Abstract
Objective
To test the reliability and validity of the Nutrition Literacy Assessment Instrument (NLit) in adult primary care and to identify the relationship between nutrition literacy and diet quality.
Design
This instrument validation study included a cross-sectional sample participating in up to two visits one month apart.
Participants/setting
429 adults with nutrition-related chronic disease were recruited from clinics and patient registry affiliated with a Midwestern university medical center.
Main outcome measures
Nutrition literacy was measured by the NLit, comprised of six subscales: Nutrition & Health, Energy Sources in Food, Food Label & Numeracy, Household Food Measurement, Food Groups, and Consumer Skills. Diet quality was measured by Healthy Eating Index (HEI)- 2010 using nutrient data from Diet History Questionnaire II surveys.
Analysis
Factor validity and reliability were measured by binary confirmatory factor analysis, test-retest reliability was measured by Pearson’s r and the intraclass correlation coefficient, and relationships between nutrition literacy and diet quality were analyzed by linear regression.
Results
The NLit demonstrated substantial factor validity and reliability (0.97, CI =0.96–0.98) and test-retest reliability (0.88, CI=0.85–0.90). Nutrition literacy was the most significant predictor of diet quality (β=0.17, R2 =0.10, p<0.0001).
Conclusions
The NLit is a valid and reliable tool for measuring nutrition literacy in adult primary care patients.
Keywords: nutrition literacy, health literacy, patient education, chronic disease, primary health care, adults, nutrition surveys, nutrition assessment
INTRODUCTION
Six of the top ten leading causes of death in the US are chronic diseases preventable by consuming a healthy diet1,2, yet unhealthy nutrient consumption and dietary patterns persist for a majority of Americans3,4. Although healthy eating behaviors are multifactorial, it is possible that an important overlooked contributor is nutrition literacy; that is, health literacy applied to the nutrition context.
Nearly half of US adults have difficulty understanding and utilizing commonly provided types of health information5, making health literacy an important mediator of health outcomes6. These deficits in health literacy are associated with poorer use of preventive care services7 ; difficulty with self-management of disease8,9, and poorer health status10. Because nutrition is a major fundamental factor in the development and treatment of diabetes11, hypertension12 ; hyperlipidemia13, and obesity14, low nutrition literacy may be particularly problematic.
Nutrition literacy is “the degree to which individuals have the capacity to obtain, process, and understand nutrition information and skills needed in order to make appropriate nutrition decisions”15. While the research literature in nutrition literacy is growing, it is nonetheless small, requiring inclusion of general health literacy literature within discussions of nutrition literacy. Increasing evidence demonstrates that most people encounter difficulty using information found on food labels16–18 and those with low health literacy and/or numeracy struggle more19–21 and suffer worse health outcomes. Zoellner et al demonstrated in a low-income rural population that as health literacy scores decrease, diet quality also decreases22.
In order to identify the presence and potential consequences of low nutrition literacy, researchers and clinicians must first be able to measure nutrition literacy. Many tools exist for measuring health literacy and these have evolved from simply measuring print literacy within the context of health care terminology23, to print literacy and numeracy24–26, to a broader range of health literacy related skills, utilizing a variety of approaches to measurement27. Most often, researchers measuring health literacy in the context of nutrition have used the Newest Vital Sign26, which references a Nutrition Facts Panel of ice cream. The Diabetes Numeracy Test28 is also relevant to nutrition for the diabetes population because it includes carbohydrate counting. The Nutrition Literacy Scale29 is described in the literature, and by description appears to measure print literacy within the context of nutrition although further use has not been described in the literature. More recently, the Critical Nutrition Literacy Scale30 was developed to measure perceived ability to critically analyze nutrition information and engage in actions to reduce barriers to healthy eating. While any of these tools could be used for specific purposes, none provide a broad assessment of nutrition literacy skills important for implementing nutrition recommendations for nutrition-related chronic illnesses commonly seen in primary care.
The Nutrition Literacy Assessment Instrument (NLit) was designed to assess print literacy and numeracy within nutrition contexts and the capability to apply nutrition knowledge and skills. A multistep process of engaging nutrition professionals and patients was employed to develop the constructs and items of the NLit. First, experts in nutrition education were interviewed to identify constructs of nutrition literacy and registered dietitians were surveyed to provide feedback on approaches for measuring nutrition literacy within these constructs31,32. Variations of the instrument were developed and pil ot tested separately in 2 populations including breast cancer patients (NLit-BCa)33 and parents (NLit-P)34 demonstrating moderate to substantial reliability for individual instrument domains, and positive linear relationships with diet quality.
The purposes of this study were to measure the validity and reliability of the NLit among primary care patients with nutrition-related chronic illness and to identify the extent to which nutrition literacy is associated with diet quality. It was hypothesized that the NLit would stratify participants by nutrition literacy and that those with higher nutrition literacy would demonstrate higher diet quality than patients with lower nutrition literacy.
METHODS
Study design
This instrument validation study was conducted at an urban University Medical Center in the Midwest. All participants were recruited and data was collected between January 2015 and July 2016.
Participants and Recruitment
Participants were recruited using a variety of approaches including by telephone outreach to an existing patient registry, by flyer and invitations to patients in waiting rooms of 2 University-affiliated safety net clinics and 2 primary care clinics, and by campus broadcast email. Eligible participants were over 18 years of age, could speak and read in English, and self-reported a current diagnosis of diabetes, hyperlipidemia, hypertension, or overweight/obesity. These conditions were targeted based on high population frequency and because they comprise a large portion of nutrition education encounters in clinical practice. Ineligibility criteria included overt psychiatric illness, visual acuity insufficient to read the testing instrument, cognitive impairment, or weight of 500 pounds or more (due to scale limit of the research facility). Participants were compensated up to $40 in gift cards for completing both study visits.
The University’s Institutional Review Board approved the study, all subjects provided written informed consent, and all procedures were in accordance with the ethical standards described in the Declaration of Helsinki.
Measures
All surveys were completed online or in print, based on participant preference and level of comfort with technology. Participants completed a brief demographic survey, followed by the Nutrition Literacy Assessment Instrument (NLit), and the Diet History Questionnaire II (DHQII)35. Participants returned for a second visit approximately 1 month later to complete the NLit a second time. Participants completed the NLit, either online or in print, in a quiet exam room with research personnel present to ensure outside resources were not consulted while answering the questions.
Nutrition Literacy
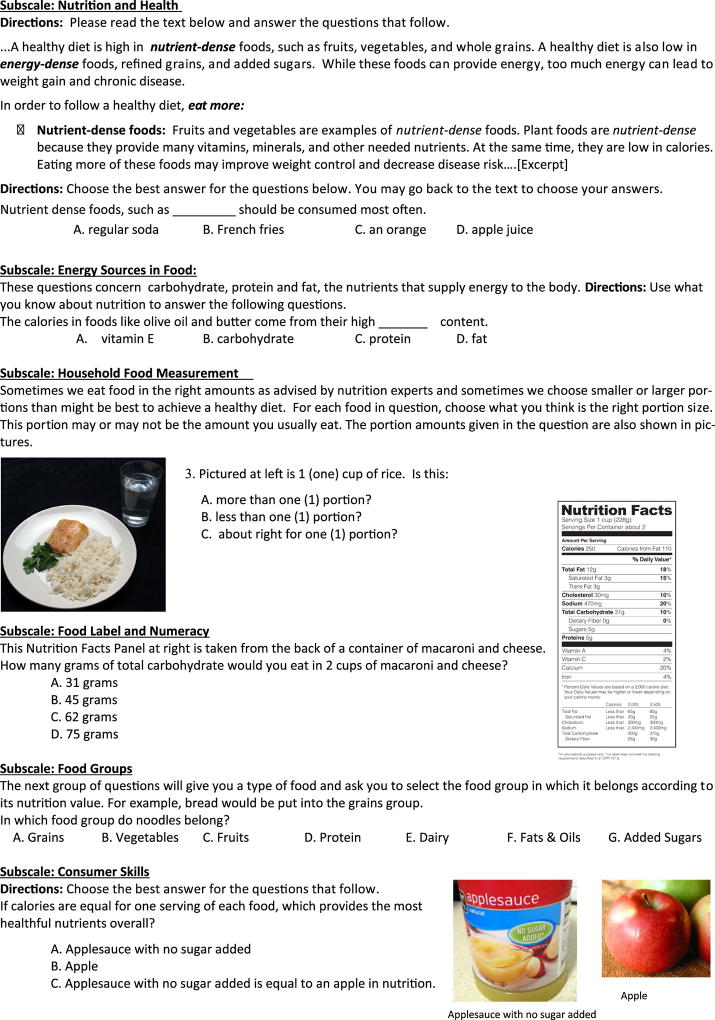
Following the pilot test of the instrument in breast cancer patients33 the NLit was revised by the research team for the nutrition-related chronic disease population and reviewed by 4 experts in nutrition education and 1 psychometrician, in which it demonstrated an acceptable Scale Content Validity Index of 0.90. After suggested revisions, 12 patients with at least 1 of the targeted nutrition-related chronic diseases (hypertension, hyperlipidemia, diabetes, and overweight/obesity) from primary care clinics provided feedback through cognitive interviews, resulting in additional changes to improve the clarity of the format and content for the target patient population36. The resulting NLit contained 66 items and covered six subscales including Nutrition & Health, Energy Sources in Food, Household Food Measurements, Food Label & Numeracy, Food Groups, and Consumer Skills. Example items and excerpts of the NLit are provided in Figure 1.
Figure 1.
Excerpts and One Example Question from Each Subscale of the Nutrition Literacy Assessment Instrument. The University of Kansas holds the copyright of the Nutrition Literacy Assessment Instrument (used with permission).
Diet Quality
Diet quality was measured by the Healthy Eating Index-2010 (HEI-2010)3, which is a metric used to assign a quality score based upon comparison of the reported dietary intake to the recommendations outlined in the Dietary Guidelines for Americans37. The “past year, with portion size” version of the DHQII is a 153-item food frequency questionnaire validated to estimate nutrient intake and is distributed freely by the National Cancer Institute (NCI)35. Using the nutrient data generated by the DHQII, an HEI-2010 score was calculated using methods provided by the NCI38. The total scores of HEI-2010 ranges 0–100, with higher scores indicating higher diet quality.
Body Mass Index
Participants were measured for height and weight using clinic standard procedures39, and these data were used to calculate body mass index (BMI) based on weight (kg)/height (m2).
Data Analysis
The relationship of constructs via subscales of NLit and its respective items was analyzed by Item Response Theory via binary confirmatory factor analysis (CFA) in order to measure factor validity as well as reliability. Binary CFA is a generalization of Rasch models40. The binary CFA analysis was conducted using Classical and Bayesian Instrument Development (CBID) software, which ha s comparable output to the Mplus software41,42. When fitting the model for each subscale, we used a 1-factor model and treated the response of each item as a binary variable (correct or incorrect). The model fit was evaluated by 2 statistical fit indexes: Comparative Fit Index (CFI>.90) and Root Mean Square Error of Approximation (RMSEA<.06)43. In addition to classic CFA, the CBID software calculated a CFA-based measure of reliability called entired reliability and associated 95% interval was estimated with the output obtained by binary CFA44. Entire reliability is better than Cronbach’s alpha since the latter is a lower bound estimate of reliability. The interpretation of reliability was according to Shrout’s adjectives, which is: 0.00–0.10 as virtually none, 0.11–0.40 as slight, 0.41–0.60 as fair, 0.61–0.80 as moderate, and 0.81–1.0 as substantial reliability45.
Test-retest reliability, or stability of survey items, was conducted to determine if questions were answered the same after a 1 month interval by the same people using both Pearson’s correlation and the intraclass correlation coefficient.
Sample Size
Many references on classical instrument development46 recommend 10 subjects per item (therefore requiring 10× participants for the project). A more formal justification of the sample size was examined using a Monte Carlo simulation study for the CFA. We performed the simulation using the Mplus software at various sample sizes (n=50, 100, 200, 300, 400, & 500). At each of these sample sizes we performed 500 simulations and examined the estimate of the standard deviation of estimates and average standard error. First, as the sample size gets larger the errors get smaller. Second, as sample size gets larger the standard errors are very close to standard deviation of estimates. This gave us confidence that at n=400 we would get correct inferences from the CFA. This simulation also showed that increasing the sample size bigger than n=400 had diminishing returns of reduction in standard deviations, consistent with the cited reference above.
Because there is no standard for measuring nutrition literacy and health literacy represents importantly different constructs than nutrition literacy, diet quality (HEI-2010) was considered a convergent construct of nutrition literacy in that both constructs were expected to trend in the same direction. Linear regression tests were used to determine significant (p <0.05) associations between NLit total score, HEI-2010, and other factors selected in step-wise fashion. Independent variables in the models included continuous variables (NLit scores, age, and BMI) and categorical variables (ethnicity, gender, income, education, previous consultation with a dietitian, and self-reported hypertension, hyperlipidemia, and/or diabetes) with HEI-2010 as the dependent variable. Similarly, linear regression tests were used to determine significant associations between each NLit domain score, HEI-2010, and other factors selected in step-wise fashion.
Two items were removed from the long form resulting in a 64 item NLit. One item was removed due to a change in nutrition recommendations (“A healthy diet is low in saturated fat,___, sodium, and foods with added sugar.” [correct answer: cholesterol]) and another item had negative factor loading (“If portions are equal, which food provides the best nutrition?” [correct answer: whole potato; incorrect answer: oven reds frozen potatoes]. All analyses of the 64-item tool were performed with these omissions. With the goal of achieving a shorter set of items, items with the lowest “estimate” (e.g. item to domain correlation) in each domain were removed and subscale reliability was subsequently recalculated. If the subscale’s overall reliability was too low (<0.80), all items that positively contributed to reliability were retained. For example, the 3 lowest reliabilities from items retained was 0.127, 0.330, and 0.436 respectively. While it could be argued that the lowest be removed (0.127), removal would result in fruit (i.e. strawberries) not represented in the subscale. The end result was a short form NLit (42 items) that omits the least reliable items out from the long form (64 items). Pearson’s correlation coefficient was used to compare scoring results between 64-item and 42-item versions.
Scoring thresholds were determined post hoc using regression analysis of NLit 64-item quintile scores as related to HEI-2010 quintile scores, and were chosen based upon HEI-2010 percentiles seen in the original validation study3 as well as Reedy et al’s study of diet quality indices and mortality47.
RESULTS
A total of 445 men and women consented to participate in the study, and 429 had complete NLit surveys for at least 1 visit. Subjects missing ≥ 10 NLit items were excluded from the final analysis (n= 16 visit 1; n=65 visit 2). Of these, 402 had complete DHQ II surveys and 380 completed the NLit at a subsequent visit. Although a majority of the sample were educated females, there was diversity in race (37% African American), ethnicity (11% Hispanic), and income (24% < $25,000 annual household income). The majority of the sample was obese (mean BMI = 34.9 kg/m2), and hypertension was the most common reported chronic disease diagnosis after overweight/obesity. Completing the NLit required 25 minutes on average. Selected characteristics of the sample are provided in Table 1.
Table 1.
Characteristics of the Study Population
| Characteristic | Total n1 | Mean ± SD or n (%) |
|---|---|---|
| Age, years | 424 | 54.0 ± 14.54 |
| Race | 429 | |
| Caucasian | 248 (58%) | |
| African American | 154 (36%) | |
| Other/Undisclosed | 27 (6%) | |
| Ethnicity | 429 | |
| Non-Hispanic | 330 (77%) | |
| Hispanic | 45 (11%) | |
| Other/Undisclosed | 54 (12%) | |
| Gender | 428 | |
| Male | 119 (28%) | |
| Female | 309 (72%) | |
| Annual Household Income | 413 | |
| <$25,000 | 98 (23%) | |
| $25,000 to 49,999 | 126 (29%) | |
| $50,000 to 99,999 | 135 (31%) | |
| $100,000 and above | 54 (12%) | |
| Education | 421 | |
| High school/GED or less | 62 (14%) | |
| Some college/associate’s degree | 163 (38%) | |
| Bachelor’s degree or higher | 196 (45%) | |
| Body Mass Index (BMI), m/kg2 | 424 | 34.9 ± 8.89 |
| Chronic Disease Diagnosis | 429 | |
| Diabetes | 127 (30%) | |
| Hypertension | 242 (56%) | |
| Hyperlipidemia | 192 (45%) | |
| Overweight/Obesity | 361 (84%) | |
| Previous Dietitian Consultation | 411 | |
| Yes | 189 (44%) | |
| No | 222 (52%) | |
| Participation in Public Food Assistance | 429 | |
| No participation | 367 (86%) | |
| Supplemental Nutrition Assistance Program | 37 (9%) | |
| Commodity Supplemental Food Program | 9 (2%) | |
| Women, Infants and Children Program | 7 (2%) | |
| Temporary Assistance for Needy Families | 5 (1%) |
Values <429 had missing data
Results of the confirmatory factor analysis demonstrated substantial factor validity and reliability (0.97, 95% CI = 0.96 – 0.98) for the combined subscale NLit. Analysis of the subscales demonstrates substantial factor validity and reliability for 5 of 6 subscales, while Consumer Skills demonstrated moderate factor reliability with a confidence interval that spans moderate to substantial (0.75, 95% CI = 0.68–0.83). Test-retest reliability was substantial overall (r=0.88, 95% CI = 0.85–0.90) while subscale test-retest reliability varied between fair to substantial reliability. Scores on the 64-item and 42-item NLits were substantially correlated overall (r=0.96, CI = 0.96–0.97) and for each subscale (subscale correlation ranged r=0.86 for Household Food Measurement to r=0.96 for Food Label and Numeracy). Reliability and factor validity statistics are presented in Table 2 for the 64-item NLit and Table 3 for the 42-item NLit.
Table 2.
Validity and reliability statistics by subscale for 64 item Nutrition Literacy Assessment Instrument
| NLita Subscale | Comparative Fit Index (CFI)b |
Root Mean Square of Approximation (RMSEA)c |
Entire Reliabilityd (95% Confidence Interval, CI) |
Test-retest reliability (95% Confidence Intervals, CI)e |
Test- retest reliability (ICC)f |
|---|---|---|---|---|---|
| All subscales combined | 0.975* | 0.021** | 0.97 (CI: 0.96–0.98)*** | 0.88 (CI: 0.86–0.90)### | 0.88### |
| Nutrition & Health | 0.961* | 0.026** | 0.84 (CI: 0.78–0.88)*** | 0.63 (CI: 0.56–0.69)## | 0.63## |
| Energy Sources in Food | 0.998* | 0.012** | 0.92 (CI: 0.88–0.93)*** | 0.80 (CI: 0.76–0.83)## | 0.80## |
| Household Food Measurement | 0.967* | 0.031** | 0.82 (CI: 0.77–0.88)*** | 0.51 (CI: 0.43–0.58)# | 0.51# |
| Food Label and Numeracy | 1.000* | 0.000** | 0.95 (CI: 0.92–0.95)*** | 0.77 (CI: 0.73–0.81)## | 0.77## |
| Food Groups | 0.875 | 0.052** | 0.92 (CI: 0.87–0.94)*** | 0.61 (CI: 0.54–0.67)## | 0.60## |
| Consumer Skills | 0.925 | 0.033** | 0.75 (CI: 0.68–0.82)** | 0.66 (CI: 0.60–0.71)## | 0.66## |
Nutrition Literacy Assessment Instrument
CFI=Comparative Fit Index ≥0.90 indicate acceptable model fit*
RMSEA=Root Mean Square of Approximation ≤ 0.06 indicate acceptable model fit**
Entire reliability is the reliability of the entire domain. 0.61–0.80 is moderate reliability**, 0.81–1.0 is substantial reliability***
Test-retest reliability evaluates the consistency of measurement results between two testing occasions using Pearson’s r and
Intraclass Correlation Coefficients.
We classified reliability as follows: fair reliability#, moderate reliability##, and substantial reliability### according to Shrout’s guidelines (Shrout, PE. Measurement reliability and agreement in psychiatry. Statistical Methods in Medical Research. 1998; 7: 301–317)
Table 3.
Validity and reliability statistics by subscale for 42 item Nutrition Literacy Assessment Instrument
| NLita Subscale | Comparative Fit Index (CFI)b |
Root Mean Square of Approximation (RMSEA)c |
Entire Reliabilityd (95% Confidence Interval, CI) |
Test-retest reliability (95% Confidence Intervals, CI)e |
|---|---|---|---|---|
| All subscales combined | 1.000* | 0.000** | 0.96 (CI: 0.95–0.96)*** | 0.88 (CI: 0.85–0.90)### |
| Nutrition & Health | 0.995* | 0.012** | 0.81 (CI: 0.75–0.86)*** | 0.58 (CI: 0.51–0.64)# |
| Energy Sources in Food | 0.991* | 0.033** | 0.84 (CI: 0.81–0.90)*** | 0.72 (CI: 0.67–0.76)## |
| Household Food Measurement | 1.000* | 0.000** | 0.80 (CI: 0.69–0.86)*** | 0.43 (CI: 0.35–0.51)# |
| Food Label and Numeracy | 1.000* | 0.000** | 0.92 (CI: 0.89–0.94)*** | 0.76 (CI: 0.72–0.80)## |
| Food Groups | 0.924* | 0.048** | 0.94 (CI: 0.81–0.94)*** | 0.58 (CI: 0.51–0.64)# |
| Consumer Skills | 0.925* | 0.033** | 0.75 (CI: 0.68–0.82)** | 0.66 (CI: 0.60–0.71)## |
Nutrition Literacy Assessment Instrument
CFI=Comparative Fit Index ≥0.90 indicate acceptable model fit*
RMSEA=Root Mean Square of Approximation ≤ 0.06 indicate acceptable model fit**
Entire reliability is the reliability of the entire domain. 0.61–0.80 is moderate reliability**, 0.81–1.0 is substantial reliability***
Test-retest reliability evaluates the consistency of measurement results between two testing occasions using Pearson’s r.
We classified reliability as follows: fair reliability#, moderate reliability##, and substantial reliability### according to Shrout’s guidelines (Shrout, PE. Measurement reliability and agreement in psychiatry. Statistical Methods in Medical Research. 1998; 7: 301–317)
Mean HEI-2010 scores were 63.9 (SD = 12.39) and ranged between 29.2 – 89.9. Multiple linear regression indicates a positive and significant relationship between 64-item NLit scores and HEI-2010 (R2 =0.10; p < .0001) as shown in Table 4. Results were similar for multiple linear regression of the relationship between 42-item NLit scores and HEI-2010 (R2 =0.09; p<.0001). Factors considered that were not significant in the model included race, income, and previous consultation with a registered dietitian. Although age, BMI, diabetes, and education attainment all contributed significantly to the model, NLit score was the most significant predictor (β=0.30, p=0.003; β=0.16, p=0.004; 64-item and 42-item respectively).
Table 4.
Summary of Linear Regression Analysis for Variables Predicting Diet Quality (Healthy Eating Index, 2010)
| Model One* | Model Two** | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| Variable | Parameter Estimate |
Standard Error |
Standardize d Parameter Estimate |
p value^ |
Parameter Estimate |
Standard Error |
Standardized Parameter Estimate |
p value^ |
| Intercept | 44.32 | 4.99 | 0 | <.0001 | 42.68 | 7.05 | 0 | <.0001 |
| Nutrition Literacy Assessment Instrumenta | 0.36 | 0.09 | 0.2 | <.0001 | 0.3 | 0.1 | 0.17 | 0.003 |
| Ageb | 0.11 | 0.04 | 0.13 | 0.009 | ||||
| Body Mass Index (BMI)b | −0.14 | 0.07 | −0.1 | 0.054 | ||||
| Diabetes (No Vs Yes)c | −2.94 | 1.36 | −0.11 | 0.032 | ||||
| Education (below college Vs College and above)c | 2.92 | 1.35 | 0.12 | 0.031 | ||||
| R Squared | 0.04 | 0.1 | ||||||
| Adjusted R Squared | 0.04 | 0.08 | ||||||
| F Value | 15.67 | 7.82 | ||||||
| p value^^ | <.0001 | <.0001 | ||||||
Model One is fitted by simple linear regression, and the only predictor is the Nutrition Literacy Assessment Instrument (64 item);
Model Two is fitted by multiple linear regression selected in step-wise fashion. Nutrition Literacy Assessment Instrument (64-item), Age, BMI, Diabetes status and Education level are all included in the model as predictors;
p value for each parameter, which indicates whether the predictor significantly contributes to the variability of the outcome (HEI);
: p value for the whole model, which indicates whether the model is statistically significant;
Nutrition Literacy Assessment Instrument is the average of the summation of the NLit scores from each visit, and it serves as a continuous predictor for HEI in Model One and Model Two;
Age, BMI were collected at Visit 1 and they both serve as continuous predictors for HEI in Model Two;
Diabetes Diagnosis results and Education level were collected at Visit 1 and both serve as discrete predictors for HEI in Model Two.
Domain scores that were significantly related to HEI-2010 included Nutrition & Health (β=0.13, p=0.004), Energy Sources in Food (β=0.19, p<0.001), Food Label & Numeracy (β=0.13, p=0.011), Food Groups (β=0.12, p=0.025), & Consumer Skills (β=0.18, p<0.001). In the step-wise multiple linear regression, when age, BMI, diabetes diagnosis, and education were factored into the model, Energy Sources in Food and Consumer Skills remained significant (p<0.05) after Bonferroni adjustment.
Scoring Thresholds
Three scoring categories emerged when comparing the linear relationship between NLit scores and HEI-2010 scores. NLit scores of 44/64 correct or below were associated with HEI-2010 scores <60.4, which corresponds with the lowest quintile of HEI-2010 scores associated with higher risk of all-cause, cardiovascular, and cancer mortality47. NLit scores of 58 correct or higher were associated with HEI-2010 scores >65.5, which corresponds with the 90th percentile of population HEI-2010 in Guenther’s validation study3. Thus, we suggest that scores ≤44/64 correct may be interpreted as “likelihood of poor nutrition literacy”; scores of 45–57 correct may be interpreted as “possibility of poor nutrition literacy”; and scores ≥58 may be interpreted as “possibility of good nutrition literacy.” Predicted HEI-2010 scores from NLit scores and interpretation for long and short versions of the NLit are presented in Table 5.
Table 5.
Proposed Scoring Thresholds for the Long and Short Versions of the Nutrition Literacy Assessment Instrument Based Upon Associated Healthy Eating Index-2010 Scores.
| Full NLita (64 items) | Shortened NLita (42 Items) | Scoring Interpretation |
||||||
|---|---|---|---|---|---|---|---|---|
| Group | NLita Percentile |
NLita Score |
Range of HEIb Score |
Group | NLita Percentile |
NLita Score |
Range of HEIb Score |
|
| 1 | Min-10%-tile | ≤44 | 51.7 – 60.4 | 1 | Min-10%-tile | ≤28 | 52.5 – 60.8 | Likelihood of poor nutrition literacy |
| 2 | 10%~25%-tile | 45 – 57 | 60.4 – 63.2 | 2 | 10%~25%-tile | 29–38 | 60.8 – 63.1 | Possibility of poor nutrition literacy |
| 3 | 25%-tile~50-tile | 63.2 – 64.1 | 3 | 25%-tile~50-tile | 63.1 – 64.7 | |||
| 4 | 50%-tile~75%-tile | 64.1 – 65.5 | 4 | 50%-tile~75%-tile | 64.7 – 65.6 | |||
| 5 | 75%-tile~90%-tile | ≥58 | 65.5 – 66.2 | 5 | 75%-tile~90%-tile | ≥39 | 65.6 – 66.1 | Likelihood of good nutrition literacy |
| 6 | 90%-tile~Max | 66.2 – 67.5 | 6 | 90%-tile~Max | 66.1 – 67.0 | |||
Nutrition Literacy Assessment Instrument
Associated Healthy Eating Index -2010 with NLita score using linear regression. HEI-2010 scores were calculated from the Diet History Questionnaire II.
DISCUSSION
This is the first study to test the reliability and validity of a tool for comprehensively measuring nutrition literacy in an adult primary care population with nutrition-related chronic disease. The NLit demonstrates substantial factor validity and entire reliability, both overall and by domain, substantial overall test-retest reliability and acceptable test-retest reliability by domains. Additionally, convergent validity of the NLit is demonstrated by the strong relationship found between nutrition literacy scores and diet quality scores (HEI-2010).
Based on formative research completed prior to development of the NLit indicating the time required to assess nutrition literacy was a barrier to measurement in practice31, we identified a shortened version that retains adequate validity and reliability and is substantially correlated with the longer version. Although not measured here, removing one-third of the items could theoretically reduce the average time for assessment by one-third (9 minutes), or require approximately 16 minutes on average for measurement. Availability of both versions allows researchers and clinicians greater flexibility in choosing which version best meets their needs.
This work builds upon the existing tools used to measure health literacy and/or nutrition literacy by applying techniques used to measure print literacy in established health literacy tools24 to the nutrition context while also expanding the constructs of nutrition literacy beyond food label numeracy26. Some tools that seek to measure nutrition knowledge have been validated in college students, which offers the advantage of establishing validity by using nutrition or nursing majors as comparison scorers30,48,49. Development and validation of the NLit within the primary care population, however, is a clear strength in this study to ensure the relevance and difficulty of the tool for the adult primary care population. Because diet quality was evaluated as a comparison construct that demonstrated a positive linear relationship, we might predict that higher nutrition literacy, which is the immediate goal of nutrition education, would subsequently lead to higher diet quality. The approach to use an outcome as the comparison measure for validity is novel in the context of health literacy tools which have established validity through measures of reading comprehension and/or mathematical competency23,24,28, or these tools have served as the comparison measure for additional tools26. While HEI-2010 is not considered a clinical marker, and there are no established thresholds for good or bad diet quality, the substantially lower risk for all-cause, cardiovascular, and cancer mortality in those with the highest quintile of intake in Reedy’s study substantiates the health benefit of recommended dietary patterns47.
Nutrition literacy was the most significant predictor of diet quality in this study, which underscores the importance of incorporating nutrition literacy concepts in efforts to improve the diet quality of adults. While research attention in this area has largely focused on nutrition label literacy18,22,50, our data demonstrate that identifying food sources of the macronutrients (Energy Sources in Food) and the ability to navigate food and nutrition products and marketing to choose between similar options (Consumer Skills) are two skills that have greater importance for choosing a healthy diet than an ability to read a food label. Although diet quality was not reported, a related study of parent nutrition knowledge and label use found that nutrition label literacy and nutrition knowledge was related to parental blood lipids, but only nutrition knowledge was related to child adiposity51.
Increasing age and lower educational attainment are factors consistently related to low health literacy and health outcomes52, consistent with our findings here. It is also unsurprising that our multivariate model predicting diet quality accounted for only 10% of the variance because there are many components that theoretically drive healthy eating that were not measured in this study. This list may include behavioral factors such as attitudes, subjective norms, perceived behavioral control, behavioral intention, motivation, and self-efficacy53–56, food literacy57 and environmental issues such as healthy food access58,59. While models have emerged to include health literacy behavioral models60,61, theoretical models including nutrition literacy in the pathway of a healthy diet are lacking.
There are important limitations to this study. First, diet quality was measured using nutrient data obtained via a food frequency questionnaire, which provides only reported intake, not measured. Bowen demonstrated that those with low health literacy may struggle more to report accurate portion intake via food frequency questionnaires62. Yet, even inaccuracies in reporting could demonstrate poor understanding of nutrition recommendations since people are more likely to report favorably on their dietary intake63. Second, our demographic data and HEI-2010 data suggest a sample bias toward higher than average education and higher than average diet quality, respectively. The mean HEI-2010 scores of this sample fell between the 75th and 90th percentiles of scores in the 2003–2004 NHANES nationally representative sample used to validate HEI-20103, indicating better reported diet quality than would be predicted for a general sample of US adults. While our study included a diverse group in terms of race and chronic disease, future studies of nutrition literacy should focus on assessing participants for a broader range of educational attainment. Finally, as with any measurement instrument, robust construct validity requires evidence from multiple studies, requiring that the NLit be further tested in similar samples and in populations that deviate from this sample.
A challenge to nutrition literacy research is that nutrition literacy is not a static concept, in part because nutrition recommendations change rapidly. For example, the development of the NLit has spanned three versions of the Dietary Guidelines for Americans. These guidelines are required by law to be reviewed by a voluntary appointed panel of leading nutrition experts every five years, leading to new recommendations and often new food guides (e.g. the Food Guide Pyramid in 1992, MyPyramid in 2005, and MyPlate in 2010). While these updates are important for informing health promotion and disease prevention efforts as well as changing public health program policies to better reflect the current science of food and nutrition, it can be difficult for consumers to stay informed64. Although not as rapidly changing, the nutrition facts panel on the food label has undergone recent changes that take effect beginning in July 2018. For those who consult the food label when making purchasing and/or consumption decisions, they will need to reorient themselves to the redesign. What is more, food marketing efforts, such as the use of health claims to appeal to health-conscious consumers, are often misunderstood65–67. Thus, nutrition literacy measurement will need to adapt to the changing recommendations, food guides, and product information.
IMPLICATIONS FOR RESEARCH AND PRACTICE.
The NLit is a reliable and valid tool for measuring nutrition literacy in adults with nutrition-related chronic disease. This tool can serve as a critical resource for the clinical, public health, and research communities for identifying and seeking to improve nutrition literacy skills. Clearly, there is a need for more research in nutrition literacy. Future research efforts should focus upon whether identification of those with low nutrition literacy leads to more targeted nutrition education and whether improved nutrition literacy leads to better diet quality. While our data indicate correlation between nutrition literacy and diet quality, future research is needed to determine effective methods for improving nutrition literacy and whether these improvements result in higher diet quality.
Acknowledgments
The research reported in this publication was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development Award Number R03HD081730 (PI, Heather D. Gibbs), the National Institute of Nursing Research Award Number R03NR013236 (PI, Byron Gajewksi), and by a CTSA grant from NCATS awarded to the University of Kansas Medical Center for Frontiers: The Heartland Institute for Clinical and Translational Research # UL1TR000001. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Special thanks to student assistants who were integral to data collection for this study including Sarah Owens, MS, RD; Riley Williams; Jolyn Mortenson, MS, RD; Shelby Courtright, MS, RD; Juliana Camargo, MPH; Thank you to the clinics who offered us space and opportunities for recruitment including Family Medicine, Internal Medicine, Silver City, and JayDoc Clinics.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Scientific Report of the 2015 Dietary Guidelines Advisory Committee. [Accessed 29 August 2017]; https://health.gov/dietaryguidelines/2015-scientific-report/PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf.
- 2.Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD: 2016. [PubMed] [Google Scholar]
- 3.Guenther PM, Kirkpatrick SI, Reedy J, et al. The healthy eating index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr. 2014;114:399–407. doi: 10.3945/jn.113.183079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reedy J, Krebs-Smith SM. Dietary sources of energy, solid fats, and added sugars among children and adolescents in the United States. J Am Diet Assoc. 2010;110:1477–1484. doi: 10.1016/j.jada.2010.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Neilson-Bowman L. Health Literacy: A prescription to end confusion. Washington, DC: National Academies Press; 2004. [PubMed] [Google Scholar]
- 6.Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121:245. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med. Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease: a study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 9.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 10.Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. J. Gen. Intern. Med. 1998;13:791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Franz MJ, Monk A, Barry B, et al. Effectiveness of medical nutrition therapy provided by dietitians in the management of non–insulin-dependent diabetes mellitus: a randomized, controlled clinical trial. J Am Diet Assoc. 1995;95:1009–1017. doi: 10.1016/S0002-8223(95)00276-6. [DOI] [PubMed] [Google Scholar]
- 12.Sacks FM, Svetkey LP, Vollmer WM, et al. Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. N Engl J Med. 2001;344:3–10. doi: 10.1056/NEJM200101043440101. [DOI] [PubMed] [Google Scholar]
- 13.Delahanty LM, Sonnenberg LM, Hayden D, Nathan DM. Clinical and cost outcomes of medical nutrition therapy for hypercholesterolemia: a controlled trial. J Am Diet Assoc. 2001;101:1012. doi: 10.1016/S0002-8223(01)00250-4. [DOI] [PubMed] [Google Scholar]
- 14.Pruitt JD, Bensimhon D, Kraus WE. Nutrition as a contributor and treatment option for overweight and obesity. Am Heart J. 2006;151:628. doi: 10.1016/j.ahj.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 15.Silk KJ, Sherry J, Winn B, Keesecker N, Horodynski MA, Sayir A. Increasing nutrition literacy: testing the effectiveness of print, web site, and game modalities. J Nutr Educ Behav. 2008;40:3–10. doi: 10.1016/j.jneb.2007.08.012. [DOI] [PubMed] [Google Scholar]
- 16.Cowburn G, Stockley L. Consumer understanding and use of nutrition labelling: a systematic review. Public Health Nutr. 2005;8:21–28. doi: 10.1079/phn2005666. [DOI] [PubMed] [Google Scholar]
- 17.Levy AS, Fein SB. Consumers’ ability to perform tasks using nutrition labels. J Nutr Educ. 1998;30:210–217. [Google Scholar]
- 18.Malloy-Weir L, Cooper M. Health literacy, literacy, numeracy and nutrition label understanding and use: a scoping review of the literature. J Hum Nutr Diet. doi: 10.1111/jhn.12428. [DOI] [PubMed] [Google Scholar]
- 19.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med. 2006;31:391–398. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 20.Sinclair S, Hammond D, Goodman S. Sociodemographic differences in the comprehension of nutritional labels on food products. J Nutr Educ Behav. 2013;45:767–772. doi: 10.1016/j.jneb.2013.04.262. [DOI] [PubMed] [Google Scholar]
- 21.Viswanathan M, Hastak M, Gau R. Understanding and facilitating the usage of nutritional labels by low-literate consumers. Journal of Public Policy & Marketing. 2009;28:135–145. [Google Scholar]
- 22.Zoellner J, You W, Connell C, et al. Health literacy is associated with healthy eating index scores and sugar-sweetened beverage intake: findings from the rural Lower Mississippi Delta. J Am Diet Assoc. 2011 Jul;111:1012–1020. doi: 10.1016/j.jada.2011.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davis TC, Long SW, Jackson RH, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med. 1993;25:391. [PubMed] [Google Scholar]
- 24.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults. J Gen Intern Med. 1995;10:537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 25.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999 doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 26.Weiss BD, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Altin SV, Finke I, Kautz-Freimuth S, Stock S. The evolution of health literacy assessment tools: a systematic review. BMC Public Health. 2014;14:1. doi: 10.1186/1471-2458-14-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huizinga MM, Elasy TA, Wallston KA, et al. Development and validation of the Diabetes Numeracy Test (DNT) BMC Health Serv Res. 2008;8:1–8. doi: 10.1186/1472-6963-8-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diamond JJ. Development of a reliable and construct valid measure of nutritional literacy in adults. Nutrition Journal. 2007;6 doi: 10.1186/1475-2891-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guttersrud Ø, Dalane JØ, Pettersen S. Improving measurement in nutrition literacy research using Rasch modelling: examining construct validity of stage-specific ‘critical nutrition literacy’ scales. Public Health Nutr. 2014;17:877–883. doi: 10.1017/S1368980013000530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gibbs HD, Chapman-Novakofski K. Exploring nutrition literacy: attention to assessment and the skills clients need. Health (N. Y.) 2012;4:120–124. [Google Scholar]
- 32.Gibbs HD, Chapman-Novakofski K. Establishing content validity for the nutrition literacy assessment instrument. Prev Chronic Dis. 2013;10:E109. doi: 10.5888/pcd10.120267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gibbs HD, Ellerbeck EF, Befort C, et al. Measuring nutrition literacy in breast cancer patients: development of a novel instrument. J Cancer Educ. 2016 Sep;31:493–499. doi: 10.1007/s13187-015-0851-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gibbs HD, Kerling EH, Yu Q, Gajewski B, Ptomey LT, Sullivan DK. Assessing the nutrition literacy of parents and its relationship with diet quality. J Nutr Educ Behav. 2016;31:493–9. doi: 10.1016/j.jneb.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Diet history questionnaire, version 2.0. National Institutes of Health; 2010. [Google Scholar]
- 36.Gibbs HD, Harvey S, Owens S, Boyle D, Sullivan DK. Engaging experts and patients to refine the nutrition literacy assessment instrument. BMC Nutrition. 2017;3:71. doi: 10.1186/s40795-017-0190-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guenther PM, Reedy J, Krebs-Smith SM. Development of the healthy eating index-2005. J Am Diet Assoc. 2008;108:1896–1901. doi: 10.1016/j.jada.2008.08.016. [DOI] [PubMed] [Google Scholar]
- 38.Diet history questionnaire II: Calculating the healthy eating index (HEI)-2010 using Diet*Calc output. [Accessed 29 August 2017]; http://epi.grants.cancer.gov/dhq2/dietcalc/output.html.
- 39.Centers for Disease Control. National Health and Nutrition Examination Survey: Anthropometry Procedures Manual. 2009 [Google Scholar]
- 40.Wirth R, Edwards MC. Item factor analysis: current approaches and future directions. Psychol Methods. 2007;12:58. doi: 10.1037/1082-989X.12.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bott MKA, Garrard L, Price LR, Mudaranthakam DP, Fajewski BJ. Confirmatory factor analysis alternative: free, accessible CBID (classical bayesian instrument development) software. West J Nurs Res. 2016 doi: 10.1177/0193945916681564. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muthén LK, Muthén BO. Mplus: statistical analysis with latent variables; user's guide;[Version 5] Muthén & Muthén; 2007. [Google Scholar]
- 43.PM HLB. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:56. [Google Scholar]
- 44.Alonso A, Laenen A, Molenberghs G, Geys H, Vangeneugden T. A unified approach to multi- item reliability. Biometrics. 2010;66:1061–1068. doi: 10.1111/j.1541-0420.2009.01373.x. [DOI] [PubMed] [Google Scholar]
- 45.Shrout PE. Measurement reliability and agreement in psychiatry. Stat Methods Med Res. 1998;7:301–317. doi: 10.1177/096228029800700306. [DOI] [PubMed] [Google Scholar]
- 46.Lackey NR, Sullivan JJ, Pett MA. Making sense of factor an alysis: The use of factor analysis for instrument development in health care research. Sage Publications; 2003. Incorporated. [Google Scholar]
- 47.Reedy J, Krebs-Smith SM, Miller PE, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144:881–889. doi: 10.3945/jn.113.189407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Parmenter K, Wardle J. Development of a general nutrition knowledge questionnaire for adults. Eur J Clin Nutr. 1999;53:298–308. doi: 10.1038/sj.ejcn.1600726. [DOI] [PubMed] [Google Scholar]
- 49.Feren A, Torheim LE, Lillegaard ITL. Development of a nutrition knowledge questionnaire for obese adults. Food & Nutrition Research. 2011;55 doi: 10.3402/fnr.v3455i3400.7271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Katz DL, Katz CS, Treu JA, et al. Teaching healthful food choices to elementary school students and their parents: the nutrition detectives™ program*. J Sch Health. 2011;81:21–28. doi: 10.1111/j.1746-1561.2010.00553.x. [DOI] [PubMed] [Google Scholar]
- 51.Kakinami L, Houle-Johnson S, McGrath JJ. Parental nutrition knowledge rather than nutrition label use is associated with adiposity in children. J Nutr Educ Behav. 2016;48:461–467. doi: 10.1016/j.jneb.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 53.Zoellner J, Estabrooks PA, Davy BM, Chen YC, You W. Exploring the theory of planned behavior to explain sugar-sweetened beverage consumption. J Nutr Educ Behav. 2012 Mar-Apr;44:172–177. doi: 10.1016/j.jneb.2011.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Conner M, Norman P, Bell R. The theory of planned behavior and healthy eating. Health Psychol. 2002;21:194. [PubMed] [Google Scholar]
- 55.Blanchard CM, Fisher J, Sparling PB, et al. Understanding adherence to 5 servings of fruits and vegetables per day: A theory of planned behavior perspective. J Nutr Educ Behav. 2009;41:3–10. doi: 10.1016/j.jneb.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dunn KI, Mohr P, Wilson CJ, Wittert GA. Determinants of fast-food consumption. An application of the theory of planned behaviour. Appetite. 2011;57:349–357. doi: 10.1016/j.appet.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 57.Vidgen HA, Gallegos D. Defining food literacy and its components. Appetite. 2014;76:50–59. doi: 10.1016/j.appet.2014.01.010. [DOI] [PubMed] [Google Scholar]
- 58.Moore LV, Roux AVD, Nettleton JA, Jacobs DR. Associations of the local food environment with diet quality—a comparison of assessments based on surveys and geographic information systems the multi-ethnic study of atherosclerosis. Am J Epidemiol. 2008;167:917–924. doi: 10.1093/aje/kwm394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the US. Am J Prev Med. 2009;36:74–81. e10. doi: 10.1016/j.amepre.2008.09.025. [DOI] [PubMed] [Google Scholar]
- 60.Von Wagner C, Steptoe A, Wolf MS, Wardle J. Health literacy and health actions: a review and a framework from health psychology. Health Educ Behav. 2009;36:860–877. doi: 10.1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 61.Tseng H-M, Liao S-F, Wen Y-P, Chuang Y-J. Stages of change concept of the transtheoretical model for healthy eating links health literacy and diabetes knowledge to glycemic control in people with type 2 diabetes. Prim Care Diabetes. doi: 10.1016/j.pcd.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 62.Bowen ME, Cavanaugh KL, Wolff K, Davis D, Gregory B, Rothman RL. Numeracy and dietary intake in patients with type 2 diabetes. The Diabetes Educator. 2013;39:240–247. doi: 10.1177/0145721713475841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gibson RS. Principles of nutritional assessment. Oxford university press; USA: 2005. [Google Scholar]
- 64.Nicklas TA, Jahns L, Bogle ML, et al. Barriers and facilitators for consumer adherence to the dietary guidelines for Americans: The HEALTH Study. J Acad Nutr Diet. 2013;113:1317–1331. doi: 10.1016/j.jand.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 65.Andrews J Craig, Netemeyer Richard G, Burton S. The nutrition elite: do only the highest levels of caloric knowledge, obesity knowledge, and motivation matter in processing nutrition ad claims and disclosures? Journal of Public Policy & Marketing. 2009;28:41–55. [Google Scholar]
- 66.van Trijp HCM, van der Lans IA. Consumer perceptions of nutrition and health claims. Appetite. 2007;48:305–324. doi: 10.1016/j.appet.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 67.Roe B, Levy AS, Derby BM. The impact of health claims on consumer search and product evaluation outcomes: results from FDA experimental data. Journal of Public Policy & Marketing. 1999;18:89–105. [Google Scholar]