Abstract
Objectives. To evaluate whether a public program providing long-acting reversible contraceptive (LARC) methods free of charge increases the LARC initiation rate and reduces the unintended pregnancy rate in the general population.
Methods. Since 2013, all women in Vantaa, Finland, have been entitled to 1 LARC method free of charge. With time-series analysis between 2000 and 2015, we assessed whether this public program was associated with changes in steady-state mean rates of LARC initiation and abortions.
Results. The initiation rate of LARCs (1/1000 women) increased 2.2-fold from 1.9 to 4.2 after the intervention (P < .001). Concomitantly, the abortion rate (1/1000 women) declined by 16% from 1.1 to 0.9 in the total sample (P < .001), by 36% from 1.3 to 0.8 among those aged 15 to 19 years (P < .001), and by 14% from 2.0 to 1.7 among those aged 20 to 24 years (P = .01).
Conclusions. The LARC program was associated with increased uptake of LARC methods and fewer abortions in the population.
Public Health Implications. Entitling the population to LARC methods free of charge is an effective means to reduce the unmet need of contraception and the need for abortion, especially among women younger than 25 years.
Of all pregnancies worldwide, 40% are unintended, and among women aged 15 to 19 years in the United States, up to 75% of the pregnancies are unintended.1,2 Half of all unintended pregnancies lead to an induced abortion (hereafter abortion),3 but unintended and adolescent pregnancy are also associated with several adverse outcomes for both mother and child.4–6 The most effective reversible method of preventing unintended and adolescent pregnancy are the long-acting reversible contraceptive (LARC) methods (i.e., intrauterine devices and contraceptive implants).7,8 These methods are no more expensive than short-acting methods over the long run,9 but the high up-front costs are considered a barrier to the initiation of LARC methods.10,11 In a recent study, public funding for contraception was associated with an increased LARC initiation rate.12 Therefore, providing LARC methods free of charge is potentially an effective way of increasing LARC initiation and reducing unintended pregnancy.
Several international family planning organizations have recommended LARC methods as first-line contraceptives for both adults and adolescents,13,14 and policies that reduce their up-front costs have been advocated.15,16 Indeed, providing contraceptive methods at no cost was shown to increase use of LARC methods in a selected study sample.17 However, when the Affordable Care Act reduced cost sharing for contraceptive methods, there was no significant increase in LARC use at 1-year follow-up.18 Because the evidence is limited and mixed, more information is needed to determine whether a public intervention providing LARC methods free of charge increases their uptake in a general population and, more important, decreases the rate of unintended pregnancy.
In the city of Vantaa, Finland, located in the Helsinki metropolitan area, all women have been entitled to their first LARC method free of charge since January 1, 2013. The introduction of this public program offered a unique setting to study the effects of providing LARC methods free of charge at the population level. We hypothesized that such a public LARC program increases the initiation rate and thereby better meets the family planning needs in the population. As information on unintended pregnancy is scarce, we used the abortion rate in the population as a proxy for unintended pregnancy.
METHODS
Vantaa is the fourth-largest city in Finland, with approximately 210 000 inhabitants and 42 000 women aged 15 to 44 years. Vantaa has provided public family planning services at specialized clinics since 1975. At these clinics, all visits are free of charge, and the service is available for all residents of Vantaa. When the LARC program was launched in 2013, all other services remained unchanged. The public family planning clinics are well known and frequently used, especially by young women. In 2014, 1 out of 4 women aged 15 to 24 years visited a public family planning clinic (1400 visitors aged 15–19 years of 6000 women in this age group, and 2100 visitors aged 20–24 years of 6800 women). The service covers contraceptive counseling; initiation and removal of LARC methods; referral for abortion, sterilization, and infertility; counseling on sexuality; and diagnostics and treatment of sexually transmitted infections. The employees are general practitioners and health care professionals with special education and experience in the field. Abortion care is provided mainly by the Helsinki University Hospital (> 95%; https://www.thl.fi/fi/tilastot/tilastot-aiheittain/seksuaali-ja-lisaantymisterveys/raskaudenkeskeytykset/raskaudenkeskeytykset). Abortion-related hospital visits are subsidized but not completely free; the mean price for an abortion-related outpatient visit is around 33€ ($37).
Study Design
In this population-based quasi-experimental study, we used interrupted time series methods and high-quality data derived from the Finnish national registers to investigate the effects of a public LARC program. The program was designed to reach all women equally, without targeting risk groups, although it was only offered to women who had not previously used LARC methods. No investment in campaigning was made to raise awareness of this public program, but women were informed of the new benefit at counseling visits.
The primary outcome measure was the monthly abortion rate per 1000 women aged 15 to 44 years, and the secondary outcome measure was the monthly initiation rate of LARC methods per 1000 women aged 15 to 44 years. We stratified our data into 3 age groups (15–19, 20–24, and 25–44 years), to explicitly evaluate the effect of the intervention on abortions among adolescents (aged 15–19 years) and young adults (aged 20–24 years). We used the abortion rate from a neighboring municipality, Espoo, to control for unrelated factors that might have affected the abortion rate concurrently with the intervention.19 Both Espoo and Vantaa reside in the Helsinki metropolitan area and are simultaneously influenced by changes in the region. Espoo had no free-of-charge LARC program at the time of this study.
Data
Our time series spanned 192 months, from January 2000 to December 2015. It has 156 time points before and 36 time points after initiation of the intervention on January 1, 2013. All data were gathered continuously and independently of our research question. We obtained data on monthly abortions from the Register on Induced Abortions, which is maintained by the National Institutes of Health and Welfare in Finland. All hospitals that provide abortion care must report abortions to the register on a continuous basis, within 30 days after the abortion. Reporting is mandatory and based on law (https://www.thl.fi/en/web/thlfi-en/statistics/information-on-statistics/description-of-statistics/induced-abortions).
Each LARC initiation at the public family planning clinics is registered in Vantaa’s electronic health records. These data are reliable, as general practitioners receive a pay supplement for each recorded LARC insertion. This supplement has been in use from the early 2000s and throughout the study period. No private clinics provide LARC methods free of charge, and LARC initiations at private clinics were not included in this study.
As covariates, we included the abortion rate in Espoo, the unemployment rate among women in Vantaa, the proportion of women in Vantaa with no education beyond elementary school (i.e., first to ninth grade), and the proportion of the population in each age group in Vantaa living in households belonging to the lowest income decile, to control for poor education and low socioeconomic status. We obtained these data on the aggregated level from Statistics Finland (http://www.tilastokeskus.fi). Other known risk factors for abortion, such as marital status, parity, and previous abortions were not available on the aggregated level and hence were not included.
Economic Aspects
This population-based intervention was carried out in a single-payer system. After establishing that there was no change in birth rates over the sample period, we compared the costs of the LARC methods provided (i.e., the additional outlays they entailed for the public clinics) with the savings, directly attributable to averted abortions. We obtained the number of LARC methods and their price from the Central Hospital Pharmacy (104€ per method, 3398 methods). Of all abortions in Finland, 90% are medically induced, and we obtained the mean price of 1 such abortion (991€) from the national report on public medical costs in Finland. We included only direct costs of LARC methods and estimated savings from averted abortions. We did not include any further cost or savings.
Statistical Analysis
As a precursory analysis, we computed descriptive difference-in-difference estimates from the mean monthly abortions in Vantaa and Espoo, 3 years before (2010–2012) and after (2013–2015) the start of the LARC program in Vantaa.
For the main analysis, we applied time-series methods to study specific time-dependent properties of LARC initiations and abortions. Time-series methods are widely used and recommended when one is analyzing public health interventions, as these methods permit taking the preintervention level and trend into account when comparing the outcome measures between different time periods.20–23 To optimize causal inference, we tested our hypothesis in 3 steps, as shown in Figure A, available as a supplement to the online version of this article at http://www.ajph.org. First, by using a controlled interrupted time series design, we assessed whether the long-run mean properties of the LARC initiation rate time series changed following the introduction of the program and with control for confounding factors. Second, we repeated the analysis for the abortion rate time series, additionally controlling for the abortion rate time series in Espoo. In our third step, we analyzed the relationship between the LARC initiation rate and the abortion rate in Vantaa, adjusting for confounders. We also conducted a cobreaking test to explore whether the LARC uptake mediated the effect of the intervention on the abortion rate.24
We used linear regression coupled with mean shifts and explicit time dependence. To capture possible breaks and trends in the data, other than those induced by the intervention, we allowed for stochastic trends21,25 by including autoregressive terms as additional regressors. Using autoregressive terms is a convenient way of correcting for serial correlation (i.e., when the outcome at 1 time point is correlated to the outcome at 1 or more preceding time points). Moreover, autoregressive terms explicitly capture transition dynamics from one steady state to another without necessitating deterministic trends, such as changes in slope. In all 3 steps, we estimated the step change by the difference in steady-state means before and after the intervention. A drawback is that Poisson regression, which is appropriate for count data, is not easily adapted to time series applications.26 We relied on the normal distribution instead. The Appendix, available as a supplement to the online version of this article at http://www.ajph.org, presents a detailed description of the methods used, including discussion on distributional assumptions.
We used an indicator variable for the intervention time point to model breaks in the mean. We assumed that the intervention had an immediate effect on the LARC initiation rate and a delayed effect on the abortion rate. We considered lags of up to a year of the intervention variable in the model for abortion rate and chose the lag length that optimized the fit, which turned out to be 3 months. As a precautionary measure, we tried leads of up to a year, but this only reduced the fit. In our full regression model (steps 1 and 2 in Figure A) we included the abortion rate in Vantaa; the intervention indicator (at the precise time point in step 1 and at 3 months after the true intervention in step 2); the covariates of education, unemployment, low income, and the abortion rate in Espoo (in step 2); and 12 lags of each variable and seasonal dummy variables to adjust for monthly variation. As it was difficult to form a precise a priori theory for the lag structure, we used automatic model selection to obtain a parsimonious model from the initially overparameterized system.27 The final selected confounding variables for each model are presented in the supplemental Appendix.
To assess the connection between the abortion rate and the LARC initiation rate, we included the initiation rate as an explanatory variable in our third step. Given the possible time lags between the LARC initiation and its effect on abortion, as well as possible serial correlation, we again included 12 lags of all variables in the model. In a consistency check, formally known as a cobreaking test,24 we re-entered the indicator variable and tested the null hypothesis that its coefficient was undistinguishable from zero. If the step increase in the initiation rate associated with the intervention was the underlying cause for the downward shift in the abortion rate, the indicator variable would no longer be significant in this model. In this case, a rejection of the null would suggest that other concurrent factors at least in part were responsible of the break in the abortion rate series.
We assessed statistical significance at the 5% level and conducted statistical analyses in OxMetrics version 6.10 (OxMetrics Technologies Limited, Oxford, United Kingdom).
RESULTS
In the descriptive difference-in-difference analysis of abortion rates among women aged 15 to 44 years, we found a significant negative result indicating a larger decrease in mean monthly abortion rate in Vantaa than in Espoo (–0.11; SD = 0.05; P = .03). We also found that the variance of the abortion rate time series changed at the time of the intervention (0.04 vs 0.02), but there was no evidence of autoregressive conditional heteroscedasticity within the 2 regimes. Otherwise, the 2 municipalities showed similar developments regarding the covariates (unemployment, low income, elementary education) during the 3 years before and after the intervention (Table 1). Birth rates in both municipalities were stable and stationary throughout the study period.
TABLE 1—
Descriptive Characteristics of Women 3 Years Before and 3 Years After the Introduction of the Long-Acting Reversible Contraceptive Program in January 2013: Vantaa and Espoo, Finland
| Vantaa (Intervention Site) |
Espoo (Comparison Site) |
|||
| Characteristics | 2010–2012, No. (%) | 2013–2015, No. (%) | 2010–2012, No. (%) | 2013–2015, No. (%) |
| No. of womena | ||||
| Aged 15–19 y | 6 343 | 6 491 | 7 945 | 7 738 |
| Aged 20–24 y | 6 491 | 6 811 | 7 502 | 8 043 |
| Aged 25–44 y | 29 109 | 29 823 | 36 865 | 37 815 |
| All (aged 15–44 y) | 41 942 | 42 660 | 52 312 | 53 597 |
| No. of abortions | ||||
| Aged 15–19 y | 275 (4.3) | 188 (3.1) | 240 (3.0) | 169 (2.2) |
| Aged 20–24 y | 450 (6.9) | 420 (6.2) | 412 (5.5) | 390 (4.8) |
| Aged 25–44 y | 926 (3.2) | 839 (2.8) | 914 (2.5) | 981 (2.6) |
| All (aged 15–44 y) | 1 651 (3.9) | 1 451 (3.4) | 1 566 (3.0) | 1 540 (2.9) |
| No. of births | ||||
| Aged 15–19 y | 129 (2.0) | 110 (1.8) | 131 (1.6) | 126 (1.6) |
| Aged 20–24 y | 890 (13.7) | 892 (13.1) | 1 103 (14.7) | 996 (12.4) |
| Aged 25–44 y | 9 064 (31.1) | 8 707 (29.2) | 6 552 (17.7) | 6 483 (17.1) |
| All (aged 15–44 y) | 10 083 (24.0) | 9 709 (22.8) | 7 756 (14.8) | 7 605 (14.2) |
| No. of LARC initiations in Vantaa | ||||
| Aged 15–19 y | 117 (1.8) | 415 (6.9) | . . . | . . . |
| Aged 20–24 y | 357 (5.5) | 983 (14.4) | . . . | . . . |
| Aged 25–44 y | 2 788 (9.6) | 3 986 (13.4) | . . . | . . . |
| All (aged 15–44 y) | 3 256 (7.8) | 5 379 (12.6) | . . . | . . . |
| No. of womena with elementary education only | ||||
| Aged 15–19 y | 5 517 (87.0) | 5 191 (86.2) | 6 810 (85.7) | 6 634 (85.7) |
| Aged 20–24 y | 1 633 (25.2) | 1 612 (23.7) | 1 528 (20.4) | 1 652 (20.5) |
| Aged 25–44 y | 4 961 (17.0) | 5 404 (18.1) | 4 741 (12.9) | 5 338 (14.1) |
| All (aged 15–44 y) | 12 111 (28.9) | 12 207 (28.6) | 13 079 (25.0) | 13 624 (25.4) |
| No. of residentsb in the lowest income decile | 12 783 (6.4) | 13 622 (6.6) | 15 190 (6.1) | 17 046 (6.6) |
| No. of unemployed womenc | 3 893 (5.9) | 5 309 (7.9) | 3 398 (4.2) | 5 463 (6.5) |
Note. LARC = long-acting reversible contraceptive.
Mean number of women in the 3-year-intervals.
Mean number of residents in the lowest income decile of the total population, in the 3-year intervals.
Mean number of women aged 18–64 years in the 3-year intervals.
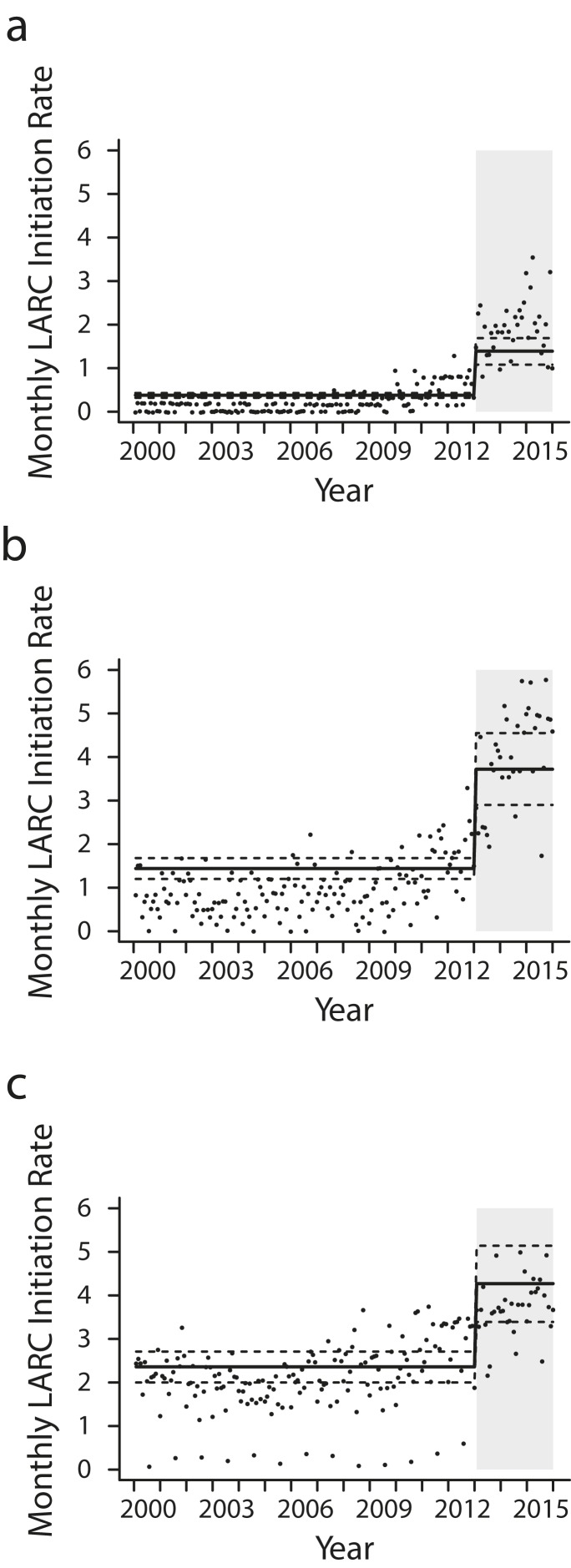
Figure 1 presents the unadjusted time series of the monthly LARC initiation rate, together with the steady-state estimates from the first model (step 1 in Figure A). The mean monthly initiation rate increased in all age groups after the implementation of the intervention (Table 2): almost 4-fold among those aged 15 to 19 years, with a step change of 1.01 more initiations per 1000 women (95% confidence interval [CI] = 0.68, 1.34); almost 2.5-fold among those aged 20 to 24 years (step change of 2.28; 95% CI = 1.38, 3.19); and almost 2-fold among those aged 25 to 44 years (step change of 1.91; 95% CI = 1.10, 2.73).
FIGURE 1—
Crude Monthly Rates of LARC Initiation and Adjusted Regression Estimates Before and After Intervention Among Women Aged (a) 15–19 Years, (b) 20–24 Years, and (c) 25–44 Years: Vantaa, Finland, January 2000–December 2015
Note. LARC = long-acting reversible contraceptive. Rates are per 1000 women. The intervention was in January 2013. The solid black line indicates the regression estimate of the mean before and after the intervention, and the dashed lines indicate the 95% confidence interval. The gray box is the time after the intervention.
TABLE 2—
Regression Estimates of the Monthly Mean Rates of Long-Acting Reversible Contraceptive Initiations and Abortions Before and After the Intervention in January 2013: Vantaa, Finland
| Mean Monthly Ratea |
||||
| Preinterventionb (95% CI) | Postinterventionb (95% CI) | Absolute Step Changeb,c (95% CI) | Rate Ratiod (95% CI) | |
| LARC initiations | ||||
| Aged 15–19 y | 0.38 (0.32, 0.43) | 1.39 (1.08, 1.69) | 1.01 (0.68, 1.34) | 3.67 (2.54, 4.80) |
| Aged 20–24 y | 1.44 (1.20, 1.68) | 3.72 (2.90, 4.55) | 2.28 (1.38, 3.19) | 2.59 (1.81, 3.37) |
| Aged 25–44 y | 2.36 (2.00, 2.71) | 4.27 (3.39, 5.14) | 1.91 (1.10, 2.73) | 1.81 (1.44, 2.18) |
| All (aged 15–44 y) | 1.94 (1.70, 2.18) | 4.20 (3.57, 4.83) | 2.26 (1.71, 2.82) | 2.17 (1.86, 2.47) |
| Abortions | ||||
| Aged 15–19 y | 1.32 (1.26, 1.38) | 0.84 (0.71, 0.97) | −0.48 (−0.61, −0.34) | 0.64 (0.54, 0.74) |
| Aged 20–24 y | 1.99 (1.90, 2.09) | 1.70 (1.50, 1.89) | −0.30 (−0.52, −0.08) | 0.85 (0.74, 0.96) |
| Aged 25–44 y | 0.86 (0.82, 0.89) | 0.80 (0.72, 0.88) | −0.06 (−0.14, 0.03) | 0.94 (0.84, 1.03) |
| All (aged 15–44 y) | 1.10 (1.07, 1.12) | 0.92 (0.87, 0.97) | −0.17 (−0.23, −0.12) | 0.84 (0.79, 0.89) |
Note. CI = confidence interval; LARC = long-acting reversible contraceptive.
Monthly rates per 1000 women in each age group.
Results from the solved steady-state step change model, adjusted for seasonality and selected covariates, with the preintervention period from January 2000 to December 2012 and the postintervention period from January 2013 to December 2015.
The step change is the difference between the post- and preintervention steady-state means.
Confidence intervals for rate ratio based on standard errors calculated by the delta method.
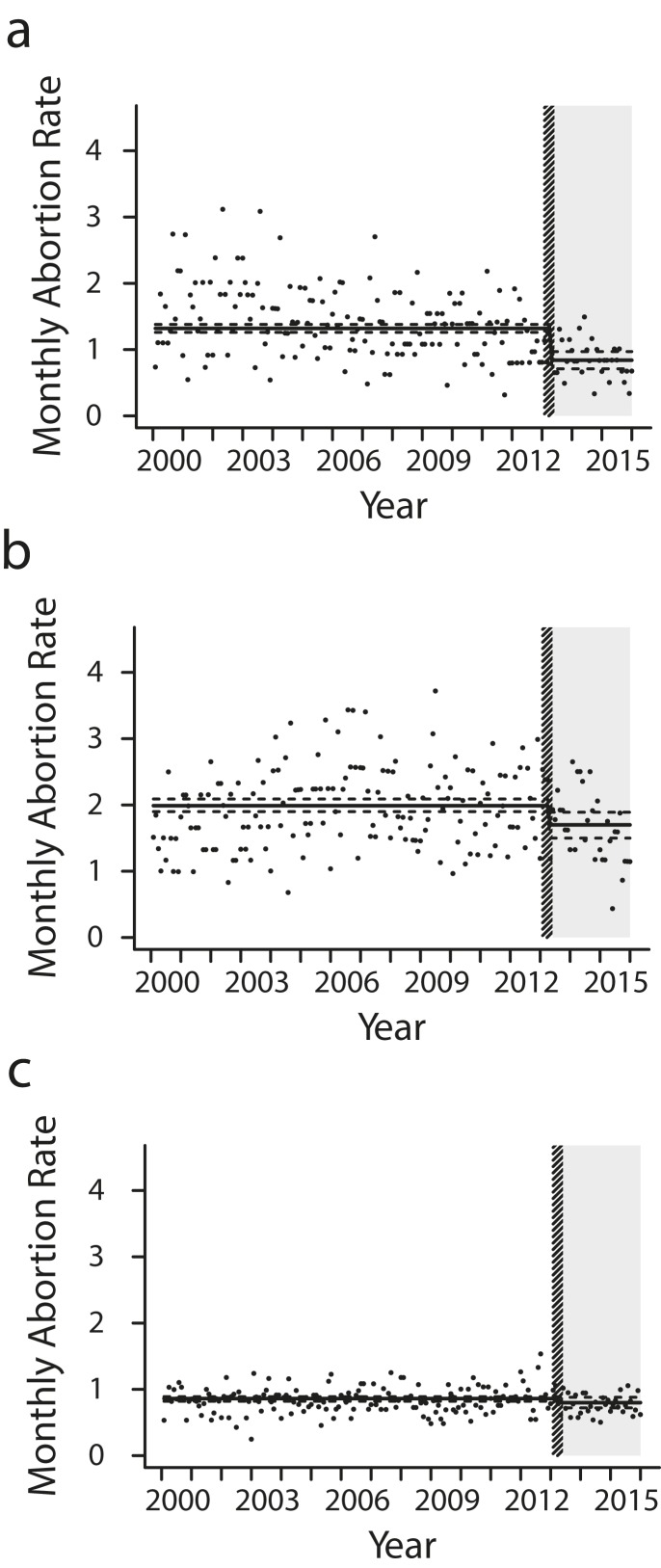
The monthly abortion rate was stable and stationary before the intervention. The results from the second steady-state model (step 2 in Figure A) show a reduction in the mean monthly abortion rate in all age groups after the start of the intervention (Figure 2 and Table 2). Among women aged 15 to 19 years, the mean monthly abortion rate per 1000 women decreased by 36%, from 1.32 to 0.84, with a step change of −0.48 abortions (95% CI = −0.61, −0.34). In the age group of 20 to 24 years, the monthly abortion rate declined by 14% (step change of −0.28; 95% CI = −0.50, −0.06). Among those aged 25 to 44 years, there was a statistically nonsignificant decline of 6% (step change of −0.06; 95% CI = −0.14, 0.03).
FIGURE 2—
Crude Monthly Abortion Rates and Adjusted Regression Estimates Before and After the Intervention Among Women Aged (a) 15–19 Years, (b) 20–24 Years, and (c) 25–44 Years: Vantaa, Finland, January 2000–December 2015
Note. Rates are per 1000 women. The intervention was in January 2013. The solid black line indicates the regression estimate of the mean before and after the intervention, and the dashed lines indicate the 95% confidence interval. The gray box is the time after the intervention. The dashed box indicates the 3-month period of January to March 2013 before the full effect of the intervention on the abortion rate was seen.
In the third model (step 3 in Figure A) of the abortion rate on the LARC initiation rate and the confounding factors, we found a significant negative correlation between increased LARC initiations and abortions in all age groups: among those aged 15 to 19 years (B = −0.24; 95% CI = −0.33, −0.16), 20 to 24 years (B = −0.13; 95% CI = −0.20, −0.07), and 25 to 44 years (B = −0.044; 95% CI = −0.071, −0.016). This implies that the abortion rate decreased when use of efficient contraception methods increased. With the LARC initiation rate as a covariate, the indicator variable was nonsignificant in all age groups (P = .44 for the full sample; 0.44, 0.94, and 0.77 among those aged 15 to 19, 20 to 24, and 25 to 44 years, respectively). Together with the findings in steps 1 and 2 of the analysis, this implies cobreaking between the LARC initiation rate and the abortion rate and, as such, provides evidence that the LARC uptake may be the underlying mediator between the intervention and the subsequent reduction in the rate of abortion.
To describe the economic aspects of the program, we required that the time series of birth rates would remain stable throughout the study period, and that the intervention indicator variable would be nonsignificant when modeling birth rates. As these criteria were met, we compared the costs and spending directly attributed to methods provided and abortions averted. The preliminary yearly net cost of the program was as follows: +25 000€ for those aged 15 to 19 years, +0€ for those aged 20 to 24 years, and −67 000€ for those aged 25 to 44 years.
DISCUSSION
We found that the public free-of-charge LARC program in Vantaa was associated with both an increased initiation of these methods and a reduction in the abortion rate. Finland has a high rate (> 40%) of modern contraceptive use, and the abortion rate is one of the lowest in the developed world (10 abortions per 1000 women aged 15–44 years in 2013).28 Therefore, Finland might not be the most sensitive setting to study the effects of such a program. Nevertheless, the initiation rate of LARC methods increased significantly in all age groups, and the reduction in the abortion rate among young women suggests that there was an unmet need for contraception that the present program was able to meet in part.
Our study adds to the literature by providing estimates on both LARC uptake and abortion rate in the general population. In the CHOICE study performed in the St Louis, Missouri, region in the United States, 75% of the study participants chose a LARC method when contraceptive methods were provided at no cost.29 The abortion rate among the study participants was lower than that at national levels,17 but only limited conclusions for the abortion rate in the population could be drawn from this high-risk study sample. Our results regarding adolescents are also in line with earlier studies. The declining trend in the abortion rate among adolescents in the United Kingdom has been associated with increased LARC usage in the same age group.30
Although the benefits of the public LARC program in Vantaa should not only be evaluated on economic grounds, we find its economic aspects to be promising. Among those aged 15 to 19 years, the estimated resources saved from reduced abortions exceeded the money spent on LARC methods, and among those aged 20 to 24 years, the costs and savings were of equal amounts. This is in line with earlier studies of the cost efficiency of contraceptive methods and public programs.31,32
Strengths and Limitations
The strengths of the study include the use of Finnish administrative data that are of high quality. The register on induced abortions is well validated and a reliable data source on both medical and surgical abortions, also with respect to specific age groups.33 The coverage of public family planning clinic services is high, which improves the generalizability of our results. We derived data on LARC initiations from electronic health records, and there have been no changes in the recording of medical procedures during the study period.
However, because this was an observational study, limitations regarding causal inference need to be considered. To address this, we used interrupted time series, which is considered the strongest quasi-experimental design for estimating intervention effects in nonrandomized settings.34 It has been shown to estimate the effects of interventions in concordance with randomized study designs.35 In addition, instead of assuming linear trends, which have problematic interpretations and predictive properties for ratios and may therefore possibly exaggerate our results, we allowed for stochastic trending that flexibly catches any underlying shifts and trends, and autocorrelation. Specific time-series considerations include that our basic time-series design had only 1 interruption, which made the study vulnerable to the possibility of another concurrent event affecting the time series at hand. Indeed, an overall reduction in the abortion rate has been noted in Finland and elsewhere in recent years. Therefore, we made a great effort to establish the association between the public program and the decline in the abortion rate. The findings from all 3 steps of the analysis supported the hypothesis that the increase in LARC initiations after the intervention was the mediating factor behind the subsequent decline in the abortion rate.
Finally, there were a few limitations with respect to the data and the setting. We lacked data on LARC initiations in Espoo and could hence not use it as a comparison group in the first step of the analysis. Also, we could not control for the possibly diluting effect of in-and-out migration, as approximately 7% of the population in Vantaa moves to or from Vantaa each year. However, we controlled for multiple other variables at the population level and kept the risk of residual confounding to a minimum.
Public Health Implications
Our study demonstrates that providing LARC methods free of charge is associated with an increased initiation of these methods in all age groups. It is also associated with a reduced rate of unintended pregnancies, measured as the number of induced abortions among young women younger than 25 years. Thus, providing LARCs free of charge is an effective means to satisfy, in part, the unmet need of contraception among young women.
ACKNOWLEDGMENTS
This study was supported by research funds from the Hospital District of Helsinki and Uusimaa, Finska Läkaresällskapet, The Finnish Medical Foundation, and Stiftelsen till Dorothea Perklens minne.
Note. The funders/sponsors had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the article; or decision to submit the article for publication.
HUMAN PARTICIPANT PROTECTION
The ethics committee of the Hospital District of Helsinki and Uusimaa approved the study (304/13/03/03/2015). No informed consents were needed as only aggregated data were used in this register-based study.
Footnotes
See also Trussell, p. 435.
REFERENCES
- 1.Sedgh G, Singh S, Hussain R. Intended and unintended pregnancies worldwide in 2012 and recent trends. Stud Fam Plann. 2014;45(3):301–314. doi: 10.1111/j.1728-4465.2014.00393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008–2011. N Engl J Med. 2016;374(9):843–852. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Singh S, Sedgh G, Hussain R. Unintended pregnancy: worldwide levels, trends, and outcomes. Stud Fam Plann. 2010;41(4):241–250. doi: 10.1111/j.1728-4465.2010.00250.x. [DOI] [PubMed] [Google Scholar]
- 4.Institute of Medicine. The Best Intentions: Unintended Pregnancy and the Well-Being of Children and Families. Washington, DC: The National Academies Press; 1995. [PubMed] [Google Scholar]
- 5.Paranjothy S, Broughton H, Adappa R, Fone D. Teenage pregnancy: who suffers? Arch Dis Child. 2009;94(3):239–245. doi: 10.1136/adc.2007.115915. [DOI] [PubMed] [Google Scholar]
- 6.Leppälahti S, Gissler M, Mentula M, Heikinheimo O. Is teenage pregnancy an obstetric risk in a welfare society? A population-based study in Finland, from 2006 to 2011. BMJ Open. 2013;3(8):e003225. doi: 10.1136/bmjopen-2013-003225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winner B, Peipert JF, Zhao Q et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366(21):1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 8.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83(5):397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Trussell J, Hassan F, Lowin J, Law A, Filonenko A. Achieving cost-neutrality with long-acting reversible contraceptive methods. Contraception. 2015;91(1):49–56. doi: 10.1016/j.contraception.2014.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eisenberg D, McNicholas C, Peipert JF. Cost as a barrier to long-acting reversible contraceptive (LARC) use in adolescents. J Adolesc Health. 2013;52(4 suppl):S59–S63. doi: 10.1016/j.jadohealth.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Thompson KM, Speidel JJ, Saporta V, Waxman NJ, Harper CC. Contraceptive policies affect post-abortion provision of long-acting reversible contraception. Contraception. 2011;83(1):41–47. doi: 10.1016/j.contraception.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 12.Thompson KM, Rocca CH, Kohn JE et al. Public funding for contraception, provider training, and use of highly effective contraceptives: a cluster randomized trial. Am J Public Health. 2016;106(3):541–546. doi: 10.2105/AJPH.2015.303001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Committee on Gynecologic Practice Long-Acting Reversible Contraception Working Group. Committee Opinion No. 642: Increasing access to contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2015;126(4):e44–e48. doi: 10.1097/AOG.0000000000001106. [DOI] [PubMed] [Google Scholar]
- 14.Committee on Adolescence. Contraception for adolescents. Pediatrics. 2014;134(4):e1244–e1256. doi: 10.1542/peds.2014-2299. [DOI] [PubMed] [Google Scholar]
- 15.Fox J, Barfield W. Decreasing unintended pregnancy: opportunities created by the Affordable Care Act. JAMA. 2016;316(8):815–816. doi: 10.1001/jama.2016.8800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cleland K, Peipert JF, Westhoff C, Spear S, Trussell J. Family planning as a cost-saving preventive health service. N Engl J Med. 2011;364(18):e37. doi: 10.1056/NEJMp1104373. [DOI] [PubMed] [Google Scholar]
- 17.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120(6):1291–1297. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pace LE, Dusetzina SB, Keating NL. Early impact of the Affordable Care Act on uptake of long-acting reversible contraceptive methods. Med Care. 2016;54(9):811–817. doi: 10.1097/MLR.0000000000000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin; 2002. [Google Scholar]
- 20.Biglan A, Ary D, Wagenaar AC. The value of interrupted time-series experiments for community intervention research. Prev Sci. 2000;1(1):31–49. doi: 10.1023/a:1010024016308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zeger SL, Irizarry R, Peng RD. On time series analysis of public health and biomedical data. Annu Rev Public Health. 2006;27(1):57–79. doi: 10.1146/annurev.publhealth.26.021304.144517. [DOI] [PubMed] [Google Scholar]
- 22.Bernal JL, Cummins S, Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol. 2017;46(1):348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kontopantelis E, Doran T, Springate DA, Buchan I, Reeves D. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750. doi: 10.1136/bmj.h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hendry DF, Massmann M. Co-breaking: recent advances and a synopsis of the literature. J Bus Econ Stat. 2007;25(1):33–51. [Google Scholar]
- 25.Hamilton JD. Time Series Analysis. Princeton, NJ: Princeton University Press; 1994. [Google Scholar]
- 26.Winkelmann R. Counting on Count Data Models. IZA World of Labor; 2015. p. 148. [Google Scholar]
- 27.Hendry DF, Krolzig HM. The properties of automatic GETS modelling. Econ J (Lond) 2005;115(502):C32–C61. [Google Scholar]
- 28.Lindh I, Skjeldestad FE, Gemzell-Danielsson K et al. Contraceptive use in the Nordic countries. Acta Obstet Gynecol Scand. 2017;96(1):19–28. doi: 10.1111/aogs.13055. [DOI] [PubMed] [Google Scholar]
- 29.McNicholas C, Madden T, Secura G, Peipert JF. The contraceptive CHOICE project round up: what we did and what we learned. Clin Obstet Gynecol. 2014;57(4):635–643. doi: 10.1097/GRF.0000000000000070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Connolly A, Pietri G, Yu J, Humphreys S. Association between long-acting reversible contraceptive use, teenage pregnancy, and abortion rates in England. Int J Womens Health. 2014;6:961–974. doi: 10.2147/IJWH.S64431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–161. doi: 10.1016/j.contraception.2012.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Foster DG, Rostovtseva DP, Brindis CD, Biggs MA, Hulett D, Darney PD. Cost savings from the provision of specific methods of contraception in a publicly funded program. Am J Public Health. 2009;99(3):446–451. doi: 10.2105/AJPH.2007.129353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Heino A, Niinimaki M, Mentula M, Gissler M. How reliable are health registers? Registration of induced abortions and sterilizations in Finland. Inform Health Soc Care. 2017:1–10. doi: 10.1080/17538157.2017.1297306. [DOI] [PubMed] [Google Scholar]
- 34.Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Acad Pediatr. 2013;13(6 suppl):S38–S44. doi: 10.1016/j.acap.2013.08.002. [DOI] [PubMed] [Google Scholar]
- 35.Fretheim A, Zhang F, Ross-Degnan D et al. A reanalysis of cluster randomized trials showed interrupted time-series studies were valuable in health system evaluation. J Clin Epidemiol. 2015;68(3):324–333. doi: 10.1016/j.jclinepi.2014.10.003. [DOI] [PubMed] [Google Scholar]