Adaptive resistance mediated by inhibitory ligands such as PD-L1 has emerged as an important mechanism of malignant cell survival and spurred the development of new agents that disrupt the PD-L1/PD-1 immune checkpoint.1 Analysis of patient specimens from clinical trials of novel immune checkpoint inhibitors indicates that high basal expression of PD-L1 on tumor cells may predict sensitivity to and be necessary to elicit significant clinical benefit from this drug class.2, 3 These data suggest that strategies that increase PD-L1 levels could potentially prime malignant cells with low PD-L1 expression and render them sensitive to anti-PD-1/PD-L1 blockade. In order to investigate this possibility, we first conducted an analysis of basal PD-L1 transcript levels in multiple myeloma (MM) patients (n = 351) from the total therapy 2 (TT2) trial. These analyses demonstrated that expression is very heterogeneous amongst MM patients and that MM patients as a group do not significantly overexpress PD-L1 compared to normal plasma cells (Supplementary Figure 1). Consistent with the low basal PD-L1 expression we identified, significant clinical responses were not observed in any MM patients in a phase I study of nivolumab in patients with relapsed/refractory lymphoid malignancies.4
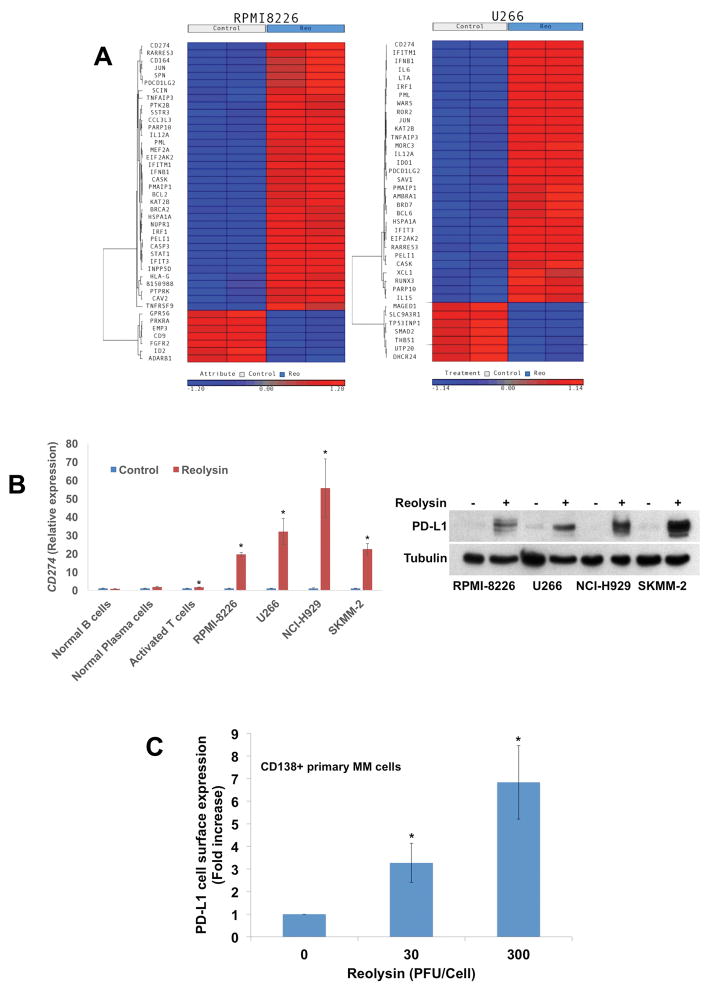
The oncolytic reovirus-based anticancer agent Reolysin is known to have significant immunomodulatory effects and has demonstrated promising preclinical efficacy in MM models and favorable safety and tolerability in early MM clinical trials.5–7 We hypothesized that Reolysin treatment could be used as a precision priming strategy to potentiate the anti-MM efficacy of PD-1/PD-L1 targeted therapy by promoting myeloma immune recognition and PD-L1 upregulation. To test this possibility, we infected a panel of MM cell lines and normal B, plasma, and activated T cells with 30 PFU/cell Reolysin for 48h. Reolysin treatment produced significant and selective reovirus replication in MM cell lines, but not in normal B cells (Supplementary Figure 2 and Supplementary Methods). Expression profiling analyses of U266 and RPMI-8226 cells demonstrated that Reolysin treatment induced a dramatic increase in CD274 (PD-L1) levels (Figure 1A). Quantitative RT-PCR (qRT-PCR) analyses of MM cell lines, normal B, plasma, and activated T cells treated with Reolysin revealed a significant and selective induction of PD-L1 in MM cell lines (Figure 1B). The results were confirmed by immunoblotting in MM cell lines (Figure 1B). Reolysin also upregulated PD-L2 expression in a manner that mirrored PD-L1, albeit to a lesser extent than PD-L1 induction (Supplementary Figures 3A–B). Importantly, flow cytometric analysis showed that Reolysin significantly increased the cell surface expression of PD-L1 in both MM cell lines and primary CD138+ cells from MM patients (Figure 1C, Supplementary Figures 4A–B, and Supplementary Table 1). Since reovirus failed to replicate and induce PD-L1 expression in normal B cells, we investigated whether active reovirus replication was essential for PD-L1 upregulation. A comparison of the anti-MM effects achieved by live reovirus versus UV-inactivated reovirus demonstrated that live reovirus is required to decrease MM cell viability (Supplementary Figure 5A) and upregulate PD-L1 expression (Supplementary Figures 5B–C). PD-L1 levels can be induced by interferon (IFN) exposure. To determine if Reolysin-induced PD-L1 expression was mediated by IFN, we blocked IFNγ using a neutralizing antibody, which significantly reduced Reolysin-mediated PD-L1 upregulation (Supplementary Figure 6). This study reveals that the IFNγ/JAK/STAT axis primarily regulates PD-L1 expression in response to Reolysin. Collectively, our data demonstrate proof of concept that reovirus infection and replication in MM cells can efficiently and selectively upregulate PD-L1 levels in malignant cells with low target expression.
Figure 1. Oncolytic reovirus increases PD-L1 expression in MM cell lines, primary patient specimens, and a xenograft model of MM.
(A) Reolysin treatment upregulates CD274 (PD-L1) and anti-viral response genes. RPMI-8226 and U266 MM cells were treated with 300 PFU/cell Reolysin for 48h. Gene expression changes were determined using Affymetrix expression arrays. Genes with 10-fold or greater induction/repression are illustrated in the heat maps. (B) Reolysin selectively induces CD274 (PD-L1) expression in MM cell lines. MM, normal B and plasma cells, and activated T cells were treated with 30 PFU/cell Reolysin for 48h and CD274 (PD-L1) levels were measured by qRT-PCR and immunoblotting. Mean ± SD, n = 3. *Denotes a significant difference compared to controls, p < 0.05. (C) Reolysin promotes PD-L1 upregulation in CD138+ primary cells from MM patients. CD138+ cells from MM patients were treated with 30 and 300 PFU/cell Reolysin for 24h. PD-L1 surface expression was measured by flow cytometry. Mean ± SD, n = 5. *Indicates a significant difference compared to controls, p < 0.05.
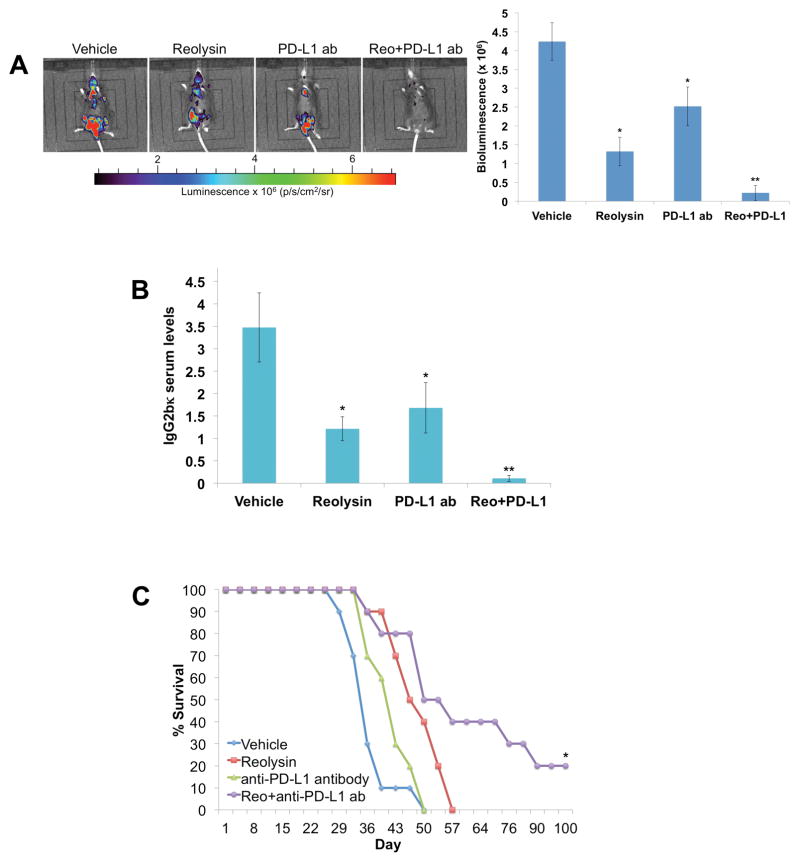
We next conducted a xenograft study to investigate the therapeutic potential of Reolysin-based PD-L1 expression priming in vivo. Reolysin treatment produced significant anti-myeloma activity against RPMI-8226 xenografts (Supplementary Figure 7A) and promoted in vivo viral replication in tumors (Supplementary Figure 7B). Consistent with our in vitro findings, reovirus infection induced a significant increase in PD-L1 levels in RPMI-8226 xenografts (Supplementary Figure 7C). To further evaluate the immune priming effects of Reolysin in an immunocompetent system, we utilized the 5TGM1-luc syngeneic MM bone disease mouse model, which produces lesions throughout the mouse skeleton, replicates many other clinical, cytogenetic, histologic, and molecular features of human MM, and secretes IgG2bκ immunoglobulin.5, 8 In agreement with our human MM cell line data, in vitro treatment of murine 5TGM1 cells with Reolysin robustly increased PD-L1 expression (Supplementary Figure 8A). As expected, IV injection of 5TGM1-luc cells efficiently homed to the skeletons of mice (Figure 2A, far left). Preliminary therapeutic scheduling studies revealed that pre-treatment with Reolysin followed by anti-PD-L1 therapy demonstrated superior efficacy compared to simultaneous co-administration. The pre-treatment with Reolysin is required in order to allow sufficient time for oncolytic reovirus to replicate inside MM cells and subsequently increase PD-L1 expression. We therefore treated mice once a week with Reolysin (5 x 108 TCID50, IV) for 3 weeks (D1, D7, and D14) followed by anti-PD-L1 antibody (200 μg/mouse, IP) every other day for 8 treatments beginning on D15. Single agent therapy with Reolysin or murine anti-PD-L1 antibody significantly reduced skeletal tumor burden (Figure 2A). Notably, Reolysin pre-treatment strongly improved the anti-myeloma efficacy of anti-PD-L1 therapy as bioluminescent quantification of MM disease showed near complete resolution of the skeletal tumor burden in mice treated with the combination of Reolysin and anti-PD-L1 antibody therapy (Figure 2A, far right). In addition, measurement of IgG2bκ levels in mouse serum by ELISA demonstrated a potent (>95%) reduction in M protein levels by combination therapy further illustrating the promising activity of this therapeutic approach (Figure 2B). Analysis of bone marrow samples collected from Reolysin treated mice by qRT-PCR detected a significant increase in CD274 (PD-L1) expression (Supplementary Figure 8B). Importantly, dual treatment with Reolysin and anti-PD-L1 antibody resulted in a significant increase in overall animal survival including several mice with sustained disease regression (Figure 2C). In agreement with several clinical trials that have reported no serious adverse toxicities associated with Reolysin alone or in combination with chemotherapy, no significant signs of toxicity or animal weight loss were observed in any of the treatment groups (Supplementary Figure 9). Our results show for the first time that the combination of Reolysin and anti-PD-L1 antibody therapy is highly effective in a syngeneic mouse model of MM that mimics many of the hallmark features of MM pathogenesis.
Figure 2. Oncolytic reovirus augments the in vivo anti-myeloma activity of anti-PD-L1 antibody therapy in the 5TGM1-luc syngeneic MM bone disease mouse model.
(A) Reolysin and anti-PD-L1 antibody cooperate to reduce MM bone disease. 1 x 106 5TGM1-luc cells were injected IV into C57BL/KaLwRijHsd mice. Bone disease was allowed to establish for 7 days, mice were randomized by equivalent disease (bioluminescence), and were then treated with vehicle (PBS, isotype control antibody), 5 x 108 TCID50 Reolysin IV once a week for 3 weeks (D1, D7, D14), 200 μg/mouse anti-PD-L1 antibody IP every other day for a total of 8 treatments starting D15 or the combination. 24h after the last treatment, mice were imaged using the Xenogen animal imaging system. Each group contained 10 animals and a representative image from each group is shown. Bioluminescence was quantified as a measure of MM disease using Living Image software from 10 mice/group. Mean ± SD. *Indicates a significant difference compared to controls or **either single agent treatment, p < 0.05. (B) Determination of M protein levels. 24h after the last treatment, serum samples were collected from 3 mice/group and IgG2bκ levels were measured by ELISA as an additional measure of MM disease burden. Mean ± SD. *Indicates a significant difference compared to controls or **single agent treatments, p < 0.05. (C) Reolysin and anti-PD-L1 therapy extends overall survival in mice with 5TGM1-luc MM bone disease. Mice were treated with vehicle, Reolysin, anti-PD-L1 antibody, or the combination as described above. Animals were monitored twice weekly for distress. *Denotes a significant difference compared to vehicle or single agent treatment groups, p < 0.01.
Preliminary results of a phase I study of nivolumab as a single agent in patients with relapsed/refractory lymphoid malignancies did not demonstrate significant efficacy in patients with MM.4 However, preclinical and phase 1 studies targeting PD-1 in combination with lenalidomide have shown significant activity.9–12 These findings suggest that immune checkpoint blockade in MM may be most effective in combination with agents that increase MM tumor immunogenicity. Measurement of the levels of PD-L1 in MM patients has produced varied results with some studies finding significant expression and others finding low levels.13–15 In our study, we found that PD-L1 was expressed on MM cells, but was not significantly upregulated compared to normal plasma cells, albeit with considerable variability among patients. Since PD-L1 expression has been identified as a potential predictive biomarker of PD-L1/PD-1 therapy, many MM patients with low PD-L1 expression may not benefit from targeting the PD-L1/PD-1 axis with monotherapy.
With the use of the fully immunocompetent 5TGM1-luc MM bone disease mouse model, we demonstrated that anti-PD-L1 antibody therapy displayed very modest single agent activity. It is notable that 5TGM1 MM cells express low but detectable basal levels of PD-L1, which may explain the partial response in the animal study. Importantly, reovirus infection was able to dramatically upregulate PD-L1 expression and lead to significantly greater efficacy of anti-PD-L1 therapy in this model including several mice with complete responses.
While we show that Reolysin strongly upregulates PD-L1 expression in MM cell lines and primary patient specimens, it is important to note that Reolysin is also able to increase PD-L1 expression in other hematological and solid tumor types that are susceptible to oncolytic reovirus infection and replication (data not shown). Therefore, this therapeutic approach could have immediate and broad clinical applications against a diverse array of malignancies. Collectively, we provide the framework for clinical testing of the combination of Reolysin and PD-1/PD-L1 targeted therapy for patients with MM. These findings demonstrate proof of concept that oncolytic reovirus immune priming is a novel precision approach to selectively induce upregulation of PD-L1 in malignant cells and sensitize cancer cells with low basal PD-L1 expression to anti-PD-1/PD-L1 antibody therapy.
Supplementary Material
Acknowledgments
This project was supported by grants from the National Cancer Institute (R01CA190789 to STN and R01CA172443 to JSC) and the University of Arizona Cancer Center Support Grant P30CA023074.
Footnotes
Conflicts of interest
The authors declare no competing financial interests.
Author contributions
K.R.K. performed experiments, analyzed and interpreted data, and wrote the manuscript; C.M.E., W.Z., K.W., and C.M.C. performed experiments, analyzed and interpreted data and participated in manuscript preparation; F.A., V.V., and J.S.C. contributed to data interpretation and manuscript preparation; S.T.N. designed the study, analyzed and interpreted data, performed experiments, and wrote the manuscript. All authors approved the manuscript before submission.
Supplementary methods and data are available on the Leukemia website (http://www.nature.com/leu).
References
- 1.Tumeh PC, Harview CL, Yearley JH, Shintaku IP, Taylor EJ, Robert L, et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014 Nov 27;515(7528):568–571. doi: 10.1038/nature13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015 May 21;372(21):2018–2028. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 3.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012 Jun 28;366(26):2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lesokhin AM, Ansell SM, Armand P, Scott EC, Halwani A, Gutierrez M, et al. Nivolumab in Patients With Relapsed or Refractory Hematologic Malignancy: Preliminary Results of a Phase Ib Study. J Clin Oncol. 2016 Aug 10;34(23):2698–2704. doi: 10.1200/JCO.2015.65.9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kelly KR, Espitia CM, Mahalingam D, Oyajobi BO, Coffey M, Giles FJ, et al. Reovirus therapy stimulates endoplasmic reticular stress, NOXA induction, and augments bortezomib-mediated apoptosis in multiple myeloma. Oncogene. 2012 Jun 21;31(25):3023–3038. doi: 10.1038/onc.2011.478. [DOI] [PubMed] [Google Scholar]
- 6.Kelly KR, Espitia CM, Zhao W, Wendlandt E, Tricot G, Zhan F, et al. Junctional adhesion molecule-A is overexpressed in advanced multiple myeloma and determines response to oncolytic reovirus. Oncotarget. 2015 Dec 01;6(38):41275–41289. doi: 10.18632/oncotarget.5753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sborov DW, Nuovo GJ, Stiff A, Mace T, Lesinski GB, Benson DM, Jr, et al. A phase I trial of single-agent reolysin in patients with relapsed multiple myeloma. Clin Cancer Res. 2014 Dec 1;20(23):5946–5955. doi: 10.1158/1078-0432.CCR-14-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oyajobi BO, Munoz S, Kakonen R, Williams PJ, Gupta A, Wideman CL, et al. Detection of myeloma in skeleton of mice by whole-body optical fluorescence imaging. Mol Cancer Ther. 2007 Jun;6(6):1701–1708. doi: 10.1158/1535-7163.MCT-07-0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Badros AZKMMN, Rapoport AP, Lederer E, Philip S, Lesho P, Dell C, Hardy NM, Yared J, Goloubeva O, Singh Z. A Phase II Study of Anti PD-1 Antibody Pembrolizumab, Pomalidomide and Dexamethasone in Patients with Relapsed/Refractory Multiple Myeloma (RRMM) Blood. 2015;126:506. [Google Scholar]
- 10.Benson DM, Jr, Bakan CE, Mishra A, Hofmeister CC, Efebera Y, Becknell B, et al. The PD-1/PD-L1 axis modulates the natural killer cell versus multiple myeloma effect: a therapeutic target for CT-011, a novel monoclonal anti-PD-1 antibody. Blood. 2010 Sep 30;116(13):2286–2294. doi: 10.1182/blood-2010-02-271874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorgun G, Samur MK, Cowens KB, Paula S, Bianchi G, Anderson JE, et al. Lenalidomide Enhances Immune Checkpoint Blockade-Induced Immune Response in Multiple Myeloma. Clin Cancer Res. 2015 Oct 15;21(20):4607–4618. doi: 10.1158/1078-0432.CCR-15-0200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miguel JS, MMSJ, Ocio EM, Rodriguez-Otero P, Reece D, Munshi NC, Avigan DE, Ge Y, Balakumaran A, Marinello P, Orlowski RZ, Siegel DS. Pembrolizumab in Combination with Lenalidomide and Low-Dose Dexamethasone for Relapsed/Refractory Multiple Myeloma (RRMM): Keynote-023. Blood. 2015;126:505. [Google Scholar]
- 13.Liu J, Hamrouni A, Wolowiec D, Coiteux V, Kuliczkowski K, Hetuin D, et al. Plasma cells from multiple myeloma patients express B7-H1 (PD-L1) and increase expression after stimulation with IFN-{gamma} and TLR ligands via a MyD88-, TRAF6-, and MEK-dependent pathway. Blood. 2007 Jul 01;110(1):296–304. doi: 10.1182/blood-2006-10-051482. [DOI] [PubMed] [Google Scholar]
- 14.Ray A, Das DS, Song Y, Richardson P, Munshi NC, Chauhan D, et al. Targeting PD1-PDL1 immune checkpoint in plasmacytoid dendritic cell interactions with T cells, natural killer cells and multiple myeloma cells. Leukemia. 2015 Jun;29(6):1441–1444. doi: 10.1038/leu.2015.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tamura H, Ishibashi M, Yamashita T, Tanosaki S, Okuyama N, Kondo A, et al. Marrow stromal cells induce B7-H1 expression on myeloma cells, generating aggressive characteristics in multiple myeloma. Leukemia. 2013 Feb;27(2):464–472. doi: 10.1038/leu.2012.213. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.