Abstract
Purpose:
To compare the protective properties and ease of manipulation during cataract surgery of corneal coating with a gel (eyeDRO; AL.CHI.MI.A. S.R.L, Italy) and corneal irrigation with balanced salt solution (BSS).
Methods:
We analyzed the data of 51 patients receiving either eyeDRO or BSS during routine cataract surgery performed within a 20-day period in 2016. The selected parameters were intraoperative clarity and ease of manipulation; postoperative epithelial integrity; and patient discomfort.
Results:
Compared with BSS irrigation, eyeDRO coating significantly increased intraoperative clarity and ease of manipulation (P < 0.01). Single application was required in eyeDRO-treated eyes, whereas BSS was applied 5.3 ± 0.4 times on average (P < 0.01). Two hours postoperatively, a normal epithelium was observed in 90.0% and 60.0% of eyeDRO-coated and BSS-irrigated eyes, respectively; punctate epithelial damage was observed in 9.7% and 40.0% (P < 0.05) of eyeDRO-coated and BSS-irrigated eyes, respectively; eye irritation and foreign body sensation were experienced by 13.0% and 37.0% of eyeDRO-treated patients and by 65.0% and 100% of BSS-treated patients, respectively (P < 0.01). Twenty-four hours postoperatively, 80.0% of BSS-treated patients versus 19.0% of eyeDRO-treated patients still experienced foreign body sensation (P < 0.01).
Conclusions:
EyeDRO coating was shown to be a safer and more effective option than BSS irrigation in cataract surgery because single application provided optimal hydration and intraoperative clarity during the entire surgery, better preserved the corneal epithelium, and offered postoperative comfort to the patient.
Key Words: balanced salt solution irrigation, corneal hydration, viscoelastic, cataract surgery, corneal protection
The use of topical drops, corneal irrigation, and mechanical maneuvers during cataract surgery disturbs the balance of the corneal surface.1–4 Intraoperatively, a lid speculum is placed to prevent blinking of the eyelids, and an eye lubricant is required as a tear film substitute to ensure epithelial hydration and provide sufficient optical clarity. For anterior segment surgery, balanced salt solution (BSS) is usually used as an irrigating agent; however, the hydrating effect is short lasting, leading to frequent application by the surgeon or nurse. Repeated irrigations with BSS present a number of disadvantages. First, they may disturb and prolong the surgical procedure and be unpleasant for the patient, especially if the surgery is performed under topical anesthesia. Second, they may increase the risk of corneal epithelial damage, with possible discomfort caused by epithelial alterations and potentially prolonged postoperative recovery.5,6 As an alternative solution to BSS irrigation, coating using viscoelastic agents to ensure prolonged corneal hydration and optical clarity during cataract surgery has been studied since the late 1990s.5–8 Reports suggested that fewer rewetting events were required when a viscoelastic fluid was applied over the corneal surface, instead of BSS.7–9 However, most of the currently available viscoelastic agents were developed primarily for intraocular use to maintain anterior chamber stability during surgical maneuvers and protect the corneal endothelium.6,10 Therefore, it has been suggested that refinements in viscoelastic formulations may improve their efficacy and ease of use during cataract surgery.6 eyeDRO (AL.CHI.MI.A. S.R.L, Italy) is a commercially available medical device made of an advanced tripolymeric gel containing hydroxypropyl methylcellulose (HPMC), xanthan gum, and carrageenan and is intended to protect and hydrate the corneal surface during ophthalmic surgery and eye examination and to maintain maximum clarity of the operating field during surgery.
In this study, we retrospectively analyzed 51 cases in which patients received either eyeDRO or BSS during cataract surgery. Our aim was to compare both treatments for intraoperative clarity of the operative field, ease of manipulation, epithelial integrity, and patient comfort.
MATERIALS AND METHODS
Study Population
This study was conducted in compliance with the Declaration of Helsinki. Institutional review board approval was not required for the retrospective analysis of deidentified data, including quality management questionnaire data of 51 consecutive patients who underwent routine cataract surgery at Casa di Cura S. Camillo in Brescia, Italy, within a 20-day period in 2016. Patients having evidence of eye dryness (corresponding approximately to ≥ grade II of the Oxford test), any other ocular pathologies revealed by slit-lamp preoperative screening, and/or previous corneal or refractive surgery were excluded from the analysis. Patients with any systemic disease, such as diabetes, that could influence the ocular surface were also excluded. In addition, patients were excluded if complications occurred during or after surgery, which affected the outcomes.
Surgical Procedures
All cataract surgeries were performed by a single surgeon (P.G.) in an ambulatory day surgery setting according to internal standard protocols. The surgeon alternated the use of eyeDRO gel and BSS on a daily basis. The procedures were performed under anesthesia with only 1 drop of 0.4% benoxinate hydrochloride (Alfa Intes Srl, Italy), 5 minutes before surgery, followed by intracameral injection of 200 μL of Tropicamide, phenylephrine, lidocaine solution (Mydrane Laboratoires Théa, France) through a small side port, before the first 2.2-mm corneal incision. Subsequently, a lid speculum was placed, and either 1 drop of eyeDRO corneal coating gel was applied before surgery (if necessary, reapplied during surgery) or 2 mL of the BSS irrigating solution (Alcon) was applied repeatedly during surgery by the nurse. For each patient, the number of applications of the appropriate hydrating substance was recorded.
All patients underwent routine cataract extraction by phacoemulsification using Infinity equipment (Alcon), with a temporal incision and posterior chamber foldable intraocular lens implantation in the capsular bag. After surgery, eyeDRO residues were removed completely by rinsing with 20 mL of BSS.
The postsurgery regimen included netilmicin and dexamethasone eye drops for 4 days, a transparent shield at night, and sunglasses during the day for 1 week.
Intraoperative Assessment and Follow-up
Intraoperative and postoperative measurements were analyzed. Intraoperatively, the surgeon scored the clarity of the operative field and ease of manipulation using a 10-point arbitrary-unit grading scale at the end of surgery, adopted routinely with the aim of improving the procedure, with 10 being the highest and 1 being the lowest. Two hours after surgery, the cornea was stained using fluorescein ophthalmic strips (Optitech Eyecare, India) and assessed using a slit-lamp (Topcon Sl-7, Nikon, Japan); the extent of epithelial cell damage was scored by positive fluorescein staining (grades 1–3; 1 = no damage; 2 = punctate damage; and 3 = damaged area).
Patients' yes/no feedback to simple questions concerning postoperative pain, such as burning or itching, was used for the assessment of eye irritation or discomfort of foreign body sensation 2 and 24 hours after surgery. Postoperative observations were collected by medical staff other than the surgeon.
Statistical Analysis
The sample size estimate was obtained a priori based on a Mann–Whitney test using a Cohen d value of 0.9, an alpha error of 0.05, and a power of 80%, with an allocation ratio of 0.6 and increased by 10%. We performed the statistical analysis using Excel 2010 software. The box plots were generated by the BoxPlotR Web tool, http://boxplot.tyerslab.com. The Mann–Whitney U test was used to compare intraoperative parameters (clarity of the operative field, ease of manipulation, and the number of applications) between groups. Control of the family-wise error rate consequent to repeated statistical tests was performed using the Bonferroni correction. The χ2 test was used to analyze categorical variables (grade of fluorescent staining, eye irritation, and foreign body sensation) in 2-by-2 contingency tables. The results are presented as mean and SE. Differences yielding P < 0.05 were considered statistically significant.
RESULTS
The analysis compared 20 patients who received BSS irrigation with 31 patients who received eyeDRO coating gel during cataract surgery. Mean age of the patients included in the analysis was 74.7 ± 1.3 years (range 45–89 yr). Seven patients were excluded from the analysis because of diabetes and 5 because of corneal surface irregularities. All surgeries were uneventful, with standard surgery times. All types of cataracts were included in both groups. The grade 4 cataracts corresponded to 4 (20%) and 6 (19%) patients in the BSS and eyeDRO groups, respectively.
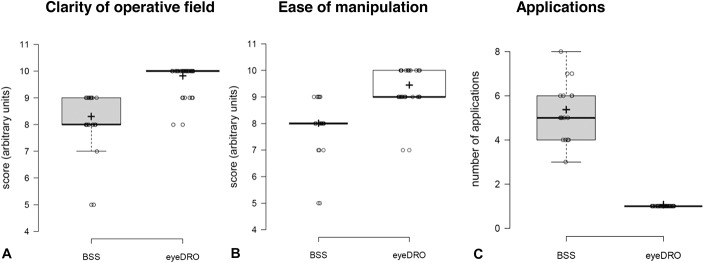
Application of eyeDRO significantly improved operative field clarity and ease of manipulation during ophthalmic surgery (Mann–Whitney U test, P < 0.01 for both parameters) (Fig. 1). All eyeDRO-treated patients required only 1 application of the coating gel during the entire surgery. By contrast, 5.3 irrigations with BSS were needed on average (with the use of 13.7 ± 1.5 mL of BSS irrigating solution, on average) to complete surgery in BSS-treated patients (Fig. 1); the difference in the frequency of application of the 2 hydrating solutions was statistically significant (Mann–Whitney U test, P < 0.01) (Fig. 1).
FIGURE 1.
Box plots show the data distribution of intraoperative measurements. (A) Clarity of operative field, (B) ease of manipulation, and (C) the number of applications in eyeDRO- (n = 31) and BSS-treated (n = 20) patients. P < 0.01 for all measured parameters, Mann–Whitney U test between groups, + mean value.
Two hours postoperatively, no epithelial damage was observed by fluorescein staining (grade 1) in 90.3% of eyeDRO-coated eyes, a significantly higher percentage (χ2 test, P < 0.05) than in the BSS-treated patients, who showed 60.0% of eyes without epithelial damage (Fig. 2). Only 9.7% of eyeDRO-treated eyes showed punctate epithelial damage (grade 2) compared with 40.0% of BSS-irrigated eyes. The difference between both groups was statistically significant (χ2 test, P < 0.05). No extended areas of damage (grade 3) were found in the eyes of any of the 51 patients (Fig. 2).
FIGURE 2.
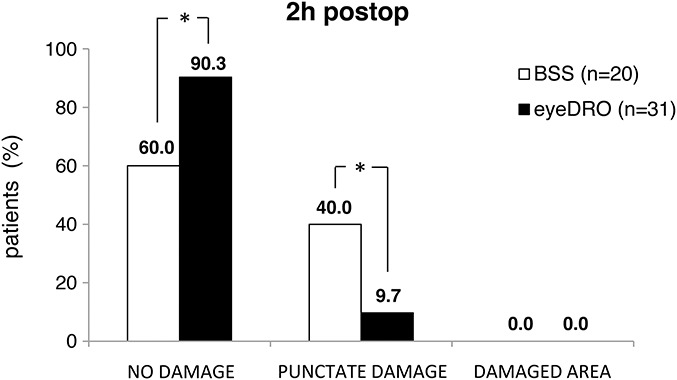
Two-hour postoperative outcomes in terms of fluorescein staining of the eyes in eyeDRO- and BSS-treated patients. *P < 0.05, χ2 test between groups.
Two hours after surgery, eye irritation and foreign body sensation were experienced by 13.0% and 37.0% of eyeDRO-treated patients, respectively, and 65.0% and 100.0% of BSS-treated patients, respectively. The difference between both groups was statistically significant for both parameters (χ2 test, P < 0.01) (Fig. 3A). Twenty-four hours postoperatively, eye irritation was still experienced by 9.0% and 25.0% of eyeDRO- and BSS-treated patients, respectively. This difference was not statistically significant. Foreign body sensation was experienced by 19.0% and 80.0% of patients treated with eyeDRO and BSS, respectively, which was a statistically significant difference (χ2 test, P < 0.01) between both groups (Fig. 3B).
FIGURE 3.
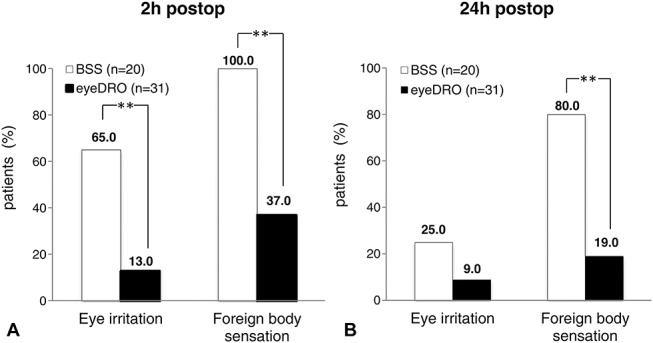
Results of the patient's feedback on postoperative pain in eye irritation (ie, burning or itching) and foreign body sensation in the eyeDRO group (▪) and in the BSS group (▫). A, Two hours postoperatively; (B) 24 hours after cataract surgery. **P < 0.01, χ2 test between groups.
DISCUSSION
Some of the most important functions of the precorneal tear film include lubricating the ocular surface and providing a smooth, regular optical surface for the eye.11,12 Blinking of the eyelids prevents breaking up of the tear film; however, the eyelids must remain open during cataract surgery. As a consequence, several environmental factors (e.g., the use of anesthetics and topical mydriatic agents, long surgery, high temperature and/or low humidity in the operating room, and the intensity of the microscope illumination) may compromise lubrication of the ocular surface and leave the cornea hazy.6,13 Therefore, agents that maintain optimal hydration and corneal transparency must be applied to the ocular surface to ensure a clear view for the surgeon and prevent damage and discomfort to the patient. BSS, which is the most commonly used corneal wetting agent, has the disadvantage of leaving the cornea hazy because it tends to evaporate quickly; therefore, frequent irrigations are required, which may harm the epithelium, stroma, and endothelium.7,9 Similarly, cohesive and dispersive viscoelastics, which are intended for intraocular use and used off-label as superficial lubricants to provide epithelial protection, surface hydration, and optical clarity,5,10 present some drawbacks.14 Based on our experience, cohesive agents do not provide an optimal thin coating layer because they form a sphere, which tends to slip on the wet corneal surface and is easily washed away. Dispersive viscoelastics do not cover the surface homogenously because they have a toothpaste-like consistency and must be spread on the corneal surface, thus resulting in very poor visibility of the operating field and difficult removal.14 Conversely, eyeDRO gel coated the entire corneal surface with a thin, uniform, and transparent layer that remained stable throughout surgery and also provided helpful magnification of the operating field. These effects could be due to the blend of 3 viscoelastic substances present in the eyeDRO formulation, in which each component contributes to the optimal rheological, thickening, stabilizing, bioadhesive, and magnifying properties of the gel.14–16
Our retrospective analysis showed that all the eyeDRO-treated patients required single application of gel to complete surgery, whereas 5 applications were required on average to maintain sufficient corneal hydration and optical clarity in patients treated with BSS. This corresponds to a slightly lower irrigation frequency than reported previously,5 in which 10 BSS irrigations were needed. Similarly, other studies indicated that second application of corneal wetting agents, such as the elastoviscous hylan surgical shield, 0.45% (HsS, Biomatrix, Canada) or 2.0% lignocaine gel, was required in many patients during surgery.7,8
Even if based on subjective evaluation by the surgeon, our analysis clearly indicated that eyeDRO significantly improved corneal transparency and operative field clarity with respect to the use of BSS. Similarly, previous reports by Arshinoff and Khoury7 and Kalyanasundaram and Hasan8 found that HsS and 2.0% lignocaine gel, respectively, maintained corneal clarity longer than BSS.
More recently, Chen et al5 compared a 2.0% HPMC corneal lubricant gel and BSS during cataract surgery under topical anesthesia and found that the use of a single dose (as a median, with a range of 1–8 applications) of HPMC gel showed significant advantages over BSS in both frequency of application and optical clarity for the surgeon. These findings are in agreement with our results, which were obtained with a formulation that, along with other polymers, is also HPMC based. The fact that some—although very few—patients in the study by Chen et al required second application of 2.0% HPMC might be related to the different composition of the 2.0% HPMC formulation with respect to that of the tripolymeric eyeDRO gel; nevertheless, it cannot be excluded that the larger population evaluated in the study by Chen et al might have accounted for this subtle difference in the frequency of application.
Considering the previous studies on viscoelastic corneal lubricants, we obtained significantly better results in epithelial preservation and patient comfort, while using eyeDRO instead of BSS. Conversely, in the study by Arshinoff and Khoury,7 the use of HsS did not show significant advantages over BSS in postoperative corneal health. In the study by Chen et al,5 1 hour postoperatively, the difference in fluorescein staining between the 2% HPMC-treated and control group patients was not significant, and the 1-hour postoperative subjective grading of patients' discomfort and perception of dry eye was similar in both groups. Thus, it is tempting to speculate that the “enriched” formulation of the tripolymeric gel might have accounted for the more consistent advantages for both surgeon and patients compared with the 2.0% HPMC coating gel during cataract surgery because both xanthan gum and carrageenan-based formulations are known to have a protective effect on the corneal surface.17,18 However, further studies are needed to test this hypothesis.
Our study provided some important information on the postoperative safety and tolerability of eyeDRO corneal coating gel that, to our knowledge, has so far not been reported. In addition, we suggest that the combination of the intraoperative use of a single drop of eyeDRO with the preoperative use of an intraocular mydriatic agent, rather than mydriatic drops, might further simplify the whole surgical procedure. Obviously, this hypothesis needs further investigation.
In conclusion, our retrospective analysis found that single application of 1 drop of eyeDRO at the beginning of surgery may be a preferable option in cataract surgery because it provides optimal corneal hydration, clear view of the surgical field during the entire surgery, less discomfort to the patients, and a simplified procedure. Cost–benefit analyses were outside the scope of this study. Nevertheless, the cost of eyeDRO gel is only slightly higher than that of a sterile BSS vial; however, considering the benefits to patients and surgeon, and the simplification of surgery, the use of the product has been implemented in our surgical practice.
Footnotes
C. Gatto and J. D'Amato Tóthová are employed by the company Alchilife S.r.l, which was involved in the development of the medical device discussed in this article. The remaining authors have no funding or conflicts of interest to disclose.
REFERENCES
- 1.Li XM, Hu L, Hu J, et al. Investigation of dry eye disease and analysis of the pathogenic factors in patients after cataract surgery. Cornea. 2007;26:16–20. [DOI] [PubMed] [Google Scholar]
- 2.Khanal S, Tomlinson A, Esakowitz L, et al. Changes in corneal sensitivity and tear physiology after phacoemulsification. Ophthalmic Physiol Opt. 2008;28:127–134. [DOI] [PubMed] [Google Scholar]
- 3.Cetinkaya S, Mestan E, Acir NO, et al. The course of dry eye after phacoemulsification surgery. BMC Ophthalmol. 2015;15:68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schulze D, Bertelmann T, Manojlovic I, et al. Changes in corneal endothelium cell characteristics after cataract surgery with and without use of viscoelastic substances during intraocular lens implantation. Clin Ophthalmol. 2015;9:2073–2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen YA, Hirnschall N, Findl O. Comparison of corneal wetting properties of viscous eye lubricant and balanced salt solution to maintain optical clarity during cataract surgery. J Cataract Refract Surg. 2011;37:1806–1808. [DOI] [PubMed] [Google Scholar]
- 6.Nankivil D, Gonzalez A, Arrieta E, et al. A new, specular reflection-based, precorneal tear film stability measurement technique on a rabbit model: viscoelastic increases tear film stability. Invest Ophthalmol Vis Sci. 2014;55:4158–4163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arshinoff A, Khoury E. HsS versus a balanced salt solution as a corneal wetting agent during routine cataract extraction and lens implantation. J Cataract Refract Surg. 1997;23:1221–1225. [DOI] [PubMed] [Google Scholar]
- 8.Kalyanasundaram T, Hasan M. Corneal-wetting property of lignocaine 2% jelly. J Cataract Refract Surg. 2002;28:1444–1445. [DOI] [PubMed] [Google Scholar]
- 9.Wessels IF, DeBarge R, Wessels DA. Salvaged viscoelastic reduces irrigation frequency during cataract surgery. Ophthalmic Surg Lasers. 1998;29:688–691. [PubMed] [Google Scholar]
- 10.Lee IJ, Lee H, Kim HK. Comparison of balanced salt solution and ophthalmic viscosurgical device to maintain optical clarity during phacoemulsification. J Korean Ophthalmol Soc. 2013;54:1514–1519. [Google Scholar]
- 11.Ohashi Y, Dogru M, Tsubota K. Laboratory findings in tear fluid analysis. Clin Chim Acta. 2006;369:17–28. [DOI] [PubMed] [Google Scholar]
- 12.Lu N, Lin F, Huang Z, et al. Changes of corneal wavefront aberrations in dry eye patients after treatment with artificial lubricant drops. J Ophthalmol. 2016;2016:1342056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schena E, Silvestri S, Franzesi GT, et al. Theoretical model and design of a device to reduce the influence of environmental factors on refractive surgery outcomes. Conf Proc IEEE Eng Med Biol Soc. 2016;1:343–346. [DOI] [PubMed] [Google Scholar]
- 14.Simon-Castellivi G, Simon-Castellivi S, Simon-Castellivi JM, et al. Viscoelastic and ophthalmic viscosurgical devices (OVDs) in ophthalmic surgery. In: Agarwal A, Jacob S, eds. Phacoemulsification. 4th ed Chennai, India: Jaepey Highlights Medical Publishers Inc; 2012:102–116. [Google Scholar]
- 15.Faraldi F, Papa V, Santoro D, et al. A new eye gel containing sodium hyaluronate and xanthan gum for the management of post-traumatic corneal abrasions. Clin Ophthalmol. 2012;6:727–731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khare A, Grover K, Pawar P, et al. Mucoadhesive polymers for enhancing retention in ocular drug deliver. In: Mittal KL. ed. Progress in Adhesion and Adhesives. Hoboken, NJ: John Wiley & Sons, Inc; 2015:451–484. [Google Scholar]
- 17.Llamas-Moreno JF, Baiza-Durán LM, Saucedo-Rodríguez LR, et al. Efficacy and safety of chondroitin sulfate/xanthan gum versus polyethylene glycol/propylene glycol/hydroxypropyl guar in patients with dry eye. Clin Ophthalmol. 2013;7:995–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernández-Ferreiro A, González Barcia M, Gil-Martínez M, et al. In vitro and in vivo ocular safety and eye surface permanence determination by direct and Magnetic Resonance Imaging of ion-sensitive hydrogels based on gellan gum and kappa-carrageenan. Eur J Pharm Biopharm. 2015;94:342–351. [DOI] [PubMed] [Google Scholar]