Abstract
Purpose
The aim of the study was to evaluate the progression and rotation of the fetal head during the second stage of labor using translabial ultrasound and to compare ultrasonographic data obtained in nulliparous women both receiving and not receiving neuraxial analgesia.
Methods
The 49 patients enrolled in the study were divided into two groups according to receiving or not receiving neuraxial analgesia. Every half hour from full dilation to delivery, the ultrasonographic translabial parameters of Angle of Progression, Head Symphysis Distance, and Midline Angle were obtained and recorded by a single operator. Then, these records were compared between the two groups of patients.
Results
Patients that underwent neuraxial analgesia presented with increased duration of the second stage of labor, with mean values of Angle of Progression significantly higher and of Midline Angle significantly lower for each time interval studied compared to patients without analgesia. A borderline significant relationship was found between administration of neuraxial analgesia and Head Symphysis Distance.
Conclusions
In this study, we demonstrated that combined spinal–epidural analgesia influences the duration of the second stage of labor and the initial progression and rotation of the fetal head through the birth canal, but not the kind of delivery. A correlation between Angle of Progression values and success in the application of a vacuum has been reported by other authors and confirmed in our study.
Keywords: Second stage of labor, Operative delivery, Translabial ultrasound, Neuraxial analgesia, Nulliparous woman, Fetal head rotation
Sommario
Obiettivo
Lo scopo dello studio è stato quello di valutare longitudinalmente la progressione e la rotazione della testa fetale durante il secondo stadio del travaglio mediante ecografia translabiale e di confrontare i dati ecografici ottenuti in pazienti nullipare sottoposte o meno ad analgesia epidurale.
Materiali e metodi
Quarantanove nullipare incluse nello studio sono state suddivise in due gruppi in base alla somministrazione o meno di analgesia perimidollare. Per ogni paziente sono stati registrati da un singolo operatore, ogni mezz’ora dalla dilatazione completa al parto, i seguenti parametri ecografici translabiali: Angolo di Progressione, Distanza sinfisi materna-testa fetale e Angolo di Rotazione. I risultati ottenuti sono poi stati confrontati tra i due gruppi di pazienti.
Risultati
Le pazienti sottoposte ad analgesia perimidollare presentano durata aumentata del secondo stadio del travaglio, valori di Angolo di Progressione maggiori e di Angolo di Rotazione inferiori rispetto alle pazienti senza parto analgesia. Sul parametro Distanza sinfisi materna-testa fetale la valutazione statistica si è dimostrata ai limiti della significatività.
Conclusioni
Nello studio si dimostra che l’analgesia perimidollare aumenta la durata del secondo stadio del travaglio, influenza l’iniziale discesa e rotazione della testa fetale nel canale del parto ma non incide sulla tipologia di parto (spontaneo vs operativo vs taglio cesareo). Una correlazione tra valori di Angolo di Progressione e successo di parto operativo è stata riportata da altri autori e confermata dal nostro studio.
Introduction
Accuracy in the diagnosis of station and position of the fetal head through traditional obstetrics digital exploration is low because of interoperator variability and poor reproducibility. The use of ultrasound during labor was introduced by the Italian Society of Ultrasound in Gynecology and Obstetrics (SIEOG) [1] as a valid support to obstetric semeiotics because it allows obtaining objective and reproducible data about station, progression, and position of the fetal head [1].
The second stage of labor is the period between full dilatation of the cervix and birth. The duration of this period in nulliparous women should be less than 3 h in the case of administration of analgesia, and less than 2 h in cases without analgesia [2–4]. San Giovanni Calibita Fatebenefratelli Hospital’s study on labor analgesia contributed to the realization of a prospective clinical cohort study of 545 patients designed to evaluate the effects of epidural analgesia and combined spinal–epidural analgesia (CSEA) on the progression of labor, thus allowing analysis of variations to partogram induced by labor analgesia [5]. However, the exact evaluation of the hypothesized analgesia-induced extension of the second stage has not yet been objectively studied. In cases of prolonged labor, clinicians should identify the cause of the missed progression of the fetal head and the level of the fetal presenting part. This evaluation is paramount to decide if it is possible to have a spontaneous birth (SD) or if it is necessary to carry out an operative delivery (OD) or a cesarean section (CS). Progression Angle (AoP), Head Symphysis Distance (HSD), and Midline Angle (MLA) are translabial parameters for evaluating the progress of labor and can help clinicians to make the best clinical decisions in case of a dystocic labor. The aims of this study were to assess the longitudinal changes of various sonographic parameters of fetal head progression and station in relation to length of the second stage of labor and then to compare ultrasound findings obtained longitudinally among nulliparous women with and without combined spinal–epidural analgesia.
Subjects and methods
Transperineal ultrasound measures were prospectively acquired in the delivery room of the department of obstetrics and gynecology at the San Giovanni Calibita Fatebenefratelli Hospital in Rome. The eligible inclusion criteria were: nulliparity, spontaneous onset of pregnancy, absence of materno-fetal disease, singleton pregnancies at term (38–41 weeks), fetuses in cephalic presentation, spontaneous onset of labor, and no abnormal cardiotocographic traces nor premature rupture of membranes at time of admission to the hospital. Recruitment was carried out at time of admission to the delivery room by a single trained investigator. Sixty patients were recruited between September 2015 and May 2016 and enrolled in the study. Eleven were excluded due to the onset of pathologic cardiotocographic patterns or placental abruption (one case) requiring rapid processing of birth (by cesarean section), or because maternal alternative position during delivery (“all four” or “squatting” position) did not make it possible to record ultrasonographic measurements in this specific setting. Data from the remaining 49 women were used for the longitudinal analysis of sonographic parameters. These patients were divided into two groups depending on the administration (29 patients—Group 1) or not (20—Group 2) of combined spino–epidural analgesia. In our hospital, neuraxial analgesia is administered to patients who request it after performing a detailed anesthesiologic consultation at around 34 weeks’ gestation. Table 1 summarizes the protocol used by anesthesiologists in our delivery room for combined spinal–epidural analgesia in nulliparous women. Obstetric clinical examination was performed by a midwife and recorded step by step for each patient for head station, cervical dilatation, Bishop score, and time of evaluation. In our prospective study, ultrasonographic evaluation was blinded to the findings on clinical examination and was performed using a portable machine (Esaote My Lab) equipped with a transabdominal probe (3.5 MHz). The evaluation began at full cervical dilatation (T0) and then was repeated every 30 min (T1 = 30 min, T2 = 60 min, T3 = 90 min, T4 = 120 min, T5 = 150 min, T6 = 180 min) thereafter until delivery. We used a translabial approach in the absence of maternal pushing and uterine contractions [6]. The recorded transperineal measurements were Angle of Progression (AoP), defined by a tangent to the fetal head from the lower margin of the pubic symphysis and its long axis; Midline Angle (MLA), the angle between the anteroposterior axis of the maternal pelvis and the head midline; and Head Symphysis Distance (HSD), the distance along the infrapubic line between the caudal end of the pubic symphysis and the fetal skull. These were calculated as described by SIEOG [1], Barbera [7], Kalache [4], Youssef [8], and Ghi [9], as recorded in Fig. 1. All sonographic parameters obtained at different time intervals were longitudinally compared between the two groups of patients to obtain information about the influence of CSEA on the progression of the second stage of labor and on the incidence of operative delivery (vacuum application or cesarean section) or fetal head position with posterior occiput.
Table 1.
Protocol of CSEA administration in primiparous woman
| Cervical dilatation | Station of fetal head | Initial dose | Subsequent dose | ||
|---|---|---|---|---|---|
| Centimeters | Level | Medication, and intrathecal dose | Intrathecal volume (ml) | Medication, and epidural dose | Epidural volume (ml) |
| 2–3 | − 2/− 1 | Sufentanil 2.5 mg | 5 | Ropivacaine 0.05–0.10% or levobupivacaine 0.05–0.0625% | 15–20 |
| 3–5 | − 1 | Ropivacaine 0.04% or levobupivacaine 0.025% and sufentanil 2.5 mg | 5 | Ropivacaine 0.05–0.10% or levobupivacaine 0.0625% | 15–20 |
| > 6 | − 1 | Ropivacaine 0.05–0.06% or levobupivacaine 0.03–0.04% and sufentanil 2.5 mg | 5 | Ropivacaine 0.10% or levobupivacaine 0.0625% | 20 |
| Full cervical dilatation | − 1/0 | Ropivacaine 0.06% or levobupivacaine 0.05% | 5 | Ropivacaine 0.15% or levobupivacaine 0.0625% | 15 |
At full cervical dilation, after the complete rotation of the fetal head, it can be administered 5–7 ml of mepivacaine or lidocaine 1% for perineal analgesia or for an episiotomy/episiorrhaphy
Fig. 1.
Ultrasonographic measurements of the translabial parameters. a Angle of Progression (AoP); b Head Symphysis Distance (HSD); C Midline Angle (MLA)
Statistical analysis
The normality of continuous variables was checked through the Shapiro–Wilk test. Variables that verified the assumptions of normality are reported in terms of the mean (standard deviation, SD), while variables that did not verify this hypothesis are reported in terms of median (interquartile range, 25–75th percentile). Categorical variables are reported in terms of absolute frequency (frequency percentage). To compare the two groups of women, we applied the parametric T test or, when necessary, the non-parametric Mann–Whitney test or Chi-squared test. Correlations between the ultrasonographic parameters were assessed by the Pearson correlation coefficient, while correlation with the station of the fetal head, ordinal variable, was assessed by the non-parametric correlation of Spearman. Separate multivariate analyses were performed through the application of mixed models to assess the differences between ultrasound parameters (AOP, HSD, and MLA) in the two groups. The models are made up of a fixed part (the membership group and the type of birth) and a random part, as intercepts, (the patients have their value at time 0, which differs from that of the others). Also, the trend of values over time differed from woman to woman. It was considered significant at a p value < 0.05. In the case of multiple comparisons, the Bonferroni correction was applied; the level of significance α = 00:05 was divided by the number of comparisons made.
Results
The two groups of patients were homogenous, without significant differences in maternal age, body mass index (BMI), or fetal weight at birth (Table 2). The only differences were that in Group 1, the mean gestational age was significantly higher than in Group 2 and that patients with CSEA more often experienced spontaneous rupture of membranes than did patients without CSEA. No differences in terms of kind of delivery (spontaneous vs operative vs cesarean section) emerged in the two groups of patients. The average duration of the second stage of labor in Group 1 was significantly higher than in Group 2 (p < 0.001). As shown in Table 3, we reported eight births in the posterior occiput position without statistically significant differences between the two groups.
Table 2.
Demographic features, kind of delivery and duration of the second stage of labour in the two groups of patients
| Group 1 | Group 2 | p value | |
|---|---|---|---|
| n = 29 | n = 20 | ||
| Age | |||
| Mean (sd) | 32 (4.81) | 30.2 (2.93) | 0.193 |
| BMI | |||
| Mean (sd) | 25.3 (2.41) | 24.6 (1.98) | 0.326 |
| Gestational age | |||
| Median | 41 (40–41) | 39.9 (39.3–40.7) | 0.001 |
| Oxytocin use | |||
| n (%) | 19 (65.5%) | 10 (50%) | 0.277 |
| Spontaneous rupture of membranes | |||
| n (%) | 16 (55.2%) | 2 (10%) | 0.001 |
| Kind of delivery | |||
| Operative, n (%) | 6 (20.7%) | 2 (10%) | 0.661 |
| Spontaneous, n (%) | 21 (72.4%) | 17 (85%) | |
| Cesarean section, n (%) | 2 (6.9%) | 1 (5%) | |
| Duration of the second stage of labour (hours) | |||
| Mean (sd) | 02:21 (0:56) | 01:19 (0:40) | < 0.001 |
Table 3.
Birth outcomes in case of posterior occiput position of fetal head
| Group 1 | Group 2 | p value | ||
|---|---|---|---|---|
| Posterior occiput | ||||
| N (%) | 6 (20.7%) | 2 (10%) | 0.445 | |
| Spontaneous delivery | 1 | 1 | ||
| Operative delivery | ||||
| Vacuum | 2 | 1 | ||
| Vacuum + forceps | 1 | 0 | ||
| Cesarean section | 2 | 0 | ||
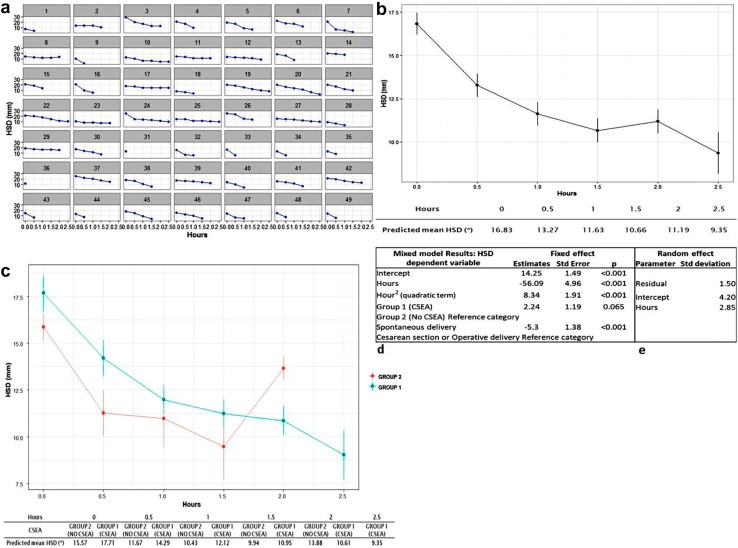
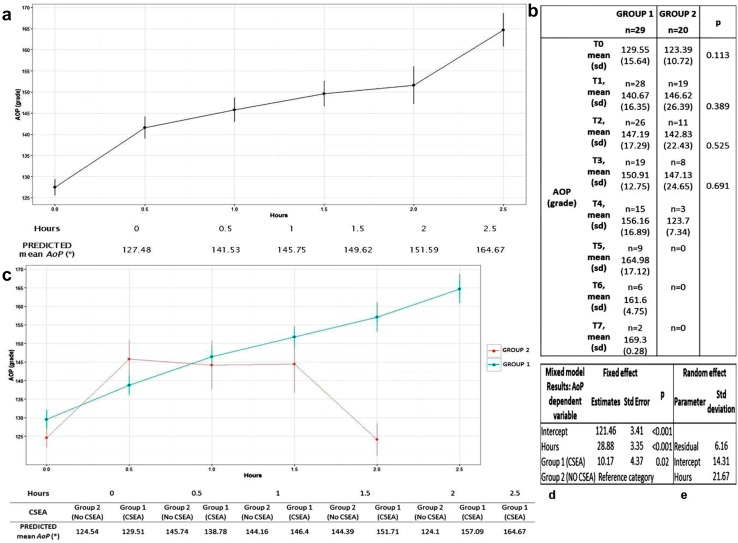
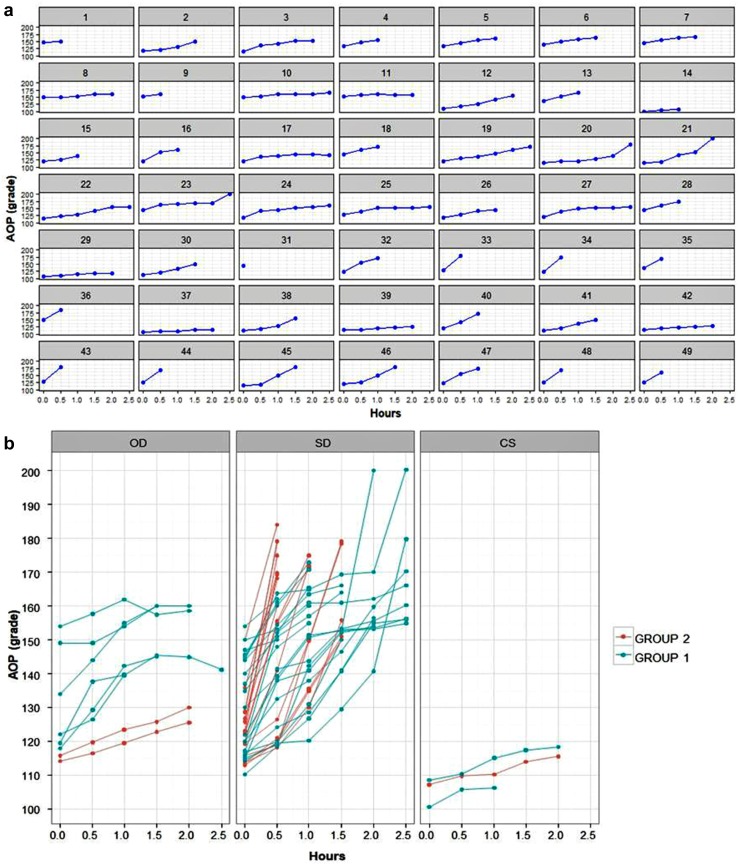
Figures 2 and 3 show the results progression angle (AoP). Each woman at the first measurement at T0 had a unique initial AoP and trend of values (Fig. 2a). No statistically significant differences were found between Groups 1 and 2 regarding the relation of AoP with the kind of delivery (Fig. 2b). In relation to time, we recorded that AoP increased linearly with the study intervals (Fig. 3a). In fact, we noticed that over time, among all patients (Group 1 + Group 2), the AoP grew by an average of 28.88° (standard error: 3.35). The average value of AoP at T0 was 129.55° in Group 1 and 123.39° in Group 2. Similar values were reproduced for all durations of the second stage in the two groups (Fig. 3b). Figures 3c and d show that neuraxial analgesia had a significant effect on the increase of AoP values (p = 0.024). In fact, the estimated value indicates that women with analgesia had an AoP higher than did women without. The average value of AoP for women without neuraxial analgesia at time 0 was 121.46°; for women with CSEA, AoP was 131.63°, considering only the fixed effects (Fig. 3d). Looking at the results of the random effects (Fig. 3e) for each group of patients, the intercept would be about 14.31° from the average of the group. There was no statistical evidence that over time the shape of the growth curve for AoP was different between Group 1 and Group 2.
Fig. 2.
a AOP performance of individual patients over time. Group 1: patients No. 1–29; Group 2: patients no 30–49; b birth outcomes divided by groups (OD operative delivery, SD spontaneous delivery, CS cesarean section)
Fig. 3.
a Overall average performance of AoP (Group 1 + 2) in relation with time; b average values of AOP in relation to time. Comparison between Group 1 and Group 2; c Average trend of AoP values divided by groups; d mixed model results for AOP: fixed effects; e mixed model results for AOP: random effects
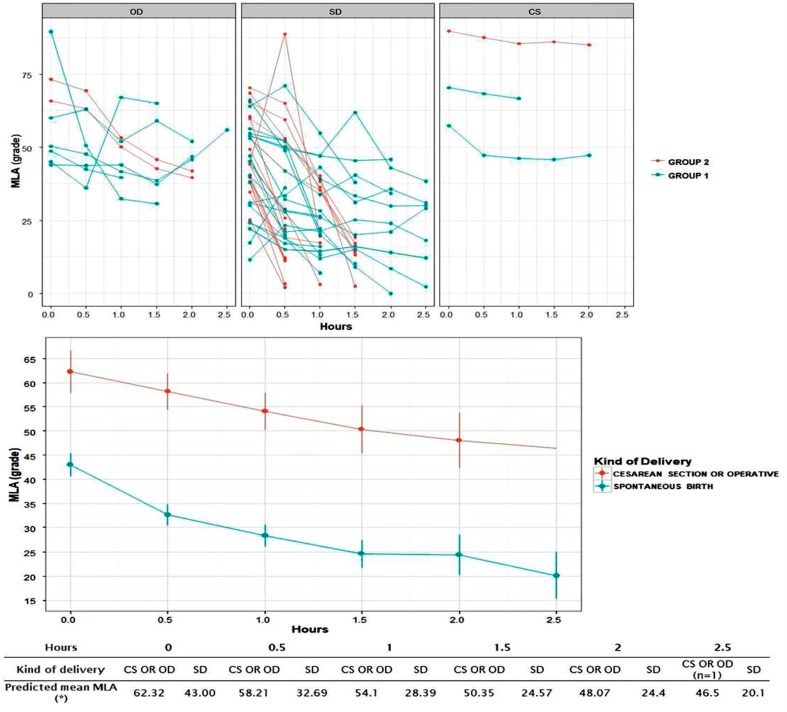
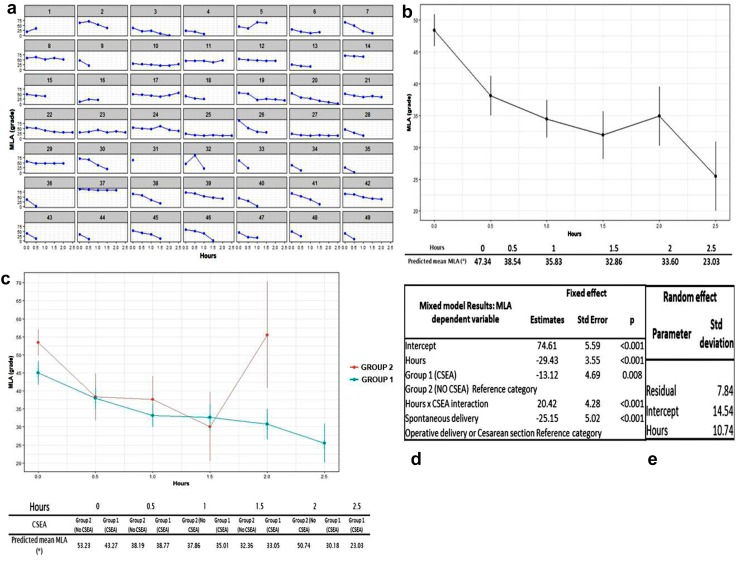
Figures 4 and 5 show the results for midline angle (MLA). Each woman at the first measurement at T0 had a unique MLA and trend of MLA values (Fig. 4a). Focusing on the changes of MLA values over time, we observed a decreasing trend (Fig. 4b). To explain the changes in MLA values, we considered a linear relationship with time. For constant parameters, we considered the kind of delivery, the CSEA factor, and the interactions between this factor and time; we found that the shape of the curve for women who received CSEA differed from that of women who did not receive it (Fig. 4c). Figure 4d presents the mixed model considering the fixed effects. The average MLA at time 0 in women who had CS or OD and without epidural was 74.61°. The effect of CSEA was significant (p = 0.008) and women who received neuraxial analgesia had MLA values lower than women who did not receive it. The average value of MLA expected for women undergoing neuraxial analgesia and who had cesarean or operative delivery was about 61.49°. We also found evidence that the shape of the growth curve for Group 1 was significantly different from that of Group 2 (p value < 0.001). Looking at the results for the random effects (Fig. 4e), we found that the variability between patients in the initial values of MLA was high. Figure 5a and b present the relationship between MLA and kind of delivery. The two curves, parallel, show that MLA values in patients that underwent a spontaneous birth tended to decrease over time and were statistically lower than the MLA values of women who had cesarean section or operative birth (p < 0.001) (Fig. 4e).
Fig. 4.
a MLA performance of individual patients over time. Group 1: patients No. 1–29; Group 2: patients no 30–49; b Overall average performance of MLA (Group 1 + 2) in relation to time; c Average trend of MLA values divided by groups; d mixed model results for MLA: fixed effects; e mixed model results for MLA: random effects
Fig. 5.
a Birth outcomes divided by groups; b MLA values in relation with birth outcomes (spontaneous delivery (SD) vs cesarean section (CS)-operative delivery (OD)
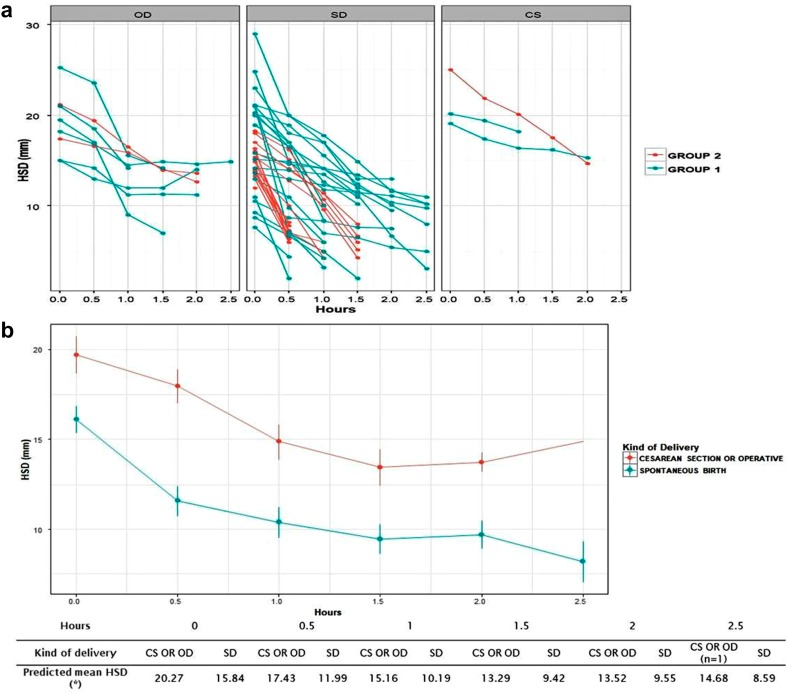
Figures 6 and 7 show the results for Head-Symphysis distance (HSD). Every woman presented with her own HSD and had her own trend of HSD values at T0 (Fig. 6a). Also, in this case we applied a “mixed model”. For fixed parameters, we considered neuraxial analgesia and the type of delivery (Fig. 6d). The random variables were the intercept and time (Fig. 6e). Women without neuraxial analgesia who underwent cesarean section or operative delivery had an average HSD value at T0 of 14.25 mm. The hour value described the rate of growth of HSD over time. In this case, we found a decreasing trend [b = − 56.09 min (standard error = 4.96 min)] that lasted at least up to 2 h (Fig. 6b). The effect of CSEA was of borderline significance. Over time, women with neuraxial analgesia had higher HSD values than those without (Fig. 6c). Patients who underwent cesarean section or operative delivery had an average HSD value of 16.49 mm, while patients who had a spontaneous vaginal birth had lower values (p < 0.001) (Fig. 7). Neither of the fixed factors considered showed a significant interaction with time; therefore, there was no evidence that the shapes of the curves relating to HSD differ between the two groups or in relation to the kind of delivery (Fig. 7a, b).
Fig. 6.
a HSD performance of individual patients over time. Group 1: patients No. 1–29; Group 2: patients no 30–49; b overall average performance of HSD (Group 1 + 2) in relation with time; c Average trend of HSD values divided by groups; d mixed model results for HSD: fixed effects; e mixed model results for HSD: random effects
Fig. 7.
a Birth outcomes divided by groups; b HSD values in relation with birth outcomes (spontaneous delivery (SD) vs cesarean section (CS)-operative delivery (OD)
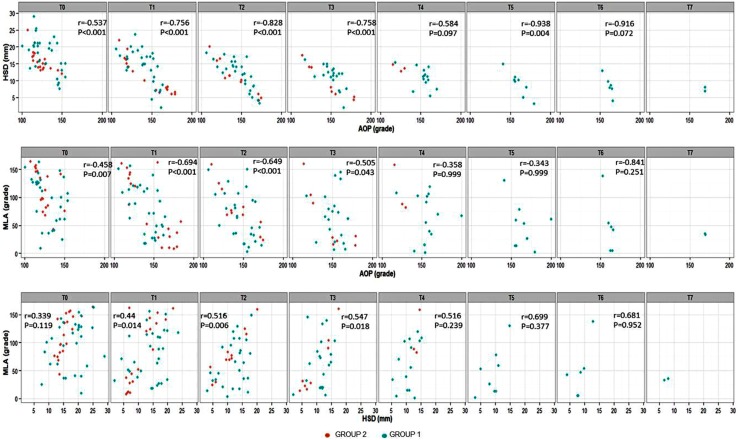
We also evaluated the correlation between the ultrasound parameters at a given time by correcting the p value for the number of comparisons made (Fig. 8). Results showed how AoP negatively correlates with HSD and MLA: high AoP values corresponded with low HSD and MLA values. Conversely, between HSD and MLA there was a positive correlation. From T5 on, the sample size was small and unbalanced between the two groups of patients, which affected the results.
Fig. 8.
Correlation between MLA–AoP–HSD
Focusing on the outcome of birth, we found that patients who underwent spontaneous birth had significantly lower values of MLA and HSD (p < 0.001) and a trend of constant increase in AoP values in each time interval than patients who underwent operative birth or cesarean section. In the case of a prolonged second stage of labor that required operative delivery, the prediction of success of a vacuum application correlated with AoP values more than 120°. In the eight cases of birth in the posterior position of fetal occiput, we had four operative deliveries (patients no 5, no 11, no 17, and no 39, as reported in Figs. 2a, 4a, 6a), two spontaneous births (patients no 1 and no 32, as reported in Figs. 2a, 4a, 6a), and two cesarean sections (patients no 14 and no 29, as reported in Figs. 2a, 4a, 6a). In the eight cases of operative birth, we had seven successes and a single case of failure in vacuum application that resulted in the need to perform an emergency CS. In this single case, the values of translabial ultrasonographic parametric before vacuum application were: AoP 115.6°; HSD 14.7 mm; and MLA 85.1°. The HSD evaluation for seven of the eight patients at T0 had values of more than 14 mm. All three patients that underwent TC presented AoP values less than 120°, MLA values more than 45°, and HSD values more than 14 mm before performing surgery.
In all our figures and tables, we reported abnormal values of HSD, MLA, and AoP at T4. This was because at this time, we evaluated only three patients, of which none underwent spontaneous birth: two had operative births and the other underwent cesarean section after unsuccessful application of vacuum.
Discussion
Combined spinal–epidural analgesia refers to a combination of procedures used for epidural and spinal analgesia. According to the period of labor during which the analgesia has to be performed, different combination of drugs can be used [10]. There is no consensus in the literature regarding the effects of analgesia on the progress of labor. Some authors suggest that epidural anesthesia results in an increase in the duration of the second stage of labor and in the incidence of operative deliveries or cesarean sections [11–16], as well as in persistent posterior occiput fetal head position at birth [17–20]. Others report that the basis of fetal malposition may be a result of maternal susceptibility [21].
More than 90% of the patients referred to our department require neuraxial analgesia, so it was not simple for us to obtain data about patients who did not require it. To get two numerically homogeneous groups of patients, we could not provide data about a larger sample.
In our experience, combined spinal–epidural analgesia did not increase the number of operative deliveries, cesarean sections, or persistent posterior occiput position of fetal head, but it caused a significative increase of duration of the second stage of labor.
Regarding the Angle of Progression, we noticed that the more it grew over time, the more likely was the possibility of spontaneous birth. In the case of limited variations between the subsequent measurements, it was more frequently necessary to perform operative delivery or cesarean section. In our experience, the successful application of vacuum correlated with Angle of Progression values of at least 120°, which is in agreement with Kalache’s findings [4].
Ghi and colleagues [22] reported that the lower were Midline Angle values at 40 min from full cervical dilatation, the greater was the probability to have a spontaneous birth. We found that in the case of non-spontaneous delivery, Midline Angle values remained almost unchanged or showed an increase rather than diminishing significantly over time. Such considerations may suggest that a delay in rotation of the fetal head is a plausible cause of slow fetal head disengagement resulting in a prolonged second stage of labor. In our study, it was not possible to establish a real relationship between Midline Angle values and kind of birth because of the small number of patients.
We noticed that higher Head Symphysis Distance correlated with a longer duration of the second stage of labor and that the more the Head Symphysis Distance values decreased, the greater was the chance of spontaneous birth. Youssef [23] reported that after 20 min from full cervical dilatation, 90% of patients requiring an operative delivery presented with Head Symphysis Distance values more than 14 mm. In our experience, 87.5% of patients that underwent operative delivery had Head Symphysis Distance values more than 14 mm after 30 min from full cervical dilatation, which is in agreement with the literature.
The results obtained in our study regarding posterior occiput position of the fetal head did not allow us to reach significant conclusions because of the small simple size. However, they seem to be in line with the literature [24] suggesting that this presentation influences the trends of Angle of Progression, Midline Angle, and Head Symphysis Distance and can lead to an increased duration of the second stage and a higher risk of operative delivery.
Regarding the relationship between combined spinal–epidural analgesia and transperineal ultrasonographic parameters, we found that analgesia correlated with significantly higher mean values of Angle of Progression and significantly lower values of Midline Angle for each time interval studied. A borderline statistical significance was, therefore, found between the effect of neuraxial analgesia on Head Symphysis Distance measurements, without conclusive evidence of differences between the two Groups of patients. The real mechanisms by which combined analgesia influences the trend of ultrasound parameters are not clear. One possibility is the nervous blockage of the pelvis that may result in a reduction of physiological reflexes, the strength of the pushing, and the perception of fetal head progression in the birth canal. Another mechanism could be the relaxation of pelvic muscles induced by drugs used for combined spino–epidural analgesia. These are only hypotheses that deserve further research on the effects induced by drugs used for combined spino-epidural analgesia on the diastatic arc of the anus, on the pelvic floor muscle, and on changes in the soft tissues of the birth canal.
The main limitation of our study was the small number of patients, in particular for the group of women without analgesia. The ultrasound scans performed after 2 h from full dilation (T4) were heavily influenced by a very small number of patients. This factor may have influenced the results of our clinical study. We propose expanding the number of patients to obtain more realistic and significant scientific results.
Acknowledgements
Special thanks to Dr. Paolo Fusco for the clinical and scientific contribution provided during data collection in our delivery room.
Compliance with ethical standards
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study protocol has been sent to the local Ethics Committee for evaluation and a written informed consent form, signed at the onset of labor, was obtained from each eligible patient. The study protocol conforms to the ethical guidelines of the ‘World Medical Association Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects’ adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964, and amended by the 64th WMA General Assembly, Fortaleza, Brazil, October 2013.
Informed consent
Informed consent was obtained from all the patients included in the study.
References
- 1.SIEOG (Società Italiana di Ecografia Ostetrico Ginecologica) (2014) Manuale di ecografia in travaglio di parto. Editeam
- 2.Nice (2014) Intrapartum care for healthy women and babies (2016 update)
- 3.RCOG (2011) Green-top Guideline No. 26. Operative vaginal delivery
- 4.Kalache KD, Duckelmann AM, Michaelis SA, Lange J, Cichon G, Dudenhausen JW. Transperineal ultrasound imaging in prolonged second stage of labor with occipitoanterior presenting fetuses: how does the “angle of progression” predict the mode of delivery? Ultrasound Obstet Gynecol. 2009;33(3):326–330. doi: 10.1002/uog.6294. [DOI] [PubMed] [Google Scholar]
- 5.Frigo MG, Larciprete G, Rossi F, Fusco P, Todde C, Jarvis S, Panetta V, Celleno D. Rebuilding the labor curve during neuraxial analgesia. J Obstet Gynaecol Res. 2011;37(11):1532–1539. doi: 10.1111/j.1447-0756.2011.01568.x. [DOI] [PubMed] [Google Scholar]
- 6.Ghi T, Contro E, Farina A, Nobile M, Pilu G. Three-dimensional ultrasound in monitoring progression of labor: a reproducibility study. Ultrasound Obstet Gynecol. 2010;36:500–506. doi: 10.1002/uog.7752. [DOI] [PubMed] [Google Scholar]
- 7.Barbera AF, Imani F, Becker T, Lezotte DC, Hobbins JC. Anatomic relationship between the pubic symphysis and ischial spines and its clinical significance in the assessment of fetal head engagement and station during labor. Ultrasound Obstet Gynecol. 2009;33(3):320–325. doi: 10.1002/uog.6322. [DOI] [PubMed] [Google Scholar]
- 8.Youssef A, Maroni E, Ragusa A, De Musso F, Salsi G, Iammarino MT, Paccapelo A, Rizzo N, Pilu G, Ghi T. The fetal head-symphysis distance: a simple and reliable ultrasound index of fetal station in labor. Ultrasound Obstet Gynecol. 2013;41(4):419–424. doi: 10.1002/uog.12335. [DOI] [PubMed] [Google Scholar]
- 9.Ghi T, Farina A, Pedrazzi A, Rizzo N, Pelusi G, Pilu G. Diagnosis of station and rotation of the fetal head in the second stage of labor with intrapartum translabial ultrasound. Ultrasound Obstet Gynecol. 2009;33:331–336. doi: 10.1002/uog.6313. [DOI] [PubMed] [Google Scholar]
- 10.Felis S, Parmigiani S. Il parto. Edi Ermes: Manuale di ostetricia e neonatologia; 2016. [Google Scholar]
- 11.Thorp JA, Hu DH, Albin RM, McNitt J, Meyer BA, Cohen GR, et al. The effect of intrapartum epidural analgesia on nulliparous labor: a randomized, controlled, prospective trial. Am J Obstet Gynecol. 1993;169:851–858. doi: 10.1016/0002-9378(93)90015-B. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman E, Lang JM, Cohen A, D’Agostino R, Jr, Datta S, Frigoletto FD., Jr Association of epidural analgesia with cesarean delivery in nulliparas. Obstet Gynecol. 1996;88:993–1000. doi: 10.1016/S0029-7844(96)00359-6. [DOI] [PubMed] [Google Scholar]
- 13.Halpern SH, Abdallah FW. Effect of labor analgesia on labor outcome. Curr Opin Anaesthesiol. 2010;23:317–322. doi: 10.1097/ACO.0b013e3283385492. [DOI] [PubMed] [Google Scholar]
- 14.Marucci M, Cinnella G, Perchiazzi G, Brienza N, Fiore T. Patient requested neuraxial analgesia for labor: impact on rates of cesarean and instrumental vaginal delivery. Anesthesiology. 2007;106:1035–1045. doi: 10.1097/01.anes.0000265165.06760.c2. [DOI] [PubMed] [Google Scholar]
- 15.Anim-Somuah M, Smyth RM, Jones L. Epidural versus non-epidural or no analgesia in labor. Cochrane Database Syst Rev. 2011;12:CD000331. doi: 10.1002/14651858.CD000331.pub3. [DOI] [PubMed] [Google Scholar]
- 16.Malvasi A, Tinelli A, Brizzi A, Guido M, Martino V, Casciaro S, Celleno D, Frigo MG, Stark M, Benhamou D. Intrapartum sonography for occiput posterior detection in early low dose combined spinal epidural analgesia by sufentanil and ropivacaine. Eur Rev Med Pharmacol Sci. 2010;14:799–806. [PubMed] [Google Scholar]
- 17.Ponkey SE, Cohen AP, Heffner LJ, Lieberman E. Persistent fetal occiput posterior position: obstetric outcomes. Obstet Gynecol. 2003;101:915–920. doi: 10.1016/s0029-7844(03)00068-1. [DOI] [PubMed] [Google Scholar]
- 18.Fitzpatrick M, McQuillan K, O’Herlihy C. Influence of persistent occiput posterior position on delivery outcome. Obstet Gynecol. 2001;98:1027–1031. doi: 10.1016/s0029-7844(01)01600-3. [DOI] [PubMed] [Google Scholar]
- 19.Lieberman E, Davidson K, Lee-Parritz A, Shearer E. Changes in fetal position during labor and their association with epidural analgesia. Obstet Gynecol. 2005;105:974–982. doi: 10.1097/01.AOG.0000158861.43593.49. [DOI] [PubMed] [Google Scholar]
- 20.LeRay C, Carayol M, Jaquemin S, Mignon A, Cabrol D, Goffinet F. Is epidural analgesia a risk factor for occiput posterior or transverse positions during labor? Eur J Obstet Gynecol Reprod Biol. 2005;1(123):22–26. doi: 10.1016/j.ejogrb.2005.02.009. [DOI] [PubMed] [Google Scholar]
- 21.Yancey MK, Pierce B, Schweitzer D, Daniels D. Observations on labor epidural analgesia and operative delivery rates. Am J Obstet Gynecol. 1999;180:353–359. doi: 10.1016/S0002-9378(99)70213-9. [DOI] [PubMed] [Google Scholar]
- 22.Ghi T, Youssef A, Maroni E, Arcangeli T, De Musso F, Bellussi F, et al. Intrapartum transperineal ultrasound assessment of fetal head progression in active second stage of labor and mode of delivery. Ultrasound Obstet Gynecol. 2013;41(4):430–435. doi: 10.1002/uog.12379. [DOI] [PubMed] [Google Scholar]
- 23.Youssef A, Maroni E, Ragusa A, Salsi G, Cariello L, Montaguti E et al (2013) The fetal head-symphysis distance and the mode of delivery in the second stage of labor. In: 22nd World Congress on ultrasound in obstetrics and gynecology; oral communication abstracts (submitted data)
- 24.Ghi T, Maroni E, Youssef A, Morselli-Labate AM, Paccapelo A, Montaguti E, Rizzo N, Pilu G. Sonographic pattern of fetal head descend: relationship with duration of active second stage of labour and occiput position at delivery. Ultrasound Obstet Gynecol. 2014;44:82–89. doi: 10.1002/uog.13324. [DOI] [PubMed] [Google Scholar]