Summary
Medical cannabis patients, including two-thirds with chronic-pain, report health benefits including improved pain management and sleep. Pharmacoeconomic factors were the greatest limitation of medical cannabis.
Introduction
Medical cannabis (MC) is conditionally condoned in many countries including Bangladesh, Canada, Columbia, Finland, Germany, Italy, North Korea, Poland, Portugal, Spain, Sweden, the United Kingdom, Uruguay and in much of the United States. Although there have been a wide variety of indications in the past few decades for which MC has been purported to be both efficacious and safe (e.g. glaucoma), the most common use of MC today is for chronic pain.4, 34 There is a developing basic science evidence base linking the cannabinoid neurotransmitter system to nociception.14 The cannabinoid (CB1) receptors are localized in several structures important for pain like the periaqueductal gray, spinal trigeminal nucleus, amygdala, and basal ganglia.15, 39 Endogenous retrograde signaling molecules anandamide and 2-arachidonlyglycerol, or exogenous tetrahydocannabinol (THC), bind presynaptic CB1 receptors and inhibit neurons that are engaged by pain. The CB2 receptors, localized outside of the central nervous system, have also been implicated in pain management.17, 31 Importantly, other cannabinoids besides THC also contribute to the nociceptive properties of MC.15
Chronic pain is a complex construct which has cellular, anatomical, and psychological substrates and has been proposed to be viewed within a biopsychosocial lens. Pain, and especially chronic pain, exists within a context of biological and psychological variables such as genetics, gender, sleep, stress, and others.9 Despite extensive research and efforts at treating chronic pain, the efficacy of most pharmacologic and interventional modalities is incomplete. Increasingly, it is recognized that there is heterogeneity and overlap in chronic pain conditions. Pain management strategies are often limited by variable efficacy, side effects, toxicity and safety concerns, addiction, and expense. As such, the search continues for effective, safe, and ideally affordable treatments for chronic pain.
MC, like all drugs, exists within a socio-cultural environment that incorporates historical, legal, and extra-nociceptive elements which influences the perceptions of both patients and healthcare providers. Surveys have consistently identified efficacy in symptom management24, 36, 37, 41 and improved quality of life4 with MC. The majority of Australians indicated that cannabis provided “great relief” (55%) or “good relief” (45%) from pain.30 Three-quarters of UK dispensary members reported that MC was more effective than their prescribed medications.37 Unfortunately, interviews completed with a small (N = 23) number of Canadian dispensary patients determined that the quasi-legal status of this agent resulted in stigmatization from family members and others.5 Similarly, interviews of MC patients in California revealed that the negative connotations associated with marijuana caused them to delay raising this topic with healthcare providers.25 The objective of this report was to expand upon this foundation and examine both the strengths and limitations of MC in the northeastern United States.
Methods
Participants
Study participants (N = 984) were legal members of MC dispensaries in the north-eastern U.S. including Maine (57.9%), Vermont (30.6%), and Rhode-Island (11.5%). The Maine dispensary staff complete an educational intake session with each new patient. The intake time averages 45 minutes, but may be longer depending upon a patient’s educational needs. Educational topics covered include different methods of cannabis ingestion, proper/appropriate dosage of cannabis for the patient, and what patients can expect in terms of this form of treatment addressing their specific symptom relief. The intake also includes education of the patient on state laws regarding the use of medical cannabis and the use of dispensary services to acquire MC. Other dispensaries follow a similar procedure.
Procedures
Participants completed a 77-item online survey (Supplementary Appendix) which was hosted on Survey Monkey and included forced-choice demographics and medical history items and open-ended questions (What do you like most/least about medical cannabis?). A total N of 1,513 completed the informed consent. Half (47.4%) of potential respondents in Maine that received and opened the invitation email completed the survey and two-fifths (40.8%) of Vermont members with an active email address participated. Items were constructed after pilot studies were completed and items were found to be interpretable by the general public. Although the only required item was the informed consent, this report primarily focuses on the 61.7% of participants that completed the open-ended (most/least) items. As each state has somewhat different medical cannabis laws, slightly different versions of the survey were constructed for each state. At the time of data-collection (8/2015 – 4/2016), chronic pain was not a condition to become part of the Vermont registry but was subsequently added. Respondents further classified their pain as abdominal, back/neck, cancer, chronic pain following surgery, neuropathic, or trauma/injury. The intended sample size (1,000) was selected to provide a sufficient representation of different pain types. This investigation was conducted and communicated according to the Standards for Reporting Qualitative Research.19 All procedures were approved by the IRBs of Bowdoin College and Maine Medical Center.
Data-analysis
The MC patient survey (Supplementary Appendix or https://www.dropbox.com/s/xy36d8prhl1oz7m/Appendix_1_2.pdf?dl=0) included quantitative and qualitative items. Quantitative analysis was completed with Systat (San Jose, California), version 13.1. Variability was expressed as the SEM. If a range of values was reported in response to the item “How much money do you spend on medical cannabis each week?” (e.g. 20–40), the midpoint was entered. The weekly amount was multiplied by 52.14 to estimate the yearly value. Qualitative analyses were conducted from a Grounded Theory perspective.10 A psychologist who was not a cannabinoid expert identified themes and subthemes, first using the results with one dispensary (N = 150) and then with full-dataset. Sorted data were then uploaded to QSR International (Melbourne, Australia) NVivo 9 which quantified the number of responses. Ten percent of responses were re-examined by another co-author for theme/subtheme verification. Descriptive statistics were completed on the word count (“most” responses total words = 18,462, “least” responses total words = 14,269). Example responses are provided verbatim. Figures were prepared with Graphpad Prism version 7.01.
Results
Participant characteristics
Slightly over half of participants were female, predominately white (1.5% Native American, 1.2% black, 1.2% Hispanic), and, on average, middle-aged and over-weight (2.2% underweight, 33.1% overweight, 23.9% obese, and 6.0% morbidly obese). Additional demographic information may be found in Table 1.
Table 1.
Demographic characteristics of participants (N = 984).
| % female | 52.9 |
| Age (± SEM) | 49.1 (0.5) |
| Ethnicity (% non-white) | 5.8% |
| Education | |
| Less than high-school | 2.7% |
| High-School | 17.2% |
| Associates or Vocational degree | 37.9% |
| Bachelor’s degree | 25.9% |
| Graduate or professional degree | 16.3% |
| Employment | |
| Full-time | 33.2% |
| Disability | 27.9% |
| Retired | 14.7% |
| Student | 1.6% |
| Body Mass Index (± SEM) | 27.9 ± 0.2 |
Two-thirds (64.0%) reported that they had been diagnosed by a medical professional with chronic pain. Among this group, the vast majority (91.0%) reported back/neck pain, 30.3% neuropathic pain, 23.3% post-surgical pain, 21.7% with abdominal pain, 20.2% with chronic-pain following trauma or an injury, 6.7% with cancer pain, and 5.1% with menstrual pain. Other conditions reported by participants with a pain component included arthritis (39.5%), migraines/chronic headaches (18.8%), fibromyalgia (16.1%), %), Irritable Bowel Syndrome (12.1%), cancer (10.0%), and diabetes (6.7%). Psychiatric disorders were also commonly reported including Generalized or Social Anxiety Disorder(34.9%), Major Depressive Disorder (31.1%), Post-Traumatic Stress Disorder (25.0%), insomnia or another sleep disorder (22.4%), bipolar (6.5%), or Obsessive Compulsive Disorder (4.3%). Other health conditions and diseases reported by participants were hypertension (18.9%), asthma (10.6%), and Chronic Obstructive Pulmonary Disorder (4.0%).
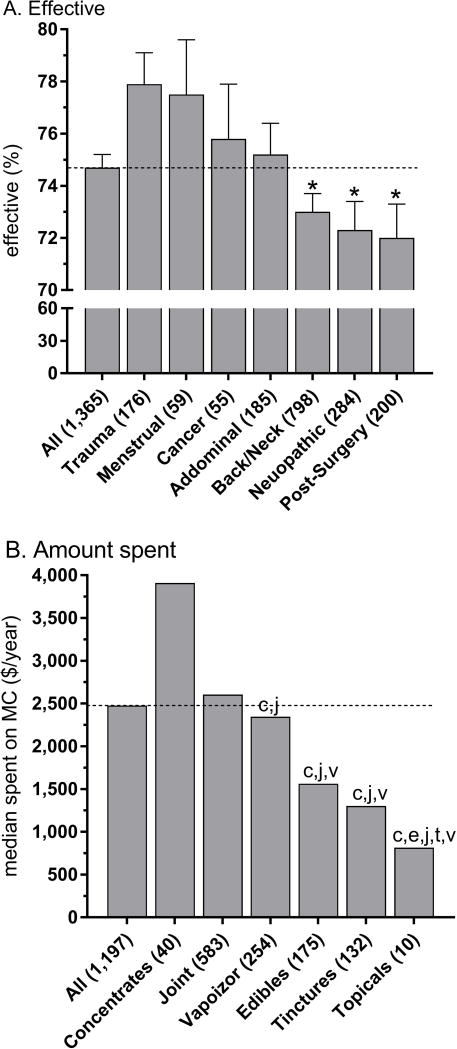
The preferred route of administration of MC for almost half (46.2%) of respondents was joint, pipe, or bong; vaporizer for one-quarter (23.4%), edibles (13.8%) or tincture (12.0%) for one-eighth, while concentrates (3.9%) or topicals (0.7%) were least common. In response to “How effective is medical cannabis in treating your symptoms or conditions?” the average was 74.7% (SEM = 0.6, Min = 0% “no relief”, Max = 100 “complete relief”, 10th percentile = 50%, 90th percentile = 100%). Figure 1A shows that the rating was above a 7 for all pain types but the relief was greater for trauma and injury than post-surgical pain (t(374) = 3.36, p < .001), neuropathic pain (t(458) = 3.35, p < .001), and back or neck pain (t(972) = 3.26, p ≤ .001). The relief for menstrual pain was larger than post-surgical (t(254) = 2.10, p < .05) and neuropathic pain (t(338) = 2.00, p < .05). The average amount spent on MC each year was $3,118.24 (SEM = 95.24, Min = 52.14, Max = 52,140.00, Skewness = 4.8, 5th Percentile = 391.05, Median = 2,476.65, 95th percentile = 7,821.00). Due to the positively skewed distribution, Figure 1B reports the median and shows that the preferred formulation substantially impacted the yearly expenditure with concentrates ($3,910.50) being over four-fold the cost of topicals ($814.69). MC administered with joints was significantly more expensive than via vaporizer (difference of $260.70), edibles ($1,402.80), or tinctures ($1,303.50).
Figure 1.
Mean (±SEM) response to “How effective is medical cannabis in treating your symptoms or conditions?” on a 0 to 100% scale, by pain type. * p < .001 versus trauma or injury (A). Median amount spent on medical cannabis each year by formulation type. cp < .0005 versus concentrates, ep ≤ .0005 versus edibles, jp < .0005 versus joint, tp < 005 versus tinctures, vp ≤ .001 versus vaporizer. Horizontal dashed lines depict the central tendency and numbers in parentheses depict the number of observations (B).
Positive Themes
There were 2,592 responses (total words = 18,462, mean words/response = 7.1) to “What do you like most about medical cannabis?”. Figure 2A shows the ten themes which were identified. Over one third (36.0%) of responses were about medical benefits. The largest sub-theme of health benefits was pain relief. Many respondents were highly favorable (“It stops the pain,” “Changes perception and experience of my chronic pain,” “It will break the cycle of chronic pain”, “It’s been life changing for my pain.”). Some pain responses were more qualified (“While it doesn’t take away the pain completely, it seems to numb some of it,” “I can tolerate the chronic pain a little better,” “I feel no pain…anyone who hasn’t had chronic pain would not even understand how good it feels to even have it gone for a few hours.”). The next most common sub-theme of health benefits was sleep including sleep onset (“It helps me to fall asleep”), sleep maintenance (“It helps me sleep ALL night long,” “Help with my insomnia”) and reduced nightmares (“This is the first time since I was 8 years old that I have been nightmare free”).
Figure 2.
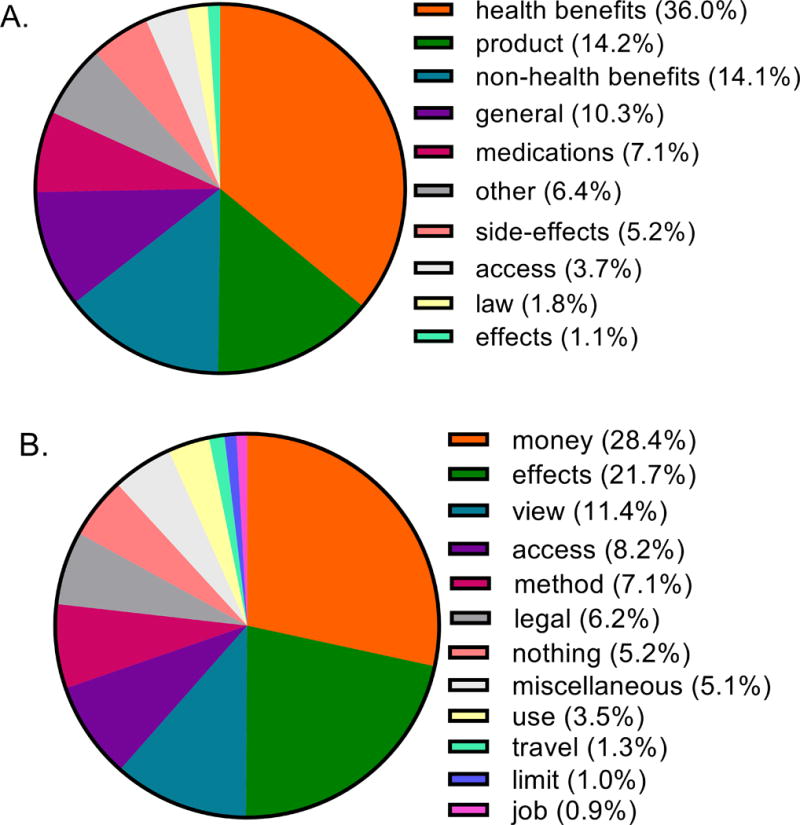
Themes and percentage of total for “What do you like most about medical cannabis?” (A, N = 2,592) and “What do you like least about medical cannabis (B, N = 1,678) from New England dispensary members.
The second theme was characteristics of MC. There were responses about over-dose potential (“you can’t OD,” “It will not kill me,” “That it is safe”), natural (“All natural”, “It’s organic,” “Not a synthetic”), and strains (“The availability of strains,” “Knowing exactly what strain you are getting and THC/CBD content”). A sub-theme that emerged was the limited addictive potential (“It is not an addictive substance,” or “It is non habit forming”).
Non-health benefits were identified in one-seventh (14.1%) of responses. This included a general improvement in the quality of life (“It lets me enjoy life more fully,” “I get to feel normal,” “lets me live a more productive life and a more fulfilling one”) and functionality (“It gives me the ability to function throughout the day,” “I am more active and able to do things I want”). Cognitive aspects (“Distracts me from the pain and dwelling on negative thoughts,” “Promotes focus,” and “I can think more clearly”) were noted. A sub-theme was relaxation (“The degree of relaxation that I get from it,” “It helps me relax,” and “The calm relaxed feeling that I get shortly after”).
One-tenth (10.3%) of responses fell into a general theme mentioning efficacy (“the efficacy is amazing,” “It works!,” “It works on so many levels”) or their general response (“I get relief when nothing else has worked,” “I had no idea that it could help me so much.” “This is the best that I have felt in years”).
Non-cannabis medications was the next most common (7.1%) theme. This was divided into a decrease in prescription medications (“Not needing prescription pain pills,“ “Not having to use prescription meds,” “the medical marijuana has all but eliminated the need to take them (oxycodone and hydrocodone) totally”), and effectiveness of cannabis compared to prescription medications (“That it works better than any pharmaceutical I’ve used,” “The benefits far outweighs ANY of the pain medications I have been prescribed!,” “It is truly amazing that finding the right strain, and the right mode of delivery (vaporizer) can help lessen pain better that prescription drugs”), and relative safety (“medical cannabis, even if smoked, is a safer alternative to so many prescription drugs,” “replaces dangerous pharmacy drugs”) subthemes. Painkillers were another subtheme (“Decreased pain meds by 80%,” “I like that I am almost off all painkillers,” “Pain is treated with out (sic) have to use pharmaceuticals”).
Over one out of every twenty (5.2%) responses was about side-effects, either specific to cannabis (“The lack of side effects!,“ “With therapeutic cannabis the side effects are nominal,” “It has the least amount of side effects of all the treatments I have used”) or relative to other medications (“I don’t have terrible stomach pain from anti-inflammatory drugs,” “It makes it easier for me to tolerate the side effects of my medications”). Supplemental Table 1 provides additional information on positive themes and subthemes.
Negative Themes
There were 1,678 responses (total words = 14,269, words/response = 8.5) to “What do you like least about medical cannabis?”. Figure 2B shows the themes that emerged. Over one-quarter (28.4%) of responses were to economic considerations including cost (“It costs too much,” “The cost is ridiculous,” “The cost is expensive for someone on a fixed income and limits accessibility”) and price (“I wish the price at dispensaries was lower,” “Over priced,” “Price is way too high”).
The second theme was to effects (21.7%) including olfactory (“The smell. If you have, and you know because you smell it, everyone else can too,” “Pungent odor,” “Don’t like the smell,”) respiratory (“The effects on my lungs,” “A lot of coughing,” “What it does to my lungs,” “Heavy chest”), and appetite (“Makes me graze,” “The munchies and weight gain,” “Increase in appetite”), cognitive (“Decrease ability to concentrate,” “Brain fog,” “Marijuana “hangover”: a foggy, non-alert feeling in the morning”), or emotional (“Occasional paranoia,” “Sometimes anxious”).
The third theme was view of others toward cannabis (11.4%) with stigma being frequently mentioned directly (“The stigma associated with it,” “The negative stigma around the misinformation in society about the drug,” “the ignorant stigma associated with it”) or indirectly (“Feeling like it is frowned upon by the general society,” “Negative connotation associated with use,” “The negative attitude many people have,”), specifically related to employers (“The secrecy from my employer”) or healthcare providers (“That I couldn’t tell my PCP (primary care provider) about using it due to his intolerant attitude toward it,” “not supported by family or many medical doctor (sic),” “The stigma still attached especially by healthcare workers”).
Access, or the lack of access to cannabis, was the next most common theme (8.2%) including physical access (“The locations, so far away,” “My commute to acquire my medicine,” “there are not many medical dispensaries near me so I have to travel far to get it”), and dispensary characteristics (“Dispensary hours,” “It can be hard to get appointments at the dispensary.”). Access to strains (“strains that work well are not always available.”, “I wish more strains were available”, “All kinds of strains out there, but you have to take what is currently available in your area”) was identified primarily by patients in Vermont.
The method or route of administration was identified in 7.1% of responses. Patients made references to smoking (“Smoking is isn’t not always convenient”, “Smoking it. It’s gross.”, “The taste when smoking.”), vaporizers (“It’s a bit cumbersome to use the vaporizer (which works best”, “The vaporizers just burn it up or too expensive.”, “Coughing when using vaporizer”, tincture (“Tincture takes too long for effect.”, “I wish there was a clearer dosing and strain labeling for tincture”), or edibles (“Can’t get a handle on edible dosing”, “hard to gage (sic) correct dosage with edibles”, or “The lack of edible product that is available”).
Legal considerations were noted in 6.2% of responses. This includes the difference between federal and state laws (“That while I'm following state laws, I'm breaking federal laws.”, “Schedule 1 conflict between state and federal enforcement“), and practical implications of the law (“crossing boarders into non-medical states”, “inconvenience of dosing in secret.”, and “I am made to feel like a criminal”). Additional negative themes and subthemes may be found in Supplemental Table 2.
Discussion
This well-powered investigation characterizes the many strengths, and also limitations, of MC in New England from a dispensary member’s perspective. The sample consisted primarily of patients with chronic pain from a wide variety of often overlapping sources including back-pain, arthritis, neuropathic pain, post-surgical pain, abdominal pain, and headaches.
The largest positive theme identified related to health benefits. Respondents described in great depth how medical cannabis improved their treatment of chronic-pain and enhanced their quality of life. These results are consistent with prior quantitative examinations of MC among patients from the United Kingdom,37 Canada,36 and Australia,30 as well as more regionally focused efforts in the US (e.g. San Francisco,24 Michigan,4 and Rhode Island41). Importantly, these findings were collected during a period in which opioid prescriptions were extremely common22 but clinical guidelines have stressed that nonopioids and nonpharmacological interventions are preferred over opioids for chronic pain.11 Although the overall benefits in symptom management were moderately high based on a quantitative measure (Figure 1A), most prominently for pain following trauma, there were some individual differences in pain relief as reported by open-ended reports. Additional research is needed to identify why some patients had temporary or incomplete pain relief. In addition to pain, the next most frequent health benefit was to improve sleep. Sleep impairments such as problems falling asleep and sleep maintenance are commonly experienced by patients with chronic pain.28 However, sleep disruption (including nightmares) is also an important component of Post-Traumatic Stress Disorder (PTSD)2 symptomology and one-quarter of this sample had been diagnosed with PTSD.
The second positive theme involved characteristics of MC. Respondents emphasized the very modest overdose potential with MC.12 Participants also believed that MC is not addictive. This population also had substantial experience with opioids so many of their MC comments were relative to these agents. Maine and Vermont, like many states, were in a high-profile opioid epidemic21, 33 where there was a high level of concern about escalation from prescription opioids to heroin and opioid fatalities.29 Another positive theme identified was to other medications. A decrease in other prescription and non-prescription medications following initiation of MC is a very robust phenomenon which has been identified with diverse methodologies.3, 4, 6 This is also the topic of a separate report which also showed reduction in opioids.21
The primary negative theme identified by MC patients was cost. The typical amount spent on MC was over two-thousand dollars per year although this varied depending on the formulation and the preferred route of administration. As MC, unlike other treatments for pain, is not covered by insurance; perhaps this fiscal finding is unsurprising. The median household income is $46,974 in Maine, $52,278 in Vermont, and $55,902 in Rhode Island23 and two-thirds of participants were not employed full-time which further exacerbates the economic burden experienced by some MC patients. The average dispensary purchase in Maine ($101) was 44.3% larger than in California ($70)20 possibly due to the more rural character of Maine. Americans spent $5.4 billion on legal and recreational marijuana in 201518 and some dissatisfaction with the cost of MC has been noted by others.15 Nabiximol, a mixture of tetrahydrocannabinol and cannabidiol, is currently reimbursed by some Israeli health maintenance organizations.1 We suspect that the participants in this study would be extremely enthusiastic about similar policies in the United States although these policies currently face some legal barriers.38 On the other hand, repeated exposure to THC may downregulate and desensitize cannabinoid receptors.7 The diagnostic criteria for Cannabis Use Disorder include taking larger amounts over a longer period than was intended and tolerance, a marked increase in cannabis use to achieve the desired effect.2 Spending thousands, or tens of thousands of dollars each year on MC may be indicative that a subset of users are misusing MC.
The second most common negative theme regarded the negative effects of MC. This includes olfactory and respiratory consequences of smoking. While smoking may provide rapid symptom relief, oral administration would provide more sustained pain management, albeit with a more delayed onset. We suspect that economic considerations, resulting from first pass metabolism and less active substances reaching their receptors, are the primary reason that edibles were the preferred delivery modality by less than one-seventh of participants. As an elevated Body Mass Index (BMI) may be a risk-factor for lower-back pain,16 the well-known appetite stimulating effects of cannabinoids12 was a dispensary member concern. However, it is also noteworthy that the percent of participants with a BMI ≥ 25 (63%) is similar to that identified in the National Health Nutrition Examination Survey (64%).8 Further monitoring of food intake and body weight, particularly among dispensary members with diabetes,27 and whether orexigenic tolerance occurs with MC should be the topic of further longitudinal investigations.
The third negative characteristic surrounding MC concerns the views of others including their health care providers. Perceived bias against MC and being viewed as a “pothead” or “stoner” has also been identified in studies of individuals in California.25 Potential stigma may contribute to patients obtaining their certification for MC from healthcare providers with whom they do not have a long-term relationship. Effective healthcare delivery depends upon effective communication between patients and providers. This may be an important finding that healthcare providers should be aware of in order to facilitate improved communication with patients who may not feel comfortable disclosing their use of MC. This could be especially important in high risk patient populations with contra-indications to MC (e.g. adolescents and young-adults, pregnant women, people with a family history of schizophrenia, patients with lung diseases such as asthma and COPD) where providers with an established patient relationship would be most appropriate to convey key information about the appropriateness of MC.
There are clearly some limitations to this study. First, the sample, although appreciably larger than other similar surveys,4, 5, 34 is limited to dispensary members in New England. There are substantial variations in how each state implements medical cannabis (e.g. in the qualifying conditions or in the involvement of medical professionals) and also in demographics. California has the longest history in the U.S. with MC (since 1996), and the minority population in California (59.9%) is over ten-fold greater than that of Maine (5.6%) or Vermont (5.7%).35 Ethnicity is an important characteristic because Hispanics are at greater risk of cannabis dependence than whites40 and MC dispensaries are more likely to be located in areas with more minorities26, particularly Hispanics.32 Further, California has 815 active dispensaries (1 dispensary / 520 km2) which is twenty-fold more accessible than Maine’s eight (1 dispensary / 11,546 km2). Additional qualitative investigations with much more ethnically diverse and urban samples are needed. These findings may not generalize to other states with less restrictive medical, or recreational, cannabis laws. Although there has been limited research about MC in Maine and Vermont, these findings may not generalize to other states or to groups that procure or distribute their marijuana through other means. Second, the open-ended items were located at the end of a 77-item survey and the earlier items, although wide-ranging, may have encouraged participants to think about some specific issues over others or created demand characteristics. However, given the depth of negative responses (e.g. surrounding price), we believe respondents were wholly engaged and fully disclosing their perspective. Finally, these findings were based on patients’ self-report. For example, medical diagnoses were self-reported, and further research with electronic medical records or from prescription drug monitoring programs could corroborate or refute some findings. The patient’s perspective may occasionally reflect inaccurate beliefs held by the general public (e.g. equating “natural” with “safe”) and some findings may form the foundation for further patient education. Although these data are self-reported and mostly qualitative, they do provide insights into the perceived benefits and disadvantages of MC from the patient’s point of view. Increasingly, patient centric metrics are used as outcomes and linked to reimbursement through such measures as Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS). The Centers for Medicare and Medicaid Services also uses ratings from HCAHPS to determine a hospital’s performance in several domains and ties these ratings to payment.
Overall, this report identified many beliefs about the efficacy, and cost, of MC among patients. Independent of an individual providers, or their institutions, views about MC or its evidence base, an awareness of patients’ perspectives about these topics could enhance an open-discussion about MC and its role as part of a multimodal approach to chronic pain. Although this study is limited in some ways, it does provide a window into the chronic pain patient’s favorable and unfavorable experiences with MC. It is increasingly apparent that the patient’s perspective is important.
Supplementary Material
Acknowledgments
BJP has received research support from and is on the Advisory Board of the Center for Wellness Leadership, a non-profit organization, to complete this study, travel from the Wellness Connection of Maine, and research supplies and travel from the National Institute of Drug Abuse. RMD was employed by the Wellness Connection of Maine, a medical cannabis dispensary. Data-analysis was conducted using software provided by the NIEHS (T32-ES007060-31A1). David The berge provided technical assistance. A special thanks to the participants of this study for sharing their experiences.
Footnotes
Disclosures: All other authors have no relevant disclosures.
Prior Presentation: Earlier versions of this dataset were presented at the American Psychological Association and Maine Society for Neuroscience annual meetings.
References
- 1.Ablin J, Ste-Marie PA, Schafer M, Hauser W, Fizcharles MA. Medical use of cannabis products: Lessons to be learned from Israel and Canada. Schmerz. 2016;30:3–13. doi: 10.1007/s00482-015-0083-4. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. DSM-5. Arlington; VA: [Google Scholar]
- 3.Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999–2010. JAMA Internal Medicine. 2014;174:1668–1673. doi: 10.1001/jamainternmed.2014.4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boehnke LF, Litinas E, Clauw DJ. Medical cannabis use is associated with decreased opiate medication use in a retrospective cross-sectional survey of patients with chronic pain. Journal of Pain. 2016;17:739–744. doi: 10.1016/j.jpain.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Bottoroff JL, Bissell LJL, Balneaves LG, Oliffe JL, Capler NR, Buxton J. Perceptions of cannabis as a stigmatized medicine: A qualitative descriptive study. Harm Reduction Journal. 2013;10:2. doi: 10.1186/1477-7517-10-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bradford AC, Bradford WD. Medical marijuana laws reduce prescription medication use in Medicare Part D. Health Affairs. 2016;35:1230–1236. doi: 10.1377/hlthaff.2015.1661. [DOI] [PubMed] [Google Scholar]
- 7.Breivogel CS, Childers SR, Deadwyler SA, Hampson RE, Vogt LJ, Sim-Selley LJ. Chronic Δ-tetrahydrocannabinol treatment produces a time-dependent loss of cannabinoid receptors and cannabinoid receptor-activated G proteins in rat brain. J Neurochemistry. 1999;73:2447–2459. doi: 10.1046/j.1471-4159.1999.0732447.x. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control. [accessed 11/9/2016];Healthy weight, overweight, and obesity among U.S. adults. Available at: https://www.cdc.gov/nchs/data/databriefs/adultweight.pdf.
- 9.Clark JD. Preclinical pain research: Can we do better? Anesthesia. 2016:846–849. doi: 10.1097/ALN.0000000000001340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corbin J, Strauss A. Sage. 4. Thousand Oaks; California: Basics of qualitative research: Techniques and procedures for developing Grounded Theory. [Google Scholar]
- 11.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMMW. 2016;65:1–50. doi: 10.15585/mmwr.rr6501e1. [DOI] [PubMed] [Google Scholar]
- 12.Earleywine M. Understanding marijuana: A new look at the scientific evidence. Oxford: 2002. [Google Scholar]
- 13.Eschker E. Active medical marijuana dispensaries in California, 2015. Humboldt Institute for Interdisciplinary Marijuana Research; [Accessed 12/13/16]. at: http://www2.humboldt.edu/hiimr/docs/california%20dispensaries.pdf. [Google Scholar]
- 14.Jensen B, Chen J, Furnish T, Wallace M. Medical marijuana and chronic pain: A review of basic science and clinical evidence. Current Pain & Headache Reports. 2015;19:50. doi: 10.1007/s11916-015-0524-x. [DOI] [PubMed] [Google Scholar]
- 15.Ko GD, Bober SL, Mindra S, Moreau JM. Medical cannabis – The Canadian perspective. Journal of Pain Research. 2016;9:735–744. doi: 10.2147/JPR.S98182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leboeuf-Yde C. Body weight and low back pain. A systematic literature review of 56 journal articles reporting on 65 epidemiologic studies. Spine. 2000:226–237. doi: 10.1097/00007632-200001150-00015. [DOI] [PubMed] [Google Scholar]
- 17.Morales P, Hernandez-Folgado L, Goya P, Jagerovic N. Cannabinoid receptor (CB2) agonists and antagonists: A patent update. Expert Opinion on Therapeutic Patents. 2016;26:843–856. doi: 10.1080/13543776.2016.1193157. [DOI] [PubMed] [Google Scholar]
- 18.Morris C. [accessed 11/9/16];The next big billion-dollar cannabis markets investors are rushing to. Available at: www.cnbc.com/2016/10/21/the-next-big-billion-dollar-cannabis-markets-investors-are-rushing-to.html.
- 19.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine. 2014;89:1245–1251. doi: 10.1097/ACM.0000000000000388. [DOI] [PubMed] [Google Scholar]
- 20.Olson B. [accessed 12/13/16];Chart of the week: Average purchase amount at dispensaries ranges from $60 to $100+ 2015 Available at: https://mjbizdaily.com/chart-week-average-marijuana-dispensary-purchase-amounts-range-60-100/
- 21.Piper BJ, DeKeuster R, Beals ML, Cobb C, Burchman CA, Perkinson L, Lynn ST, Nichols SD, Abess AT. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. Journal of Psychopharmacology. doi: 10.1177/0269881117699616. in review. [DOI] [PubMed] [Google Scholar]
- 22.Piper BJ, Desrosiers CE, Lipovsky JW, Rodney MA, Baker RP, McCall KL, Nichols SD, Martin SL. Use and misuse of opioids in Maine: Results from pharmacists, the Prescription Monitoring, and the Diversion Alert programs. Journal of Studies on Alcohol and Drugs. 2016;77:556–565. doi: 10.15288/jsad.2016.77.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reeves P. This is what it takes to be middle class in Maine. [Accessed 10/30/2016];Bangor Daily News, 4/6/15. at: http://bangordailynews.com/2015/04/06/the-point/what-you-need-to-earn-to-be-middle-class-in-maine-in-one-handy-chart/email/
- 24.Reiman A. Cannabis as a substitute for alcohol and other drugs. Harm Reduction Journal. 2009;6:35. doi: 10.1186/1477-7517-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Satterlund TD, Lee JP, Moore RS. Stigma among California’s medical marijuana patients. Journal of Psychoactive Drugs. 2015;47:10–17. doi: 10.1080/02791072.2014.991858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shi Y, Meseck K, Jankowska MM. Availability of medical and recreational marijuana stores and neighborhood characteristics in Colorado. Journal of Addiction. 2016:7193740. doi: 10.1155/2016/7193740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sidney S. Marijuana use and Type 2 diabetes: a review. Current Diabetes Reports. 2016;16:117. doi: 10.1007/s11892-016-0795-6. [DOI] [PubMed] [Google Scholar]
- 28.Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature. Sleep Medicine Reviews. 2004;8(2):119–132. doi: 10.1016/S1087-0792(03)00044-3. [DOI] [PubMed] [Google Scholar]
- 29.Sorg MH, Greenwald M, Wren JA. Patterns of drug related mortality in Maine, 2015 update. Maine Policy Review. 2016;25:34–46. [Google Scholar]
- 30.Swift W, Gates P, Dillon P. Survey of Australians using cannabis for medical purposes. Harm Reduction Journal. 2005;2:18–27. doi: 10.1186/1477-7517-2-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Temple LM. Medical marijuana and pain management. Disease-a-Month. 2016;62:346–352. doi: 10.1016/j.disamonth.2016.05.014. [DOI] [PubMed] [Google Scholar]
- 32.Thomas C, Freisthler B. Examining the locations of medical marijuana dispensaries in Los Angeles. Drug and Alcohol Review. 2016;35:334–337. doi: 10.1111/dar.12325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Toth AR, Possidente CJ, Sawyer LM, DiParlo MA, Fanciullo GJ. National and northern New England opioid prescribing patterns, 2013–2014. Pain Medicine. doi: 10.1093/pm/pnw231. in press. [DOI] [PubMed] [Google Scholar]
- 34.Troutt WD, DiDonato MD. Medical cannabis in Arizona: Patient characteristics, perceptions, and impressions of medical cannabis legislation. Journal of Psychoactive Drugs. 2015;47:259–266. doi: 10.1080/02791072.2015.1074766. [DOI] [PubMed] [Google Scholar]
- 35.US Census Bureau. [Accessed 12/13/16];Overview of Race and Hispanic Origin: 2010 Census Briefs. at: http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf.
- 36.Walsh Z, Callaway R, Belle-Isle L, Capler R, Kay R, Luca P, Holtzman S. Cannabis for therapeutic purposes: Patient characteristics, access, and reasons for use. International Journal of Drug Policy. 2013;24:511–516. doi: 10.1016/j.drugpo.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 37.Ware M, Adams H, Guy G. The medicinal use of cannabis in the UK: Results of a nationwide survey. International Journal of Clinical Practice. 2005;59:291–295. doi: 10.1111/j.1742-1241.2004.00271.x. [DOI] [PubMed] [Google Scholar]
- 38.Wehrwein P. Medical marijuana coverage still lost in the legal weeds. Managed Care. 2013;22:23–25. [PubMed] [Google Scholar]
- 39.Wilson-Poe AR, Morgan MM, Aicher SA, Hegarty DM. Distribution of CB1 cannabinoid receptors and their relationship with mu-opioid receptors in the rat periaqueductal gray. Neuroscience. 2012;213:191–200. doi: 10.1016/j.neuroscience.2012.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wu LT, Zhu H, Swartz MS. Trends in cannabis use disorders among racial/ethnic population groups in the United States. Drug and Alcohol Dependence. 2016;165:181–190. doi: 10.1016/j.drugalcdep.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zaller N, Toplelz A, Frater S, Yates G, Lally M. Profiles of medicinal cannabis patients attending compassion centers in Rhode Island. Journal of Psychoactive Drugs. 2015;47:18–23. doi: 10.1080/02791072.2014.999901. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.