Abstract
Background:
The majority of the global burden of cervical cancer is affecting developing countries. Despite improvement in treatment of patients presenting at a locally advanced stage, approximately 50% experience recurrence within the 1st two years. This study was conducted to analyse contributory factors for recurrence within 24 months.
Methods:
The present retrospective study was undertaken to analyse factors affecting recurrence, type of failure and the follow up pattern of patients who completed treatment with a minimum follow-up period of 6 months during the study period of 5 years.
Results:
Out of 323 patients included in the study, 112 (34.7%) presented with recurrence within the follow-up period. The stage and histology had a significant impact on disease free survival (DFS). Of those who were followed-up regularly, recurrence was observed in 28.7% with a DFS of 81.3 months, in contrast to the 48. 5% patients with a DFS of 45.0 months for whom follow-up was irregular. The failure pattern was mostly in the form of nodal recurrence (61%). On univariate analysis, treatment time, EBRT and ICBT gap and mean EQD2 point A were found to associated with a better outcome in terms of 2yr DFS. On Cox regression analysis, stage, histology, treatment gap (HR-0.48) and follow up pattern (HR-0.24) retained their effects on survival. Point A dose was higher in patients without recurrence (P value 0.000) unlike other assymmetric parameters.
Conclusion:
Apart from point A cumulative dose (mean EQD2), stage, histology and treatment gap were the factors that affected early local failure. An interesting result was that follow-up pattern had a significant impact on DFS period.
Keywords: Retrospective audit, locally advanced cervical cancer, early local recurrence
Introduction
Cervical cancer is the fourth most common cancer in women worldwide and seventh overall with an estimated 528,000 new cases in 2012. The large majority of global burden occurs in the less developed regions like Africa, Asiawhere it accounts for almost 12% of all female cancers. As far as the mortality rate is concerned, almost 87% cervical cancer deaths occur in these less developed countries (Globocan, 2012). In India, It is the second most common cause of cancer accounting for approximately 1,22,644 new cases (2012). Though there has been a decreasing trend of incidence in the last forty years, still it accounts for an age standardized mortality rate of 9.8- 17.5 per 100,000 in India.
In our country, majority of patients present at an advanced stage where radiotherapy forms the main treatment option. Though there are various guidelines for exact dose scheduling, the practice pattern varies widely from institution to institution as per availability of resources and workload. The standard treatment that is practiced widely in our country constitutes of 50Gy of EBRT by conventional fractionation to whole pelvis with concurrent cisplatin based chemotherapy followed by intracavitary brachytherapy of 21Gy (HDR) in three Fractions of 7 Gy each, weekly. With this standard of care, the 5 year recurrence free survival is about 79% for stage IB, IIA disease and 59% for III/IVAdisease with about 36.7% failing locally within the central pelvis despite this aggressive course of chemoradiation (Zola et al., 2007).
Cervical cancer recurrences can be loco regional or distant. Loco regional disease includes Para-aortic nodal recurrence and disease limited to pelvis. Central pelvic recurrence develops from the cervix and vagina after primary radiotherapy or from the vaginal cuff and central scar after radical hysterectomy. Lateral pelvic recurrence includes parietal and visceral pelvic side disease. The former consists of pelvic lymph node metastases and is usually located above the level of the obturator nerve, whereas the latter originates from the paracervix or from scars of the paracervical resection and is placed below the obturator nerve (Gadducci et al., 1995).
This study is a small endeavour to retrospectively analyse all the clinicopathological factors in detail responsible for recurrence in those subset of patients who fail locally and simultaneously compare the dosimetric variations in relation to failure and toxicity profile in the service setting of Government Medical College, Hospital.
Aims and Objectives
The aim of this study was to retrospectively determine the factors affecting recurrence, failure patterns, disease free survivalof cervical cancer patients treated with definitive or adjuvant radiotherapy with or without concurrent chemotherapy. The follow up pattern was analyzed and detailed assessment of failure pattern and late toxicity was made.
Materials and Methods
A single institutional retrospective analysis with a period of 5 years (2006-2012) was undertaken. Patients who received treatment in form of definitive or adjuvant radiation with adequate follow up reports of minimum of six months were considered in the study. The women those were included in this study from the follow up records had biopsy proven squamous cell carcinoma, adenocarcinoma of the cervix FIGO stage I-IVAand received adjuvant or definitiveradiotherapy at our institution comprising External beam radiation with or without chemotherapy followed by brachytherapy. Excluded were those patients who did not complete treatment, patients older than 70 years, patients presenting with para-aortic node, patients having history of prior malignancy, patients receiving neoadjuvant chemotherapy or EBRT from other hospitals, FIGO stage IVB and those patients who did not follow up permanently after treatment completion. Hence, out of 1069 patients enrolled during the study period of 5 years (2007-2012), 323 patients were found to be eligible and evaluated for the study.
The pre-treatment evaluation included a Contrast enhanced CT scan of abdomen and Pelvis, digital X ray of Chest, proper clinical staging including per-speculum examination, pervaginal and per rectal examination. Blood parameters like haemogram, total and differential counts, platelet counts along with renal and liver function test are sought before starting treatment. Urine analysis including cytology and biochemistry and cardiological evaluation for elderly patients were also done routinely at our institute during the study period. In patients with suspected bladder and rectal involvement went for cystoscopy and procto-sigmoidoscopy respectively. Whole pelvic irradiation was administered for all cases with Co60 γ ray through anterior-posterior parallel opposing ports (AP/PA) with a field size of 14-16 to 16-17 cm with conventional fractionation of 2Gy per fraction; more or less every one received 45 to50 Gy. Four field box techniques was observed for 27 patients. No midline shielding was done in any of the patients. Weekly chemotherapy was administered with injection Cisplatin 35 mg/m2 when deemed suitable, for a maximum of 5 cycles. ICRT procedures using Ir192 source included LDR brachytherapy with 30 Gy at point A and mostly HDR bachytherapy with 7 Gy dose at point A for three fractions or 9 Gy dose at point A for two fractions thatwas delivered after post EBRT response assessment. Applicator used was Fletcher type (both original and modified) or Manchester type (with rectal guard) ICRT brachytherapy applicators. For post operative cases, vaginal cylinder using HDR brachytherapy with 7Gy/3# were carried out for 38 patients. The gap following EBRT completion for Intracavitary applications were noted. Interdigitation of ICRT was not done for any of the cases studied. After treatment completion, follow-up data was observed every 3 monthly which included clinical examination and cervical cytology. Chest radiograph and abdomino-pelvic CT were observed to be carried out in patients every 6 monthly or when clinically required.
Patients who followed up regularly till recurrence or upto a period of two years after treatment completion were categorised as regular. Rest of the patients who followed up on recurrence or for period of less than two years were considered irregular. Local recurrence was considered if disease was detected centrally or in the parametrium within the pelvis (in field). Recurrences were defined as distant if they occurred in the para-aortic lymph nodes or elsewhere outside the pelvis. Time to failure or disease free survival period was defined as the interval between completion of last fraction of brachytherapy and clinical presentation of symptoms of recurrence during follow up. This was further analysed radiologicaly and confirmed cytological or histological whenever possible. Apart from time to event analysis of disease free survival, an independent analysis of factors attributing to early local recurrence within 1st 24 months after completion of radiation was undertaken. Follow-up time was defined by the interval between the first day of radiotherapy and the last information about the patient. Patients presenting with rectal or bladder complications during follow up period were evaluated and managed by department of surgical gastroenterology and urologists. Toxicity was graded according to the LATE Toxicity criteria by RTOG (Cox et al., 1995).
The main purpose of the study was the evaluation of pattern and determinants of pelvic recurrence as well as distant metastasis. Detailed analysis of form of brachytherapy, fractionation schedule, dosimetric parameters of target organ, organs at risk and point A dose i.e mean EQD2 were also studied. For those patients whose CT based planning was done and data was available, cumulative EQD2 was calculated as per LQ model.Correlation of both dosimetric and non dosimetric parameters were studied with respect to time to failure and documented late toxicities for both arms. Inference was made putting emphasis on clinicopathological presentation, dosimetric features, follow up pattern and treatment related factors affecting recurrence.
Statistical Analysis: The data were analyzed with SPSS software. Results were calculated applying Chi square test, cox regression analysis wasdone and P-value was calculated using an alpha level of 0.05 for Type I error.
Results
Out of 1069 patients enrolled during the study period of 5 years (2007-2012), 323 patients were eligible and evaluated for the study, of which 112 (34.7%) patients presented with recurrence during a median follow up period was 45 months. Mean age of presentation was 49.47yrs (49.41 years in those presenting with recurrence). Overall, majority of stage of presentation was at stage II (52.6%) followed by stage III (35.6%), stage I (9.3%) stage IV (2.5%).38 post operative cases underwent adjuvant radiation (20-stage I and 18-stage II). Most common histology was moderately differentiated squamous cell carcinoma (52.9%), followed by WDSCC(26.0%), PDSCC(9.6%), Adenocarcinoma (7.7%), non-keratinizing large cell carcinoma(3.7%). The baseline characteristics of all patients were comparable (as shown in Table-1 below)
Table 1.
Patient Characteristics According to the Type of Barchytherapy Received
| Patient characteristics | (7Gy x 3#)-222 | (9Gyx2#) -73 | LDR-28 | Significance (p value) |
|---|---|---|---|---|
| Age (Mean) | 51.86 | 50.91 | 50.06 | 0.542 |
| Menopausal status | ||||
| Premenopausal | 75 | 22 | 7 | |
| Post menopausal | 147 | 51 | 21 | |
| Stage | ||||
| I | 20 | 8 | 2 | 0.276 |
| II | 119 | 31 | 20 | |
| III | 77 | 32 | 6 | |
| IVA | 6 | 2 | 0 | |
| Differentiation | ||||
| Well differentiated | 51 | 25 | 8 | 0.116 |
| Moderately differentiated | 116 | 39 | 16 | |
| Poorly differentiated | 26 | 5 | 0 | |
| Histology | ||||
| Squamous | 193 | 69 | 24 | 0.113 |
| Adenocarcinoma | 19 | 2 | 4 | |
| Others | 10 | 2 | 0 | |
| Mean treatment time (weeks) | 10.18 | 10.04 | 8.71 | 0 |
| Mean EQD2 | 79.35Gy10 | 76.67Gy10 | - | 0.444 |
Overall treatment duration was 10.02 weeks. Overall disease free survival period was 67 months. For stage I, DFS observed was 96months, stage II-88months, stage III-56months and stage IVA-50months. There was no significant association found between type of ICRT treatment received and recurrence. Inference could not be drawn because of smaller subset of patients receiving LDR and HDR brachytherapy with 9Gy/# as compared to sample size receiving 7Gy/# HBR-ICBT.
Recurrence was observed in 28.76% of patients who followed up regularly unlike 48.45% patients who were irregular and presented with symptoms on relapse of the disease (P value-0.001). Clinical presentation on recurrence was mostly in form of hydronephrosis,hydroureter in patients who didn’t follow up after treatment. The cause behind irregular follow up pattern was either symptoms due to toxicity or recurrence. Patients who underwent regular follow up on recurrence developedPap smear positive for malignancy or vault biopsy. Failure pattern (Table 1) was mostly in form of nodal recurrence (61%) and distant metastasis (5.6%) was mostly in form of liver and lung metastasis. It was mostly observed in locally advanced cases who had undergone delay in definitive radiotherapy because of referral from health care centres after receiving 1-2 cycles neoadjuvant chemotherapy as well as in early (stage II)cases who had inadequate surgical resection due to under diagnosis on clinical staging followed by delay in adjuvant radiation. Interstitial radiotherapy showed better survival rates than Intracavitary brachytherapy in stage III patients though significance could not of be established due to small subset of patients.
Figure 1.

STROBE Diagram of Derivation of the Study Sample Size
Figure 2.

Locoregional Disease Free Survival as per Initial Stage of Presentation
Figure 3.
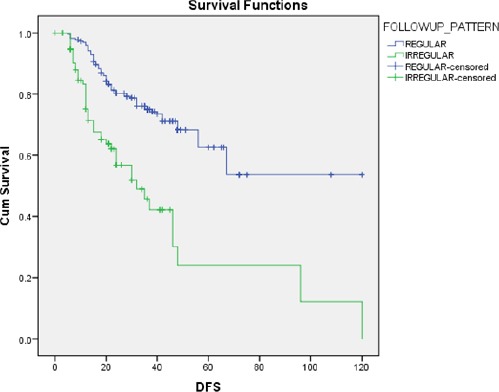
Comparison of Locoregional Disease Free Survival Patients with or without Regular Follow up
Univariate (Chi square) analysis of histology of the tumour with the failure pattern showed a trend towards significance (P value-0.048). Moderately differentiated carcinoma was associated with nodal recurrence while Adenocarcinoma was more associated with distant metastasis though significance level was not reached. The stage on presentation and histology was found to have significant impact on overall survival (Table 4). On detailed analysis of time of recurrence, it was found that most of the recurrences in stage II and III cervical cancers occurred within the time span of 1st two years during follow up. Hence, statistical analysis was made to find the impact of various factors on 2 year survival period.On univariate analysis (Table 2), treatment duration,gap between EBRT and ICBT and mean EQD2 at point A was found to be significant associated with 2yr DFS.Cox regression analysis (Table 5) considering histology, stage, age, treatment duration, toxicity gap, ICRT type, response and follow up pattern as variables was undertaken. Out of these; stage, histology, toxicity gap (HR-0.48) and follow up pattern (HR-0.24) were found to retain their effect on survival. The type of response also had an impact on survival, though it was not found to be significant (P value-0.01) The interesting observation found in the study was the association of regular follow up pattern with the survival time(Graph-B). There was a trend of better survival period in patients who followed up regularly i.e. survival time for patients with regular follow up was 81.33months versus 44.96 months of those who followed up on recurrence. Moreover, the 5 year DFS was 81.3% versus 62.1% respectively. This could be justified with the fact that the subset of patients, who followed up regularly,was those who presented at an early stage and had minimum treatment delay.
Table 4.
Univariate Analyses of Factors affecting Disease Free Survival
| Variables | DFS(months) | P value |
|---|---|---|
| Stage | 0.02 | |
| I | 88.85 | |
| II | 80.13 | |
| III | 44.75 | |
| IV | 36 | |
| Age | 0.77 | |
| <50yrs | 67 | |
| ≥50yrs | 76 | |
| Histology and Differentiation | 0.008 | |
| Well differentiated Squamous Cell Carcinoma | 96 | |
| Moderately differentiated Squamous Cell Carcinoma | 56 | |
| Poorly differentiated Squamous Cell Carcinoma | 48 | |
| Adenocarcinoma | 33.97 | |
| Non keratinising Large cell carcinoma | 32 | |
| Treatment duration | 0.718 | |
| <8weeks | 57 | |
| ≥8weeks | 54.3 |
Table 2.
Pattern of Recurrence
| Frequency | Count within 24 months of completion of treatment (n=323) | Percentage | |
|---|---|---|---|
| Local recurrence | Nodal | 61 | 18.9 |
| Central | 28 | 8.7 | |
| Distant metastases | 18 | 5.6 | |
| Clinically Controlled disease | 216 | 66.9 | |
| Total | 323 | 100 | |
Table 5.
Multivariate Analysis of Factors Affecting Overall Survival (Cox-Proportional Hazard Ratio)
| Variable | Degree of freedom | significance | Hazard ratio |
|---|---|---|---|
| Histology | 4 | 0.004 | |
| Stage | 3 | 0.001 | |
| Age | 1 | 0.457 | |
| Treatment duration | 1 | 0.159 | 1.101 |
| Treatment Gap due to toxicity | 1 | 0.005 | 0.486 |
| ICRT dose | 2 | 0.123 | |
| Response | 2 | 0.042 | |
| Follow up Pattern | 1 | 0 | 0.246 |
Table 3.
Comparison of Mean Prescribed Dose to Point A among Patients with and without Pelvic Recurrence (* in a Subgroup of Patients Receiving Image Guided HDR Brachytherapy)
| Number of Patients*(197) | Recurrence | Dose at point A | P value |
|---|---|---|---|
| 56 | Yes | 76.91 ±4.86 | 0 |
| 141 | No | 79.52±4.65 |
The data in relation to the dosimetric parameters were available for 197 patients which revealed that the dose at point A was higher(76.91Gy Vs80.55Gy) in patients without recurrence and on analysis by ANOVA, there was significant association (P value 0.000) unlike other parameters. The mean D2cc for bladder and rectum was 83.05Gy and 76.55Gy respectively. Late toxicity (42% cases) was observed most commonly in form of Grade-II urinary incontinence (71.42%), Grade-II-III rectal toxicity (23.8%) and rectovaginal fistula (4.76%). There was trend towards significance (P value-0.018) for association of recurrence with clinical response following treatment (all the patients with stable disease developed recurrence unlike patientswith complete or partial response (CR-34.57% and PR-30%).
Discussion
Cancer of the cervix is one of the most common cancers among women in India presenting in locally advanced stage. Reviewing the published data on cervical cancer treatment, it is noticed that a combination of external beam irradiation and intracavitary Brachytherapy achieves excellent loco regional disease control and survival for patients with early cervical cancer. In developing countries like India, patients usually present in locally advanced stages. In our study,Overall, majority of stage of presentation was at stage II (52.6%) followed by stage III (35.6%) which was in accordance with other studies conducted by other countries like Iran,Saudi Arabia (Hong et al., 1998; GEC ESTRO, 2005).
Lowrey et al., (1992) reported on their series of 701 Stage IB1 cervical cancer patients, the 5-year disease-specific survivalrate for this group was 95% in the present study,overall 5 year DFS for all stage was found to be 67 months. According to pattern of follow up, 5 year DFS was81.3% in patients with regular follow up versus 63.7% who followed up on recurrence.
Disease free survival is one of the important prognostic factors in patients with cervical cancer. DFS average values were different in various reports. In Duyn et al., (2002) study, average disease free interval among 47 patients in different stages was 18 months. In Lim et al., (2004) study, among 53 patients, it was 17.6 months. Mahe et al., (1996) reported average of DFI as 70 months among seventy patients, which stands close to our findings i.e. overall DFI of 67 months. Thus, in our Scenario of cervical cancer recurrence, most of the patients presented as central or nodal failure mostly during two years of treatment completion. Hence detailed analysis of clinicopathogical factors predicting the outcome with respect to 2 year DFS was undertaken in our study where treatment duration, gap between EBRT and ICBT and mean EQD2 at point A was found to be significantly associated with 2yr DFS.
During the study period of 5 years in a sample size of 323 patients, 34.7% presented with recurrence. Recurrence rates ranging from 19% to 36% have been reported in various series following treatment of cervical cancer by radical surgery and postoperative RT (Atkover et al., 1995; Figgs and Tamimi, 1971; Tay SK, Tan LK, 1998).
As observed in various published literature, for Stage IIB disease, the 5-year survival rate ranges between 65% to 75%; for Stage IIIB it is 35%.(Eifel et al., 1994; lim et al., 2004) In our study, the 5 year DFS in stage II and stage III was 77.2% and 61.0% respectively which is more or less similar to other published literature.
Considering the impact of histology in our study, well differentiated carcinoma constituted only 20.2% of cases while poorly differentiated CA and adenocarcinoma had 48.3% and 40% of cases presenting with recurrence respectively. Various authors have noted higher incidence of lymph node metastasis and increased recurrence rates in adenocarcinoma, while other have not. (Burke et al., 1987; Chung et al., 1980; El-Sayed et al., 2016; Figgs and Tamimi, 1971) Moreover, on assessing the pattern of recurrence, moderately differentiated carcinoma was associated with nodal recurrence while Adenocarcinoma was more associated with distant metastasis on recurrence, though significance could not be established.
Other than stage at presentation and histology, the total treatment durationhas a significant impact on DFS. Study conducted by Eifel et al., (1994) concluded that these good results are achievable when the treatment is completed within eight weeks i.ethe maximum efficacious time frame representing an acceptable treatment duration. The mean treatment duration in this study was found to be 10.02weeks with a mean gap of 23.25 days between EBRT and ICRT. Unfortunately, in our study it didn’t emerge as a significant factor for predicting disease free survival. Interestingly, on statistical analysis of its impact on 2 year DFS,the results were close to significant values (P value-0.003).
In a case series by Lim et al., (2004), of 53 patients with recurrent cancer, only seven patients indicated routine follow up. In the present study, 48.45% of patients attending OPD irregularly on being symptomatic had recurrence unlike 28.76% of patients who followed up regularly (P value-0.001). This could be justified with the fact that the subset of compliant patients who received prompt treatment without any unnecessary delay followed up regularly and hence lesser percentage of them had recurrence.
Perez et al., (1998) conducted a study which reviewed 1499 patients (Stages IA-IVA) treated with definitive irradiation (combination of external beam plus two intracavitary insertions to deliver doses of 65-95 Gy to point A, depending on stage and tumour volume). Follow-up was obtained in 98% of patients (median 11 years, minimum 3 years, and maximum 30 years). The study concludedclinical stage and size of tumouras critical factors in prognosis and therapy efficacy. The doses to point A suggested that for lesions <2 cm, doses of 75 Gy result in < or =10% pelvic failures, whereas in more extensive lesions, even with doses of 85 Gy, the pelvic failure rate is about 30%; and in Stage IIB-III tumors, doses of 85 Gy result in 35-50% pelvic failures. In our study, the retrospective analysis of patients presenting with recurrence revealed point A dose to be lesser than that of patients without recurrence (76.91Gy Vs 80.55Gy).Moreover, on univariate and multivariate analysis the association of point A dose with recurrence was found to be significant.
Thus the recurrence rate, pattern of failure and the disease free survival period as observed in our study was comparable with other published literature. Though, as per other literature; age at diagnosis emerged as important prognostic factor in cervical cancer (Gadducci et al., 1995) but it was not found to be statistically significant in our study.
There are other cofactors used as predictors of recurrence like squamous cell carcinoma antigen, Ki67 which have been analysed in various studies unlike ours due to unavailability of data because of the retrospective nature of our study. Hong et al., (1998) concluded from his study of 401 patients of stage I-IVA concluded that pretreatment SCC levels higher than 10 ng/ml was an independent predictor for poor prognosis and persistent high levels indicate treatment failure. Moreover, other shortcomings of this study was the inability of analyse the impact of pre treatment hemoglobin as observed in other literatures. A study from Saudi Arabia by Sayed M et al., (2016) evaluated the survival outcome, pattern of failure and prognostic factors in of 60 patients with stages IB-IVA cancer. The 2- and 4-year disease-free survival (DFS) rates were found to be 80% and 69%, respectively while in our study,the 5 year DFS of patients who underwent regular follow up versus those who were irregular was 81.3% versus 62.1% respectively. Prolongation of the overall treatment time for greater than 56 days, advanced stage and pretreatment hemoglobin (Hb) levels (<10 g/dL) negatively predicted OS. Moreover, vaginal infiltration and brachytherapy (orthogonal versus CT-based planning) were observed to be significant factors for the prediction of relapse. In our study, all the patients had undergone CT guided brachytherapy while dosimetric data was available for 197 patients only.CT based planning for EBRT was also unavailable for most of the patients; hence data of pretreatment tumour burden was not available for prediction of outcome. In this regard, with the advancement in gynecological MR imaging technology, studies have been undertaken toanalyse the combined volume and dynamic enhancement pattern by MR imaging for predicting tumor control in patients with cervical cancer (Mahe et al., 1996). Results of such a study in USA by Mayr et al., (1998) show that combined analysis did not improve the prediction rate of local recurrence in small-sized tumors. However, the combined analysis did improve the prediction rate of local recurrence in intermediate- and large-sized tumors (75% and 80%, respectively) over assessment by either volume analysis (33% and 60%, respectively) or dynamic enhancement pattern analysis (64% and 64%, respectively). The combined analysis was most useful in intermediate-sized tumors (40-99 cm3; 33% recurrence), significantly improving differentiation between high-risk (80% recurrence) and low-risk 10% recurrence) patients.
Lack of follow up can be a major contributing factor for treatment failure. Possible causes include poor patient education and shortage of resources to attend on time along with poor infrastructure compared to the disease burden in a developing country like India where cancer cervix ranks second highest in malignancy among females. Our study results in relation to various prognostic factors in predicting recurrence was in accordance with other retrospective studies (Burke et al., 1987; Hong et al., 1998; Duyn et al., 2002; Acharya et al., 2014; Gattoc et al., 2014; El-Sayed et al., 2016) Lack of follow-up is a major problem we faced when conducting this study which led to selection bias. The post operative patients presenting with vault recurrence underwent interstitial brachytherapy at our Department, few patients were tumour was observed to be operable were referred to oncosurgical department. Other patients received salvage chemotherapy of taxane and platin combination. The patients who were regular in follow up had a good performance status and responded well to second line or salvage treatment unlike those who followed up on recurrence with detoriating symptoms and poor performance score or distant metastasis. This study can be taken a step further by analyzing the overall survival of these patients following treatment to recurrence. Moreover, dosimetric parameters of patients who underwent HDR brachytherapy were also analysed in detail in this study and significance of dose at point A with respect to recurrence was established.
In conclusion, this study was undertaken in a service setting of a developing country where majority of global burden of cervical cancer resides. The knowledge from various published literature was found to be in concordance with the results as observed in our East-Indian scenario. During study size derivation, drop rates at each step pointed out the increasing role of awareness to procure treatment for better quality of life and disease free survival. Heterogeneity of the sample size and poor follow up data led to limitations of inability of establishing statistically significant results. Nevertheless, the interesting result that was brought into the picture was the follow up pattern which had a statistically significant impact on disease free survival period. Being a treatable disease where radiation plays a pivotal role, many clinicopathological factors were analysed retrospectively along with establishment of dosimetric correlation that could be tackled to prevent recurrence and prolong DFS. One step further can be taken in this study by further analysing the overall survival of the patients with recurrence in good performance status that were eventually found to be regular during follow up so as to evaluate in particular, the importance of adherence to routine check up following recurrence.
References
- Acharya S, Saha AK, Mandal B, De S, Mandal S. A retrospective study of prognostic factors in locally advanced cancer of uterine cervix in a rural medical college of west Bengal. J Res Med Den Sci. 2014;13:32–5. [Google Scholar]
- Atkover G, Uzel O, Ozsahin M, et al. Postoperative radiotherapy in carcinoma of the cervix:treatmentresults and prognostic factors. Radiother Oncol. 1995;35:198–205. doi: 10.1016/0167-8140(95)01570-7. [DOI] [PubMed] [Google Scholar]
- Burke TW, Hoskins WJ, Heller PB, et al. Clinical patterns of tumour recurrence after radical hysterectomy in stage 1B cervical carcinoma. Obstet Gynecol. 1987;69:382–5. [PubMed] [Google Scholar]
- Cervical cancer estimated incidence, mortality and prevalence worldwide in. 2012. www.globocan.iarc.fr .
- Chung CK, Nahhas WA, Stryker JA, et al. Analysis of factors contributing to treatment failures in stages IB and IIA carcinoma of the cervix. Am J Obstet Gynecol. 1980;138:550–6. doi: 10.1016/0002-9378(80)90285-9. [DOI] [PubMed] [Google Scholar]
- Cox JD, Stetz J, Pajak TF, et al. Toxicity criteria of the radiation therapy oncology group (RTOG) and the European organization for research and treatment of cancer (EORTC) Int J Radiat Oncol Biol Phys. 1995;31:1341–6. doi: 10.1016/0360-3016(95)00060-C. [DOI] [PubMed] [Google Scholar]
- Duyn A, Van Eijkeren M, Kenter G, et al. Recurrent cervical cancer:detection and prognosis. Acta Obstet Gynecol Scand. 2002;81:759–63. doi: 10.1034/j.1600-0412.2002.810414.x. [DOI] [PubMed] [Google Scholar]
- Eifel PJ, Morris M, Wharton JT, Oswald NJ. The influence of tumour size and morphology on the outcome of patients with FIGO stage IB squamous cell carcinoma of the uterine cervix. Int J Radiat Oncol Biol Phys. 1994;29:9–16. doi: 10.1016/0360-3016(94)90220-8. [DOI] [PubMed] [Google Scholar]
- El-Sayed ME, Bahadur YA, Hassouna AH, Anfinan N. Outcome of cervix uteri cancer patients:Clinical treatment results and toxicity profile in a retrospective study from Saudi Arabia. Asia Pac J Clin Oncol. 2016;13:e364–e72. doi: 10.1111/ajco.12486. [DOI] [PubMed] [Google Scholar]
- Figgs DC, Tamimi HK. Patterns of recurrence of cervical carcinoma following radical hysterectomy. Am J Obstet Gynecol. 1971;110:973–8. doi: 10.1016/0002-9378(81)90110-1. [DOI] [PubMed] [Google Scholar]
- Gadducci A, Fabrini MG, Bonuccelli A, et al. Recurrence patterns in patients with early stage cervical cancer treated with radical hysterectomy and external pelvic irradiation. Anticancer Res. 1995;15:1071–8. [PubMed] [Google Scholar]
- Gadducci A, Tana R, Cosio S, Cionini L. Treatment options in recurrent cervical cancer (Review) Oncol Lett. 2010;1:3–11. doi: 10.3892/ol_00000001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gajalakshmi V, Rajaraman S, Shanta V. A survival study of cervical cancer in Chennai, India. Indian J Cancer. 2000;37:158–64. [PubMed] [Google Scholar]
- Gattoc L, Viswanathan AN, Perez CA, et al. Cervical cancer. cancernetwork.com. 2015 [Google Scholar]
- Ghaemmaghami F, Saleh-Gargari S, Sahebdel B, Behtash N, Samiei F. Risk factors and clinical aspects of recurrent invasive cervical carcinoma. J Obstet Gynaecol India. 2012;62:674–8. doi: 10.1007/s13224-012-0227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong JH, Tsai CS, Chang JT, et al. The prognostic significance of pre and post treatment SCC levels in patients with squamous cell carcinoma of the cervix treated by radiotherapy. Int J Radiat Oncol Biol Phys. 1998;41:823–30. doi: 10.1016/s0360-3016(98)00147-3. [DOI] [PubMed] [Google Scholar]
- Lim KC, Howells RE, Evans AS. The role of clinical follow up in early stage cervical cancer in South Wales. Br J Obstet Gynaecol. 2004;111:1444–8. doi: 10.1111/j.1471-0528.2004.00280.x. [DOI] [PubMed] [Google Scholar]
- Lowrey GC, Mendenhall WM, Million RR. Stage IB or IIA-B carcinoma of the intact uterine cervix treated with irradiation :A multivariate analysis. Int J Radiat Oncol Biol Phys. 1992;24:205–10. doi: 10.1016/0360-3016(92)90672-5. [DOI] [PubMed] [Google Scholar]
- Mahe MA, Gerard JP, Dubois JB, et al. Intraoperative radiation therapy in recurrent carcinoma of the uterine cervix:Report of the French intraoperative group on 70 patients. Int J Radiat Oncol Biol Phys. 1996;34:21–6. doi: 10.1016/0360-3016(95)02089-6. [DOI] [PubMed] [Google Scholar]
- Mayr NA, Yuh WT, Zheng J, et al. Prediction of tumor control in patients with cervical cancer:Analysis of combined volume and dynamic enhancement pattern by MR imaging. AJR Am J Roentgenol. 1998;170:177–82. doi: 10.2214/ajr.170.1.9423627. [DOI] [PubMed] [Google Scholar]
- Perez CA, Grigsby PW, Chao KS, Mutch DG, Lockett MA. Tumor size, irradiation dose, and long-term outcome of carcinoma of uterine cervix. Int J Radiat Oncol Biol Phys. 1998;41:307–17. doi: 10.1016/s0360-3016(98)00067-4. [DOI] [PubMed] [Google Scholar]
- Recommendations from the (GYN) GEC ESTRO working group. Concepts and terms in 3D image based treatment planning in cervical cancer brachytherapy with emphasis on MRI assesement of GTV and CTV. Radiother Oncol. 2005;74:235–45. doi: 10.1016/j.radonc.2004.12.015. [DOI] [PubMed] [Google Scholar]
- Tay SK, Tan LK. Outcome of early cervical carcinoma treated by wertheim hysterectomy with selective postoperative radiotherapy. Ann Acad Med Singapore. 1998;27:613–7. [PubMed] [Google Scholar]
- Zola P, Fuso L, Mazzola S, et al. Could different follow-up modalities play a role in asymptomatic cervical cancer relapses diagnosis? An Italian multicenter retrospective analysis. Gynecol Oncol. 2007;107:150–4. doi: 10.1016/j.ygyno.2007.07.028. [DOI] [PubMed] [Google Scholar]


