Abstract
Purpose
The purpose of this study is to analyze the sperm morphology of a Chinese man affected with multiple morphological abnormalities of the sperm flagella (MMAF) and observe the intracytoplasmic sperm injection (ICSI) outcome.
Methods
A Chinese man was diagnosed with multiple morphological abnormalities of the sperm flagella by semen analysis and electron microscopy. Testicular spermatozoa were injected intracytoplasmically, and the following ICSI results were observed.
Results
All the spermatozoa from his ejaculate were immotile and morphologically abnormal in the flagellum. In transmission electron microscopy assays, most spermatozoa showed disorganized fibrous sheath, accompanied by distortion of various cytoskeletal components, and missing of the central pair microtubules. Testicular sperm was injected to the oocytes in two ICSI cycles, with fertilization rates of 45.5 and 40.0%. Finally, a healthy female infant was delivered at the second ICSI cycle.
Conclusions
Fertilization and pregnancy could be achieved by intracytoplasmic sperm injection, regardless of severe flagellar defects. ICSI is effective for MMAF-affected man, and testicular sperm is an alternative when no motile sperm is available.
Keywords: Teratozoospermia, Intracytoplasmic sperm injection, Sperm tail, Testicular sperm, Multiple morphological abnormalities of the sperm flagella
Introduction
Multiple morphological abnormalities of the sperm flagella (MMAF) is a rare condition leading to male infertility, presenting with severe asthenozoospermia, and teratozoospermia in sperm tails [1, 2]. MMAF is also known as dysplasia of the fibrous sheath (DFS), which was introduced by Chemes in 1987 [3]. Other denominations include tail stump syndrome and short-tailed spermatozoa [4, 5]. The affected spermatozoa present combinations of sperm flagellar anomalies (absent, short, coiled, bent, and irregular width), and ultrastructure observation disclosed unsuccessful assembly of sperm flagella with a key phenotype of central-pair microtubules absence in the axoneme [1, 6]. MMAF is a syndrome caused by genetic defects, and as far as known, DNAH1 is the main causative gene [2, 7].
At present, no effective experimental treatment is available; however, successful intracytoplasmic sperm injection (ICSI) pregnancies are reported by several authors [5, 8, 9]. The ICSI outcomes of six Chinese men affected with MMAF were also presented in our previous manuscript [10], and infants were delivered in the following ICSI cycles. A successful ICSI result using testicular sperm will be reported in this manuscript.
Materials and methods
Patient
A 33-year-old Han Chinese man was seeking treatment for primary infertility for 4 years at Suzhou Hospital Affiliated to Nanjing Medical University. His parents were non-consanguineous and they had two early abortions. So the patient was the only child of the family. His three uncles and two aunts were fertile. No apparent organic anomalies were found by physical examination and ultrasound examination in the male reproductive system, and no significant respiratory symptoms were observed. The serum follicle-stimulating hormone (FSH, 4.77 mIU ml−1), luteinizing hormone (LH, 4.82 mIU ml−1), and testosterone (T, 3.08 ng ml−1) were within normal ranges, and his lymphocyte karyotype was 46, XY. After repeated semen analyses under light microscope and electron microscope, he was diagnosed as MMAF. The couple signed an informed consent for the ICSI procedure, and our hospital ethics committee approved this study.
Semen analysis
Semen samples were evaluated according to the World Health Organization guidelines. Sperm morphology was analyzed on slides under a microscope after modified Papanicolaou staining, and at least 200 spermatozoa were examined. Transmission electron microscopy (TEM) assessment was carried out as previously introduced [7]. The sperm DNA integrity was tested by flow cytometry (Navios, Beckman Coulter, CA, USA) using the sperm chromatin structure assay (SCSA). A minimum of 10,000 events were recorded. The sperm samples were prepared according to the regular protocol. Single-stranded nucleic acids in abnormal spermatozoa combined with acridine orange and emitted orange fluorescence. Normal sperm chromatin which is double-stranded combined with acridine orange and emitted green fluorescence. The percentage of sperm with DNA fragmentation is expressed as DNA fragmentation index (DFI) from the flow cytometer software. The reference value of DFI is below 30%.
ICSI procedures
A long protocol for ovulation induction was administrated to his 27-year-old wife. After pituitary desensitization with gonadotropin-releasing hormone agonist, recombinant follicle-stimulating hormone was administrated to stimulate follicular development. When at least two dominant follicles reached a diameter of 18 mm, 250 μg recombinant human chorionic gonadotropin (hCG, Ovidrel, Merck-Serono) was injected. Oocytes were retrieved 36 h after hCG administration, and metaphase II oocytes were fertilized 4–6 h after retrieval. Transcervical embryo transfer was performed 72 h after the oocytes were retrieved. Pregnancy was confirmed by two hCG tests conducted 12 days after embryo transfer, and clinical pregnancy was determined by a fetal heartbeat on ultrasound screening after 35 days.
Results
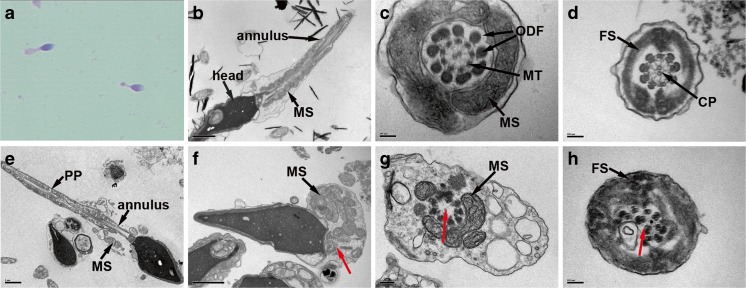
Several semen analyses showed sperm concentrations of 5.6–20.2 million ml−1, volume of 1.0–2.4 ml, with seminal pH at 7.4. But all the sperm were immotile, and the majority was abnormal in the sperm flagellum. The sperm DNA fragmentation index was 15.8%. All spermatozoa presented abnormal flagellar morphology under light microscopy after modified Papanicolaou staining (Fig. 1a). The sperm flagellar phenotype was in accordance with MMAF [1], showing absent 20.0%, short 38.5%, coiled 30.5%, irregular 5.5%, and bent 5.5%, respectively. A normal spermatozoon is composed of a sperm head and flagellum, and the flagellum has a unique 9 + 2 arrangement of microtubules within the flagellar axoneme. TEM observation from an individual with normal semen parameters displayed normal flagellar ultrastructure (Fig. 1b–d). The MMAF-affected man presented poorly assembled flagella by TEM assessment. Both longitudinal and cross sections showed disorganized fibrous sheath and distortion of various cytoskeletal components, with central pair of microtubules mostly absent, but the normal centrosome complex was observed (Fig. 1e–h).
Fig. 1.
Morphological observation on sperm flagella. a Light microscopy observation of the man affected with multiple morphological abnormalities of the sperm flagella (MMAF) shows short and thick sperm flagella. Transmission electron microscopy (TEM) observation on morphologically normal spermatozoa (b–d). b A longitudinal section showed regular arranged flagellar mitochondrial sheath (MS) in the middle piece and normally formed annulus. c A cross section at middle piece displayed a normal axoneme with a 9 + 2 arrangement of nine peripheral microtubules (MT) and central pair of microtubules (CP), surrounded by nine outer dense fibers (ODF) and MS. d A cross section at principal piece (PP) showed a well-organized axoneme surrounded by normal fibrous sheath (FS). TEM observation on the MMAF affected man demonstrated several ultrastructure anomalies in the flagella (e–h). e The MS was badly assembled, and the annulus was abnormally located. In addition, the FS in principal piece was thickened and unsmooth. f The MS together with all other flagellar structures was unassembled, but the proximal centriole and the segmented columns were normally formed (red arrow). g The CP was absent at middle piece (red arrow), and the MS was incomplete. h The section at principal piece showed disorganized microtubules (red arrow) and thickened FS. Scale bars = 1 μm (b, e, f), 0.1 μm (c, d, h), and 0.2 μm (g)
On the oocytes retrieval day, no motile sperm was found in the ejaculate. Testicular spermatozoa were obtained by needle aspiration, which showed that most were tailless and 100% immotile. Testicular sperm with comparatively normal morphology were injected to the oocytes in the two successive ICSI cycles. The first cycle achieved a 45.5% (5/11) fertilization rate and a failed pregnancy after embryo transfer. The second cycle obtained a 40.0% (4/10) fertilization rate and successful pregnancy after one blastocyst transfer. A fetal heartbeat was detected by ultrasound at the 32nd day after transfer. A healthy, 3150-g female infant was delivered at 40 weeks of gestation. The ICSI results are summarized in Table 1.
Table 1.
Intracytoplasmic sperm injection outcomes of the MMAF couple
| Cycle1 | Cycle2 | |
|---|---|---|
| No. oocytes retrieved | 13 | 10 |
| Metaphase II oocytes | 11 | 10 |
| Sperm origin | Testis | Testis |
| Injected oocytes | 11 | 10 |
| Normal fertilization | 5 | 4 |
| Good quality embryos | 4 | 2 |
| Embryo scores | ||
| Day 2 | 411,412,421,411,211 | 421,622,411,323 |
| Day 3 | 902,812(T),811,802(T),411 | 821,1022,811,422 |
| Day 5 | 6CC,−,3BB(T),-,Deg | 3AB(T),deg, 3BC,Deg |
| No. embryos transferred | 3 | 1 |
| No. transfers | 2 | 1 |
| Clinical pregnancy | 0 | 1 |
| Delivery | 0 | 1 |
MMAF multiple morphological abnormalities of the sperm flagella, Deg degeneration, T transferred
The embryo scores are cell number, fragmentation, and symmetry, respectively, according to the criterion by Racowsky [11]
Discussion
Nonspecific flagellar anomalies are common among men with severe asthenozoospermia, which could be secondary to various reproductive conditions [5, 12]. However, nonspecific anomalies have no definite pattern and fluctuate in their incidence during treatment [13]. MMAF is one kind of specific sperm ultrastructural anomalies. The tailless testicular sperm of this patient confirms that MMAF is not secondary to a hostile epididymal environment, but occurs in the process of spermatogenesis. The axoneme is the core of the sperm flagellum, and some of the defects could cause certain forms of infertility [14]. The ultrastructure examination of spermatozoa is an important evidence to diagnose MMAF and other ciliopathies [12].
ICSI provides an effective therapeutic method for patients with sperm flagellar defects, including MMAF, but selecting live sperm when no motile sperm are present is crucial for successful ICSI [15, 16]. In our previous observation, the viability of MMAF spermatozoa varied from 9.0 to 80.0% [1]. A randomly selected immotile ejaculated spermatozoa would negatively influence the reproductive results [17, 18]. When no motile sperm is present, the hypoosmotic swelling (HOS) test is valuable to identify live sperm [19, 20]. Given that sperm tails of the MMAF man are severely distorted, HOS test would be inaccurate. Testicular sperm was effective for ICSI in case of 100% immotility [21–23]. Injection of testicular sperm from MMAF-affected man could also obtain successful fertilization and delivery [24]. One more successful ICSI using testicular sperm is reported in this manuscript. Although failed ICSI outcomes have been reported [25], most MMAF patients present an overall good prognosis following ICSI [4, 5, 8, 9, 24, 26, 27].
In conclusion, ICSI is an effective method to achieve a pregnancy in those men affected with MMAF, and testicular sperm is an alternative when no motile sperm is available. Although the MMAF men obtained comparable ICSI outcomes despite of carrying DNAH1 mutations or not [26], the pathogenic gene should be disclosed for further genetic counseling. Recently, our group identified new MMAF causative genes CFAP43 and CFAP44, and more causative genes would be disclosed through whole exome sequencing (WES) technology [7].
Funding
This study was funded by Maternal and Child Health Research Project of Jiangsu Province (F201521) and Suzhou Key laboratory for male reproduction (SZS201718).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no competing interest.
Contributor Information
Yongle Xu, Email: chenyanzhu2009@sina.cn.
Hong Li, Email: hongliszivf@163.com.
References
- 1.Yang SM, Li HB, Wang JX, Shi YC, Cheng HB, Wang W, et al. Morphological characteristics and initial genetic study of multiple morphological anomalies of the flagella in China. Asian J Androl. 2015;17:513–515. doi: 10.4103/1008-682X.138190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ben Khelifa M, Coutton C, Zouari R, Karaouzene T, Rendu J, Bidart M, et al. Mutations in DNAH1, which encodes an inner arm heavy chain dynein, lead to male infertility from multiple morphological abnormalities of the sperm flagella. Am J Hum Genet. 2014;94:95–104. doi: 10.1016/j.ajhg.2013.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chemes HE, Brugo S, Zanchetti F, Carrere C, Lavieri JC. Dysplasia of the fibrous sheath: an ultrastructural defect of human spermatozoa associated with sperm immotility and primary sterility. Fertil Steril. 1987;48:664–669. doi: 10.1016/S0015-0282(16)59482-5. [DOI] [PubMed] [Google Scholar]
- 4.Stalf T, Sanchez R, Kohn FM, Schalles U, Kleinstein J, Hinz V, et al. Pregnancy and birth after intracytoplasmic sperm injection with spermatozoa from a patient with tail stump syndrome. Hum Reprod. 1995;10:2112–2114. doi: 10.1093/oxfordjournals.humrep.a136244. [DOI] [PubMed] [Google Scholar]
- 5.Chemes HE, Alvarez SC. Tales of the tail and sperm head aches: changing concepts on the prognostic significance of sperm pathologies affecting the head, neck and tail. Asian J Androl. 2012;14:14–23. doi: 10.1038/aja.2011.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coutton C, Escoffier J, Martinez G, Arnoult C, Ray PF. Teratozoospermia: spotlight on the main genetic actors in the human. Hum Reprod Update. 2015;21:455–485. doi: 10.1093/humupd/dmv020. [DOI] [PubMed] [Google Scholar]
- 7.Tang S, Wang X, Li W, Yang X, Li Z, Liu W, et al. Biallelic mutations in CFAP43 and CFAP44 cause male infertility with multiple morphological abnormalities of the sperm flagella. Am J Hum Genet. 2017;100:854–864. doi: 10.1016/j.ajhg.2017.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olmedo SB, Nodar F, Chillik C, Chemes HE. Successful intracytoplasmic sperm injection with spermatozoa from a patient with dysplasia of the fibrous sheath and chronic respiratory disease. Hum Reprod. 1997;12:1497–1499. doi: 10.1093/humrep/12.7.1497. [DOI] [PubMed] [Google Scholar]
- 9.Olmedo SB, Rawe VY, Nodar FN, Galaverna GD, Acosta AA, Chemes HE. Pregnancies established through intracytoplasmic sperm injection (ICSI) using spermatozoa with dysplasia of fibrous sheath. Asian J Androl. 2000;2:125–130. [PubMed] [Google Scholar]
- 10.Yang SM, Yang XY, Ding Y, Li H, Wang W, Liu JY, et al. Intracytoplasmic sperm injection outcomes in Chinese men with multiple morphological abnormalities of sperm flagella. Asian J Androl. 2016;18:809–811. doi: 10.4103/1008-682X.150038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Racowsky C, Ohno-Machado L, Kim J, Biggers JD. Is there an advantage in scoring early embryos on more than one day. Hum Reprod. 2009;24:2104–2113. doi: 10.1093/humrep/dep198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chemes HE, Olmedo SB, Carrere C, Oses R, Carizza C, Leisner M, et al. Ultrastructural pathology of the sperm flagellum: association between flagellar pathology and fertility prognosis in severely asthenozoospermic men. Hum Reprod. 1998;13:2521–2526. doi: 10.1093/humrep/13.9.2521. [DOI] [PubMed] [Google Scholar]
- 13.Chemes EH, Rawe YV. Sperm pathology: a step beyond descriptive morphology. Origin, characterization and fertility potential of abnormal sperm phenotypes in infertile men. Hum Reprod Update. 2003;9:405–428. doi: 10.1093/humupd/dmg034. [DOI] [PubMed] [Google Scholar]
- 14.Linck RW, Chemes H, Albertini DF. The axoneme: the propulsive engine of spermatozoa and cilia and associated ciliopathies leading to infertility. J Assist Reprod Genet. 2016;33:141–156. doi: 10.1007/s10815-016-0652-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nordhoff V. How to select immotile but viable spermatozoa on the day of intracytoplasmic sperm injection? An embryologists view. Andrology. 2015;3:156–62. [DOI] [PubMed]
- 16.Ortega C, Verheyen G, Raick D, Camus M, Devroey P, Tournaye H. Absolute asthenozoospermia and ICSI: what are the options. Hum Reprod Update. 2011;17:684–692. doi: 10.1093/humupd/dmr018. [DOI] [PubMed] [Google Scholar]
- 17.Nagy ZP, Verheyen G, Tournaye H, Van Steirteghem AC. Special applications of intracytoplasmic sperm injection: the influence of sperm count, motility, morphology, source and sperm antibody on the outcome of ICSI. Hum Reprod. 1998;13(Suppl 1):143–154. doi: 10.1093/humrep/13.suppl_1.143. [DOI] [PubMed] [Google Scholar]
- 18.Vandervorst M, Tournaye H, Camus M, Nagy ZP, Van Steirteghem A, Devroey P. Patients with absolutely immotile spermatozoa and intracytoplasmic sperm injection. Hum Reprod. 1997;12:2429–2433. doi: 10.1093/humrep/12.11.2429. [DOI] [PubMed] [Google Scholar]
- 19.Casper RF, Meriano JS, Jarvi KA, Cowan L, Lucato ML. The hypo-osmotic swelling test for selection of viable sperm for intracytoplasmic sperm injection in men with complete asthenozoospermia. Fertil Steril. 1996;65:972–976. doi: 10.1016/S0015-0282(16)58271-5. [DOI] [PubMed] [Google Scholar]
- 20.Kordus RJ, Price RL, Davis JM, Whitman-Elia GF. Successful twin birth following blastocyst culture of embryos derived from the immotile ejaculated spermatozoa from a patient with primary ciliary dyskinesia: a case report. J Assist Reprod Genet. 2008;25:437–443. doi: 10.1007/s10815-008-9254-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kahraman S, Isik AZ, Vicdan K, Ozgur S, Ozgun OD. A healthy birth after intracytoplasmic sperm injection by using immotile testicular spermatozoa in a case with totally immotile ejaculated spermatozoa before and after Percoll gradients. Hum Reprod. 1997;12:292–293. doi: 10.1093/humrep/12.2.292. [DOI] [PubMed] [Google Scholar]
- 22.Kahraman S, Tasdemir M, Tasdemir I, Vicdan K, Ozgur S, Polat G, et al. Pregnancies achieved with testicular and ejaculated spermatozoa in combination with intracytoplasmic sperm injection in men with totally or initially immotile spermatozoa in the ejaculate. Hum Reprod. 1996;11:1343–1346. doi: 10.1093/oxfordjournals.humrep.a019384. [DOI] [PubMed] [Google Scholar]
- 23.Shulman A, Feldman B, Madgar I, Levron J, Mashiach S, Dor J. In-vitro fertilization treatment for severe male factor: the fertilization potential of immotile spermatozoa obtained by testicular extraction. Hum Reprod. 1999;14:749–752. doi: 10.1093/humrep/14.3.749. [DOI] [PubMed] [Google Scholar]
- 24.McLachlan RI, Ishikawa T, Osianlis T, Robinson P, Merriner DJ, Healy D, et al. Normal live birth after testicular sperm extraction and intracytoplasmic sperm injection in variant primary ciliary dyskinesia with completely immotile sperm and structurally abnormal sperm tails. Fertil Steril. 2012;97:313–318. doi: 10.1016/j.fertnstert.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 25.Ravel C, Chantot-Bastaraud S, Siffroi JP, Escalier D, Antoine JM, Mandelbaum J. Tail stump syndrome associated with chromosomal translocation in two brothers attempting intracytoplasmic sperm injection. Fertil Steril. 2006;86:719.e1–719.e7. doi: 10.1016/j.fertnstert.2005.12.078. [DOI] [PubMed] [Google Scholar]
- 26.Wambergue C, Zouari R, Ben F, Mustapha S, Martinez G, Devillard F, et al. Patients with multiple morphological abnormalities of the sperm flagella due to DNAH1 mutations have a good prognosis following intracytoplasmic sperm injection. Hum Reprod. 2016;31:1164–1172. doi: 10.1093/humrep/dew083. [DOI] [PubMed] [Google Scholar]
- 27.Favero R, Rizzo F, Baccetti B, Piomboni P. Embryo development, pregnancy and twin delivery after microinjection of ‘stump’ spermatozoa. Andrologia. 1999;31:335–338. doi: 10.1046/j.1439-0272.1999.00288.x. [DOI] [PubMed] [Google Scholar]