Abstract
Objective
Preeclampsia (PE) occurs in 4.6% of pregnancies worldwide. The social phenomenon of increasing maternal age has raised the demand for donor oocytes. Egg donation has allowed women with poor ovarian reserve, premature ovarian failure, genetic disorders or surgical menopause to get pregnant. Recipients provide a unique model of immune response because of the differences in the genetic makeup of mothers and fetuses. In PE, immune tolerance may be impaired as a result of having non-autologous eggs implanted. Egg donation is a highly successful assisted reproductive technology, despite the significant number of issues arising from the implantation of non-autologous eggs. This study aimed to determine whether there is an association between egg donation and preeclampsia.
Methods
A systematic review of the literature available in PubMed and Google Scholar was carried out from January of 1995 to August of 2016 using the terms 'oocyte donation, preeclampsia', 'oocyte donation, in vitro fertilization, preeclampsia', 'oocyte donation, preeclampsia, outcomes pregnancies', 'oocyte donation, obstetric outcome.' Only six retrospective cohort studies met the selection criteria.
Result
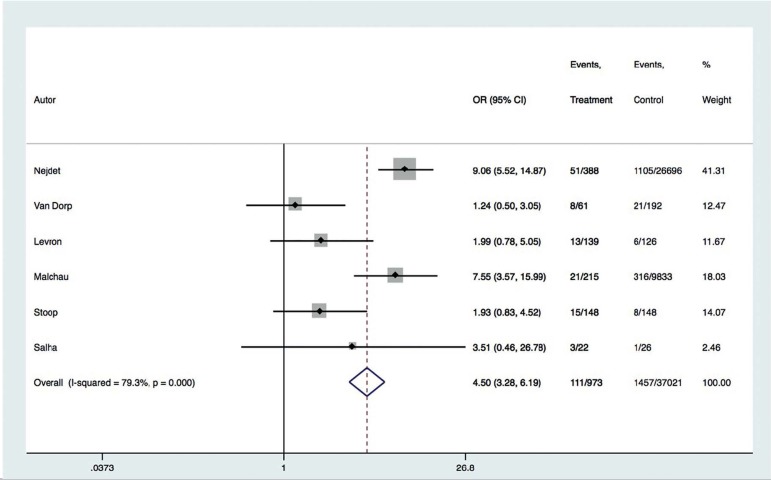
The meta-analysis revealed a statistically significant association between egg donation and onset of preeclampsia (OR 4.50; 95% CI: 3.28-6.19; p<0.0001).
Conclusion
Oocyte donation is associated with increased risk of preeclampsia in singleton pregnancies. Therefore, it is crucial to properly record and assess this finding when egg donation is the chosen assisted reproductive technology to attain pregnancy.
Keywords: oocyte donation, preeclampsia, in vitro fertilization
INTRODUCTION
Estimates indicate that 4.6% of all pregnancies are complicated by pre-eclampsia (PE). Incidence varies depending on maternal age and on whether the mother is in her first pregnancy (Hutcheon et al., 2011). Maternal age and the number of donor oocyte procedures have increased steadily in recent years (Berkowitz et al., 1993; Ferraretti et al., 2013).
Egg recipients provide a unique model of immune response because of the differences in the genetic makeup of mothers and fetuses (Levron et al., 2014). The presence of an immune component in the etiology of preeclampsia has been suggested. While in pregnancies without PE there is a certain tolerance for foreign antigens, in the presence of preeclampsia immune tolerance is hampered in cases of non-autologous egg implantation (Redman & Sargent, 2010).
Many issues have been described in donor egg pregnancies (Van der Hoorn et al., 2010). Previous studies have shown inconsistent results when comparisons were made between complications of in-vitro fertilization (IVF) procedures with and without donor oocytes, for reasons ranging from small simple sizes to inadequate control groups (Abdalla et al., 1998; Krieg et al. 2008; Wiggins & Main 2005).
The purpose of this systematic review and meta-analysis was to determine whether donor oocyte pregnancies have higher incidences of preeclampsia when compared to IVF using autologous oocytes.
MATERIAL AND METHODS
Search
The search for literature was performed in MEDLINE via PubMed and Google Scholar (January 1995 to August 2016) using combinations of the terms "oocyte donation, preeclampsia", "oocyte donation, in vitro fertilization, preeclampsia", "oocyte donation, preeclampsia, outcomes pregnancies", "oocyte donation, obstetric outcome" in all search fields. Only papers written in English were included.
Study selection
Cohort studies were eligible for inclusion in the review. Case reports, case series, and secondary studies were excluded. Studies comparing IVF, using donor eggs or autologous oocytes, were selected for inclusion. Women aged 35 to 49 years with singleton pregnancies and diagnosed with preeclampsia were eligible for inclusion. Studies enrolling patients with gestational hypertension and PE occurring concurrently were excluded.
Data extraction
Two independent unmasked reviewers screened all potentially relevant papers for their titles and abstracts, and retrieved full texts only for the papers meeting the selection criteria. Disagreements were resolved with the involvement of a third reviewer (CO). The references of the selected papers were searched for additional studies. Data was extracted by one of the authors (PB) using a standardized extraction form that included number of cases with and without PE and in vitro fertilization pregnancies with or without donor eggs.
Synthesis of studies
Studies were combined using a fixed-effect model. The statistical analysis included 2x2 contingency tables, from which ORs and their 95% confidence intervals were calculated for donor oocyte pregnancies using the Peto method. Meta-analysis was performed with Stata 11.0 (Statacorp, USA). Additionally, results were shown in a forest plot. Heterogeneity was evaluated using the I2 test and Cochrane's Q test. Heterogeneity was considered significant when p<0.1 and I2>40%.
RESULTS
The search retrieved 193 papers. After manually excluding duplicates, 114 articles remained for screening by title and abstract. Only 18 studies remained for full text revision. Eight studies were excluded because their samples comprised women with multiple pregnancies (Simeone et al., 2012; Klatsky et al., 2010; Le Ray et al. 2012; Söderström-Anttila et al., 1998; Tranquilli et al. 2013; Wiggins & Main 2005; Michalas et al., 1996; Henne et al., 2007); one was excluded due to undifferentiated diagnosis of PE with gestational hypertension (Jeve et al., 2016); two did not record the number of singleton pregnancies with PE (Corradetti et al., 2012; Krieg et al., 2008); and one had a study group that was not homogeneous for oocyte donation (Porreco et al., 2005). Additionally, references from the selected papers were checked for new unidentified studies. In the end, six papers meeting the inclusion criteria were considered in the meta-analysis (Nejdet et al., 2016; Van Dorp et al., 2014; Levron et al., 2014; Malchau et al., 2013; Stoop et al., 2012; Salha et al., 1999). The included papers featured retrospective cohort studies. The risk of PE was adjusted for maternal age and parity; in two studies, additional adjustments were made for fetal gender (Malchau et al., 2013; Stoop et al., 2012); and in one study adjustments were made for tobacco use and BMI (Nejdet et al., 2016).
The six selected studies evinced an association between donor oocytes and preeclampsia (PE) (37,994 pregnancies with 111 donor oocytes). Nejdet et al. (2016) included cases from 2003 to 2012 from in vitro fertilization clinics. In the donor oocyte group, 13.14% (51/338) had PE, whereas in the control group 4.14% (1.105/26.696) presented PE (OR 9.059; 95% confidence interval (CI): 5.518-14.874). Van Dorp et al. (2014) included cases from the Dutch Perinatal Register between 1992 and 2009. In the donor oocyte group, 13.11% (8/61) presented PE, while 10.94% (21/192) presented PE in the control group (OR 1.238; 95% CI: 0.502-3.053). Levron et al. (2014) included cases from 2005 to 2011. In the donor oocyte group, 9.35% (13/139) showed PE, while in the control group 4.76% (6/126) had PE (OR 1.99; 95% CI: 0.782-5.052). Malchau et al. (2013) studied cases from 1995 to 2010 from the Danish IVF register. In the donor oocyte group, 9.76% (21/215) had PE whereas in the control group 3.21% (316/9.833) had PE (OR 7.55; 95% CI: 3.565-15.993). Stoop et al. (2012) analyzed cases from the Brussels center for reproductive medicine between 1999 and 2008. In the donor oocyte group, 15 of 148 patients (10.13%) had preeclampsia (OR 1.930; 95% CI: 0.825- 4.515). Salha et al. (1999) investigated cases at the St. James's University Hospital in Leeds. In the donor oocyte group, 13.63% (3/22) had PE, versus 3.8% (1/26) in the control group (OR 3.51; 95% CI: 0.459 -26.781) (Table 1).
Table 1.
Characteristics of included studies
| Author, year | Methods | Participants, period | Findings |
|---|---|---|---|
| Nejdet, 2016 | Retrospective cohort study | Women from IVF Swedish clinics, from 2003 to 2012 | Donor oocyte group consisted of 388 patients, 51 with PE (13.14%). In the control group, 1,105/26,696 (4.14%) had PE. OR 9.059 (95% CI:5.518 to 14.874). Weight: 41.31. |
| Van Dorp, 2014 | Retrospective cohort study | Women from the Dutch Perinatal Register, from 1992 to 2009 | Study group consisted of 61 patients with singleton pregnancies. 8 out of 61 had PE (13.11%). The control group had 21/192 (10.94%) cases of PE. OR 1.238 (95% CI:0.502 to 3.053). Weight 12.47. |
| Levron, 2014 | Retrospective cohort study | From 2005 to 2011. | 13 of 139 patients in the donor oocyte group had PE (9.35%). In the autologous oocyte group, 6 of 126 had PE (4.76%). OR 1.988 (95% CI:0.782 to 5.052). Weight 11.67. |
| Malchau, 2013 | Retrospective cohort study | Women from the Danish in vitro fertilization register, from 1995 to 2010. | The donor oocyte group included 215 patients and 21 cases of PE (9.76%). Control group had 316/9.833 (3.21%) with PE. OR 7.551 (95% CI:3.565 to 15.993). Weight 18.03. |
| Stoop, 2012 | Retrospective cohort study | Matched pair-analysis for age, ethnicity, parity and plurality from the Centre for Reproductive Medicine,Brussels. Data obtained from 1999 to 2008. | Donor oocyte had 15 of 148 pregnant women diagnosed with PE (10.13%). Control group had 8 of 148 (5.4%) with PE. OR 1.930 (95% CI:0.825 to 4.515). Weight 14.07. |
| Salha, 1999 | Retrospective cohort study | Women from St. James's University Hospital, Leeds(UK), from 1992 to 1997 | Donor oocyte group had 3 of 22 patients diagnosed with PE (13.63%). In the control group, only 1 pregnant woman of 26 was diagnosed with PE (3.8%). OR 3.508 (95% CI:0.459 to 26.781). Weight 2.46. |
Preeclampsia was present in 11.5% of the pregnant patients with donor oocytes (n=111), versus 3.9% (n=1,457) of the individuals with autologous oocytes. After the meta-analysis, women who conceived using donor oocytes showed a significant increment in the risk of preeclampsia (RR 2.62; 95% CI: 2.13-3.21) (Figure 1). In general, heterogeneity across studies was assessed as not relevant (p=0.175; I2=34.9%).
Figure 1.
Forest plot
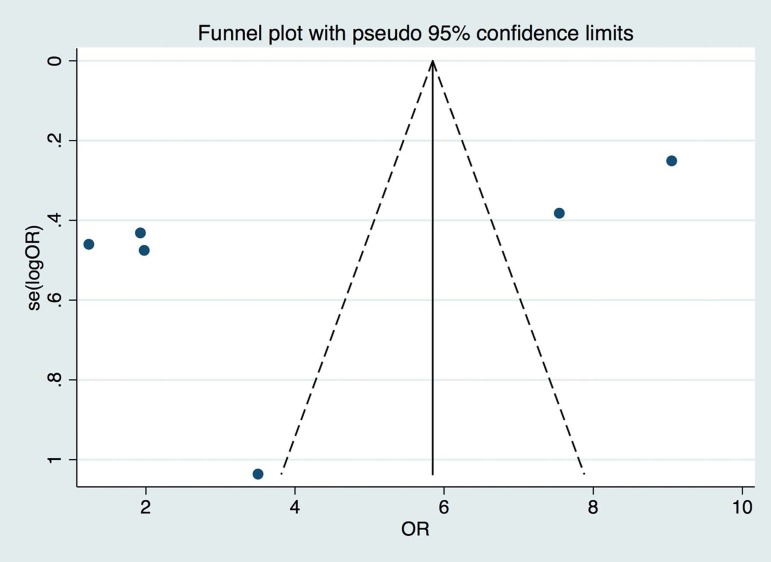
Publication bias was assessed using a funnel plot (Figure 2), and significant scatter of effect size and study size was found in both directions.
Figure 2.
Funnel Plot
DISCUSSION
The purpose of this systematic review and meta-analysis was to determine whether donor oocyte pregnancies were associated with increased risk of preeclampsia. In this review, a summary of six articles comparing the frequency of preeclampsia according to oocyte origin - autologous or donor - was performed. The findings revealed a significant increase in preeclampsia when donor oocytes were used.
A major strength of this study was that it focused exclusively on studies that compared IVF patients with oocyte origin as the variable of interest. Another important feature to be considered is that only singleton pregnancies were incorporated; maternal age and parity were accounted for in the analysis. A study limitation is the lack of information on the underlying causes for choosing of IVF with or without donor eggs, since the etiology of infertility might have been an independent risk factor for preeclampsia. All included papers featured retrospective cohort studies, which lack methodological robustness.
The etiology of preeclampsia in donor oocyte pregnancies is yet to be clarified. An immune theory has been postulated based on the allogenicity of the fetus in relation to the mother. In the implantation phase of pregnancy, the uterine decidua is invaded by trophoblast cells expressing HLA-C, a ligand of the immunoglobulin-type receptor of natural killer (NK) cells. NK cells facilitate the neovascularization of the decidua through proangiogenic and endothelial factors, which in turn modulate the adaptive changes of the uterine spiral arteries (Blázquez et al., 2016). When this process unfolds appropriately, adequate blood flow to the fetus is guaranteed. Fetal HLA-C differs from maternal HLA-C because it contains paternal alleles. When a donor egg is used, fetal HLA-C is even less recognizable by the maternal immune system, as it is completely allogeneic. This can disturb the blood flow to the placenta and, in turn, facilitate the onset of certain disorders such as preeclampsia and intrauterine growth restriction (Klatsky et al., 2010; Madeja et al., 2011; Hiby et al., 2004). The role of acetylsalicylic acid in preeclampsia prevention in women given donor oocytes is yet to be elucidated.
The evidence summarized in this paper revealed an association between oocyte origin and incidence of preeclampsia in singleton pregnancies from IVF. We believe that this study will allow physicians and patients to make informed decisions about the fertilization procedures available needed to attain reproductive success.
Footnotes
CONFLICT OF INTERESTS
No conflict of interest has been declared.
REFERENCES
- Abdalla HI, Billett A, Kan AK, Baig S, Wren M, Korea L, Studd JW. Obstetric outcome in 232 ovum donation pregnancies. Br J Obstet Gynaecol. 1998;105:332–337. doi: 10.1111/j.1471-0528.1998.tb10096.x. [DOI] [PubMed] [Google Scholar]
- Berkowitz GS, Skovron ML, Lapinski RH, Berkowitz RL. Does delayed childbearing increase risk? JAMA. 1993;269:745–746. doi: 10.1001/jama.1993.03500060045020. [DOI] [PubMed] [Google Scholar]
- Blázquez A, García D, Rodríguez A, Vassena R, Figueras F, Vernaeve V. Is oocyte donation a risk factor for preeclampsia? A systematic review and meta-analysis. J Assist Reprod Genet. 2016;33:855–863. doi: 10.1007/s10815-016-0701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corradetti A, Talebi Chahvar S, Biondini V, Giannubilo SR, Tranquilli AL. PP093 Maternal and fetal outcomes in oocyte donor pregnancies. Pregnancy Hypertens. 2012;2:290–291. doi: 10.1016/j.preghy.2012.04.204. [DOI] [PubMed] [Google Scholar]
- Ferraretti AP, Goossens V, Kupka M, Bhattacharya S, de Mouzon J, Castilla JA, Erb K, Korsak V, Nyboe Andersen A, European IVF-Monitoring. Consortium for the European Society of Human Reproduction and Embryology Assisted reproductive technology in Europe, 2009: results generated from European registers by ESHRE. Hum Reprod. 2013;28:2318–2331. doi: 10.1093/humrep/det278. [DOI] [PubMed] [Google Scholar]
- Henne MB, Zhang M, Paroski S, Kelshikar B, Westphal LM. Comparison of obstetric outcomes in recipients of donor oocytes vs. women of advanced maternal age with autologous oocytes. J Reprod Med. 2007;52:585–590. [PubMed] [Google Scholar]
- Hiby SE, Walker JJ, O'Shaughnessy KM, Redman CW, Carrington M, Trowsdale J, Moffett A. Combinations of maternal KIR and fetal HLA-C genes influence the risk of preeclampsia and reproductive success. J Exp Med. 2004;200:957–965. doi: 10.1084/jem.20041214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutcheon JA, Lisonkova S, Joseph KS. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol. 2011;25:391–403. doi: 10.1016/j.bpobgyn.2011.01.006. [DOI] [PubMed] [Google Scholar]
- Jeve YB, Potdar N, Opoku A, Khare M. Three-arm age-matched retrospective cohort study of obstetric outcomes of donor oocyte pregnancies. Int J Gynaecol Obstet. 2016;133:156–158. doi: 10.1016/j.ijgo.2015.09.024. [DOI] [PubMed] [Google Scholar]
- Klatsky PC, Delaney SS, Caughey AB, Tran ND, Schattman GL, Rosenwaks Z. The role of embryonic origin in preeclampsia: a comparison of autologous in vitro fertilization and ovum donor pregnancies. Obstet Gynecol. 2010;116:1387–1392. doi: 10.1097/AOG.0b013e3181fb8e59. [DOI] [PubMed] [Google Scholar]
- Krieg SA, Henne MB, Westphal LM. Obstetric outcomes in donor oocyte pregnancies compared with advanced maternal age in in vitro fertilization pregnancies. Fertil Steril. 2008;90:65–70. doi: 10.1016/j.fertnstert.2007.06.014. [DOI] [PubMed] [Google Scholar]
- Le Ray C, Scherier S, Anselem O, Marszalek A, Tsatsaris V, Cabrol D, Goffinet F. Association between oocyte donation and maternal and perinatal outcomes in women aged 43 years or older. Hum Reprod. 2012;27:896–901. doi: 10.1093/humrep/der469. [DOI] [PubMed] [Google Scholar]
- Levron Y, Dviri M, Segol I, Yerushalmi GM, Hourvitz A, Orvieto R, Mazaki-Tovi S, Yinon Y. The 'immunologic theory' of preeclampsia revisited: a lesson from donor oocyte gestations. Am J Obstet Gynecol. 2014;211:383.e1–383.e5. doi: 10.1016/j.ajog.2014.03.044. [DOI] [PubMed] [Google Scholar]
- Madeja Z, Yadi H, Apps R, Boulenouar S, Roper SJ, Gardner L, Moffett A, Colucci F, Hemberger M. Paternal MHC expression on mouse trophoblast affects uterine vascularization and fetal growth. Proc Natl Acad Sci U S A. 2011;108:4012–4017. doi: 10.1073/pnas.1005342108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malchau SS, Loft A, Larsen EC, Aaris Henningsen AK, Rasmussen S, Andersen AN, Pinborg A. Perinatal outcomes in 375 children born after oocyte donation: a Danish national cohort study. Fertil Steril. 2013;99:1637–1643. doi: 10.1016/j.fertnstert.2013.01.128. [DOI] [PubMed] [Google Scholar]
- Michalas S, Loutradis D, Drakakis P, Milingos S, Papageorgiou J, Kallianidis K, Koumantakis E, Aravantinos D. Oocyte donation to women over 40 years of age: pregnancy complications. Eur J Obstet Gynecol Reprod Biol. 1996;64:175–178. doi: 10.1016/0301-2115(95)02335-6. [DOI] [PubMed] [Google Scholar]
- Nejdet S, Bergh C, Källén K, Wennerholm UB, Thurin-Kjellberg A. High risks of maternal and perinatal complications in singletons born after oocyte donation. Acta Obstet Gynecol Scand. 2016;95:879–886. doi: 10.1111/aogs.12904. [DOI] [PubMed] [Google Scholar]
- Porreco RP, Harden L, Gambotto M, Shapiro H. Expectation of pregnancy outcome among mature women. Am J Obstet Gynecol. 2005;192:38–41. doi: 10.1016/j.ajog.2004.07.035. [DOI] [PubMed] [Google Scholar]
- Redman CW, Sargent IL. Immunology of pre-eclampsia. Am J Reprod Immunol. 2010;63:534–543. doi: 10.1111/j.1600-0897.2010.00831.x. [DOI] [PubMed] [Google Scholar]
- Salha O, Sharma V, Dada T, Nugent D, Rutherford AJ, Tomlinson AJ, Philips S, Allgar V, Walker JJ. The influence of donated gametes on the incidence of hypertensive disorders of pregnancy. Hum Reprod. 1999;14:2268–2273. doi: 10.1093/humrep/14.9.2268. [DOI] [PubMed] [Google Scholar]
- Simeone S, Rambaldi MP, Ottanelli S, Serena C, Mello G, Mecacci F. PP109. Risk of preeclampsia in homologous and oocyte donation IVF pregnancies. Pregnancy Hypertens. 2012;2:298–298. doi: 10.1016/j.preghy.2012.04.220. [DOI] [PubMed] [Google Scholar]
- Söderström-Anttila V, Tiitinen A, Foudila T, Hovatta O. Obstetric and perinatal outcome after oocyte donation: comparison with in-vitro fertilization pregnancies. Hum Reprod. 1998;13:483–490. doi: 10.1093/humrep/13.2.483. [DOI] [PubMed] [Google Scholar]
- Stoop D, Baumgarten M, Haentjens P, Polyzos NP, De Vos M, Verheyen G, Camus M, Devroey P. Obstetric outcome in donor oocyte pregnancies: a matched-pair analysis. Reprod Biol Endocrinol. 2012;10:42–42. doi: 10.1186/1477-7827-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tranquilli AL, Biondini V, Talebi Chahvar S, Corradetti A, Tranquilli D, Giannubilo S. Perinatal outcomes in oocyte donor pregnancies. J Matern Fetal Neonatal Med. 2013;26:1263–1267. doi: 10.3109/14767058.2013.777422. [DOI] [PubMed] [Google Scholar]
- van der Hoorn ML, Lashley EE, Bianchi DW, Claas FH, Schonkeren CM, Scherjon SA. Clinical and immunologic aspects of egg donation pregnancies: a systematic review. Hum Reprod Update. 2010;16:704–712. doi: 10.1093/humupd/dmq017. [DOI] [PubMed] [Google Scholar]
- van Dorp W, Rietveld AM, Laven JS, van den Heuvel-Eibrink MM, Hukkelhoven CW, Schipper I. Pregnancy outcome of non-anonymous oocyte donation: a case-control study. Eur J Obstet Gynecol Reprod Biol. 2014;182:107–112. doi: 10.1016/j.ejogrb.2014.09.019. [DOI] [PubMed] [Google Scholar]
- Wiggins DA, Main E. Outcomes of pregnancies achieved by donor egg in vitro fertilization--a comparison with standard in vitro fertilization pregnancies. Am J Obstet Gynecol. 2005;192:2002–2008. doi: 10.1016/j.ajog.2005.02.059. [DOI] [PubMed] [Google Scholar]