Abstract
Background
Mastery of laparoscopic skills is essential in surgical practice and requires considerable time and effort to achieve. The Virtual Basic Laparoscopic Skill Trainer (VBLaST-PC©) is a virtual simulator that was developed as a computerized version of the pattern cutting task in the Fundamentals of Laparoscopic Surgery (FLS) system. To establish convergent validity for the VBLaST-PC©, we assessed trainees’ learning curves using the cumulative summation (CUSUM) method and compared them with those on the FLS.
Methods
Twenty-four medical students were randomly assigned to an FLS-training group, a VBLaST-training group, or a control group. Fifteen training sessions, 30 minutes in duration per session per day, were conducted over three weeks. All subjects completed pre-test, post-test, and retention-test (2 weeks after post-test) on both the FLS and VBLaST© simulators. Performance data, including time, error, FLS score, learning rate, learning plateau, and CUSUM score, were analyzed.
Results
The learning curve for all trained subjects demonstrated increasing performance and a performance plateau. CUSUM analyses showed that five of the seven subjects reached the intermediate proficiency level but none reached the expert proficiency level after 150 practice trials. Performance was significantly improved after simulation training, but only in the assigned simulator. No significant decay of skills after 2 weeks of disuse was observed. Control subjects did not show any learning on the FLS simulator, but improved continually in the VBLaST simulator.
Conclusions
Although VBLaST©- and FLS-trained subjects demonstrated similar learning rates and plateaus, the majority of subjects required more than 150 trials to achieve proficiency. Trained subjects demonstrated improved performance in only the assigned simulator, indicating specificity of training. The virtual simulator may provide better opportunities for learning, especially with limited training exposure.
Keywords: Learning curve, Cumulative summation, CUSUM, virtual reality, surgical training, convergent validity
Introduction
The laparoscopic approach has become the standard of care for a wide variety of surgical procedures and has the advantages of faster recovery, minimal blood loss, and lower cost of treatment(1). Despite the many benefits of minimally invasive surgery (MIS), the technique is more demanding for surgeons and requires extensive training. This is due to the increased sensorimotor challenges associated with this technique such as hand-eye coordination, two-dimensional field of view, and lack of perceivable haptic feedback(2). As a result, laparoscopic surgery trainees must undergo a substantial amount of preparation using simulators prior to performing live operations.
The current standard for basic laparoscopic skill development is the Fundamentals of Laparoscopic Surgery (FLS) curriculum (3,4), which is administered by the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) and the American College of Surgeons (ACS). The FLS trainer is a physical box-trainer based on the McGill Inanimate System for Training and Evaluation of Laparoscopic Skills (MISTELS) (5). The five FLS tasks used in the manual skills portion of the curriculum are: peg transfer, pattern cutting, ligating loop, suture with intracorporeal knot, and suture with extracorporeal knot. Achieving proficiency in these tasks provides the foundation of laparoscopic surgical skill performance. Since 2009 in the USA, successful completion of the FLS exam is a requirement before being eligible to take the Qualifying Examination of the American Board of Surgery.
Despite being the standard in laparoscopic training there are major drawbacks to the FLS practical exam, including difficulty in evaluating performance objectively and the time needed to score manually. To overcome these issues, virtual reality (VR) based simulators can be used to replace physical models. VR simulators enable objective and automated assessment of performance, in real-time, and without the need for proctors. Moreover, they permit unlimited training without the expense of consumables. They can also provide haptic feedback, which has already been shown to be an essential component of minimally invasive surgery simulations (6,7). VR-based simulators have been shown to transfer effective technical skills to the operating room environment(8,9). The Virtual Basic Laparoscopic Skill Trainer (VBLaST) was developed as the VR version of the FLS trainer (10) and maps the five FLS skills to a virtual environment. The VBLaST has shown face validity, as well as construct, concurrent, and discriminant validity (10–13).
The cumulative summation (CUSUM) is a criterion-based method that is commonly used for characterizing learning curves. It is a statistical and graphical tool that analyzes trends for sequential events in time and hence can be used for quality control of individual performance and group performance. It can be applied in the learning phases, such as while learning a new procedure, and at the end of the training phase after the acquisition of the skill (14,15). Previous research has examined the learning curve for the VBLaST peg transfer task and found it to be comparable to that of the FLS peg transfer task. The objective of this study was to continue the validation process of the VBLaST simulator and demonstrate the convergent validity of the pattern cutting (PC) task using the CUSUM method. To demonstrate convergent validity, the system must be at least as effective as a commonly accepted training system, such as the FLS. Therefore, it was expected that the learning curves on the VBLaST-PC and FLS are similar, with performance improving with practice. In addition, subjects with training on either simulator would perform better than those with no training in the post- and retention tests.
Materials and Methods
Subjects
Based on prior learning curve studies, and power calculations, five subjects were necessary for each of the 3 conditions in this learning curve study. Thirty medical students were recruited to allow for attrition, which was anticipated due to the long time commitment required.
An IRB-approved recruitment email was sent to all Tufts University Medical students. Inclusion criteria were as follows: little or no prior experience with surgery or surgical simulators, normal or corrected to normal vision, and no motor impairment that prevented the handling of two laparoscopic tools in the surgical simulators. Subjects were compensated for their participation.
Ten subjects were randomly assigned to each of the 3 conditions (control, FLS, and VBLaST). At the end of the study, there were nine subjects in the Control group, eight in the FLS-training group, and seven in the VBLaST-training group, due to attrition.
Equipment
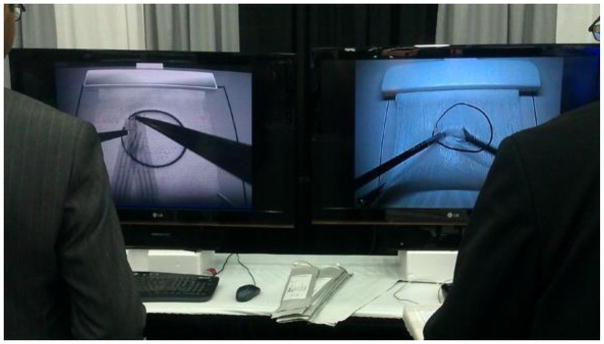
The FLS system (fig. 1a) used was the standard SAGES-approved trainer box. The view of the task space was filmed with fixed focal length camera and displayed on a monitor for the subject. A digital capture device (AVerMedia, Milpitas, CA, USA) was used to record subjects’ performance inside the task space. The video was used to gather timing and error measurements for data analysis.
Fig. 1.
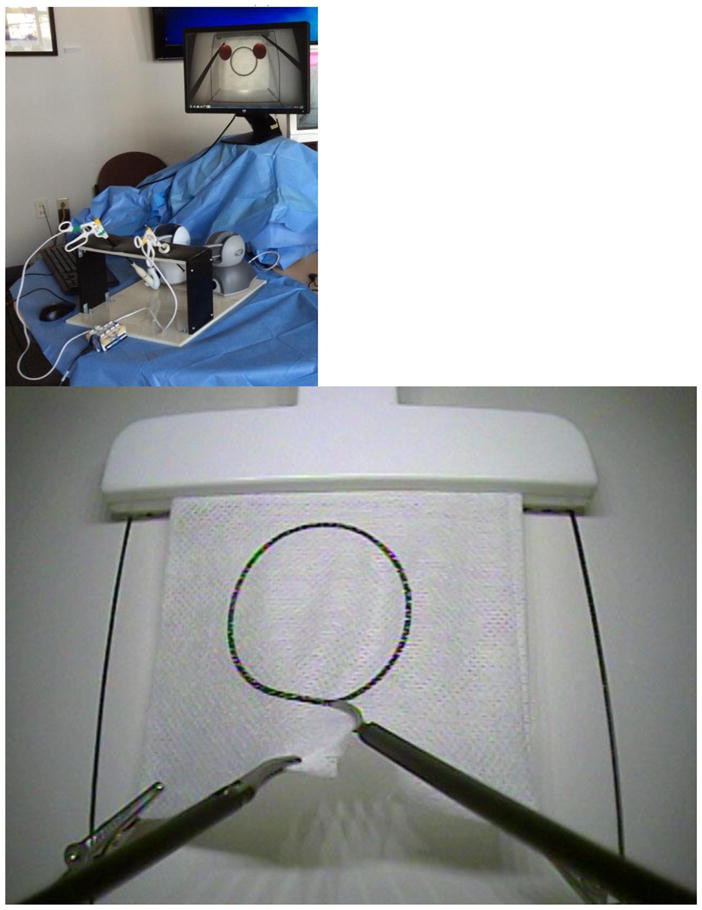
(a) VBLaST-PC (b) FLC-PC (www.flsprogram.org) (c) Comparison of VBLaST-PC on the and FLS-PC on the right
The VBLaST-PC system (fig. 1b) consisted of two laparoscopic tools connected to haptic devices mounted in front of a monitor, and a virtual reality environment simulating the FLS pattern cutting task. Custom developed computational software in the VBLaST-PC simulated the interaction between the tools, and objects in the virtual environment. The two Geomagic Touch haptic devices (3D Systems Inc.) connected to the instrumented tools provided force feedback to the user. Fig. 1c shows side-by-side comparison of the two systems. Even though the system is capable of tracking and calculating performance variables such as instrument path length and smoothness, only time to task completion and errors were used in this study to provide a fair comparison to the FLS.
Experiment Design and Procedure
The pattern cutting (PC) task was used in this convergent validity study. The FLS-PC task requires the subject to cut a circle out of a 4cm × 4cm piece of gauze along a pre-marked black line as quickly and accurately as possible. The task is completed using laparoscopic instruments and the official FLS box trainer as shown below. The same task was completed with the VBLaST© system using laparoscopic instruments and computational software.
In this mixed experimental design, participants were randomly assigned to one of three conditions: control, VBLaST, and FLS. Subjects in the control group did not receive any training on the task, while those in the two training groups received training on the assigned simulator over a period of three weeks. Demographic data including age, medical school year, and information regarding previous experience and laparoscopic surgery were gathered for all subjects. Before the testing session began, all subjects watched an instructional video that demonstrated the proper procedure to perform the pattern cutting task in both the FLS and VBLaST systems. All subjects then performed the task once using both simulators to establish their own baseline performance. This also served as the pre-test assessment. The order of simulators was counterbalanced – half the subjects used the FLS system first for the pre-test and half the subjects used the VBLaST system first.
Subjects randomized in the training groups were asked to attend one training session per day, five days per week, for three consecutive weeks equaling a total of 15, 30-minute sessions. During each 30-min session, subjects were asked to perform 10 trials of the pattern cutting task, or attempt as many trials as possible, whichever was shorter. The experimenter was always present during these training sessions to answer questions and provide instruction when needed. VBLaST-PC time and error data were automatically recorded by the simulator. FLS training scores were computed manually and time was measured using a stopwatch.
At the end of three weeks, all subjects (training and control) performed the pattern cutting task on both the FLS and VBLaST to record post-test data. To assess retention, a final session was held two weeks after the last training session. Table 1 summarizes our experiment design.
Table 1.
Learning Curve Study Timeline
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | |
|---|---|---|---|---|---|
| Control Group | Pretest (Day 1), No Training | No Training | No Training, Posttest (Day 15) | No Training | No Training, Retention Test (Day 16) |
| Trained Groups | Pretest (Day 1), Five Training Sessions | Five Training Sessions (30minutes each) | Five Training Sessions (30minutes each), Posttest (Day 15) | No Training | No Training, Retention Test (Day 16) |
Data Analysis
Performance data Analysis
Using SPSS, the pretest, posttest, and retention test data (time, error, score) were analyzed using a two-way ANOVA mixed design and Tukey HSD post-hoc test, as well as multiple pairwise comparisons with Bonferroni correction. The criterion for statistical significance was set at alpha = 0.05. Outliers were removed from the data and replaced with the group means before analysis. On the FLS simulator, one data point on the time measure and 4 data points on the error measure were considered outliers. On the VBLaST simulator, 3 data points in time and 4 data points in error were considered outliers.
CUSUM Analysis
CUSUM analysis was performed by generating CUSUM charts for all the subjects in both the FLS and the VBLaST training groups. For both the training groups, a criterion on the normalized score was established based on the current accepted proficiency score for the FLS pattern cutting task (score = 72) and an Intermediate proficiency score (score =56) calculated based on average value of the score for all subjects in the first 40 trials. When the computed pattern cutting score for each trial for both groups equaled or exceeded the criterion score, it was defined as a ‘success’ (1), while a lower score was deemed as ‘failure’ (0). The acceptable failure rate (p0) was set at 5%, and the unacceptable failure rate (p1) was set at 10% (2 × p0). Type I and Type II errors (α and β) were set at 0.05 and 0.20, respectively. Based on those parameters, two decision limits (h0 and h1) and the s, the target value for CUSUM, were calculated for each successive trial. For each ‘success’, s was subtracted from the previous CUSUM score. For each ‘failure’, 1 – s was added to the previous CUSUM score. A negative slope of the CUMSUM line indicates success, whereas a positive slope suggests failure. This procedure was repeated for each subject on both training groups. Table 2 shows the CUMSUM variables for data analysis.
Table 2.
CUSUM criteria score and parameters
| Variable | Values |
|---|---|
| FLS PC intermediate proficiency score | 56 |
| FLS PC proficiency score | 72 |
| VBLaST PC intermediate proficiency score | 56 |
| VBLaST PC proficiency score | 72 |
| p0 | 0.05 |
| p1 = 2 × p0 | 0.10 |
| α | 0.05 |
| B | 0.20 |
| P = ln(p1/p0) | 0.69 |
| Q = ln[(1 − p0)/(1 − p1)] | 0.05 |
| s = Q/(P + Q) | 0.07 |
| 1 − s | 0.93 |
| a = ln[(1 − β)/α] | 2.77 |
| b = ln[(1 − α)/β] | 1.56 |
| h0 = −b/(P + Q) | −2.09 |
| h1 = a/(P + Q) | 3.71 |
Learning Plateau and Learning Rate Analysis
We calculated the learning plateau and learning rate using the learning curve data of all subjects in both FLS and VBLaST training conditions based on the method of inverse curve-fitting. The learning plateau was defined as the asymptote of the fitted curve and learning rate was defined as the number of trials required to reach 90% of the plateau (16).
Results
Subjects’ baseline performance (pretest) are summarized as group means in Table 3. Analysis results indicate that the groups were similar at the beginning of the study, even though the differences in their performance scores on the FLS were significant (p=.048). No other measures showed a significant difference between groups.
Table 3.
Subjects’ baseline performance as measured by the pre-test on FLS and VBLaST. (n.s. = not significant)
| Simulator | Training Group | Mean Time (SD) | Mean Error (SD) | Mean Score (SD) | |||
|---|---|---|---|---|---|---|---|
| FLS | Control | 282.33 (76.84) | n.s. | 11.62 (7.06) | n.s. | 11.62 (7.06) | p=.048 |
| FLS | 233.53 (85.30) | 15.34 (6.04) | 22.41 (16.70) | ||||
| VBLaST | 210.79 (61.70) | 10.61 (5.60) | 27.49 (21.66) | ||||
| VBLaST | Control | 312.78 (138.80) | n.s. | 47544.71 (18106.46) | n.s. | 13.43 (10.08) | n.s. |
| FLS | 272.60 (115.70) | 61120.23 (27923.55) | 11.24 (10.40) | ||||
| VBLaST | 314.55 (77.56) | 57732.77 (22062.74) | 6.17 (9.51) |
FLS Simulator
Time to task completion
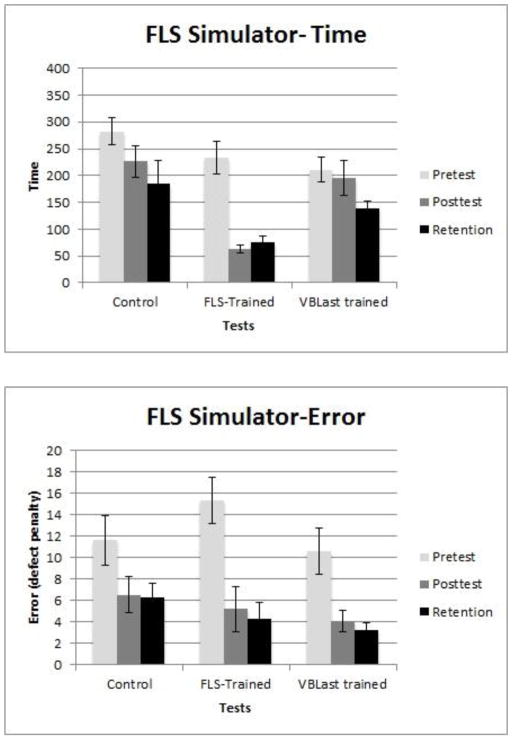
Analysis of variance results (see Table 4) show a significant main effect in training condition (F(2,21)=7.749, p=.003, η2=.425), and learning effect as measured in pretest, posttest and retention test (F(2,42)=21.924, p<.001, η2= .511). No significant interaction between training condition and learning effect was found. Post-hoc Tukey HSD showed that FLS-trained group was significantly different from the control group. There was no difference between the control group and the VBLaST-trained group. Post-hoc pairwise comparisons, with Bonferroni correction, show a significant difference between pretest and posttest, suggesting significant improvement over time, and no significant differences between posttest and retention test (Fig 2a).
Table 4.
ANOVA results for the 3×3 mixed design (3 training conditions × 3 tests)
| Simulator | Performance Measure | Training Condition | η2 | Tests | η2 | Training x Test Interaction | η2 |
|---|---|---|---|---|---|---|---|
| FLS | Time (sec) | F(2,21)=7.749, p=0.003 | .425 | F(2,42)=21.924, p<.001 | .511 | F(4,42)=3.61, p=.013 | .256 |
| Error | F(2,21)=1.074, p=.360 | .093 | F(2,42)=22.957, p<.001 | .522 | F(4,42)=1.078, p=.379 | .093 | |
| Score | F(2,21)=42.87, p<.001 | .803 | F(2,42)=40.03, p<.001 | .656 | F(4,42)=23.67, p<.001 | .693 | |
| VBLaST | Time (sec) | F(2,21)=4.101, p=.031 | .281 | F(2,42)=42.087, p<.001 | .667 | F(4,42)=3.373, p=.018 | .243 |
| Error | F(2,21)=1.407, p=.267 | .118 | F(2,42)=2.773, p=.074 | .117 | F(4,42)=2.371, p=.068 | .184 | |
| Score | F(2,21)=10.362, p=.001 | .497 | F(2,42)=63.61, p<.001 | .752 | F(4,42)=8.414, p<.001 | .445 |
Fig. 2.
Performance group means for the three training groups in pretest, posttest and retention test on the FLS simulator (the error bars represent standard deviation) (a) Completion time (b) Error (c) Normalized Score
Error
There was a significant learning effect in the error measure (F(2,42)=22.957, p<0.001, η2=.522), but no difference as a function of training condition. No interaction between the two factors were observed. Post-hoc pairwise comparisons, with Bonferroni correction, show that errors improved significantly from pretest to post-test, but no significant changes were observed from post-test to retention test, suggesting learning occurred with training, and the learning effect did not decay with time after the training period (Fig. 2b).
Normalized score
The normalized score showed a significant main effect in the training condition (F(2,21)=42.87, p<.001, η2=.803), and a significant learning effect (F(2,42)=40.03, p<.001, η2=.656). There was also a significant interaction between training condition and testing condition (F(4,42)=23.67, p<.001, η2=.693). Post-hoc Tukey HSD showed a significant difference between all training groups. Post-hoc pairwise comparisons, with Bonferroni correction, show that pre-test and post-test were significantly different, suggesting learning, but no difference between post-test and retention test scores, indicating no skill decay with time after the training period (Fig. 2c).
Pretest-posttest
The change in performance from pretest to posttest as an indicator of learning was analyzed. Results from individual t-tests show that the change in performance for the VBLaST-trained group was not different from that of the control group, whereas the change in performance for the FLS-trained group was significantly different from the control group. This suggests that there was no transfer of learning from the VBLaST environment.
VBLaST Simulator
Time to task completion
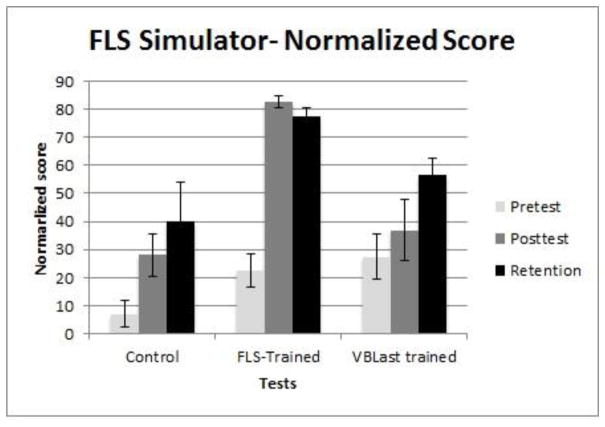
Analysis of variance results (see Table 4) show a significant difference in subjects’ time to task completion as a function of training condition (F(2,21)=4.101, p=.031, η2=.281). There was also a significant learning effect as measured in pretest, posttest and retention test (F(2,42)=42.087, p<.001, η2=.667). A significant interaction between training and learning was noted (F(4,42)=3.373, p=.018, η2=.243). Post-hoc Tukey HSD showed that the only difference was between the control group and the VBLaST-trained group. There was no significant differences between the other groups, suggesting FLS skills did not transfer to the VBLaST simulator. Post-hoc pairwise comparisons, with Bonferroni correction, show a significant difference between pretest and post-test, suggesting improvement with training. There was no significant differences between post-test and retention test, suggesting that there was no decay in skill with time after the training period (Fig. 3a).
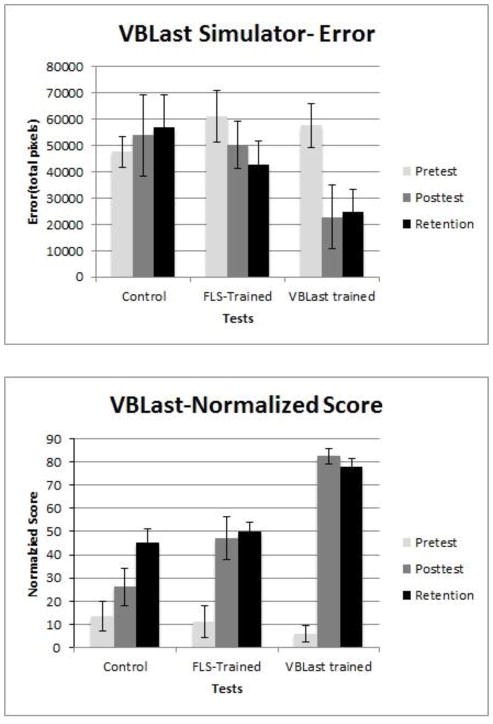
Fig. 3.
Performance group means for the three training groups in pretest, posttest and retention test on the VBLaST-PC simulator (the error bars represent standard deviation) (a) Completion time (b) Error (c) Normalized Score
Error
No significant differences were found in any of the factors for the error measure on the VBLaST simulator (Fig. 3b).
Normalised score
The normalized score showed a significant main effect in the training factor (F(2,21)=10.362, p=.001, η2=.497), and a significant learning effect (F(2,42)=63.61, p<.001, η2=.752). There was a significant interaction between training condition and testing condition (F(4,42)=8.414, p<.001, η2=.445). Post-hoc Tukey HSD showed a significant difference between the subjects in the control and VBLaST-trained groups, and between subjects in the FLS- and VBLaST-trained groups. Control subjects and FLS-trained subjects were not different, suggesting that FLS skills did not transfer to the VBLaST simulator. Again, the pairwise comparisons with Bonferroni correction indicate that significant learning occurred from pre-test to post-test, and no significant decay took place between post-test and retention test (Fig. 3c).
Pretest-posttest
The change in performance from pretest to posttest as an indicator of learning was analyzed. Results from individual t-tests show that the change in performance for the FLS-trained group was not different from that of the control group, whereas the change in performance for the VBLaST-trained group was significantly different from the control group. This suggests that there was no transfer of learning from the FLS environment.
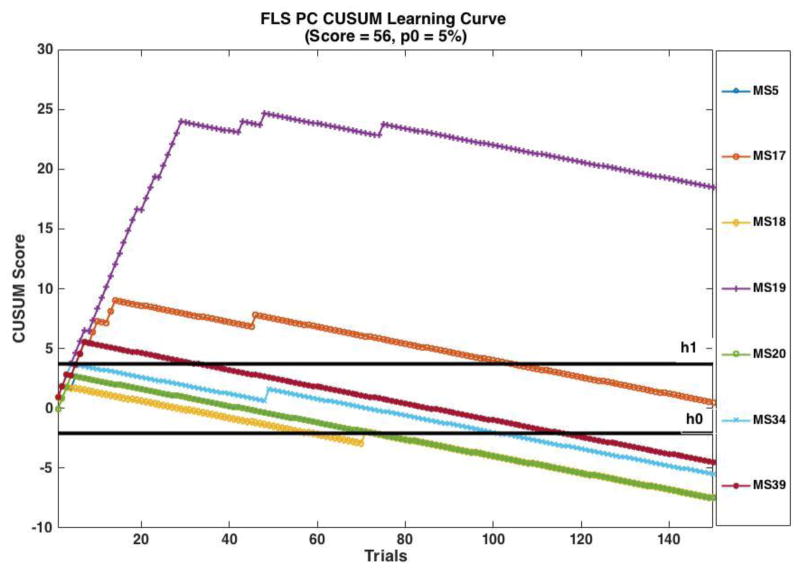
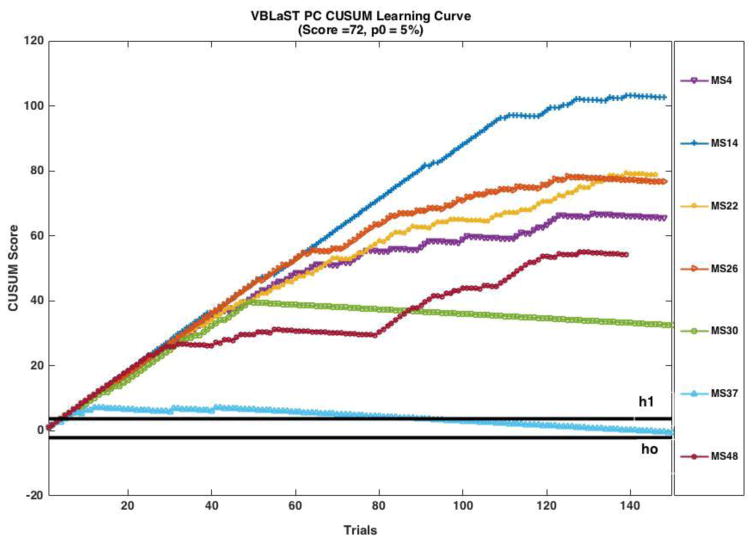
Cumulative Summation Analyses for FLS PC and VBLaST PC Training Groups
Based on the intermediate proficiency criterion (score =56) (Fig. 4), five of the seven medical students (MS) achieved the acceptable failure rate of 5% by 150 trials (MS 20, MS 18 & MS 5 at the 73rd trial, MS 34 at the 101st trial, MS39 115th trial). All subjects showed performance transition points (the trial at which the slope of the CUSUM curve becomes negative) indicating that they reached the targeted score and were improving as trials progressed (MS 18 at the 3rd trial, MS 20 at the 4th trial, MS 5 at the 5th trial, MS 39 at the 7th trial, MS 17 at the 14th trial and MS 19 at the 29th trial). The performance of MS 17 was between the two decision limits of h0 and h1 and did not reach the acceptable failure rate. MS 39 did not achieve proficiency with acceptable failure rate in the 150 trials.
Fig. 4.
CUSUM learning curves for medical students trained on FLS simulator using intermediate criterion success score of 56, acceptable failure rate p0=5%
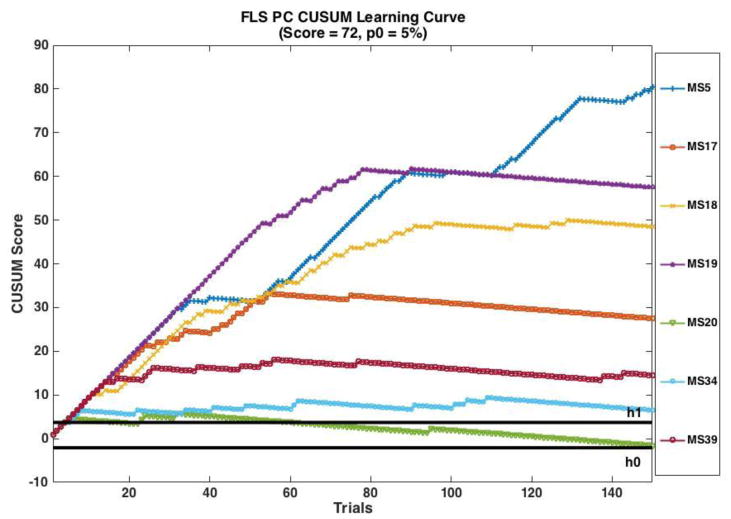
Based on the proficiency score of 72, none of the students achieved the acceptable failure rate of 5% (Fig. 5). For one student (MS 20), the performance crossed the upper decision limit h1 but not the lower decision limit h0 within 150 trials. Six students showed performance transition points (MS 17 at the 75th trial, MS 39 at the 77th trial, MS 19 at the 90th trial, MS 20 at the 95th trial, MS 34 at the 109th trial).
Fig. 5.
CUSUM learning curves for medical students trained on FLS simulator using the FLS proficiency criterion success score of 72, acceptable failure rate p0=5%
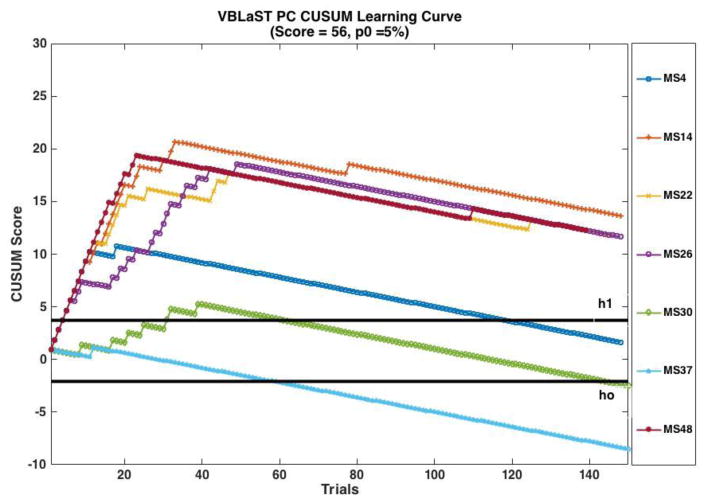
Based on the intermediate proficiency criteria score of 52, two students achieved the 5% acceptable failure rate (see Fig. 6) on the VBLaST simulator (MS 37 achieved at the 58th trial and MS 30 at the 143rd trial). The performance of MS 4 was between the two decision limits. All students showed transition points (MS 37 at the 12th trial, MS4 at the 18th trial, MS 14 at the 32 trial, Ms 26 & MS 22 at the 49th trial and MS 14 at the 79th trial).
Fig. 6.
CUSUM learning curves for medical students trained on VBLaST-PC simulator using intermediate criterion success score of 56, acceptable failure rate p0=5%
Based on the proficiency criteria score of 72, none of the students achieved the acceptable failure rate of 5% (Fig 7.) One student (MS 37) performance was between the two decision limit h0 and h1. Two medical students showed transition points (MS 30 at the 49th trial and MS 37 at the 41st trial).
Fig. 7.
CUSUM learning curves for medical students trained on VBLaST-PC simulator using the FLS proficiency criterion success score of 72, acceptable failure rate p0=5%
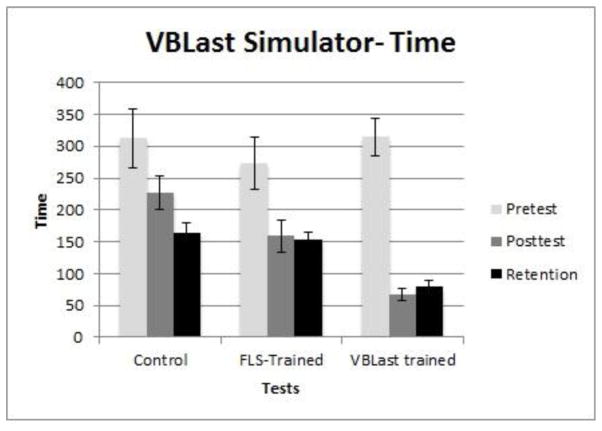
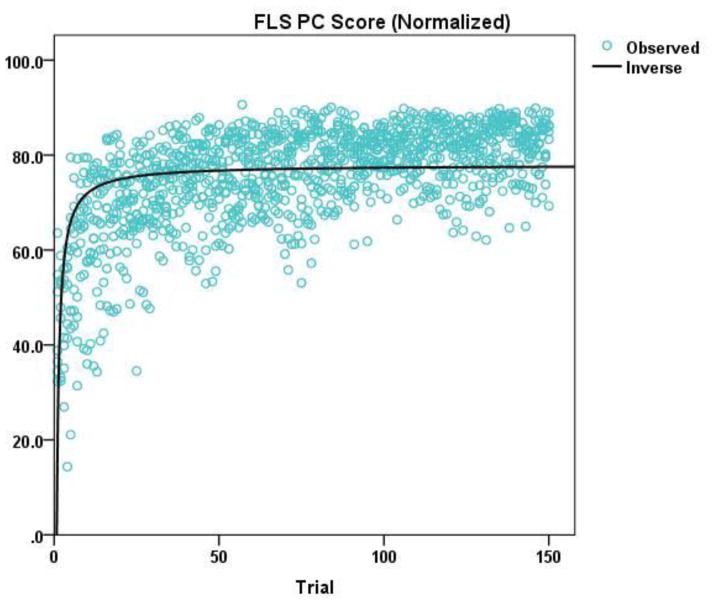
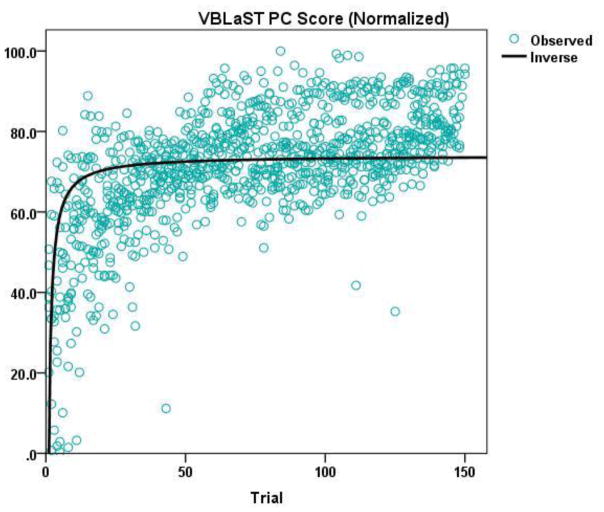
Learning Plateau and Learning Rate for FLS PC and VBLaST PC Training Groups
The inverse curve-fitting results for the FLS PC and the VBLaST PC groups are shown in Figure 8(a) and (b). The learning plateau and the learning rate calculated from the inverse curve-fitting are presented in Table 5. The FLS group achieved a higher plateau (77.93, p < 0.001) compared to the VBLaST group (70.00, p < 0.001) in normalized scores. The FLS group also had a higher learning rate of 7 trials compared to the VBLaST group which required an average of 10 trials to reach 90% of the plateau.
Fig. 8.
Inverse curve-fitting for the derivation of learning plateau and learning rate based on (a) normalized FLS scores, and (b) normalized VBLaST scores
Table 5.
Learning plateau and learning rate for subjects trained on FLS or VBLaST
| Simulator | Measure | Learning Plateau | Learning Rate (trials) |
|---|---|---|---|
| FLS PC | Score | 77.93 | 7 |
| VBLaST PC | Score | 74.00 | 10 |
Discussion
Learning curves capture gains in performance with repetition and have been widely used in assessing learning in surgical tasks (17–28). There are multiple types of learning curves (linear, S-shaped and positively or negatively accelerated) (29). Though learning curves are useful, they are not adequate as it is hard to assess performance over time with knowledge of only the performance plateau and time to reach that level. Cumulative Summation Analysis (CUSUM) is a method where performance over time can be studied with set criteria(15). CUSUM has been widely used in surgery to assess the learning progress for many different procedures (17,18,21,23,25,27,28,30–52).
In our previous study on assessing learning of the VBLaST Peg Transfer task(17), we had analyzed the performance using three criterias (junior, intermediate and senior) based on classification by Fraser et al(27). In this work, we analyzed the learning of the VBLaST pattern cutting task with a study using medical students.
Based on the two criteria (Intermediate and proficient), four students in FLS and two students in VBLaST reached the acceptable failure rate of 5%. For the proficient score, none of the medical students were able to reach the acceptable failure rate at the end of 150 trials for both the simulators. It should be noted that all but one subject showed improvement in performance with a transition point on the CUSUM learning curve. Compared to peg transfer, the pattern cutting task is more challenging and 150 trials were not enough to train subjects at the 5% failure rate.
When comparing the learning plateau reached by both groups on their respective simulators and learning rate, the FLS group achieved slightly higher learning plateau than VBLaST. The subjects in the FLS group also took 3 fewer trials than the VBLaST group to reach 90% of the plateau. Based on our experience working with VR simulators, we attribute this difference to the fact that subjects needed more time to become familiarizes with the VR and haptics technology in the simulator. This hypothesis is difficult to test, and may become self-evident in time as technology in VR and haptics becomes more sophisticated.
In terms of learning, subjects in the control condition did not show any learning on the FLS at the end of the study, with a total exposure of 3 trials on each of the simulators. They showed continual improvement on the VBLaST simulator from pretest to posttest to retention test, as indicated by the increasing test scores (Figure xxx). This may suggest that the virtual simulator is more conducive to learning than the physical simulator during the trainee’s initial exposure to simulation training. This finding may have important implications for surgical education when time availability for training is limited.
Compared to the control group, subjects who received training on the simulators improved their skills significantly after the 3 weeks of practice on their assigned simulator only. Based on the subjects’ testing results (pretest - posttest), learning occurred from Day1 to Day15 of training. That is, VBLaST-trained subjects significantly improved in performance at posttest in the VBLaST simulator but not in the FLS simulator, whereas FLS-trained subjects showed significant improvement in the FLS simulator but not in the VBLaST simulator. This is to be expected due to specificity in learning.
Trained subjects were able to retain their skills even after a period of non-use beyond the training period. In fact, subjects who were trained on the VBLaST continued to improved their performance on the FLS simulator at retention test. This may imply that skills learned on the VBLaST simulator are being transferred to the FLS environment. Similarly, the continual improvement shown by FLS-trained subjects on the VBLaST at pretest and posttest suggests that there is some transfer of learning from the FLS environment.
Overall, our study highlights that laparoscopic surgical skill training in a virtual environment is comparable to training in a physical environment, taking into account additional time need for familiarization with the VR environment. This is a very important finding when it comes to planning simulation center experiences for surgical trainees. Repeated practice on the VBLaST simulator does not require expensive consumables and does not require replacing the materials between trials. The virtual environment is also capable of providing immediate feedback on time, error, and score, whereas the FLS simulator requires a proctor to keep time and calculate error and score, which is time consuming, labor intensive and results in significantly delayed feedback. The virtual environment is also capable of providing adaptive learning and one can imagine that a simulator can be programmed at different levels of difficulty with progression of training.
Future directions for this research include studies to investigate the transfer of learning from one simulator environment to the other, and by extension, the transfer of these laparoscopic surgery skills from the simulation lab to the operating theatre. This will allow us to validate the predictive power of the simulators as a training tool for surgical skills mastery.
Acknowledgments
Funding Information: This work was supported by a grant from the National Institutes of Health (NIBIB R01 EB010037-01)
The authors would like to thank Drs. Scott Epstein, Jesse Rideout, George Perides, and Christopher Awtrey, for assistance with the experimental setup, Jannine Dewar, Winnie Chen, Yiman Lou, Emily Diller, Nicole Santos and Jamaya Carter for their assistance in collecting and analysing the performance data.
Footnotes
Note: This work was presented as a poster at the SAGES 2016 Annual Meeting
Disclosures
Drs. Linsk, Monden, Sankaranarayanan, Ahn, De, and Cao have no conflicts of interest or financial ties to disclose. Dr. Jones is a Consultant for Allurion, and The Medical Company. Dr. Schwaitzberg is a Consultant for Covidien, and Great Venture Partner, and has equity interest in Human Extension, Acuity Bio, Arch Therapeutics, and Gordian Medical.
References
- 1.Dawson SL, Kaufman JA. The imperative for medical simulation. Proceedings of the IEEE. 1998:479–83. [Google Scholar]
- 2.Cao CGL, MacKenzie C, Payandeh S. Task and motion analyses in endoscopic surgery. ASME Dynamic Systems and Control Division (Fifth Annual Sympoisum on Haptic Interfaces for Virtual Environment and Teleoperator Systems); 1996. pp. 583–90. [Google Scholar]
- 3.Fried GM. FLS assessment of competency using simulated laparoscopic tasks. J Gastrointest Surg. 2008;12(2):210–2. doi: 10.1007/s11605-007-0355-0. [DOI] [PubMed] [Google Scholar]
- 4.Peters JH, Fried GM, Swanstrom LL, Soper NJ, Sillin LF, Schirmer B, et al. Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery [Internet] 2004 Jan;135(1):21–7. doi: 10.1016/s0039-6060(03)00156-9. [cited 2012 Jun 29] Available from: http://www.ncbi.nlm.nih.gov/pubmed/14694297. [DOI] [PubMed] [Google Scholar]
- 5.Fraser SA, Klassen DR, Feldman LS, Ghitulescu GA, Stanbridge D, Fried GM. Evaluating laparoscopic skills, setting the pass/fail score for the MISTELS system. Surg Endosc Other Interv Tech. 2003;17(6):964–7. doi: 10.1007/s00464-002-8828-4. [DOI] [PubMed] [Google Scholar]
- 6.Arikatla VS, Sankaranarayanan G, Ahn W, Chellali A, Cao CGL, De S. Development and validation of VBLaST-PT©: A virtual peg transfer simulator. Studies in Health Technology and Informatics [Internet] 2013:24–30. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23263645. [PubMed]
- 7.Sankaranarayanan G, Adair JD, Halic T, Gromski MA, Lu Z, Ahn W, et al. Validation of a novel laparoscopic adjustable gastric band simulator. Surg Endosc [Internet] 2011 Apr;25(4):1012–8. doi: 10.1007/s00464-010-1306-5. [cited 2012 Aug 30] Available from: http://www.ncbi.nlm.nih.gov/pubmed/20734069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, et al. Virtual Reality Training Improves Operating Room Performance. Ann Surg [Internet] 2002 Oct;236(4):458–64. doi: 10.1097/00000658-200210000-00008. [cited 2012 Nov 5] Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1422600/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seymour NE. VR to OR: a review of the evidence that virtual reality simulation improves operating room performance. World J Surg [Internet] 2008 Feb;32(2):182–8. doi: 10.1007/s00268-007-9307-9. [cited 2016 Jul 20] Available from: http://www.ncbi.nlm.nih.gov/pubmed/18060453. [DOI] [PubMed] [Google Scholar]
- 10.Sankaranarayanan G, Lin H, Arikatla VS, Mulcare M, Zhang L, Derevianko A, et al. Preliminary Face and Construct Validation Study of a Virtual Basic Laparoscopic Skill Trainer. J Laparoendosc Adv Surg Tech [Internet] 2010;20(2):153–7. doi: 10.1089/lap.2009.0030. [cited 2011 Jan 10] Available from: http://www.liebertonline.com/doi/abs/10.1089/lap.2009.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chellali A, Ahn W, Sankaranarayanan G, Flinn JT, Schwaitzberg SD, Jones DB, et al. Preliminary evaluation of the pattern cutting and the ligating loop virtual laparoscopic trainers. Surg Endosc [Internet] 2015 Apr;29(4):815–21. doi: 10.1007/s00464-014-3764-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25159626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arikatla VS, Sankaranarayanan G, Ahn W, Chellali A, De S, Caroline GL, et al. Face and construct validation of a virtual peg transfer simulator. Surg Endosc [Internet] 2013 May;27(5):1721–9. doi: 10.1007/s00464-012-2664-y. [cited 2016 Feb 23] Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3625247&tool=pmcentrez&rendertype=abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chellali A, Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Derevianko A, et al. Validation of the VBLaST peg transfer task: a first step toward an alternate training standard. Surg Endosc [Internet] 2014 Apr; doi: 10.1007/s00464-014-3538-2. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24771197. [DOI] [PMC free article] [PubMed]
- 14.Biau DJ, Resche-Rigon M, Godiris-Petit G, Nizard RS, Porcher R. Quality Control of Surgical and Interventional Procedures: A Review of the CUSUM. Qual Saf Heal Care [Internet] 2007 Jun;16(3):203–7. doi: 10.1136/qshc.2006.020776. [cited 2012 May 15] Available from: http://qualitysafety.bmj.com/content/16/3/203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams SM, Parry BR, Schlup MM. Quality control: an application of the cusum. BMJ Br Med J [Internet] 1992 May;304(6838):1359–61. doi: 10.1136/bmj.304.6838.1359. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1882013/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldman LS, Cao J, Andalib A, Fraser S, Fried GM. A method to characterize the learning curve for performance of a fundamental laparoscopic simulator task: defining “learning plateau” and “learning rate”. Surgery [Internet] 2009 Aug;146(2):381–6. doi: 10.1016/j.surg.2009.02.021. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/19628099. [DOI] [PubMed] [Google Scholar]
- 17.Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Grosdemouge C, Rideout JM, et al. Characterizing the learning curve of the VBLaST-PT(©) (Virtual Basic Laparoscopic Skill Trainer) Surg Endosc [Internet] 2013 Oct;27(10):3603–15. doi: 10.1007/s00464-013-2932-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23572217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fraser SA, Bergman S, Garzon J. Laparoscopic splenectomy: learning curve comparison between benign and malignant disease. Surg Innov [Internet] 2012 Mar;19(1):27–32. doi: 10.1177/1553350611410891. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21719436. [DOI] [PubMed] [Google Scholar]
- 19.Melfi FMA, Mussi A. Robotically assisted lobectomy: learning curve and complications. Thorac Surg Clin [Internet] 2008 Aug;18(3):289–95. vi–vii. doi: 10.1016/j.thorsurg.2008.06.001. [cited 2015 Sep 11] Available from: http://www.sciencedirect.com/science/article/pii/S1547412708000492. [DOI] [PubMed] [Google Scholar]
- 20.Cook JA, Ramsay CR, Fayers P. Using the literature to quantify the learning curve: a case study. Int J Technol Assess Health Care [Internet] 2007;23(2):255–60. doi: 10.1017/S0266462307070341. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/17493312. [DOI] [PubMed] [Google Scholar]
- 21.Li JCM, Lo AWI, Hon SSF, Ng SSM, Lee JFY, Leung KL. Institution learning curve of laparoscopic colectomy--a multi-dimensional analysis. Int J Colorectal Dis [Internet] 2012 Apr;27(4):527–33. doi: 10.1007/s00384-011-1358-6. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/22124675. [DOI] [PubMed] [Google Scholar]
- 22.Chang L, Satava RM, Pellegrini CA, Sinanan MN. Robotic surgery: identifying the learning curve through objective measurement of skill. Surg Endosc [Internet] 2003 Nov;17(11):1744–8. doi: 10.1007/s00464-003-8813-6. [cited 2015 Sep 12] Available from: http://www.ncbi.nlm.nih.gov/pubmed/12958686. [DOI] [PubMed] [Google Scholar]
- 23.Jaffer U, Cameron AEP. Laparoscopic appendectomy: a junior trainee’s learning curve. JSLS J Soc Laparoendosc Surg/Soc Laparoendosc Surg [Internet] 2008 Sep;12(3):288–91. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/18765054. [PMC free article] [PubMed] [Google Scholar]
- 24.Veronesi G. Thorac Surg Clin [Internet] 2. Vol. 24. Elsevier Inc; 2014. Robotic thoracic surgery technical considerations and learning curve for pulmonary resection; pp. 135–41. Available from: http://dx.doi.org/10.1016/j.thorsurg.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 25.Bokhari MB, Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM. Learning curve for robotic-assisted laparoscopic colorectal surgery. Surg Endosc [Internet] 2011 Mar;25(3):855–60. doi: 10.1007/s00464-010-1281-x. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/20734081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Petersen RH, Hansen HJ. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg. 2012;1(1):47–50. doi: 10.3978/j.issn.2225-319X.2012.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fraser SA, Feldman LS, Stanbridge D, Fried GM. Characterizing the learning curve for a basic laparoscopic drill. Surg Endosc [Internet] 2005 Dec;19(12):1572–8. doi: 10.1007/s00464-005-0150-5. [cited 2012 Jun 4] Available from: http://www.ncbi.nlm.nih.gov/pubmed/16235127. [DOI] [PubMed] [Google Scholar]
- 28.Son G-M, Kim J-G, Lee J-C, Suh Y-J, Cho H-M, Lee Y-S, et al. Multidimensional analysis of the learning curve for laparoscopic rectal cancer surgery. J Laparoendosc Adv Surg Tech A [Internet] 2010 Sep;20(7):609–17. doi: 10.1089/lap.2010.0007. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/20701545. [DOI] [PubMed] [Google Scholar]
- 29.Magill RA. Motor Learning and Control: Concepts and Applications [Internet] 8. McGraw-Hill; 2007. p. 482. Available from: http://www.amazon.com/dp/0073047325. [Google Scholar]
- 30.Kinsey SE, Giles FJ, Holton J. Cusum plotting of temperature charts for assessing antimicrobial treatment in neutropenic patients. BMJ. 1989 Sep;299(6702):775–6. doi: 10.1136/bmj.299.6702.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Calsina L, Clará A, Vidal-Barraquer F. The use of the CUSUM chart method for surveillance of learning effects and quality of care in endovascular procedures. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg [Internet] 2011 May;41(5):679–84. doi: 10.1016/j.ejvs.2011.01.003. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21333562. [DOI] [PubMed] [Google Scholar]
- 32.Okrainec A, Ferri LE, Feldman LS, Fried GM. Defining the learning curve in laparoscopic paraesophageal hernia repair: a CUSUM analysis. Surg Endosc [Internet] 2011 Apr;25(4):1083–7. doi: 10.1007/s00464-010-1321-6. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/20835725. [DOI] [PubMed] [Google Scholar]
- 33.Young A, Miller JP, Azarow K. Establishing learning curves for surgical residents using Cumulative Summation (CUSUM) Analysis. Curr Surg [Internet] 2005 Jun;62(3):330–4. doi: 10.1016/j.cursur.2004.09.016. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15890218. [DOI] [PubMed] [Google Scholar]
- 34.Van Rij AM, McDonald JR, Pettigrew RA, Putterill MJ, Reddy CK, Wright JJ. Cusum as an aid to early assessment of the surgical trainee. Br J Surg [Internet] 1995 Nov;82(11):1500–3. doi: 10.1002/bjs.1800821117. [cited 2012 May 15] Available from: http://www.ncbi.nlm.nih.gov/pubmed/8535803. [DOI] [PubMed] [Google Scholar]
- 35.Kinsey SE, Giles FJ, Holton J. Cusum plotting of temperature charts for assessing antimicrobial treatment in neutropenic patients. BMJ. 1989 Sep;299(6702):775–6. doi: 10.1136/bmj.299.6702.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Naik VN, Devito I, Halpern SH. Cusum analysis is a useful tool to assess resident proficiency at insertion of labour epidurals. Can J Anaesth [Internet] 2003 Sep;50(7):694–8. doi: 10.1007/BF03018712. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/12944444. [DOI] [PubMed] [Google Scholar]
- 37.Bartlett A, Parry B. Cusum analysis of trends in operative selection and conversion rates for laparoscopic cholecystectomy. ANZ J Surg [Internet] 2001 Aug;71(8):453–6. doi: 10.1046/j.1440-1622.2001.02163.x. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/11504287. [DOI] [PubMed] [Google Scholar]
- 38.McCarter FD, Luchette FA, Molloy M, Hurst JM, Davis K, Johannigman JA, et al. Institutional and Individual Learning Curves for Focused Abdominal Ultrasound for Trauma. Ann Surg [Internet] 2000 May;231(5):689–700. doi: 10.1097/00000658-200005000-00009. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1421056/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Papanna R, Biau DJ, Mann LK, Johnson A, Moise KJ., Jr Use of the Learning Curve–Cumulative Summation test for quantitative and individualized assessment of competency of a surgical procedure in obstetrics and gynecology: fetoscopic laser ablation as a model. Am J Obstet Gynecol [Internet] 2011 Mar;204(3):218.e1–218.e9. doi: 10.1016/j.ajog.2010.10.910. [cited 2013 Jan 10] Available from: http://www.sciencedirect.com/science/article/pii/S0002937810022258. [DOI] [PubMed] [Google Scholar]
- 40.Zhang L, Sankaranarayanan G, Arikatla VS, Ahn W, Grosdemouge C, Rideout JM, et al. Characterizing the learning curve of the VBLaST-PT(©) (Virtual Basic Laparoscopic Skill Trainer) Surg Endosc [Internet] 2013 Apr; doi: 10.1007/s00464-013-2932-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23572217. [DOI] [PMC free article] [PubMed]
- 41.Lerch L, Donald JC, Olivotto IA, Lesperance M, van der Westhuizen N, Rusnak C, et al. Measuring surgeon performance of sentinel lymph node biopsy in breast cancer treatment by cumulative sum analysis. Am J Surg [Internet] 2007 May;193(5):556–60. doi: 10.1016/j.amjsurg.2007.01.012. [cited 2013 Jan 10] Available from: http://www.sciencedirect.com/science/article/pii/S0002961007000918. [DOI] [PubMed] [Google Scholar]
- 42.Tekkis PP, Senagore AJ, Delaney CP, Fazio VW. Evaluation of the Learning Curve in Laparoscopic Colorectal Surgery. Ann Surg [Internet] 2005 Jul;242(1):83–91. doi: 10.1097/01.sla.0000167857.14690.68. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1357708/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pendlimari R, Holubar SD, Dozois EJ, Larson DW, Pemberton JH, Cima RR. Technical proficiency in hand-assisted laparoscopic colon and rectal surgery: determining how many cases are required to achieve mastery. Arch Surg (Chicago, Ill. 1960) [Internet] 2012 Apr;147(4):317–22. doi: 10.1001/archsurg.2011.879. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/22184135. [DOI] [PubMed] [Google Scholar]
- 44.Forbes TL, DeRose G, Kribs SW, Harris KA. Cumulative sum failure analysis of the learning curve with endovascular abdominal aortic aneurysm repair. J Vasc Surg [Internet] 2004 Jan;39(1):102–8. doi: 10.1016/s0741-5214(03)00922-4. [cited 2012 May 15] Available from: http://www.sciencedirect.com/science/article/pii/S0741521403009224. [DOI] [PubMed] [Google Scholar]
- 45.Novotný T, Dvorák M, Staffa R. The learning curve of robot-assisted laparoscopic aortofemoral bypass grafting for aortoiliac occlusive disease. J Vasc Surg Off Publ Soc Vasc Surg [and] Int Soc Cardiovasc Surgery, North Am Chapter [Internet] 2011 Feb;53(2):414–20. doi: 10.1016/j.jvs.2010.09.007. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21093201. [DOI] [PubMed] [Google Scholar]
- 46.Buchs NC, Pugin F, Bucher P, Hagen ME, Chassot G, Koutny-Fong P, et al. Learning curve for robot-assisted Roux-en-Y gastric bypass. Surg Endosc [Internet] 2012 Apr;26(4):1116–21. doi: 10.1007/s00464-011-2008-3. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/22044973. [DOI] [PubMed] [Google Scholar]
- 47.Kye B-H, Kim J-G, Cho H-M, Kim H-J, Suh Y-J, Chun C-S. Learning curves in laparoscopic right-sided colon cancer surgery: a comparison of first-generation colorectal surgeon to advance laparoscopically trained surgeon. J Laparoendosc Adv Surg Tech A [Internet] 2011 Nov;21(9):789–96. doi: 10.1089/lap.2011.0086. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/21854205. [DOI] [PubMed] [Google Scholar]
- 48.Filho DO, Rodrigues G. The Construction of Learning Curves for Basic Skills in Anesthetic Procedures: An Application for the Cumulative Sum Method. Anesth Analg [Internet] 2002 Aug;95(2):411–6. doi: 10.1097/00000539-200208000-00033. [cited 2012 May 15] Available from: http://www.anesthesia-analgesia.org/content/95/2/411. [DOI] [PubMed] [Google Scholar]
- 49.Murzi M, Cerillo AG, Bevilacqua S, Gilmanov D, Farneti P, Glauber M. Traversing the learning curve in minimally invasive heart valve surgery: a cumulative analysis of an individual surgeon’s experience with a right minithoracotomy approach for aortic valve replacement. Eur J cardio-thoracic Surg Off J Eur Assoc Cardio-thoracic Surg [Internet] 2012 Jun;41(6):1242–6. doi: 10.1093/ejcts/ezr230. [cited 2012 May 28] Available from: http://www.ncbi.nlm.nih.gov/pubmed/22232493. [DOI] [PubMed] [Google Scholar]
- 50.Li X, Wang J, Ferguson MK. J Thorac Cardiovasc Surg [Internet] 4. Vol. 147. Elsevier Inc; 2014. Competence versus mastery: The time course for developing proficiency in video-assisted thoracoscopic lobectomy; pp. 1150–4. Available from: http://dx.doi.org/10.1016/j.jtcvs.2013.11.036. [DOI] [PubMed] [Google Scholar]
- 51.Schlup MMT, Williams SM, Barbezat GO. ERCP: a review of technical competency and workload in a small unit. Gastrointest Endosc [Internet] 1997 Jul;46(1):48–52. doi: 10.1016/s0016-5107(97)70209-8. [cited 2012 May 28] Available from: http://www.sciencedirect.com/science/article/pii/S0016510797702098. [DOI] [PubMed] [Google Scholar]
- 52.Bould MD, Crabtree NA, Naik VN. Assessment of Procedural Skills in Anaesthesia. Br J Anaesth [Internet] 2009 Oct;103(4):472–83. doi: 10.1093/bja/aep241. [cited 2012 May 15] Available from: http://bja.oxfordjournals.org/content/103/4/472. [DOI] [PubMed] [Google Scholar]