Abstract
Background
Distinguishing temporal patterns of depressive symptoms during pregnancy and after childbirth has important clinical implications for diagnosis, treatment, and maternal and child outcomes. The primary aim of the present study was to distinguish patterns of chronically elevated levels of depressive symptoms v. trajectories that are either elevated during pregnancy but then remit after childbirth, v. patterns that increase after childbirth.
Methods
The report uses latent growth mixture modeling in a large, population-based cohort (N = 12 121) to investigate temporal patterns of depressive symptoms. We examined theoretically relevant sociodemographic factors, exposure to adversity, and offspring gender as predictors.
Results
Four distinct trajectories emerged, including resilient (74.3%), improving (9.2%), emergent (4.0%), and chronic (11.5%). Lower maternal and paternal education distinguished chronic from resilient depressive trajectories, whereas higher maternal and partner education, and female offspring gender, distinguished the emergent trajectory from the chronic trajectory. Younger maternal age distinguished the improving group from the resilient group. Exposure to medical, interpersonal, financial, and housing adversity predicted membership in the chronic, emergent, and improving trajectories compared with the resilient trajectory. Finally, exposure to medical, interpersonal, and financial adversity was associated with the chronic v. improving group, and inversely related to the emergent class relative to the improving group.
Conclusions
There are distinct temporal patterns of depressive symptoms during pregnancy, after childbirth, and beyond. Most women show stable low levels of depressive symptoms, while emergent and chronic depression patterns are separable with distinct correlates, most notably maternal age, education levels, adversity exposure, and child gender.
Keywords: Adversity, antepartum depression, offspring gender, postpartum depression, resilience
Elevated depressive symptoms among childbearing women are linked with increased morbidity in both the mother (Wisner et al. 2006; Yonkers et al. 2009; Meltzer-Brody & Stuebe, 2014) and her offspring (O’Connor et al. 2016). The peripartum period is an especially high-risk period for depression, where as many as 19.2% of new mothers may be diagnosed with either minor or major depression in the first 3 months (Gavin et al. 2005). Baseline prevalence rates for postpartum depression range from 6.5% to 12% (Gavin et al. 2005) and for antenatal depression from 7% to 13% (Bennett et al. 2004). However, when examining patterns of depressive symptoms over time, the picture may be more complex. First, most postpartum (in the period after childbirth and beyond) women exhibit a stable course of low levels of depressive symptoms during pregnancy and after childbirth (Affonso et al. 2000; Luoma et al. 2015). Second, some women report elevated depressive symptoms between 18 and 32 weeks of gestation but later report remitted symptoms in the 8 months after delivery, and therefore may not require intervention (Heron et al. 2004). For other women, elevated depressive symptoms in the antepartum (before parturition) period may be the beginning of a chronic state (McCall-Hosenfeld et al. 2016) (see also Putnam et al. (2017)). Documenting heterogeneous trajectories among childbearing women increases understanding of the varying course of depressive symptoms and may identify who to target for intervention during a period of heightened vulnerability. Identifying modifiable risk factors also has important public health implications for reducing or mitigating the effects of elevated depressive symptoms on both the mother and her offspring.
With the development of statistical modeling approaches capable of calculating depressive trajectories, there have been numerous studies on longitudinal patterns of depressive symptoms associated with childbirth, but only 13 have followed women prospectively from pregnancy to after childbirth (Santos et al. 2017). Two general approaches to statistical trajectory modeling have been used in these studies. Most prospective studies have employed latent class growth analysis (LCGA), a special case of growth mixture modeling, which restricts the variance of the intercept and growth model parameter to zero (Jung & Wickrama, 2008). While this approach has the advantage of reducing computational burden, it assumes that individual growth trajectories have homogeneous intercept and slope parameters. Of these studies, some have found evidence for anywhere from two (Parade et al. 2014) to five distinct classes (Hammerton et al. 2015) of depressive trajectories among childbearing women. Other approaches using LCGA have shown different subtypes of postpartum depression based on onset and chronicity of depressive symptoms [Postpartum Depression: Action Towards Causes and Treatment (PACT) Consortium, 2015].
In contrast to LCGA, latent growth mixture modeling (LGMM) (Muthén, 2004) allows growth parameters to be estimated separately for each class, thereby avoiding the assumption that intercept and slope terms are invariant. Because the assumption of a single homogeneous distribution is relaxed, models can be specified with unusual precision because growth parameters are tailored to fit the data. Studies using this approach have found evidence for more heterogeneity. For example, one study identified an additional trajectory of depressive symptoms that emerged 2 years after childbirth (Mora et al. 2009), whereas studies among women of low socioeconomic class suggest that either two (Glasheen et al. 2013) or three classes best characterize population heterogeneity (Christensen et al. 2011). The present report employed an LGMM approach using specifications that had not been used in prior work, including freely estimating both the intercept and slope parameters and the influence of covariates on these terms, as well as flexibly modeling time-varying changes on depressive symptoms across several measurement intervals.
Predictors of depressive trajectories
There are two categories of variables known to predict depressive symptoms among childbearing women that were of interest. First, sociodemographic factors such as level of education of the mother (Buttner et al. 2015), socioeconomic status (Beck, 2001), maternal age (Rubertsson et al. 2003), and offspring gender (Murray et al. 1993) have been shown to influence risk for depression.
Second, exposure to adversity during pregnancy increases risk for elevated depressive symptoms both during pregnancy (Lancaster et al. 2010) and after childbirth (Robertson et al. 2004). Exposure to interpersonal stressors is most closely associated with depressive symptoms among antenatal and postpartum women (Xie et al. 2009; Wright et al. 2015), although a diverse range of major life events also increases risk (Stone et al. 2015; Fredriksen et al. 2017; Mukherjee et al. 2017). Prior studies have examined stressor exposure in a yes/no self-report format, leaving open the question of outcomes associated with the perceived impact of exposure. This is an important distinction as prior research has suggested that perceptions about exposure have a substantial effect on outcomes (Bonanno et al. 2011).
Current study
The primary aim of the present study was to distinguish patterns of chronically elevated levels of depressive symptoms v. trajectories that are elevated in the antepartum phase but then remit after childbirth, v. patterns that increase after childbirth. Our secondary aim was to identify sociodemographic and adversity exposure factors that, when measured prospectively, distinguish trajectories of depression antepartum, post-partum, and beyond. The present report applies a comparative individual differences framework to a large, prospective population-based cohort using a statistical modeling technique that offers three distinct advantages over prior studies. (1) Prior work has not used an approach that allows for the flexible modeling of variation in growth parameters across different classes. (2) Second, we modeled time parameters freely as the increments of change across measurement intervals are not equivalent. (3) Third, we evaluated whether sociodemographic factors, child gender, and exposure to adversity while pregnant predicted membership in distinct classes.
Methods
Procedure
Data are drawn from the Avon Longitudinal Study of Parents and Children (ALSPAC), a longitudinal prospective observational study investigating influences on health and development across the lifespan (Boyd et al. 2013). This birth cohort population study focused on women residing in a circumscribed geographic region in the South West of England with an expected date of delivery between April 1, 1991 and December 31, 1992 [see Fraser et al. (2013) for complete details on study procedures and Golding et al. (2001) on study recruitment]. Ethical approval for the study was obtained from the ALSPAC Ethics and Law Committee and the Local Research Ethics Committees. Subjects provided written informed consent after receiving a complete description of the study. The study website contains all details through a fully searchable data dictionary (http://www.bris.ac.uk/alspac/researchers/data-access/data-dictionary/). Participants included in the present report were assessed across seven waves from 1990 to 1995 at 18 and 32 weeks of gestation, 8 weeks after the birth of the baby, and thereafter at 8, 21, 33, and 61 months.
Participants
The complete study cohort consists of 14 541 pregnancies and 13 998 children still alive at 12 months of age. Our sample in the present report consisted of 12 121 mothers who completed questionnaires assessing depressive symptoms. Participation rates for each wave of data collection were: 18 weeks gestation (n = 12 121, 100%); 32 weeks gestation, n = 12 096 (99.8%); 8 weeks postpartum, n = 11 710 (96.6%); 8 months postpartum, n = 11 195 (92.3%); 2 years post-partum, n = 10 259 (84.6%); 3 years postpartum, n = 9595 (79.2%); and 5 years postpartum, n = 8950 (73.8%). As reported in previous studies, mothers lost from the cohort were significantly more likely to endorse higher levels of depression and anxiety (Heron et al. 2004), to have lower education levels, and to report greater social adversity (Boyd et al. 2013). Complete details regarding sample distribution of ethnicity, social class, and maternal and paternal education can be found in online Supplementary material 1.
Measures
Demographics
Maternal age at delivery was calculated by subtracting the offspring delivery date from the maternal date of birth. Sex of the child was obtained from both the birth notification and postmortem examinations in the absence of birth notification. Maternal social class was determined by calculating a composite variable based on the mother’s occupation, primary tasks, and job role status (e.g. foreman, supervisor) using the UK Office of Population Census & Surveys (OPCS) classification system (Office of Population Census & Surveys, 1991), resulting in six categories: I (professional), II (managerial and technical), IIIa (skilled manual), IIIb (skilled non-manual), IV (semi-skilled), and V (unskilled). To aid in model interpretation and convergence, we collapsed maternal class into three categories by combining professional and managerial categories (I and II), skilled (IIIa and IIIb), and semi-skilled and unskilled (IV and V). Maternal and paternal education corresponded to the highest attainment at late pregnancy; 1, certificate of secondary education/none; 2, vocational; 3, ordinary level; 4, advanced level; 5, university degree.
Adversity variables
Mothers completed a life-events inventory of 42 items at 18 weeks of gestation (Brown & Harris, 1978; Barnett et al. 1983). Mothers were asked, ‘Listed below are a number of events that may have brought changes in your life. Have any of these [e.g. friend or relative died] occurred since you became pregnant? If so, please assess how much effect it had on you.’ Responses were recorded on a 1–5 scale, with 1, affected me a lot; 2, moderately affected me; 3, mildly affected me; 4, no effect; 5, did not happen. ALSPAC pilot studies suggest that both the impact score and a count tally of the number of events are highly correlated, with the former being more sensitive to emotional well-being. For the purposes of the present report, variables were first recorded (1,2,3,4, = 4,3,2,1) (5 = 0). Then, we combined variables into conceptually related domains according to theory and a principle components analyses. This generated five variables of perceived impact across several domains: bereavement (loss of a friend, relative, child, or partner); medical (illness in a partner, child, friend, or family member; mother’s hospitalization; fear of miscarriage; fetal abnormality); interpersonal (arguing with partner, friends, or family; partner cruelty to mother or child; partner physically hurting mother or child; divorce; separation; partner absence; partner not wanting child); financial and employment (partner or mother loosing job, partner or mother having problems at work, mother experiencing reduction in income or financial difficulty); and housing (becoming homeless, moving, or being burglarized). Before summing items within each domain, scores were first standardized to equalize response variability.
Maternal depression
The Edinburgh Post-Natal Depression Scale (EPDS) (Cox et al. 1987) is a 10-item questionnaire that assesses depressive symptomatology in women during pregnancy and after delivery. Each item is scored from 0 to 3 with 0 representing no endorsement and 3 representing full endorsement (note: some items are reversed scored), yielding a sum score ranging from 0 to 30. The scale has been validated with standardized psychiatric interviews (Cox et al. 1996), and has shown adequate reliability and validity in large, diverse international samples (Affonso et al. 2000).
Statistical analysis
We used Mplus, Version 7.4 (Muthén & Muthén, 1988–2015) to identify latent depression trajectories. We specified a full-information maximum-likelihood (FMIL) estimation procedure to handle missing data (Enders, 2001). FMIL assumes that missing data are unrelated to the outcome variable (missing at random) and its use is widely accepted (Graham, 2009). Most participants had complete data at a minimum of three time points, 86.3%. For all time points, the percentages of missing data were: one time point, 16.5%; two time points, 9%; three time points, 7%; four time points, 4.7%; five time points, 4.7%; and six time points, 4.4%. To assess the effects of missing data patterns, Mplus estimates covariance coverage for all pairs of variables; values should be above a minimum threshold of 0.10 for model convergence. In the present study, covariance coverage for each pair of variables did not fall below 0.77.
Analyses proceeded in three steps (Jung & Wickrama, 2008). First, we determined the number of classes that optimally characterized individual differences in depressive symptoms by identifying a univariate single-class growth model without covariates. Second, we compared fit of progressive one- to six-class models, using conventional indices to assess fit. Third, we included covariates in a multinomial logistic regression on class membership (Muthén, 2004). We inspected modification indices to determine retention of default specifications. In an iterative process, we tested models with different covariates, comparing log-likelihood ratios and using χ2 tests to adjudicate relative improvement in fit. To ensure that our final model did not represent a local solution, we varied the number of random starts and replicated the two best log-likelihoods using the OPTSEED procedure, confirming that model parameter estimates were replicated (Jung & Wickrama, 2008). We regressed covariates on class membership and on growth parameters, and used log-likelihood ratio χ2 tests to optimize model fit (Muthén, 2004). Finally, we examined the effect of exposure to adversity at baseline by including these variables as covariates within the best-fitting LGMM.
Results
Unconditional models
We began by estimating a simple growth model without covariates. To identify factor loadings for the time points, we reasoned that the increment of change in depressive symptoms was likely to vary between pregnancy and the 5 years after childbirth, and thus would assume a non-linear form. We sought to confirm this using several model fitting procedures, examining models with linear-only, linear and quadratic, and a freely estimated slope parameter (first wave set to 0 and last wave set to 1, and the remaining freely estimated). Based on log-likelihood χ2 testing, we retained the model with freely estimated factor loadings. We allowed the intercept variance to be estimated across classes, but we fixed the slope variance at 0 across classes to address problems with non-convergence.
We then compared successive solutions from one to six classes in unconditional models. Table 1 summarizes the fit statistics for the one- to six-class solutions. To adjudicate model fit, we used the Aikaike information criterion (AIC), Bayesian information criteria (BIC), the sample size-adjusted Bayesian information criteria (SSBIC), the Vuong-Lo-Mendell-Rubin likelihood ratio test (VLMRT) (Lo et al. 2001), and the bootstrapped likelihood test (BLRT) (Nylund et al. 2007). We sought a model with a significant p value for the k-1 v. k class models (VMLRT and BLRT), a higher value for entropy, and lower values for the BIC, AIC, and SSBIC, as well as theoretical coherence and interpretability (Muthén, 2004; Nylund et al. 2007). Each model from one to six classes provided successive improvements in fit according to the AIC, BIC, SSBIC. While the five-class solution showed slightly improved fit over the four-class solution, it fragmented the stable low trajectory into two close but parallel trajectories, which carries little theoretical relevance. Additionally, the VLMRT p value for the k-1 class solution at five and six classes was not significant. Based on fit indices as well as theoretical interpretability, we adopted the four-class solution for subsequent examination in conditional models.
Table 1.
Fit indices for one- to six-class growth mixture models (unconditional)
| Fit indices | Growth mixture model | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| One class | Two classes | Three classes | Four classes | Five classes | Six classes | |
| LL | −212 049.80 | −211 324.76 | −210 586.58 | −210 309.07 | −210 150.20 | −210 034.95 |
| AIC | 424 129.60 | 422 658.52 | 421 215.15 | 420 666.14 | 420 354.39 | 420 129.91 |
| BIC | 424 242.53 | 422 821.04 | 421 373.25 | 420 846.83 | 420 557.67 | 420 355.77 |
| SSBIC | 424 194.86 | 422 763.83 | 421 306.52 | 420 770.56 | 420 471.86 | 420 260.43 |
| Entropy | – | 0.76 | 0.71 | 0.75 | 0.72 | 0.74 |
| VLMRT p value | – | <0.001 | <0.001 | <0.01 | 0.12 | 0.18 |
| BLRT p value | – | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
LL, log likelihood; AIC, Akaike information criterion; BIC, Bayesian information criterion; SSBIC, sample size-adjusted Bayesian information criterion; VLMRT, Vuong-Lo-Mendell-Rubin likelihood ratio test; BLRT, parametric bootstrapped likelihood ratio test.
Conditional model
Next, we sought to extend the model to include relevant covariates. We regressed class membership on offspring gender, maternal age and education, paternal education, and maternal social class, improving model fit. Entropy for the conditional model increased from 0.75 in the unconditional four-class model to 0.77 in the conditional model, indicating improved classification accuracy. Finally, we regressed the intercept and slope growth parameters (class-invariant) on maternal age, further improving model fit. Inclusion of covariates resulted in trajectory patterns and class membership probabilities that were nearly identical to the unconditional model.
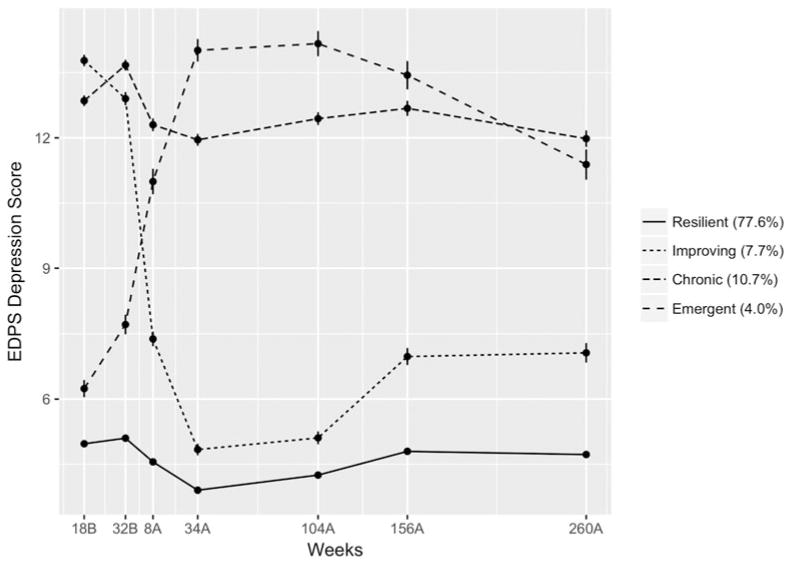
Figure 1 shows that most participants in the conditional model (77.6%) were assigned to a class with stable low depressive symptoms, which we labeled resilient. This class had the lowest intercept (b = 6.25, S.E. = 0.37, p < 0.001) and a significant negative slope (b = −1.79, S.E. = 0.27, p < 0.001). The next largest class (10.7%) had individuals with high levels of depressive symptoms both during pregnancy and after childbirth, declining slightly over the 5 years after childbirth, a group we labeled chronic depression. This group had a high intercept (b = 13.55, S.E. = 0.46, p < 0.001) and a significant negative slope (b = −1.83, S.E. = 0.35, p < 0.001). A third class of individuals (7.7%) had elevated levels of depressive symptoms during pregnancy that declined after the birth, a group we labeled improving. This class had a higher intercept (b = 13.79, S.E. = 0.48, p < 0.001) and a significant negative slope (b = −6.52, S.E. = 0.66, p < 0.001). Finally, we identified a group of participants who had moderate levels of depressive symptoms during pregnancy followed by a sharp elevation after childbirth (4.0%). This emergent group had a moderate intercept (b = 7.98, S.E. = 0.52, p < 0.001) and a significant positive slope (b = 3.53, S.E. = 0.43, p < 0.001).
Fig. 1.
Four-class conditional trajectory model of EPDS depression scores (n = 9111). B, weeks before childbirth; A, weeks after childbirth; standard error bars represent standard error of the mean (S.E.M.).
Next, we examined covariate predictors of trajectory class assignment, as shown in Table 2. In the first analyses, the resilient class served as the referent. Compared with the resilient class, mothers in the chronic class had fewer years of education (Est = −0.14, S.E. = 0.05, p = 0.008), as did their partners (Est = −0.08, S.E. = 0.04, p = 0.043). Mothers in the improving group were younger at delivery (Est = −0.06, S.E. = 0.02, p = 0.001) and were more likely to be in a lower social class (Est = 0.67, S.E. = 0.17, p = 0.000). Finally, compared with the chronic group, the emergent group was more likely to have a female child (Est = −0.35, S.E. = 0.16, p = 0.033).
Table 2.
Multinomial regression estimates for covariate predictors of class membership
| Resilient v. | Chronic v. | Improving v. | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Chronic | Emergent | Improving | Emergent | Improving | Emergent | |||||||
|
|
|
|
|
|
|
|||||||
| Est. | S.E. | Est. | S.E. | Est. | S.E. | Est. | S.E. | Est. | S.E. | Est. | S.E. | |
| Covariates | ||||||||||||
| Child gender (1 = male, 2 = female) | −0.13 | 0.09 | 0.23† | 0.13 | 0.08 | 0.10 | 0.35* | 0.16 | 0.21 | 0.14 | 0.14 | 0.16 |
| Maternal age | −0.02 | 0.02 | −0.02 | 0.02 | −0.06** | 0.02 | 0.00 | 0.02 | −0.04† | 0.02 | 0.04 | 0.03 |
| Maternal education | −0.14** | 0.05 | −0.04 | 0.08 | −0.05 | 0.06 | 0.10 | 0.10 | 0.09 | 0.08 | 0.01 | 0.09 |
| Partner education | −0.08* | 0.04 | −0.00 | 0.07 | −0.08† | 0.05 | 0.08 | 0.08 | 0.00 | 0.06 | 0.07 | 0.08 |
| Middle maternal social classa | 0.15 | 0.11 | −0.06 | 0.16 | 0.07 | 0.13 | −0.21 | 0.20 | −0.09 | 0.17 | −0.12 | 0.19 |
| Low maternal social classa | 0.28† | 0.17 | 0.30 | 0.24 | 0.67*** | 0.17 | 0.02 | 0.30 | 0.39 | 0.24 | −0.38 | 0.27 |
| Adversity domainsb | ||||||||||||
| Bereavement | 0.04 | 0.02 | −0.01 | 0.06 | 0.03 | 0.02 | −0.05 | 0.06 | −0.01 | 0.03 | −0.04 | 0.06 |
| Medical | 0.11*** | 0.01 | 0.04* | 0.02 | 0.10*** | 0.01 | −0.07*** | 0.03 | −0.01 | 0.02 | −0.06* | 0.02 |
| Interpersonal | 0.29*** | 0.04 | 0.21*** | 0.04 | 0.29*** | 0.04 | −0.08* | 0.04 | −0.01 | 0.01 | −0.07* | 0.03 |
| Financial | 0.17*** | 0.02 | 0.10*** | 0.02 | 0.15*** | 0.02 | −0.08** | 0.02 | −0.02 | 0.02 | −0.06* | 0.02 |
| Housing | 0.13*** | 0.03 | 0.06 | 0.05 | 0.10*** | 0.03 | −0.07 | 0.05 | −0.03 | 0.03 | −0.04 | 0.05 |
Est., parameter estimate; S.E., standard error.
High maternal class served as the referent.
Adversity was measured at 18 weeks of gestation.
p < 0.10;
p < 0.05;
p < 0.01;
p < 0.001.
In addition to demographic factors, we included appraised adversity exposure as additional covariate predictors of trajectory class assignment (see Table 3). Compared with mothers in the resilient group, those in the chronic, emergent, and improving groups reported that they were more severely affected by every category of stressor considered in this analysis, except for bereavement. Specifically, when compared with the resilient group, mothers in the chronic, emergent, and improving groups all reported greater exposure to medical adversity, interpersonal adversity, and financial difficulty. Again, compared with the resilient group, only mothers in the chronic and improving groups experienced greater difficulty with housing. Compared with mothers in the chronic group, mothers in the improving group were less likely to report medical adversity, interpersonal difficulty, and financial adversity. There were no significant differences between mothers in the chronic and improving groups in terms of appraised exposure to adversity. Finally, compared with the improving group, mothers in the emergent group were less likely to experience medical, interpersonal, and financial adversity.
Table 3.
Descriptive statistics by depression trajectory class
| Variable | Improving | Resilient | Emergent | Chronic | F or χ2 |
|---|---|---|---|---|---|
| Demographics | |||||
| Child gender (% female)a | 51.6% | 48.6% | 53.6% | 45.0% | 11.06* |
| Maternal age | 27.16 (5.04) | 28.9 (4.49) | 28.61 (4.74) | 28.13 (4.82) | 37.23*** |
| Maternal education | 3.02 (1.16) | 3.34 (1.15) | 3.28 (1.23) | 2.98 (1.22) | 38.60*** |
| Partner education | 3.04 (1.34) | 3.38 (1.32) | 3.36 (1.39) | 3.06 (1.36) | 27.60*** |
| Maternal class, highb | 30.0% | 41.4% | 39.6% | 30.7% | 68.28*** |
| Maternal class. middle | 49.0% | 49.2% | 47.0% | 56.2% | 18.24*** |
| Maternal class, low | 21.0% | 9.4% | 13.4% | 13.1% | 97.99*** |
| Adversity measuresc | |||||
| % Bereaved | 14.5 | 13.2 | 15.5 | 15.4 | 4.98 |
| Medical | 0.99 (4.63) | −0.29 (3.42) | 0.46 (3.81) | 1.24 (4.58) | 62.20*** |
| Interpersonal | 1.40 (5.84) | −1.01 (2.76) | 0.14 (4.82) | 1.61 (5.29) | 212.62*** |
| Financial | 1.43 (4.16) | −0.39 (2.97) | 0.56 (3.65) | 1.41 (4.16) | 129.18*** |
| Housing | 0.27 (2.35) | −0.19 (1.42) | 0.08 (2.12) | 0.36 (2.68) | 37.70*** |
| Functioning measures | |||||
| Dep. sx., 18 weeks gest. | 13.78 (3.38) | 4.97 (3.30) | 6.24 (3.65) | 12.85 (3.62) | 2526.38*** |
| Dep. sx., 32 weeks gest. | 12.90 (3.95) | 5.10 (3.63) | 7.72 (4.28) | 13.67 (3.81) | 2233.75*** |
| Dep. sx., 8 weeks post | 7.38 (4.19) | 4.55 (3.53) | 10.99 (5.36) | 12.30 (4.27) | 1367.69*** |
| Dep. sx., 8 months post | 4.84 (3.19) | 3.90 (3.23) | 14.02 (4.63) | 11.96 (3.92) | 2179.65*** |
| Dep. sx., 2 years post | 5.11 (3.41) | 4.25 (3.45) | 14.17 (4.97) | 12.44 (4.07) | 1788.02*** |
| Dep. sx., 3 years post | 6.98 (4.131) | 4.80 (3.86) | 13.44 (5.52) | 12.68 (4.56) | 1150.27*** |
| Dep. sx., 5 years post | 7.06 (4.86) | 4.72 (4.06) | 11.39 (5.70) | 11.98 (4.87) | 739.31*** |
Gest, gestation; Dep. sx’s, depressive symptoms. Standard deviations are in parentheses.
Percentages represent % within total gender. 48.7% of the total offspring sample was female.
Percentages calculated using trajectory by social class/trajectory total.
Adversity values for all variables except bereavement are reported in summed z-scores with negative values representing fewer exposures relative to the mean, and positive values indicating more exposure relative to the mean.
p < 0.05;
p < 0.01;
p < 0.001.
Discussion
This study had two aims: (1) to distinguish trajectories of chronically elevated levels of depressive symptoms from trajectories that are either elevated during pregnancy but then remit after childbirth, or increase after childbirth; (2) to identify sociodemographic and appraised adversity exposure factors that, when measured prospectively, distinguish trajectory membership. Using LGMM, a four-class solution best characterized patterns of depressive symptoms during pregnancy, after childbirth, and beyond. A clear majority of women (77.6%) demonstrated a resilient pattern characterized by stable, low levels of depressive symptoms. However, 10.7% displayed a chronic pattern characterized by consistently elevated levels of depressive symptoms both before and after childbirth, while 4.0% evidenced an emergent pattern, consisting of low depressive symptoms prior to childbirth, which became elevated after childbirth. Finally, 7.7% evidenced a rarely documented improving pattern whereby elevated levels of depressive symptoms prior to the birth steadily declined in the postpartum period.
Our study findings highlight two particularly high-risk patterns – emergent and chronic, where treatment can potentially have an impact on the 14–15% of pregnant women who may require more intensive screening and monitoring. The critical issue is to distinguish women during pregnancy who have low symptoms and will continue to do so (resilient) from emergent – and then to distinguish those who will improve from those who are chronic. In terms of prediction, the chronic group had lower maternal and partner education compared with the resilient group, as well as greater perceived exposure to adversity across medical, interpersonal, financial, and housing domains. The effects of adversity on depression among perinatal women (Seng et al. 2013; Yonkers et al. 2014) are well established, and data presented here demonstrated that interpersonal stressors exert a threefold increased risk for depression among the chronic and emergent groups compared with other types of adversity, consistent with prior work (Wright et al. 2015).
The second high-risk group is the emergent group for whom depressive symptoms do not manifest until after childbirth; they are clearly distinct from the chronic group. This group may not report elevations in depressive symptoms during pregnancy, but could be confused with women with chronically elevated profiles if assessed following childbirth. What factors distinguish these women? First, having a female offspring increased odds of experiencing emergent compared with chronic trajectories and, marginally, differentiated resilient from emergent groups. Why would female gender increase risk for membership in the emergent group v. the chronic group? Prior work has demonstrated mood-destabilizing effects associated with sensitivity to hormonal events of pregnancy and childbirth in a subgroup of women (Bloch et al. 2000; Pedersen et al. 2016), and there is sufficient evidence to suggest that fluctuations in hormones during pregnancy and the postpartum period may trigger postpartum depression (PPD) in susceptible women [see Schiller et al. (2015) for a review]. Though largely unexplored in the extant literature and a speculative interpretation, fetal gender may moderate neuroendocrine pathophysiology for PPD given the higher loading of gonadal hormones associated with female fetuses (Yaron et al. 2002). Alternatively, non-biological variables may also account for the association between offspring gender and risk for depressive symptoms.
Second, the emergent group was less likely than the chronic group to report stressful experiences. This suggests that membership in the emergent class is likely a consequence of childbirth itself. Third, our model suggests that for women who experience an increase in depressive symptoms after childbirth, this elevated pattern may persist for up to 5 years. These findings are consistent with prior population-based cohort studies that have found evidence for an increased prevalence of depressive symptoms after the first postpartum year (Aasheim et al. 2012; Woolhouse et al. 2015).
Results also offer some clues as to the factors that distinguish the improving group from the chronic, a critical distinction as these two groups could be confused during pregnancy, even though some will ultimately recover on their own. Though of marginal significance, mothers in the improving group were younger compared with those in the chronic group. Second, compared with the resilient class, the improving class was younger at age of delivery, of lower social class, and reported greater exposure to medical, interpersonal, and financial strain. A key point here is that the improving group is distinct from the resilient group, and likely to engage in different coping patterns during pregnancy and after childbirth (Bonanno, 2004). What could explain the remission of depression post-childbirth among these mothers? Though the research on postpartum recovery is sparse, this pattern of post-adversity improvement has been well documented in other exposure groups (Mancini et al. 2016). While it is possible that the improving mothers in the present study could have accessed mental health services after delivery, a study in Ghana and the Côte d’Ivoire found evidence of the improving pattern among new mothers not exposed to treatment, noting associations with reduced marital and economic stress after childbirth, as well as parity (Barthel et al. 2016). Further research on this improving group promises to identify yet undiscovered pathways to postpartum adjustment among mothers.
Finally, most women in this study reported a pattern of stable, low depressive symptoms during pregnancy, after childbirth, and beyond, suggesting that low depressive symptoms may be normative. A substantial body of work has demonstrated that resilience is often the predominant response trajectory after exposure to stressors (Bonanno, 2004), and the present report is among the first to demonstrate its presence in the context of childbirth [see also Barthel et al. (2016) and Galatzer-Levy et al. (2011)]. Resilient mothers were more likely to be older than the mothers in the improving class, consistent with prior work noting that older age is a protective factor after childbirth (Rubertsson et al. 2003; Buttner et al. 2015). Second, mothers in this class reported reduced exposure to adversity compared with those in the emergent, chronic, and improving categories. The key implication of this finding is that rather than being unusually healthy, mothers is this class have effective strategies to maintain equilibrium, even if these strategies are not necessarily universally advantageous. For example, studies have shown that self-enhancing biases are linked to coping with exposure to extreme adversity (Bonanno et al. 2002), even though self-enhancement can evoke negative impressions from others. The critical challenge for future research on peripartum resilience is to identify the complex multiple pathways to resilience that new mothers are likely to demonstrate.
Several limitations should be considered when interpreting the primary findings. Most importantly, although we controlled for baseline depressive symptoms, we did not have data on prior family or personal history of depression. Thus, we were unable to evaluate whether trajectories of depression symptoms differed by prior depression or a family history of depression. Nor could we adjust for these factors in examining the association of adversity and other risk factors with depression trajectories. This limits the interpretation we can make from these data; for example, familial loading for depression could be associated with increased exposure to adversity and risk of being in the chronic trajectory, thus inflating that association. Second, depressive symptoms were assessed via self-report and were not adequate markers of clinical depression. This has two major implications. First, we are limited in the extent to which we can generalize our findings to defined clinical criteria for perinatal depression and major depression as established in the Diagnostic and Statistical Manual of Mental Disorders (DSM) 5 (American Psychiatric Association, 2013) and International Classification of Diseases (ICD)-9 given that our postpartum measurement fell outside the 4-week postpartum window per the DSM 5, and outside the 6-week window per the ICD-9. Second, prior work has shown that prevalence estimates tend to be higher when symptoms, rather than clinical criteria are used (Bennett et al. 2004) and we may therefore have inflated estimates of depressive experiences among this group. Third, adverse event chronicity is unknown. This is important given that the type of adversity and its timing can impact the course of subsequent mood symptoms (Class et al. 2014; Keyes et al. 2014). Fourth, this study did not consider other known risk factors for depression in the modeling, such as high parity, low social support, and low self-esteem. Fifth, this sample was notable for its lack of representation from non-white ethnicities; the generalizability of our findings to other ethnicities is limited. Finally, data were collected several decades prior to this report and caution should be exercised when interpreting findings given the potentially limited generalizability to contemporary settings. These limitations notwithstanding the current report builds on a body of literature suggesting the presence of heterogeneous depressive symptoms both during pregnancy and in the 5 years after childbirth, offering some insight into variables that distinguish resilient, chronic, improving, and emergent depressive symptom trajectories.
Supplementary Material
Acknowledgments
The authors are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses. The UK Medical Research Council and Wellcome (Grant ref: 102215/2/13/2) and the University of Bristol provide core support for ALSPAC. The authors would also like to thank Lori Chibnik for her assistance with generating the graphics. This publication is the work of the authors and Christy A. Denckla, Anthony D. Mancini, Nathan S. Consedine, Snezana Milanovic, Archana Basu, Soraya Seedat, Georgina Spies, David C. Henderson, George A. Bonanno, and Karestan C. Koenen will serve as guarantors for the contents of this paper.
Footnotes
The supplementary material for this article can be found at https://doi.org/10.1017/S0033291717002549.
Conflict of Interest
None.
References
- Aasheim V, Waldenstrom U, Hjelmstedt A, Rasmussen S, Pettersson H, Schytt E. Associations between advanced maternal age and psychological distress in primiparous women, from early pregnancy to 18 months postpartum. BJOG. 2012;119:1108–1116. doi: 10.1111/j.1471-0528.2012.03411.x. [DOI] [PubMed] [Google Scholar]
- Affonso DD, De AK, Horowitz JA, Mayberry LJ. An international study exploring levels of postpartum depressive symptomatology. Journal of Psychosomatic Research. 2000;49:207–216. doi: 10.1016/s0022-3999(00)00176-8. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. DSM 5. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; Washington, DC: 2013. [Google Scholar]
- Barnett BEW, Hanna B, Parker G. Life event scales for obstetric groups. Journal of Psychosomatic Research. 1983;27:313–320. doi: 10.1016/0022-3999(83)90054-5. [DOI] [PubMed] [Google Scholar]
- Barthel D, Kriston L, Barkmann C, Appiah-Poku J, Te Bonle M, Esther Doris KY, Carine Esther BK, Jean Armel KE, Mohammed Y, Osei Y, Fordjour D, Owusu D, Eberhardt KA, Hinz R, Kofff M, N’Goran E, Nguah SB, Tagbor H, Schoppen S, Ehrhardt S, Bindt C. Longitudinal course of ante- and postpartum generalized anxiety symptoms and associated factors in West-African women from Ghana and Côte d’Ivoire. Journal of Affective Disorders. 2016;197:125–133. doi: 10.1016/j.jad.2016.03.014. [DOI] [PubMed] [Google Scholar]
- Beck CT. Predictors of postpartum depression: an update. Nursing Research. 2001;50:275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstetrics & Gynecology. 2004;103:698–709. doi: 10.1097/01.AOG.0000116689.75396.5f. [DOI] [PubMed] [Google Scholar]
- Bloch M, Schmidt PJ, Danaceau M, Murphy J, Nieman L, Rubinow DR. Effects of gonadal steroids in women with a history of postpartum depression. American Journal of Psychiatry. 2000;157:924–930. doi: 10.1176/appi.ajp.157.6.924. [DOI] [PubMed] [Google Scholar]
- Bonanno GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? American Psychologist. 2004;59:20–28. doi: 10.1037/0003-066X.59.1.20. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Field NP, Kovacevic A, Kaltman S. Self-enhancement as a buffer against extreme adversity: civil war in Bosnia and traumatic loss in the United States. Personality and Social Psychology Bulletin. 2002;28:184–196. [Google Scholar]
- Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annual Review of Clinical Psychology. 2011;7:511–535. doi: 10.1146/annurev-clinpsy-032210-104526. [DOI] [PubMed] [Google Scholar]
- Boyd A, Golding J, Macleod J, Lawlor DA, Fraser A, Henderson J, Molloy L, Ness A, Ring S, Davey Smith G. Cohort profile: the ‘children of the 90s’ – the index offspring of the Avon longitudinal study of parents and children. International Journal of Epidemiology. 2013;42:111–127. doi: 10.1093/ije/dys064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GW, Harris T. Social Origins of Depression: A Study of Psychiatric Disorder in Women. Tavistock Press; London: 1978. [Google Scholar]
- Buttner MM, Brock RL, O’Hara MW. Patterns of women’s mood after delivery: a growth curve analysis. Journal of Affective Disorders. 2015;174:201–208. doi: 10.1016/j.jad.2014.11.022. [DOI] [PubMed] [Google Scholar]
- Christensen AL, Stuart EA, Perry DF, Le HN. Unintended pregnancy and perinatal depression trajectories in low-income, high-risk Hispanic immigrants. Prevention Science. 2011;12:289–299. doi: 10.1007/s11121-011-0213-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Class QA, Abel KM, Khashan AS, Rickert ME, Dalman C, Larsson H, Hultman CM, Langstrom N, Lichtenstein P, D’Onofrio BM. Offspring psychopathology following preconception, prenatal and postnatal maternal bereavement stress. Psychological Medicine. 2014;44:71–84. doi: 10.1017/S0033291713000780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh postnatal depression scale (EPDS) in non-postnatal women. Journal of Affective Disorders. 1996;39:185–189. doi: 10.1016/0165-0327(96)00008-0. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- Enders CK. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychological Methods. 2001;6:352–370. [PubMed] [Google Scholar]
- Fraser A, Macdonald-Wallis C, Tilling K, Boyd A, Golding J, Davey Smith G, Henderson J, Macleod J, Molloy L, Ness A, Ring S, Nelson SM, Lawlor DA. Cohort profile: the Avon longitudinal study of parents and children: ALSPAC mothers cohort. International Journal of Epidemiology. 2013;42:97–110. doi: 10.1093/ije/dys066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen E, von Soest T, Smith L, Moe V. Patterns of pregnancy and postpartum depressive symptoms: latent class trajectories and predictors. Journal of Abnormal Psychology. 2017;126:173–183. doi: 10.1037/abn0000246. [DOI] [PubMed] [Google Scholar]
- Galatzer-Levy IR, Mazursky H, Mancini AD, Bonanno GA. What we don’t expect when expecting: evidence for heterogeneity in subjective well-being in response to parenthood. Journal of Family Psychology. 2011;25:384–392. doi: 10.1037/a0023759. [DOI] [PubMed] [Google Scholar]
- Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T. Perinatal depression: a systematic review of prevalence and incidence. Obstetrics & Gynecology. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- Glasheen C, Richardson GA, Kim KH, Larkby CA, Swartz HA, Day NL. Exposure to maternal pre- and postnatal depression and anxiety symptoms: risk for major depression, anxiety disorders, and conduct disorder in adolescent offspring. Developmental Psychopathology. 2013;25:1045–1063. doi: 10.1017/S0954579413000369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golding J, Pembrey M, Jones R, Team TAS. ALSPAC-The Avon longitudinal study of parents and children. Paediatric and Perinatal Epidemiology. 2001;15:74–87. doi: 10.1046/j.1365-3016.2001.00325.x. [DOI] [PubMed] [Google Scholar]
- Graham JW. Missing data analysis: making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Hammerton G, Mahedy L, Mars B, Harold GT, Thapar A, Zammit S, Collishaw S. Association between maternal depression symptoms across the first eleven years of their child’s life and subsequent offspring suicidal ideation. PLoS ONE. 2015;10:e0131885. doi: 10.1371/journal.pone.0131885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heron J, O’Connor TG, Evans J, Golding J, Glover V, Team AS. The course of anxiety and depression through pregnancy and the postpartum in a community sample. Journal of Affective Disorders. 2004;80:65–73. doi: 10.1016/j.jad.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Social and Personality Psychology Compass. 2008;2(1):302–317. [Google Scholar]
- Keyes KM, Pratt C, Galea S, McLaughlin KA, Koenen KC, Shear KM. The burden of loss: unexpected death of a loved one and psychiatric disorders across the life course in a national study. American Journal of Psychiatry. 2014;171:864–871. doi: 10.1176/appi.ajp.2014.13081132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: a systematic review. American Journal of Obstetrics and Gynecology. 2010;202:5–14. doi: 10.1016/j.ajog.2009.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Luoma I, Korhonen M, Salmelin RK, Helminen M, Tamminen T. Long-term trajectories of maternal depressive symptoms and their antenatal predictors. Journal of Affective Disorders. 2015;170:30–38. doi: 10.1016/j.jad.2014.08.017. [DOI] [PubMed] [Google Scholar]
- Mancini AD, Littleton HL, Grills AE. Can people benefit from acute stress? Social support, psychological improvement, and resilience after the Virginia Tech campus shootings. Clinical Psychological Science. 2016;4:401–417. [Google Scholar]
- McCall-Hosenfeld JS, Phiri K, Schaefer E, Zhu J, Kjerulff K. Trajectories of depressive symptoms throughout the peri- and postpartum period: results from the First Baby Study. Journal of Women’s Health. 2016;25:1112–1121. doi: 10.1089/jwh.2015.5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer-Brody S, Stuebe A. The long-term psychiatric and medical prognosis of perinatal mental illness. Best Practice & Research Clinical Obstetrics & Gynaecology. 2014;28:49–60. doi: 10.1016/j.bpobgyn.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mora PA, Bennett IM, Elo IT, Mathew L, Coyne JC, Culhane JF. Distinct trajectories of perinatal depressive symptomatology: evidence from growth mixture modeling. American Journal of Epidemiology. 2009;169:24–32. doi: 10.1093/aje/kwn283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee S, Coxe S, Fennie K, Madhivanan P, Trepka MJ. Stressful life event experiences of pregnant women in the United States: a latent class analysis. Women’s Health Issues. 2017;27:83–92. doi: 10.1016/j.whi.2016.09.007. [DOI] [PubMed] [Google Scholar]
- Murray L, Kempton C, Woolgar M, Hooper R. Depressed mothers’ speech to their infants and its relation to infant gender and cognitive development. Journal of Child Psychology and Psychiatry. 1993;34:1083–1101. doi: 10.1111/j.1469-7610.1993.tb01775.x. [DOI] [PubMed] [Google Scholar]
- Muthén B. Latent variable analysis: growth mixture modeling and related techniques for longitudinal data. In: Kaplan D, editor. The Sage Handbook of Quantitative Methodology for the Social Sciences. Sage Publications; Thousand Oaks, CA: 2004. pp. 345–368. [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7. Muthén & Muthén; Los Angeles, CA: 1988–2015. [Google Scholar]
- Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14:535–569. [Google Scholar]
- O’Connor TG, Monk C, Burke AS. Maternal affective illness in the perinatal period and child development: findings on developmental timing, mechanisms, and intervention. Current Psychiatry Reports. 2016;18:24. doi: 10.1007/s11920-016-0660-y. [DOI] [PubMed] [Google Scholar]
- Office of Population Census & Surveys. Standard Occupational Classification. Her Majesty’s Stationary Office; London: 1991. [Google Scholar]
- Parade SH, Blankson AN, Leerkes EM, Crockenberg SC, Faldowski R. Close relationships predict curvilinear trajectories of maternal depressive symptoms over the transition to parenthood. Family Relations. 2014;63:206–218. [Google Scholar]
- Pedersen C, Leserman J, Garcia N, Stansbury M, Meltzer-Brody S, Johnson J. Late pregnancy thyroid-binding globulin predicts perinatal depression. Psychoneuroendocrinology. 2016;65:84–93. doi: 10.1016/j.psyneuen.2015.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postpartum Depression: Action towards Causes and Treatment (PACT) Consortium. Heterogeneity of postpartum depression: a latent class analysis. The Lancet Psychiatry. 2015;2:59–67. doi: 10.1016/S2215-0366(14)00055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Putnam KT, Wilcox M, Robertson-Blackmore E, Sharkey K, Bergink V, Munk-Olsen T, Deligiannidis KM, Payne J, Altemus M, Newport J, Apter G, Devouche E, Viktorin A, Magnusson P, Penninx B, Buist A, Bilszta J, O’Hara M, Stuart S, Brock R, Roza S, Tiemeier H, Guille C, Epperson CN, Kim D, Schmidt P, Martinez P, Di Florio A, Wisner KL, Stowe Z, Jones I, Sullivan PF, Rubinow D, Wildenhaus K, Meltzer-Brody S. Clinical phenotypes of perinatal depression and time of symptom onset: analysis of data from an international consortium. The Lancet Psychiatry. 2017;4:477–485. doi: 10.1016/S2215-0366(17)30136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. General Hospital Psychiatry. 2004;26:289–295. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Rubertsson C, Waldenström U, Wickberg B. Depressive mood in early pregnancy: prevalence and women at risk in a national Swedish sample. Journal of Reproductive and Infant Psychology. 2003;21:113–123. [Google Scholar]
- Santos H, Jr, Tan X, Salomon R. Heterogeneity in perinatal depression: how far have we come? A systematic review. Archives of Women’s Mental Health. 2017;20:11–23. doi: 10.1007/s00737-016-0691-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiller CE, Meltzer-Brody S, Rubinow DR. The role of reproductive hormones in postpartum depression. CNS Spectrums. 2015;20:48–59. doi: 10.1017/S1092852914000480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I. Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. Journal of Midwifery & Women’s Health. 2013;58:57–68. doi: 10.1111/j.1542-2011.2012.00237.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone SL, Diop H, Declercq E, Cabral HJ, Fox MP, Wise LA. Stressful events during pregnancy and postpartum depressive symptoms. Journal of Women’s Health. 2015;24:384–393. doi: 10.1089/jwh.2014.4857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisner KL, Chambers C, Sit DY. Postpartum depression: a major public health problem. JAMA. 2006;296:2616–2618. doi: 10.1001/jama.296.21.2616. [DOI] [PubMed] [Google Scholar]
- Woolhouse H, Gartland D, Mensah F, Brown SJ. Maternal depression from early pregnancy to 4 years postpartum in a prospective pregnancy cohort study: implications for primary health care. BJOG. 2015;122:312–321. doi: 10.1111/1471-0528.12837. [DOI] [PubMed] [Google Scholar]
- Wright N, Hill J, Pickles A, Sharp H. The specific role of relationship life events in the onset of depression during pregnancy and the postpartum. PLoS ONE. 2015;10:e0144131. doi: 10.1371/journal.pone.0144131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie RH, He G, Koszycki D, Walker M, Wen SW. Prenatal social support, postnatal social support, and postpartum depression. Annals of Epidemiology. 2009;19:637–643. doi: 10.1016/j.annepidem.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Yaron Y, Lehavi O, Orr-Urtreger A, Gull I, Lessing JB, Amit A, Ben-Yosef D. Maternal serum HCG is higher in the presence of a female fetus as early as week 3 post-fertilization. Human Reproduction. 2002;17:485–489. doi: 10.1093/humrep/17.2.485. [DOI] [PubMed] [Google Scholar]
- Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, Belanger K. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014;71:897–904. doi: 10.1001/jamapsychiatry.2014.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yonkers KA, Wisner KL, Stewart DE, Oberlander TF, Dell DL, Stotland N, Ramin S, Chaudron L, Lockwood C. The management of depression during pregnancy: a report from the American Psychiatric Association and the American College of Obstetricians and Gynecologists. Obstetrics & Gynecology. 2009;114:703–713. doi: 10.1097/AOG.0b013e3181ba0632. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.