Abstract
Objective
The aim of this study was to evaluate recent publications and determine the impact of ejaculatory abstinence on semen analysis parameters as well as fertility outcomes.
Methods
This was a systematic review of 28 recent publications. The focus of this study was the impact of abstinence on semen parameters and fertility outcomes in papers published since the year 2000. The specific parameters evaluated were volume, sperm count, motility, morphology, pH, DNA fragmentation rate, viability, and pregnancy or fertilization rates following assisted reproduction.
Results
Twenty-eight recent publications met inclusion criteria. Analysis of publications showed that longer abstinence is associated with increases in semen volume and sperm count. Studies evaluating the effect of abstinence on motility, morphology, and DNA fragmentation rates are contradictory and inconclusive, although a trend appears to exist toward improvements in semen parameters with shorter abstinence. Semen pH was unaffected by abstinence. The majority of publications found no difference in rates of viability with varying abstinence times, although total number of viable sperm increases with increasing abstinence. Some studies evaluating the impact of ejaculatory abstinence on intrauterine insemination (IUI), intracytoplasmic sperm injection (ICSI), and in vitro fertilization (IVF) demonstrated an association between short abstinence and improved outcomes.
Conclusions
The impact of abstinence on sperm quality is complex. While certain semen parameters improve with longer abstinence, others appear to improve with shorter abstinence. No clear recommendations can be made regarding ideal abstinence due to the conflicting nature of current evidence. Going forward, more research is needed to evaluate the impact of abstinence on pregnancy and fertilization rates.
Keywords: Ejaculatory abstinence, Sperm quality, Semen analysis, Infertility, Semen parameters
Introduction
Many factors impact semen parameters for sperm samples used in assisted reproductive procedures. One of the factors affecting semen quality is abstinence time, or the time between ejaculatory events. The World Health Organization (WHO) recommends that for testing and analysis, semen samples should be collected after a minimum of 2 days and a maximum of 7 days of sexual abstinence [1]. Studies have evaluated duration of abstinence and sperm quality to determine if the 2- to 7-day abstinence recommendations yield the highest quality sperm [2–5]. Data have challenged the WHO recommendations, questioning the role of arbitrary abstinence times and occasionally demonstrating improvement of semen parameters after different abstinence intervals [3]. In certain studies, shorter abstinence did not negatively impact sperm quality. Strategies which alter recommended abstinence times could optimize sperm quality. Although current abstinence recommendations are for testing and analysis purposes only, it is possible that varying abstinence could lead to higher clinical rates of conception [4]. While seminal volume may decline with more frequent ejaculatory events, total sperm count, motility, morphology, and vitality may not be significantly affected [5]. However, other findings suggest that short abstinence periods of less than 24 h negatively impact sperm quality [2]. Controversy remains regarding ideal abstinence recommendations. The purpose of this study is to evaluate publications since the year 2000 to determine whether recent scientific literature supports an ideal time frame for sexual abstinence prior to semen analysis, which may have implications for assisted reproductive technologies. This study differs from many retrospective cohort studies addressing this issue by providing a comprehensive summary of recent literature, allowing for a broad perspective on the somewhat contradictory nature of publications related to this topic.
Materials and methods
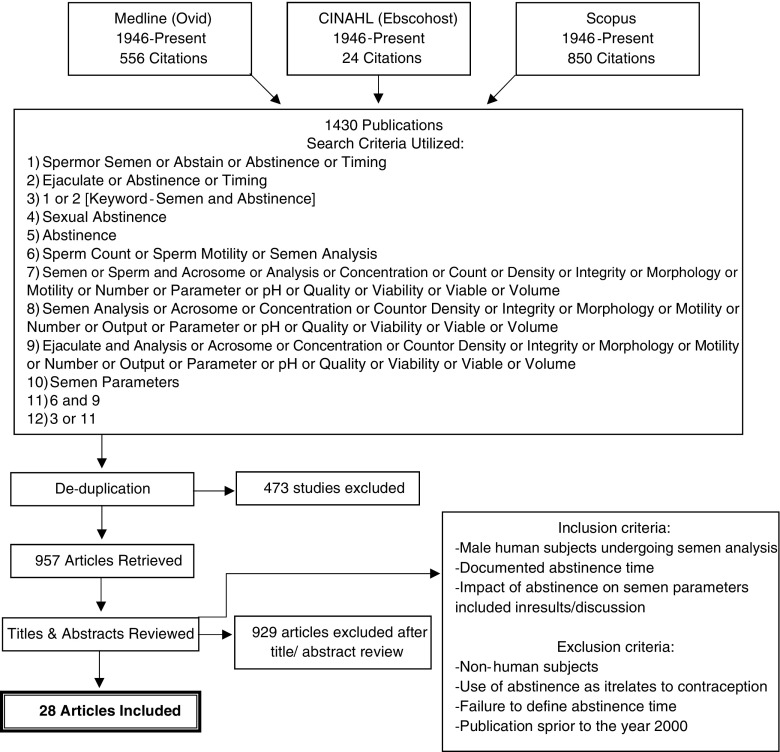
An electronic search was conducted on January 20, 2017, using three databases. The specific databases were Medline, Scopus, and the Current Index to Nursing and Allied Health Literature (CINAHL). An initial search strategy used a combination of the following MeSH terms: semen, abstinence, sexual abstinence, ejaculatory abstinence, semen analysis, sperm count, sperm motility, sperm morphology, semen parameters, semen quality, sperm integrity, and sperm viability. This search strategy yielded 957 de-duplicated search results (see Fig. 1 for details regarding the search strategy).
Fig. 1.
Systematic review search strategy details
Titles and abstracts from the 957 preliminary results were reviewed for relevance. Ultimately, 28 articles were chosen by two individuals to be highly relevant. Individual discussion was held regarding discrepant articles with a decision to include or exclude the study made by the two individuals reviewing the publications. Studies were included when the following criteria were fulfilled: participants were human male subjects who had undergone semen collection with subsequent semen analysis; abstinence time prior to semen collection was assessed as part of the data collection; and the impact of abstinence on semen parameters was included as part of the results of the publication. Studies evaluating men with normal and abnormal semen parameters were included. In order to provide a recent summary of the literature, studies published prior to the year 2000 were excluded. For details regarding the publications selected for inclusion in the systematic review, refer to Table 1.
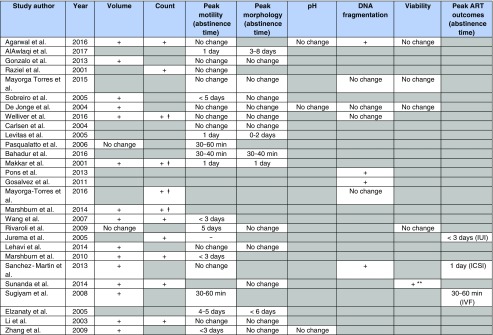
Table 1.
Study details
+ signifies an increase in parameter as abstinence time increases
– signifies a decrease in parameter as abstinence time increases
“No change” signifies no significant difference in parameter with varying abstinence time
A gray box indicates that the specific parameter was not evaluated in the study
*For within-subject testing. Between-subject testing showed decreased motility and worsened morphology with increasing abstinence
**Increase in total number of viable sperm with increased abstinence
ǂStudies which demonstrated a reduction in sperm count with short abstinence
Results
In this systematic review, the effects of abstinence on semen volume, total sperm count (not concentration), motility, morphology, semen pH, DNA fragmentation rate, viability, and pregnancy outcomes following assisted reproductive technology were evaluated.
Semen volume
Seventeen studies included in this review evaluated the impact of abstinence on semen volume (see the study results in Table 1). A summary of key findings based on multiple parameters can be found in Table 2. Fifteen of the 17 studies (88.2%) demonstrated that with longer abstinence, men can achieve statistically significant increases in overall semen volume [4, 6–19]. Using a gradual scale based on specific definitions of abstinence provided by each study, no studies demonstrated decreases in semen volume with longer abstinence times.
Table 2.
Summary of key results based on parameter
| Parameter evaluated | Number of publications | Key results |
|---|---|---|
| Volume | 17 | • 15 out of 17 publications (88.2%): volume increases with longer abstinence • 2 out of 17 publications (11.8%): there is no association between volume and varying abstinence |
| Count | 11 | • 11 out of 11 publications (100%): sperm count increases with longer abstinence. Abstinence of > 5 days is strongly associated with increased sperm count. Abstinence of < 24 h is associated with significant decreases in sperm count |
| Motility | 23 | • Studies only publishing total motile count were excluded • 10 out of 23 publications (43.5%): there was no association noted between abstinence time and motility • 13 out of 23 publications (56.5%): an association was noted between abstinence time and motility 10 out of these 13 publications: peak motility demonstrated after < 3 days abstinence 3 out of these 13 publications: peak motility was noted at 4 or 5 days abstinence |
| Morphology | 16 | • Kruger’s strict criteria for morphology utilized by 1 publication • WHO morphology guidelines utilized by 15 publications • 11 out of 16 publications (68.8%): no differences in morphology were noted based on varying abstinence times • 5 out of 16 publications (31.2%): an association was noted between abstinence time and morphology. Peak morphology ranged from 30 to 40 min to 3–8 days of abstinence. Significant variation was noted between studies |
| Semen pH | 3 | • 3 out of 3 publications (100%): semen pH did not vary based on varying abstinence |
| DNA fragmentation rate | 8 | • 5 publications utilized flow cytometry. 3 publications utilized sperm chromatin dispersion testing • 4 out of 8 publications (50%): no differences in DNA fragmentation rate were noted based on varying abstinence times. All 4 of these publications utilized flow cytometry • 4 out of 8 publications (50%): abstinence of < 24 h was associated with the lowest rates of DNA fragmentation. The 3 publications utilizing sperm chromatin dispersion testing were in this group |
| Viability | 5 | • 4 out of 5 publications (80%): no differences in rates of viability were noted based on varying abstinence • 1 out of 5 publications (20%): the total number of viable sperm increases with abstinence of 6–7 days compared to shorter abstinence |
| Pregnancy outcomes (with ART) |
3 | • 1 study evaluating pregnancy rates with IUI after varying abstinence: the highest pregnancy rates were seen following < 3 days of abstinence • 1 study evaluating pregnancy rates with ICSI after varying abstinence: the highest pregnancy rates were seen following 24 h of abstinence • 1 study evaluating fertilization rates with IVF after varying abstinence: the highest fertilization rates were seen following 30–60 min of abstinence |
Two of the 17 studies (11.8%) did not find statistically significant differences in semen volume with varying abstinence [20, 21]. Of the studies which did not find an association between abstinence time and semen volume, one specifically evaluated oligozoospermic men [20]. While this may represent a unique patient population where abstinence could have less of an impact on semen volume, the study by Sugiyam et al. which is included in this review also evaluated oligozoospermic men and was able to demonstrate that semen volume increased with increasing abstinence [17]. The final study which did not demonstrate a relationship between abstinence time and semen volume was a within-subject comparison of two semen samples collected after a “shorter abstinence” period of 1 to 4 days and a “longer abstinence” period of up to 5 days, but at least 24 h longer than the “shorter abstinence” collection [21]. The structure of this study resulted in many samples differing by only 24 h in abstinence time, which may explain the lack of a statistically significant increase in volume with longer abstinence. Overall, a strong correlation appears to exist between longer abstinence time and increased semen volume. Specifically, abstinence times of greater than 5 days showed significant increases in volume.
Total sperm count
Eleven studies included in this review evaluated the effect of abstinence time on total sperm count (see the results of the relevant studies in Table 1). All of the 11 relevant studies demonstrated that increased total sperm count was associated with longer abstinence time [4, 9–12, 14, 16, 18, 22–24]. It should be noted that all included studies reported total sperm count, not concentration. While the definition of long abstinence time varied based on the specific parameters of each study, a strong direct relationship exists between an abstinence time cutoff of greater than 5 days and increasing total sperm count. Four of the 11 studies evaluated the impact of frequent ejaculation (24 h) and found that total sperm count decreased with daily ejaculation when compared to any longer period of abstinence [9–11, 23]. Due to the previously noted strong direct relationship between increasing abstinence and increasing semen volume, it is logical that total sperm count would also be expected to rise with increasing abstinence.
Motility
Twenty-three publications included in this review evaluated the impact of abstinence on sperm motility rates (Table 1). Studies that reported total motile count but did not report the percentage of motile sperm were excluded in order to eliminate the confounding impact of volume and overall sperm count on this parameter. The effect of abstinence time on motility demonstrated conflicting results overall. Ten of the 23 studies (43.5%) were unable to show significant alterations in motility with varying abstinence times. These ten studies evaluated various populations, including healthy fertile men as well as oligozoospermic men [4–6, 8, 9, 13, 15, 18, 22, 25]. One of the studies demonstrating no impact of abstinence time on motility specifically evaluated progressive motility [5]. The remaining nine studies evaluated total motility as it relates to abstinence time.
Thirteen of the 23 publications evaluating motility (56.5%) demonstrated a significant effect of abstinence on motility. While the structure of the individual studies varied in terms of specific abstinence time evaluated, when an association was demonstrated, a trend was seen toward improved motility with shorter abstinence times. Using an abstinence time cutoff of less than 3 days, ten of the publications included in this review specifically noted peak motility in samples within this time frame [3, 10, 12, 14, 17, 19, 20, 24, 26, 27]. Three of the 13 studies demonstrating an association between abstinence time and motility noted peak motility following 4 or 5 days of abstinence [7, 21, 28]. No studies demonstrated peak motility at an abstinence time greater than 5 days. Progressive motility was evaluated in five of the 13 studies which demonstrated an association between abstinence time and motility, with peak progressive motility noted after abstinence of 3 days or less in four of the five studies [12, 19, 24, 27, 28]. The remaining eight studies which demonstrated an impact between abstinence time and motility evaluated total motility.
Morphology
Sixteen studies included in this review evaluated the effects of abstinence time on morphology [3, 5–10, 13, 16, 18, 19, 21, 25–28] (see Table 1). One study evaluated morphology using Kruger’s strict criteria [9]. The remaining studies used the World Health Organization criteria for evaluation of morphology. Eleven of the 16 studies which evaluated this issue (68.8%) did not show significant differences in morphology with varying abstinence times [5–9, 13, 16, 18, 19, 21, 25]. These 11 studies included primarily healthy men or men with suspected infertility. Importantly, of the studies which failed to show a difference in morphology based on varying abstinence times, none included populations with known abnormal sperm parameters such as oligozoospermia or asthenozoospermia, possibly suggesting that changes in morphology based on varying abstinence may be minimal in the healthy male population.
Only five of the 16 publications (31.2%) identified an association between abstinence time and morphology [3, 10, 26–28]. No clear consensus was apparent regarding an ideal abstinence time to maximize morphology. Due to methodologic differences between relevant studies, peak morphology was reported at various abstinence times. Abstinence times associated with peak morphology ranged from very brief abstinence of 30 to 40 min to much longer abstinence times of 3 to 8 days [26, 27]. While studies which failed to demonstrate a difference in morphology based on abstinence time were primarily performed in healthy men or populations without previously known semen abnormalities, three of the studies demonstrating changes in morphology based on abstinence time were performed in oligozoospermic men [3, 26, 27]. While it is difficult to draw definitive conclusions based on this limited data, men with abnormal semen parameters such as oligozoospermia may be a specific population that demonstrates a difference in morphology with varying abstinence.
Additional parameters
In addition to the parameters of volume, count, motility, and morphology, many studies included in this review evaluated the effect of abstinence on other semen parameters or outcomes. The specific outcomes which will be discussed below are semen pH, DNA fragmentation, viability, and pregnancy outcomes.
Three studies evaluated the impact of abstinence time on semen pH [4, 8, 19]. Uniformly, these studies demonstrated that there was no effect on pH with varying abstinence times (see Table 1). While there is no mechanistic explanation to suggest semen pH should be altered with varying abstinence times, pH was chosen as an included parameter since the acid-base environment of semen is known to have a profound effect on semen quality [29]. The studies included in this review are reassuring that despite variations in abstinence time, pH appears to remain stable.
One of the overall measures of semen stability is the rate of DNA fragmentation, which was evaluated in eight of the publications included in this review [2, 4, 5, 9, 15, 23, 30, 31] (see study results in Table 1). Increased rates of DNA fragmentation are correlated with poorer overall sperm quality. Five studies evaluated DNA fragmentation rates using the flow cytometry technique [4, 5, 8, 9, 23] while the remaining three studies evaluated DNA fragmentation rates using sperm chromatin dispersion testing [15, 30, 31]. Of the publications included in this review, four studies did not show any significant changes in rates of DNA fragmentation with varying abstinence times prior to sample collection [2, 5, 9, 23]. Of note, all four of these studies utilized the flow cytometry technique to measure DNA fragmentation rates. However, the remaining four studies addressing this issue found an impact of abstinence time on DNA fragmentation rates [4, 15, 30, 31]. The four studies demonstrating an impact found that DNA fragmentation rates were lower with shorter abstinence periods, indicating that sperm DNA quality may be worsened by longer abstinence. Abstinence times of 24 h or less were associated with the lowest rates of DNA fragmentation in the studies which showed a correlation between these two factors. Of the four studies demonstrating an association between abstinence time and DNA fragmentation rate, the study by Agarwal et al. utilized the flow cytometry technique, and the remaining three studies utilized sperm chromatin dispersion testing [4, 15, 30, 31]. In addition to abstinence time, differences in technique and the ability to measure DNA fragmentation rates may impact correlations between abstinence and this parameter.
Five studies included in this review evaluated the impact of abstinence on sperm viability [4, 5, 8, 16, 21] (see Table 1). Four of the five studies (80%) found that there was no significant difference in rates of viable sperm with varying abstinence [4, 5, 8, 21]. Only one study demonstrated that abstinence time did affect viability [16]. The study by Sunanda et al. which demonstrated a difference in viability based on abstinence time specifically evaluated total number of viable sperm. This study concluded that with longer abstinence time of 6 or 7 days, the total number of viable sperm increased. It should be noted that this differed in methodology from the majority of studies which did not show an impact of abstinence time on viability since the four studies showing no difference reported viability as a percentage of viable sperm rather than the total number of viable sperm. An increase in total number of viable sperm would be expected with increasing abstinence time since semen volume and total sperm count would increase as well.
Three studies looked at pregnancy outcomes from semen samples collected following various abstinence times [15, 17, 24]. While pregnancy outcomes are clearly impacted by numerous factors, shorter abstinence times appeared to be associated with improvements in pregnancy rates following assisted reproductive technology. A 2005 study by Jurema et al. evaluated 417 male partners of couples undergoing intrauterine insemination (IUI). This study noted that the highest IUI pregnancy rates were observed using sperm samples which had been collected after an abstinence period of 3 days or less [24]. A 2013 publication by Sanchez-Martin et al. evaluated 40 male partners of couples undergoing intracytoplasmic sperm injection (ICSI) and found that daily ejaculation resulted in significant increases in pregnancy rates following ICSI [15]. A 2008 study by Sugiyam et al. evaluated 22 men with a history of oligoasthenozoospermia who were undergoing in vitro fertilization (IVF) and found that samples collected after a very brief period of abstinence (30 to 60 min) resulted in higher IVF fertilization rates [17]. These studies differed from the majority of studies included in this review which only evaluated semen parameters and did not assess pregnancy outcomes.
Discussion
Data regarding abstinence and semen parameters in the literature is extremely heterogenous, and many publications from several decades ago may no longer be relevant due to newer technology and changes in semen analysis technique. This review attempts to clarify the body of recent information by summarizing trends within the literature since the year 2000 based on individual semen analysis parameters. This systematic review suggests that longer abstinence appears to be associated with improvements in semen volume and sperm count. With few exceptions, the majority of publications support the notion that increased duration of ejaculatory abstinence leads to increased semen volume [4, 6–19]. Similarly, all of the publications evaluating abstinence and sperm count demonstrated increased count with longer abstinence [4, 9–12, 14, 16, 18, 22–24]. Viewed independently, these findings indicate that longer abstinence time improves semen quality.
However, the effect of abstinence on motility, morphology, DNA fragmentation rate, and viability is contradictory and inconclusive [3–10, 12–28, 30, 31]. There does not appear to be any change in semen pH with varying abstinence [4, 8, 19]. With such discrepant data related to the association between abstinence and many semen parameters, it appears that further studies are necessary to elucidate whether an impact truly exists between abstinence and these measures. Many retrospective cohort studies have published data which suggest various abstinence times to maximize certain semen parameters, but when the recent literature is viewed in its entirety, it becomes difficult to draw conclusions. If abstinence does alter parameters such as motility, morphology, and DNA fragmentation rates, the trend toward shorter abstinence to improve these parameters would be in opposition to improvements seen in semen volume and sperm count with longer abstinence time.
IUI, ICSI, and IVF pregnancy rates appear to be highest in the setting of short abstinence, although this is an area which is significantly lacking in the literature. Overall, abstinence of less than 3 days was associated with significantly higher pregnancy rates and fertilization rates in IUI, ICSI, and IVF [15, 17, 24]. The question of whether shorter abstinence is associated with improvements in fertility outcomes is worthy of further investigation since achieving pregnancy is the ultimate goal of maximizing semen parameters. No clear recommendations can be made regarding ideal abstinence time due to the conflicting or inconclusive nature of this topic, but based on current information, the WHO 2- to 7-day abstinence recommendations appear to be arbitrary [1]. Furthermore, while longer abstinence may improve volume and count, problems with these parameters can generally be overcome with assisted reproductive techniques. While semen analysis is the cornerstone for male fertility testing, it remains imperfect in its ability to predict the fertilizing potential of spermatozoa. Which semen parameter is most predictive of subsequent fertility is a question which remains unanswered. This issue is complicated by the fact that many of the functional changes that sperm undergo during the process of fertilization cannot be assessed by semen analysis [32]. Going forward, more information is needed regarding the impact of abstinence on pregnancy and fertilization rates since this would be a clinically useful area of study.
Limitations
As with any literature review, the methodologic quality of the included studies was variable. Many of the studies included relatively small sample sizes. The significance of data from smaller studies should not be ignored, although the larger studies included in this review had the statistical power to provide more convincing evidence. While many publications evaluated healthy men or sperm donors, other studies specifically included men with known semen abnormalities, which may limit the application of findings when dealing with specific patient populations. Another limitation was that the majority of publications included in this systematic review evaluated multiple semen parameters, but not all studies evaluated the same parameters, making it difficult to draw strong conclusions about specific parameters. Additionally, variations in laboratory measurements of specific parameters such as motility and morphology may limit the external validity of the data. Ultimately, the goal of maximizing semen parameters is to achieve pregnancy. Unfortunately, only three of the studies included pregnancy outcomes as part of their results.
Contributor Information
Brent M. Hanson, Phone: 608-780-2370, Email: Brent.hanson@hsc.utah.edu
Kenneth I. Aston, Email: Ki.aston@hsc.utah.edu
Tim G. Jenkins, Email: Tim.jenkins@hsc.utah.edu
Douglas T. Carrell, Email: Douglas.carrell@hsc.utah.edu
James M. Hotaling, Email: Jim.hotaling@hsc.utah.edu
References
- 1.World Health Organization, Department of Reproductive Health and Research. WHO laboratory manual for the examination and processing of human semen. 5th ed. Switzerland: WHO Press; 2010. p. 10–11.
- 2.De Jonge C. Influence of the abstinence period on human sperm quality. Fertil Steril. 2004;82(1):57–65. doi: 10.1016/j.fertnstert.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 3.Levitas E. Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples. Fertil Steril. 2005;83(6):1680–1686. doi: 10.1016/j.fertnstert.2004.12.045. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal A. Abstinence time and its impact on basic and advanced semen parameters. Urology. 2016;94:102–110. doi: 10.1016/j.urology.2016.03.059. [DOI] [PubMed] [Google Scholar]
- 5.Mayorga-Torres B. Influence of ejaculation frequency on seminal parameters. Reprod Biol Endocrinol. 2015;13:47. doi: 10.1186/s12958-015-0045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gonzalo A. Influence of ejaculatory abstinence on the characteristics of spermiogram. Systematic review. Rev Chil Obstet Ginecol. 2013;78(4):290–292. doi: 10.4067/S0717-75262013000400007. [DOI] [Google Scholar]
- 7.Sobreiro B. Semen analysis in fertile patients undergoing vasectomy: reference values and variations according to age, length of sexual abstinence, seasonality, smoking habits and caffeine intake. Sao Paulo Med J. 2005;123(4):161–166. doi: 10.1590/S1516-31802005000400002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeJonge C. Influence of the abstinence period on human sperm quality. Fertil Steril. 2004;82(1):57–65. doi: 10.1016/j.fertnstert.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 9.Welliver C. Analysis of semen parameters during 2 weeks of daily ejaculation: a first in humans study. Transl Androl Urol. 2016;5(5):749–755. doi: 10.21037/tau.2016.08.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Makkar G. A comparative study of raw and prepared semen samples from two consecutive days. J Reprod Med. 2001;46(6):565–572. [PubMed] [Google Scholar]
- 11.Marshburn P. Influence of ejaculatory abstinence on seminal total antioxidant capacity and sperm membrane lipid peroxidation. Medecine Therapeutique Medecine de la Reproduction, Gynecologie et Endocrinologie. 2014;16(4):289–290. doi: 10.1016/j.fertnstert.2014.05.039. [DOI] [PubMed] [Google Scholar]
- 12.Wang L. Influence of the abstinence period on human semen parameters. Chin J Androl. 2007;21(8):21–23. [Google Scholar]
- 13.Lehavi O. Twenty-four hours abstinence and the quality of sperm parameters. Andrologia. 2014;46(6):692–697. doi: 10.1111/and.12137. [DOI] [PubMed] [Google Scholar]
- 14.Marshburn P. A short period of ejaculatory abstinence before intrauterine insemination is associated with higher pregnancy rates. Fertil Steril. 2010;93(1):286–288. doi: 10.1016/j.fertnstert.2009.07.972. [DOI] [PubMed] [Google Scholar]
- 15.Sanchez-Martin P. Increased pregnancy after reduced male abstinence. Syst Biol Reprod Med. 2013;59(5):256–260. doi: 10.3109/19396368.2013.790919. [DOI] [PubMed] [Google Scholar]
- 16.Sunanda P. Effect of age and abstinence on semen quality: a retrospective study in a teaching hospital. Asian Pac J Reprod. 2014;3(2):134–141. doi: 10.1016/S2305-0500(14)60017-8. [DOI] [Google Scholar]
- 17.Sugiyam R. Improvement of sperm motility by short-interval sequential ejaculation in oligoasthenozoospermic patients. Arch Med Sci. 2008;4(4):438–442. [Google Scholar]
- 18.Li W. Influence of abstinence time on young man semen quality. Fudan Univ J Med Sci. 2003;30(4):391–393. [Google Scholar]
- 19.Zhang X. The best abstinence period for donoring semen. Chin J Androl. 2009;23(1):39–41. [Google Scholar]
- 20.Pasqualotto F. Influence of abstinence period on seminal characteristics in infertile men. Rev Bras Ginecol Obstet. 2006;28(1):44–49. doi: 10.1590/S0100-72032006000100008. [DOI] [Google Scholar]
- 21.Rivaroli M. Comparison between length of sexual abstinence and semen parameters in patients of an assisted reproduction center and a hospital from Porto Alegre—RS. J Bras Reprod Assist. 2009;13(2):28–32. [Google Scholar]
- 22.Raziel A. Influence of a short or long abstinence period on semen parameters in the ejaculate of patients with nonobstructive azoospermia. Fertil Steril. 2001;76(3):485–490. doi: 10.1016/S0015-0282(01)01956-2. [DOI] [PubMed] [Google Scholar]
- 23.Mayorga-Torres J. Can a short term of repeated ejaculations affect seminal parameters? J Reprod Infertility. 2016;17(3):177–183. [PMC free article] [PubMed] [Google Scholar]
- 24.Jurema M. Effect of ejaculatory abstinence period on the pregnancy rate after intrauterine insemination. Fertil Steril. 2005;84(3):678–681. doi: 10.1016/j.fertnstert.2005.03.044. [DOI] [PubMed] [Google Scholar]
- 25.Carlsen E. Effects of ejaculatory frequency and season on variations in semen quality. Fertil Steril. 2004;82(2):358–366. doi: 10.1016/j.fertnstert.2004.01.039. [DOI] [PubMed] [Google Scholar]
- 26.AlAwlaqi A, Hammadeh ME. Sexual abstinence and sperm quality. International Journal of Women’s Health and Reproductive Sciences. 2017;5(1):11–17.
- 27.Bahadur G. Semen characteristics in consecutive ejaculates with short abstinence in subfertile males. Reprod BioMed Online. 2016;32(3):323–328. doi: 10.1016/j.rbmo.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 28.Elzanaty S. Duration of sexual abstinence: epididymal and accessory sex gland secretions and their relationship to sperm motility. Hum Reprod. 2005;20(1):221–225. doi: 10.1093/humrep/deh586. [DOI] [PubMed] [Google Scholar]
- 29.Zhou J. The semen pH affects sperm motility and capacitation. PLoS One. 2015;10(7):1–15. doi: 10.1371/journal.pone.0132974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pons I. One abstinence day decreases sperm DNA fragmentation in 90% of selected patients. J Assist Reprod Genet. 2013;30(9):1211–1218. doi: 10.1007/s10815-013-0089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gosalvez J. Shorter abstinence decreases sperm deoxyribonucleic acid fragmentation in ejaculate. Fertil Steril. 2011;96(5):1083–1086. doi: 10.1016/j.fertnstert.2011.08.027. [DOI] [PubMed] [Google Scholar]
- 32.Wang C. Limitations of semen analysis as a test of male fertility and anticipated needs from newer tests. Fertil Steril. 2014;102(6):1502–1507. doi: 10.1016/j.fertnstert.2014.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]