MVIC: maximal voluntary isometric contraction.
Figure 8.
Ultrasound images of the middle deltoid muscle at rest and during MVIC. Thickness was measured at a quarter of the distance from the acromion to the lateral epicondyle. MVIC: maximal voluntary isometric contraction.
Intervention
After the pretest, participants were randomly assigned to the elastic band exercise group (EBG) or the elastic band plus double oscillation exercise group (EB-DOG).
Participants in the EBG performed the strengthening exercise using a flexible elastic band on the dominant upper limb for 30 minutes per session, five times a week for four weeks. The extra heavy type (blue color) of Thera-Band® (TheraBand, Hygenic Corporation, Akron, OH, USA) provided the elastic band resistance. The length of the Thera-Band® was held at a constant 1.52 meters. Each session consisted of warm-up and cool-down stretching and strengthening exercises. The training program consisted of both dynamic and isometric sets of shoulder flexion, extension, abduction, scapular plane shoulder abduction (scaption), internal rotation, and external rotation. For the dynamic exercises, the participants performed two-second concentric contractions and two-second eccentric contractions according to each action. The length of the elastic band was adjusted according to the amount of resistance the participant felt “to a degree that is somewhat challenging.” As the muscle strength of the participant increased, the amount of resistance was progressively increased by shortening the band length. For the static exercises, the participants were asked to hold the band for three seconds while maintaining the appropriate elastic band length at each defined position. The participants were also instructed to relax the non-training limb during the training to limit any mirroring activity of the non-trained limb.
Participants in the EB-DOG performed resistance exercises using a Thera-Band® for 15 minutes and double oscillation exercises using a Bodyblade® (Mad Dogg Athletics, Venice, CA, USA) for 15 minutes, both using the dominant upper limb, five times a week for four weeks. The double oscillation device used in this study was a polycarbonate flexible blade (Bodyblade®) device 120 cm in length, weighing 0.68 kg, with a handgrip in the center (Bodyblade® Web site. Available at: http://www.bodyblade.com). The participants performed the oscillation exercise on each frontal, sagittal, and transverse plane with flexion of the shoulder to 90° and elbows extended, while firmly holding the flexible blade bar. The double oscillation exercises included mediolateral oscillations in the frontal plane (Figures 9-A), dorsoventral oscillations in the sagittal plane (Figure 9-B), and superior and inferior oscillations in the transverse plane (Figures 9-C). With only minimal effort, the two ends began to oscillate at a fixed rate with a natural frequency of 4.5 Hz. For the oscillating movements in the frontal and transverse planes, the wrist and elbow were held steady (isometrically held) with movement initiated using the shoulder. Moving the Bodyblade® in the sagittal plane involved small flexion and extension movements at the elbow and shoulder.
Figure 9.
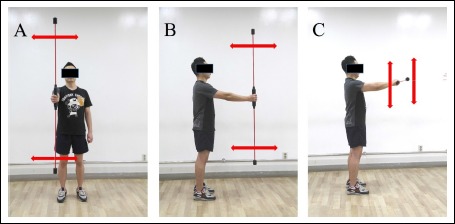
The double oscillation exercises included mediolateral oscillations in the frontal plane (A), dorsoventral oscillations in the sagittal plane (B), and superior and inferior oscillations in the transverse plane (C). Participants performed a double oscillation exercise by holding the middle portion of the flexible bar firmly with the flexion of the shoulder to 90 ° and elbows extended.
Statistical analysis
The statistical analysis was performed using SPSS ver. 21.0 (SPSS for Windows; SPSS Inc., Chicago, IL, USA). The Shapiro-Wilk test was used to confirm the normal distribution of the outcome variables. Groups were compared at baseline using t-tests for the independent samples for continuous variables and Chi-squared tests for categorical data. All outcome variables were normally distributed. For intergroup comparison of intervention effects, a paired t-test was performed on the pretest value and on the posttest value. For comparison of the intervention effects between the two groups, an independent t-test was performed on change variables that subtracted the pretest value from the posttest value. We chose to use a repeated-measures analysis of variance with an inter-subject factor at two levels (the two groups) and an intra-subject factor at two levels (pre-intervention and post-intervention). The group and time interaction determined the efficacy of the double oscillation exercise on the outcome measures. For all tests, statistical significance was set at 0.05. To account for multiple testing, we used the Bonferroni correction and considered significance achieved when p < 0.05/9 = 0.005 for shoulder muscle strength. We also used the Bonferroni correction for the shoulder muscle thickness ratio and considered significance was achieved when p < 0.05/8 = 0.006. The Bonferroni correction, which lowers the critical P values for each particular test, based on the number of tests to be performed, is frequently used to reduce problems associated with multiple comparisons (Cabin and Mitchell, 2000).
Results
A summary of the 28 participants’ general characteristics is shown in Table 1. No significant differences in baseline values were observed between the EBG and the EB-DOG.
Table 4 compares shoulder strength between the two groups. Following four weeks training, there was a statistically significant improvement in the EB-DOG in flexion, extension, abduction, adduction, horizontal abduction, external rotation, internal rotation, and protraction (Bonferroni correction p < 0.005). In the EBG, statistically significant improvements were identified in flexion, extension, horizontal abduction, horizontal adduction, external rotation, internal rotation, and protraction (Bonferroni correction p < 0.005). However, there was no significant difference in the change value of shoulder muscle strength between the two groups. Both groups showed a main effect of time on flexion (F = 36.663, p < 0.000), extension (F = 38.938, p < 0.000), abduction (F = 31.175, p < 0.000), adduction (F = 21.018, p < 0.000), horizontal abduction (F = 36.639, p < 0.000), horizontal adduction (F = 23.210, p < 0.000), external rotation (F = 70.695, p < 0.000), internal rotation (F = 120.223, p < 0.000), and protraction (F = 57.144, p < 0.000). However, no significant differences were observed for the group × time interactions.
Table 4.
Comparison of the shoulder strength between the EBG and EB-DOG (Units: lb).
| EBG | EB-DOG | F(p) for time factor |
F(p) for group x time interaction |
|||||
|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Change | Pre-test | Post-test | Change | |||
| Flexion | 32.1 (9.6) | 37.3 (9.9)* | 6.5 (5.1) | 33.8 (11.4) | 40.4 (11.8)* | 5.2 (5.2) | 36.663 (.000)† | .442 (.512) |
| Extension | 31.6(6.2) | 37.6 (8.4)* | 5.9 (5.4) | 32.6 (9.0) | 38.5 (9.7)* | 6.0 (4.7) | 38.938 (.000) † | .003 (.960) |
| Abduction | 36.2 (38.7) | 38.7 (10.1) | 4.5 (3.6) | 37.9 (11.3) | 41.8 (11.1)* | 2.5 (2.9) | 31.175 (.000) † | 2.516 (.125) |
| Adduction | 40.1(14.5) | 45.8 (14.0) | 6.9 (7.3) | 41.3(135) | 48.2 (16.0)* | 5.7 (7.3) | 21.018 (.000) † | .189 (.667) |
| H-ABD | 25.9 (6.5) | 28.8 (5.6)* | 6.2 (4.7) | 26.5 (7.2) | 32.8 (9.8)* | 33.0 (3.2) | 36.639 (.000) † | 4.564 (.042) |
| H-ADD | 22.5 (5.9) | 27.3 (7.7)* | 7.8 (8.9) | 24.1 (6.5) | 31.9 (12.8) | 4.8 (4.1) | 23.210 (.000) † | 1.350 (.256) |
| ER | 28.4 (8.3) | 31.0 (8.3)* | 4.3 (2.3) | 28.8 (8.5) | 33.0 (9.6)* | 2.5 (2.0) | 70.695 (.000) † | 4.606 (.041) |
| IR | 29.7 (8.9) | 32.6 (8.5)* | 4.2 (1.7) | 29.6 (8.9) | 33.8 (9.5)* | 2.9 (1.8) | 120.223 (.000)† | 3.832 (.061) |
| Protraction | 33.7 (6.8) | 38.1 (6.7)* | 7.8 (5.4) | 33.7 (8.3) | 41.5 (8.6)* | 4.4 (2.8) | 57.144 (.000) † | 4.517 (.043) |
Values are described mean ± SD.
* Bonferroni correction p < 0.005 for within-group differences.
† Bonferroni correction p < 0.005 for time factor. EBG: elastic band exercise group; EB-DOG: elastic band plus double oscillation exercise group; H-ABD: horizontal abduction; H-ADD: horizontal adduction; ER: external rotation; IR: internal rotation.
Table 5 compares the muscle thickness ratio of the shoulder prime movers and shoulder stabilizing muscles between the two groups. There was a statistically significant improvement in the thickness ratio of LT and SA in the EB-DOG and no significant difference was found in the EBG (Bonferroni correction p < 0.006). In comparison between the two groups, the EB-DOG showed a significant change in the thickness ratio of LT compared to the EBG. Both groups showed a main effect of time on shoulder thickness ratio of the SA and PM (Bonferroni correction p < 0.006). In addition, significant differences were observed for the group × time interactions for the thickness ratio of the LT (F = 12.177, p = 0.002; Bonferroni correction p < 0.006).
Table 5.
Comparison of the muscle thickness for shoulder prime mover and stabilizing muscles between the EBG and EB-DOG (Units: cm).
| EBG | EB-DOG | F(p) for time factor |
F(p) for group x time interaction |
|||||
|---|---|---|---|---|---|---|---|---|
| Pre-test | Post-test | Change | Pre-test | Post-test | Change | |||
| Upper trapezius | 1.42 (.19) | 1.51 (.17) | .08 (.23) | 1.40 (.24) | 1.51 (.19) | .11 (.14) | 7.502 (.011) | .158 (.694) |
| Lower trapezius | 1.53 (.36) | 1.42 (.22) | -.11 (.33) | 1.47 (.19) | 1.69 (.22)* | .21 (.12)† | 1.275 (.269) | 12.177 (.002)¶ |
| Serratus anterior | 1.28 (.12) | 1.40 (.18) | .12 (.15) | 1.29 (.09) | 1.53 (.22)* | .23 (.24) | 21.352 (.000)† | 2.218 (.148) |
| Supraspinatus | 1.36 (.16) | 1.32 (.12) | -.03 (.13) | 1.37 (.24) | 1.33 (.14) | -.03 (.22) | 1.139 (.296) | .003 (.955) |
| Infraspinatus | 1.41 (.15) | 1.37 (.22) | -.03 (.17) | 1.37 (.12) | 1.40 (.10) | .03 (.13) | .006 (.938) | 1.617 (.215) |
| Rhomboid major | 1.53 (.30) | 1.56 (.27) | .02 (.16) | 1.50 (.22) | 1.63 (.27) | .12 (.33) | 2.254 (.145) | .956 (.337) |
| Pectoralis major | 1.24 (.11) | 1.38 (.20) | .13 (.22) | 1.30 (.15) | 1.45 (.15) | .15 (.18) | 13.437 (.001)† | .022 (.883) |
| Middle deltoid | 1.36 (.21) | 1.40 (.23) | .04 (.22) | 1.47 (.19) | 1.56 (.29) | .09 (.20) | 2.618 (.118) | .374 (.546) |
Values are described mean ± SD.
*Bonferroni correction p < 0.006 for within-group differences.
†Bonferroni correction p < 0.006 for between group differences of change value (post value minus pre value). †Bonferroni correction p < 0.006 for time factor.
¶Bonferroni correction p < 0.006 for group x time interaction. EBG: elastic band exercise group; EB-DOG: elastic band plus double oscillation exercise group.
Discussion
In shoulder joints with a large range of motion, the shoulder stabilizing muscles surrounding the shoulder joint allow for proper kinematic function and are important in preventing pain and injury (Johnson and Pandyan, 2005). Oscillation exercise is effective in strengthening the shoulder stabilizing muscles and is widely used as a method to improve the physical capacity of the shoulder (Schulte and Warner, 2001). Vibration can be applied directly to muscles and tendons via specific stimulators, vibration platforms, oscillation poles, or blades (Jordan et al., 2005; Shinohara, 2005). Unlike other types of vibration training, training using oscillation poles uses a low frequency of approximately 4.5 Hz and, while vibration does not produce external forces, it does produce muscle contractions (Anders et al., 2007; Moreside et al., 2007).
Lister et al. (2007) investigated the EMG of the UT, LT, and SA when using the Bodyblade®, Thera-Band®, and cuff weights during shoulder flexion and abduction, and found that the Bodyblade® resulted in significantly higher scapular activity as compared with the other two exercises. In another EMG study, it was reported that the muscle activity of the UT, LT, and MD was significantly higher when using oscillatory poles than when using non-oscillatory poles (Hallal et al., 2011). Similarly, Arora et al. demonstrated that the Bodyblade® exhibited greater trunk and shoulder muscle activation, particularly in the transverse plane, than did the Thera-Band®’s flex bars (Arora et al., 2013). In addition, Parry et al. (2012) found that the Bodyblade® Pro produced greater deltoid, IS, SA, pectoralis major, erector spine activity than using the dumbbell trials. EMG activity for the Bodyblade® Pro exceeded 50% of the MVIC during both shoulder flexion and abduction. These EMG studies demonstrated that the muscle activity of the shoulder stabilization muscles was significantly higher than that of the other resistance exercises (e.g., elastic band exercise, dumbbell exercise) when oscillation exercises were performed using the Bodyblade® during shoulder flexion and abduction. This is similar to the training method of this study, in which the wrist and elbow were minimally moved (isometrically held) and movement was initiated from the shoulder. Moreover, the strategy of training on three planes (sagittal, frontal, transverse plan) during flexion and abduction of the shoulder is similar to that of Arora et al. (2013). In this study, the significant effect of the SA and LT thickness ratio, which are both representative stabilizing muscles, in the oscillation group demonstrated that oscillation exercise is more effective in changing the muscle structure of shoulder stabilizing muscles than shoulder prime movers. Because both groups performed resistance training using an elastic band, both groups showed significant differences in changes in muscle strength of shoulder prime movers and shoulder stabilizing muscles, but the results of the comparison between the two groups were not significant. Sugimoto and Blanpied reported that 40 young adults performed internal and external rotation exercises for eight weeks using the Bodyblade® and showed no significant increases in muscle strength, as compared with the control and elastic band groups (Sugimoto and Blanpied, 2006). In the present study, the oscillation exercises focused on the internal/external rotation of the shoulder with the elbow flexed, which differs somewhat from the oscillation exercise method of previous studies. Therefore, it is difficult to determine the oscillation effect solely based on these results, and it remains necessary to prove the effectiveness of the oscillation training method and establish an effective protocol.
The Bodyblade® with a flexible pole, used in the oscillation exercise in this study, requires body support to firmly fix the upper limb while generating the vibration. For the oscillation to be realized at a natural frequency, movements of the participant’s trunk and proximal arm should be minimized (Sanchez-Zuriaga et al., 2009). Moreover, scapulothoracic stability plays an important role in the process of transmitting the force from the lower limb and trunk to the upper limb during oscillation (Kibler and McMullen, 2003; Matias and Pascoal, 2006). As the arm is elevated, the scapula is upwardly rotated and posteriorly tilted; at the same time, the SA muscles play a stabilizing role to maintain congruency with the thorax (Solem-Bertoft et al., 1993). The LT provides stability to the thorax and is most active in horizontal abduction with external rotation movements since its movement causes the external rotation, posterior tilt, and depression of the scapula (Neumann, 2002). These results may be attributable to activation of the stabilizing muscles in order to overcome the external load during the oscillation exercise. Therefore, the LT and SA, which are among the scapular stabilizing muscles that maintain scapular position, play an important role, and structural changes in these muscles are natural outcomes of the oscillation exercise.
The shoulder stabilizing muscles (LT, SA, SS, IS, and RM) surrounding the shoulder play a critical role in shoulder stability. Of the shoulder stabilizing muscles, SA originates at the outer surface of the upper eighth or ninth rib and inserts along the medial scapular border. The SA protracts and stabilizes the scapula and plays an important role in its upward rotation, such as when a weight is lifted overhead. It performs this function in parallel with the upper and lower fibers of the trapezius (Yoo, 2014). Moreover, the inferior and superior parts of the SA and RM act as synergists and keep the scapula pressed against the thorax. One of the other muscles that contributes to shoulder joint stability, the rotator cuff (which includes the IS and SS), provides dynamic stability by compressing the humeral head within the concave glenoid fossa during upper extremity motions (Wilk and Arrigo, 1993). In this way, the rotator cuff stabilizes the glenohumeral joint, controls humeral head translation, and performs multiple functions including shoulder abduction, internal rotation, and external rotation. The IS and SS muscles play significant roles in scaption (Escamilla et al., 2009), while the SS is more effective in general shoulder abduction because of its moment arm. The results of this study, in which only SA and LT structural changes had a significant effect, show that SA and LT play a prominent role in shoulder stability. However, since the other shoulder stabilizing muscles work together to contribute to shoulder stability, training protocols for oscillation exercises that can strengthen the shoulder stabilizing muscle in a balanced manner are needed.
Our study has some limitations. First, according to the study design, participants in the EB-DOG performed both resistance and oscillation exercises. Therefore, the oscillation exercises and resistance exercises cannot be compared separately because the effects of the two exercises are mixed, and the individual effects of the oscillation versus resistance exercises could not be demonstrated. Second, the absolute oscillation amplitude and elastic band load were not exactly matched between participants because the participants had various abilities. Third, only 28 healthy young adults were included; therefore, it is difficult to generalize our findings to all patients with shoulder problems. Fourth, this study was conducted on a specific occupational group; therefore, it is difficult to generalize the results of this study to all healthy adults of the same age group.
Conclusions
The double oscillation plus elastic band exercises significantly affected the thickness ratio of the shoulder stabilizing muscles. Therefore, we consider the combination of resistance and oscillation exercises may be more effective on structural changes of the shoulder stabilizing muscles than resistance exercise alone.
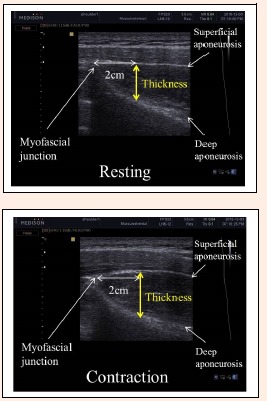
Figure 2.
Ultrasound images of the lower trapezius muscle at the level of T8 at rest and during MVIC. MVIC: maximal voluntary isometric contraction.
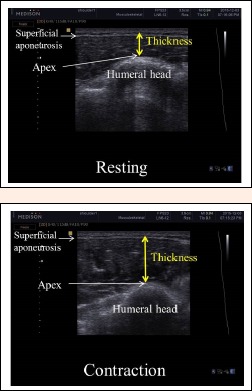
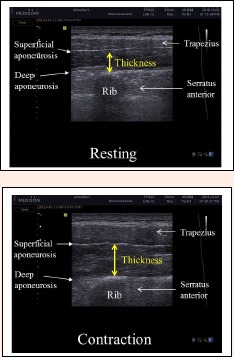
Figure 3.
Ultrasound images of the serratus anterior muscle at rest and during MVIC. The rib was used as a reference for measurement of the serratus anterior. The vertical yellow lines, spaced out to incorporate the apex of the rib, were drawn from the rib to the superior fascial border of the serratus anterior. MVIC: maximal voluntary isometric contraction.
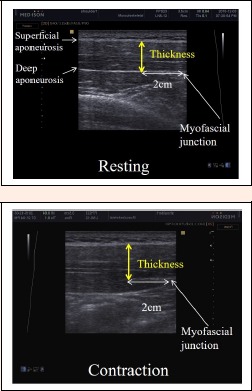
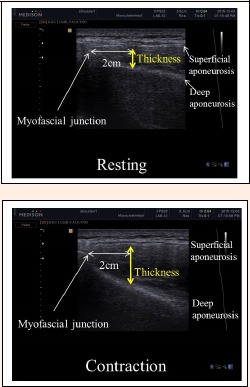
Figure 4.
Ultrasound images of the supraspinatus muscle at rest and during MVIC. The point of 2 cm from the angle formed by the superior muscular fascia of the supraspinatus was measured. Yellow lines represent the method for off-line supraspinatus muscle thickness measurement. MVIC: maximal voluntary isometric contraction.
Figure 5.
Ultrasound images of the infraspinatus muscle at rest and during MVIC. The ultrasound images were taken from the inferior-most aspect of the superficial fascia to the most superior aspect of the infraspinous fossa, which appeared as a bright, continuous hyperechoic line spanning the width of the screen.MVIC: maximal voluntary isometric contraction.
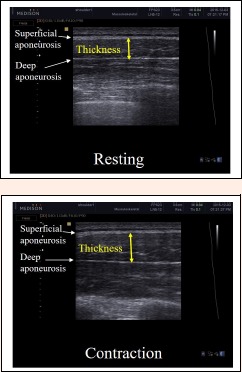
Figure 6.
Ultrasound images of the rhomboid major muscle at rest and during MVIC. Ultrasound images of the rhomboid major muscle located between the trapezius and posterior serratus muscles. The thickness can be examined as the vertical length between the inferior echogenic fascial line of the trapezius and the superior line of the posterior serratus. MVIC: maximal voluntary isometric contraction.
Figure 7.
Ultrasound images of the pectoralis major muscle at rest and during MVIC. Thickness was measured at each aspect of distance between superficial and deep aponeurosis. MVIC: maximal voluntary isometric contraction.
Acknowledgements
We confirm that there are no known conflicts of interest associated with this publication and that no significant financial support was received for this work that could have influenced its outcome.
Biographies
Jieun CHO
Employment
Department of Rehabilitation & Assistive Technology Translational Research Center for Rehabilitation Robot, National Rehabilitation Center.
Degree
MSc
Research interests
Virtual reality, Rehabilitation robot
E-mail: wldms880226@hanmail.net
Kyeongbong LEE
Employment
Physical Therapy Part, Department of Physical & Rehabilitation, Samsung Medical Center.
Degree
PhD
Research interests
Cardiopulmonary physical therapy
E-mail: pptt798@gmail.com
Minkyu KIM
Employment
Department of Physical Therapy, Myongji Choonhey Rehabilitaion Hospital.
Degree
MSc
Research interests
Virtual Reality
E-mail: mk5519@hanmail.net
Joohee HAHN
Employment
Department of Physical Therapy, Sahmyook University.
Degree
MSc
Research interests
Neurorehabilitation
E-mail: dakdagrr@naver.com
Wanhee LEE
Employment
Department of Physical Therapy, Sahmyook University College of Health Science
Degree
PhD
Research interests
Rehabilitative ultrasound imaging
E-mail: whlee@syu.ac.kr
References
- Abe T., DeHoyos D.V., Pollock M.L., Garzarella L. (2000) Time course for strength and muscle thickness changes following upper and lower body resistance training in men and women. European Journal of Applied Physiology 81, 174-180. [DOI] [PubMed] [Google Scholar]
- Anders C., Wenzel B., Scholle H.-C. (2007) Cyclic upper body perturbations caused by a flexible pole: influence of oscillation frequency and direction on trunk muscle co-ordination. Journal of Back and Musculoskeletal Rehabilitation 20, 167-175. [Google Scholar]
- Andersen L.L., Andersen C.H., Mortensen O.S., Poulsen O.M., Bjornlund I.B., Zebis M.K. (2010) Muscle activation and perceived loading during rehabilitation exercises: comparison of dumbbells and elastic resistance. Physical Therapy 90, 538-549. [DOI] [PubMed] [Google Scholar]
- Arora S., Button D.C., Basset F.A., Behm D.G. (2013) The effect of double versus single oscillating exercise devices on trunk and limb muscle activation. International Journal of Sports Physical Therapy 8, 370-380. [PMC free article] [PubMed] [Google Scholar]
- Bhansing K.J., Van Rosmalen M.H., Van Engelen B.G., Vonk M.C., Van Riel P.L., Pillen S. (2015) Increased fascial thickness of the deltoid muscle in dermatomyositis and polymyositis: An ultrasound study. Muscle Nerve 52, 534-349. [DOI] [PubMed] [Google Scholar]
- Cabin R.J., Mitchell R.J. (2000) To Bonferroni or not to Bonferroni: when and how are the questions. Bulletin of the Ecological Society of America 81, 246-248. [Google Scholar]
- Cardoso de Souza M., Trajano Jorge R., Jones A., Lombardi I., Junior, Natour J. (2009) Progressive resistance training in patients with shoulder impingement syndrome: literature review. Reumatismo 61, 84-89. [DOI] [PubMed] [Google Scholar]
- Chester R., Smith T.O., Hooper L., Dixon J. (2010) The impact of subacromial impingement syndrome on muscle activity patterns of the shoulder complex: a systematic review of electromyographic studies. BMC Musculoskeletal Disorders 11, 45, Mar 09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escamilla R.F., Yamashiro K., Paulos L., Andrews J.R. (2009) Shoulder muscle activity and function in common shoulder rehabilitation exercises. Sports Medicine 39, 663-685. [DOI] [PubMed] [Google Scholar]
- Hallal C.Z., Marques N.R., Silva S.R., Dieen J.V., Goncalves M. (2011) Electromyographic activity of shoulder muscles during exercises performed with oscillatory and non-oscillatory poles. Brazilian Journal of Physical Therapy 15, 89-94. [PubMed] [Google Scholar]
- Hess S.A. (2000) Functional stability of the glenohumeral joint. Manual Therapy 5, 63-71. [DOI] [PubMed] [Google Scholar]
- Jeong J.R., Ko Y.J., Ha H.G., Lee W.H. (2016) Reliability of rehabilitative ultrasonographic imaging for muscle thickness measurement of the rhomboid major. Clinical Physiotherapy and Functional Imaging 36, 134-138. [DOI] [PubMed] [Google Scholar]
- Johnson G.R., Pandyan A.D. (2005) The activity in the three regions of the trapezius under controlled loading conditions--an experimental and modelling study. Clinical Biomechanics 20, 155-161. [DOI] [PubMed] [Google Scholar]
- Jordan M.J., Norris S.R., Smith D.J., Herzog W. (2005) Vibration training: an overview of the area, training consequences, and future considerations. The Journal of Strength & Conditioning Research 19, 459-466. [DOI] [PubMed] [Google Scholar]
- Kang S.R., Yu C.H., Han K.S., Kwon T.K. (2014) Comparative analysis of basal physical fitness and muscle function in relation to muscle balance pattern using rowing machines. Bio-medical materials and engineering 24, 2425-2435. [DOI] [PubMed] [Google Scholar]
- Kibler W.B., McMullen J. (2003) Scapular dyskinesis and its relation to shoulder pain. Journal of the American Academy of Orthopaedic Surgeons 11, 142-151. [DOI] [PubMed] [Google Scholar]
- Kolber M.J., Beekhuizen K.S., Cheng M.S., Hellman M.A. (2009) Shoulder joint and muscle characteristics in the recreational weight training population. The Journal of Strength & Conditioning Research 23, 148-157. [DOI] [PubMed] [Google Scholar]
- Koppenhaver S., Harris D., Harris A., O’Connor E., Dummar M., Croy T., Walker M., Flynn T. (2015) The reliability of rehabilitative ultrasound imaging in the measurement of infraspinatus muscle function in the symptomatic and asymptomatic shoulders of patients with unilateral shoulder impingement syndrome. International Journal of Sports Physical Terapy 10, 128-135. [PMC free article] [PubMed] [Google Scholar]
- Lippitt S., Matsen F. (1993) Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res 20-28. [PubMed] [Google Scholar]
- Lister J.L., Del Rossi G., Ma F., Stoutenberg M., Adams J.B., Tobkin S., Signorile J.F. (2007) Scapular stabilizer activity during Bodyblade, cuff weights, and Thera-Band use. Journal of Sport Rehabilitation 16, 50-67. [DOI] [PubMed] [Google Scholar]
- Luo J., McNamara B., Moran K. (2005) The use of vibration training to enhance muscle strength and power. Sports Medicine 35, 23-41. [DOI] [PubMed] [Google Scholar]
- Magarey M.E., Jones M.A. (2003) Dynamic evaluation and early management of altered motor control around the shoulder complex. Manual Therapy 8, 195-206. [DOI] [PubMed] [Google Scholar]
- Matias R., Pascoal A.G. (2006) The unstable shoulder in arm elevation: a three-dimensional and electromyographic study in subjects with glenohumeral instability. Clinical Biomechanics 21 Suppl 1, S52-58. [DOI] [PubMed] [Google Scholar]
- Moreside J.M., Vera-Garcia F.J., McGill S.M. (2007) Trunk muscle activation patterns, lumbar compressive forces, and spine stability when using the bodyblade. Physical Therapy 87, 153-163. [DOI] [PubMed] [Google Scholar]
- Neumann D.A. (2002) Kinesiology of the musculoskeletal system : foundations for physical rehabilitation. 1st edition St. Louis: Mosby. [Google Scholar]
- O’Sullivan C., Bentman S., Bennett K., Stokes M. (2007) Rehabilitative ultrasound imaging of the lower trapezius muscle: technical description and reliability. Journal of Orthopaedic & Sports Physical Therapy 37, 620-626. [DOI] [PubMed] [Google Scholar]
- O’Sullivan C., Meaney J., Boyle G., Gormley J., Stokes M. (2009) The validity of Rehabilitative Ultrasound Imaging for measurement of trapezius muscle thickness. Manual Therapy 14, 572-578. [DOI] [PubMed] [Google Scholar]
- Parry J.S., Straub R., Cipriani D.J. (2012) Shoulder- and back-muscle activation during shoulder abduction and flexion using a Bodyblade Pro versus dumbbells. Journal of sport rehabilitation 21, 266-272. [DOI] [PubMed] [Google Scholar]
- Roy J.S., MacDermid J.C., Orton B., Tran T., Faber K.J., Drosdowech D., Athwal G.S. (2009) The concurrent validity of a hand-held versus a stationary dynamometer in testing isometric shoulder strength. Journal of Hand Therapy 22, 320-326; 327. [DOI] [PubMed] [Google Scholar]
- Sanchez-Zuriaga D., Vera-Garcia F.J., Moreside J.M., McGill S.M. (2009) Trunk muscle activation patterns and spine kinematics when using an oscillating blade: influence of different postures and blade orientations. Archives of Physical Medicine and Rehabilitation 90, 1055-1060. [DOI] [PubMed] [Google Scholar]
- Schneebeli A., Egloff M., Giampietro A., Clijsen R., Barbero M. (2014) Rehabilitative ultrasound imaging of the supraspinatus muscle: Intra- and interrater reliability of thickness and cross-sectional area. Journal of Bodywork and Movement Therapies 18, 266-272. [DOI] [PubMed] [Google Scholar]
- Schulte R., Warner C. (2001) Oscillatory devices accelerate proprioception training. Clin Biomech 6, 85-91. [Google Scholar]
- Shinohara M. (2005) Effects of prolonged vibration on motor unit activity and motor performance. Medicine & Science in Sports & Exercise 37, 2120-2125. [DOI] [PubMed] [Google Scholar]
- Solem-Bertoft E., Thuomas K.A., Westerberg C.E. (1993) The influence of scapular retraction and protraction on the width of the subacromial space. An MRI study. Clinical Orthopaedics and Related Research 99-103. [PubMed] [Google Scholar]
- Sugimoto D., Blanpied P. (2006) Flexible foil exercise and shoulder internal and external rotation strength. Journal of Athletic Training 41, 280-285. [PMC free article] [PubMed] [Google Scholar]
- Talbott N.R., Witt D.W. (2013) Ultrasound imaging of the serratus anterior muscle at rest and during contraction. Clinical Physiology and Functional Imaging 33, 192-200. [DOI] [PubMed] [Google Scholar]
- Talbott N.R., Witt D.W. (2014) Ultrasound examination of the serratus anterior during scapular protraction in asymptomatic individuals: reliability and changes with contraction. PM&R 6, 227-234. [DOI] [PubMed] [Google Scholar]
- Teyhen D., Koppenhaver S. (2011) Rehabilitative ultrasound imaging. Journal of Physiotherapy 57, 196. [DOI] [PubMed] [Google Scholar]
- Verschueren S.M., Roelants M., Delecluse C., Swinnen S., Vanderschueren D., Boonen S. (2004) Effect of 6-month whole body vibration training on hip density, muscle strength, and postural control in postmenopausal women: a randomized controlled pilot study. Journal of Bone and Mineral Research 19, 352-359. [DOI] [PubMed] [Google Scholar]
- Wilk K.E., Arrigo C. (1993) Current concepts in the rehabilitation of the athletic shoulder. Journal of Orthopaedic & Sports Physical Therapy 18, 365-378. [DOI] [PubMed] [Google Scholar]
- Yasuda T., Fujita S., Ogasawara R., Sato Y., Abe T. (2010) Effects of low-intensity bench press training with restricted arm muscle blood flow on chest muscle hypertrophy: a pilot study. Clinical Physiology and Functional Imaging 30, 338-343. [DOI] [PubMed] [Google Scholar]
- Yoo W.G. (2014) Effect of Exercise Speed and Isokinetic Feedback on the Middle and Lower Serratus Anterior Muscles during Push-up Exercises. Journal of Physical Therapy Science 26, 645-646. [DOI] [PMC free article] [PubMed] [Google Scholar]


