Abstract
Objectives
The unilateral cleft lip (UCL) repair technique has evolved extensively over the past century into its modern form and has been identified as an important determinant of treatment outcome. The aim of this study was to evaluate and compare treatment outcomes following repair of UCL using either the Tennison-Randall (triangular) technique or the Millard rotation-advancement technique.
Materials and Methods
This was a prospective randomized controlled study conducted at the Lagos University Teaching Hospital between January 2013 and July 2014. A total of 48 subjects with UCL presenting for primary surgery and who satisfied the inclusion criteria were recruited for the study. The subjects were randomly allocated into two surgical groups through balloting. Group A underwent cleft repair with the Tennison-Randall technique, while group B underwent cleft repair with the Millard rotation-advancement technique. Surgical outcome was assessed quantitatively according to anthropometric measurements, using a method described by Cutting and Dayan (2003).
Results
Our 48 enrolled subjects were evenly divided into the two surgery groups (n=24 for both group A and group B). Twenty-seven subjects were male (56.3%) and 21 were female (43.8%), making a sex ratio of 1.3:1. The Millard group showed a greater increase in postoperative horizontal length and vertical lip height and a greater reduction in nasal width and total nasal width. Meanwhile, the Tennison-Randall group showed better reduction of Cupid's-bow width and better philtral height.
Conclusion
We did not find any significant differences in the surgical outcomes from the two techniques. The expertise of the surgeon and individual patient preferences are the main factors to consider when selecting the technique for unilateral cleft repair.
Keywords: Cleft lip, Assessement, Anthropometry
I. Introduction
Over the past century, there have been major advances in unilateral cleft-lip repair techniques toward the method's modern form1. The first documented cleft-lip repair involved simple freshening and approximation of the cut cleft edges, followed by the use of curved incisions to allow lengthening of the lip2. Straight-line closure repairs were used in the early 1900s3; however, straight-line closures had the disadvantage of creating a vertical scar contracture, leading to notching of the lip3,4. This led to the development of several methods in the mid-twentieth century that are grouped as quadrangular flaps, triangular flaps, and rotation-advancement techniques1,2. Triangular flap techniques involve one or more back-cuts placed along the cleft side's medial lip philtral ridge and one or more lateral lip-element triangular advancement flap to fill in the resultant defect(s) as the medial lip element is rotated down. Tennison-Randall's triangular technique is the most widely used triangular technique due to its geometrical predictability and reliability and its consistency in decreasing vertical lip contraction, but it, along with other triangular techniques, was alleged to produce scars that violated the philtrum5. To improve this, the Millard rotation-advancement technique was developed with the goal of placing most of the scar along the natural philtral column6. Nevertheless, the technique has required several further modifications to the original rotation-advancement technique6,7,8 to overcome additional shortcomings. Arguably, two basic techniques that are most commonly used for unilateral cleft lip (UCL) closure are the Tennison-Randall and the Millard rotation-advancement techniques. Each technique has its advocates, and both techniques address the importance of repositioning the lip muscle (orbicularis oris) in the correct anatomic orientation for optimal aesthetic and functional outcomes9.
Measurement of treatment outcome is vital to evaluate the success of cleft management and the degree of improvement, especially in the present age of evidence-based medicine where treatment guidelines for best practice are becoming an integral part of contemporary clinical practice10,11,12. Many studies that compared cleft lip and palate surgical treatments have been performed and they include evaluation of dentofacial growth and development, facial appearance, speech, hearing, nasal breathing, quality of life, and patient satisfaction. However, these reports also indicate that there is lack of consensus on agreed methodology for assessing outcomes across various research centers10,13.
The methods described for assessment of nasolabial appearance can be broadly divided into qualitative and quantitative approaches. The latter aims to objectively analyze the extent of abnormal morphology and the degree of disproportion through facial measurements14. Qualitative methods are more subjective and tend to analyze facial aesthetics and appearance impairment using scales, indices, scoring systems, and rankings.
The evaluation tools employed by these methods can be grouped into the following categories: direct clinical assessment, clinical photographic evaluation, clinical videographic assessment, and three-dimensional evaluation15. Clinical photographic evaluation is generally quick, cheap, and easy15, and this evaluation method can be done qualitatively, as demonstrated by several studies10,16,17,18.
Few studies in Nigeria have attempted to document the surgical management outcomes for orofacial clefts12; specifically, to the best of our knowledge, there are no studies from Nigeria that compare cleft-lip repair outcomes from two or more surgical techniques. The purpose of this study was to evaluate and compare the treatment outcome from surgical repair of UCL using either the Tennison-Randall or Millard techniques. We evaluated outcomes according to using preoperative and postoperative anthropometry measurements.
II. Materials and Methods
This was a prospective randomized controlled study of treatment outcomes from surgical repair of UCL using either the Tennison-Randall or Millard technique at Lagos University Teaching Hospital (Lagos, Nigeria) between January 2013 and July 2014. A total of 48 subjects with UCL presenting for primary surgery who satisfied the “rule of 10” were recruited for the study. Subjects with bilateral cleft lip and those that underwent a previous initial cleft surgery were excluded from the study. This study was approved by the Research and Ethics Committee of the Lagos University Teaching Hospital (IRB no. 34512). Written informed consent was obtained from parents/guardians of subjects before study enrollment.
Using a balloting method, the subjects were then randomly allocated to one of two surgical techniques for repair: a box was filled with 48 sealed envelopes, which each had a folded piece of paper on which either “A” or “B” was written. There were 24 pieces of paper with “A” and 24 with “B.” The subjects/guardians were asked to pick from the box and those that picked group A received the Tennison-Randall technique and those that picked group B received the Millard rotationadvancement technique.
The following data were recorded preoperatively on a proforma: age, sex, weight, height, and cleft type. Cleft lip and palate were classified according to Kernahan and Stark's classification19 with modifications specified by the International Confederation for Plastic and Reconstructive Surgery in 196720.
1. Preoperative evaluation
Routine preoperative blood investigations including haemoglobin estimation, electrolyte, urea, and creatinine levels, and electrocardiography were performed for each subject. Echocardiography was also performed when indicated. Subjects were referred to their pediatrician for clinical evaluation to rule out cardiovascular congenital anomalies, upper respiratory tract infection, ear infection, and other congenital anomalies that may be of clinical significance. Subjects were at least three months old, weighed at least 4.5 kg (10 pounds), and had a minimum haemoglobin concentration of 10 g/dL.
Preoperative photographs were taken for all subjects before the surgeries were performed.
2. Operative procedures
Surgical repair was done under general anesthesia with endotracheal intubation by two consultant oral and maxillofacial surgeons with extensive experience in cleft lip and palate surgery. One of the surgeons exclusively performed Tennison-Randall's triangular technique, while the other exclusively performed Millard's rotation-advancement technique. Postoperatively, the subjects were reviewed weekly for two weeks, and then once every month for three months; the surgical-outcome evaluation was performed at the final thirdmonth follow-up.
3. Evaluation of surgical outcome
Quantitative assessments were performed on anthropometric measurements, as described by Cutting and Dayan8. Anthropometric measurements were recorded from a two-dimensional full-frontal facial photograph of subjects taken with a digital camera (30× optical zoom, 16 MP, 2-720 mm wide angle, Canon PowerShot SX500 IS; Canon, Tokyo, Japan). Each measurement was taken three times by one of the authors (AMA), and the average of the three measurements was calculated. For standardization, each photograph was taken with the camera positioned 45 cm from the subject, with the interpupillary plane parallel to the floor (the subjects were positioned so that the lens of the camera was perpendicular to the interpupillary line). The photographs were then imported into Adobe Photoshop 7.0 software (Adobe Systems, Mountain view, CA, USA), for analysis.(Fig. 1)
Fig. 1. Clinical picture of a six-monthold female following Millard's repair imported into Adobe Photoshop 7.0 software showing postoperative measurement of vertical lip height on the cleft side (D1: 11.6 mm).
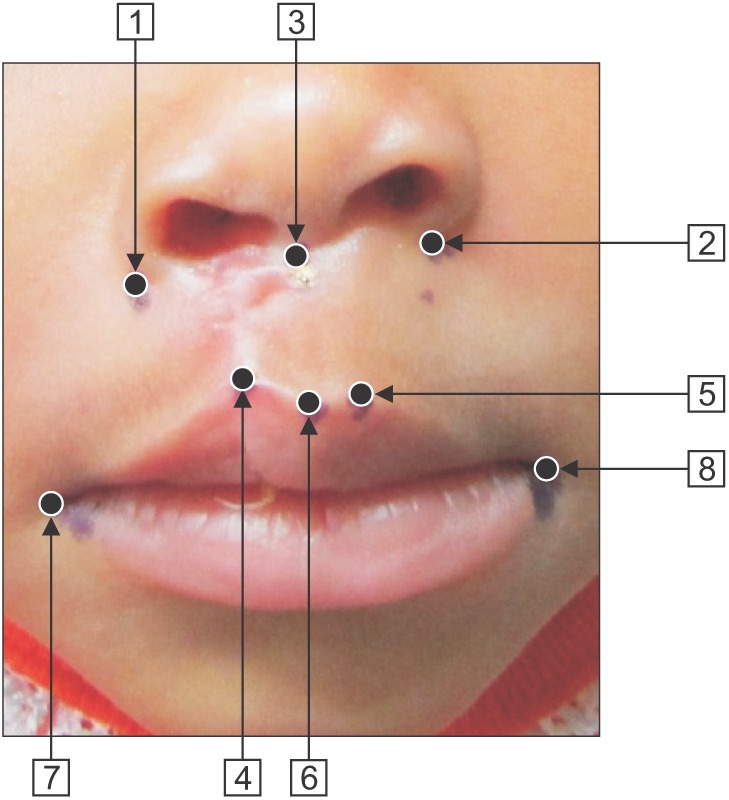
The following anthropometric measurements were taken. (Fig. 2, 3)
Fig. 2. Preoperative anthropometry reference points. (Point 1: alar base, cleft side, Point 2: alar base, non-cleft side, Point 3: midpoint of the columella, Point 4: peak of Cupid's bow, cleft side [where the white roll begins to disappear], Point 5: peak of Cupid's bow, non-cleft side, Point 6: corresponding peak of Cupid's bow, cleft side, Point 7: commissure, cleft side, Point 8: commissure, non-cleft side, Point 2 to 5: vertical lip height, non-cleft side, Point 1 to 4: vertical lip height, cleft side, Point 5 to 8: horizontal lip length, non-cleft side, Point 4 to 7: horizontal lip length, cleft side, Point 2 to 3: nasal width, non-cleft side, Point 1 to 3: nasal width, cleft side, Point 1 to 2: total nasal width).
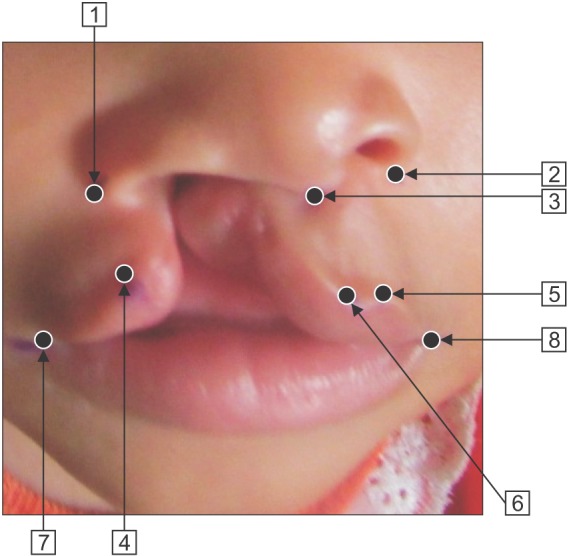
Fig. 3. Postoperative anthropometry reference points. (Point 1 to 3: nasal width, cleft side, Point 2 to 3: nasal width, non-cleft side, Point 4 to 5: Cupid's-bow width, Point 1 to 4: vertical lip height, cleft side, Point 2 to 5: vertical lip height, non-cleft side, Point 5 to 8: horizontal lip length, non-cleft side, Point 4 to 7: horizontal lip length, cleft side, Point 3 to 4: philtral height, cleft side, Point 3 to 5: philtral height, non-cleft side).
1) Preoperative
① Vertical lip height on non-cleft side: measured from the ala base to the peak of Cupid's bow on the same side.
② Vertical lip height on cleft side: measured from the ala base on the cleft side to a point where the white roll begins to disappear.
③ Horizontal lip length on non-cleft side: measured from peak of Cupid's bow on the non-cleft side to the ipsilateral commissure of the mouth.
④ Horizontal lip length on cleft side: measured from where the white roll starts to fade out to the ipsilateral commissure.
⑤ Nasal width: measured from ala base to the midpoint of the columella for both sides.
⑥ Total nasal width: measured from the ala base on the cleft side to the ala base on the non-cleft side.
2) Postoperative (measurements taken three months after the surgery)
① Vertical lip height: measured from the ala base to the peak of Cupid's bow, for both the cleft and non-cleft sides.
② Horizontal lip length: measured from the peak of Cupid's bow to the commissure for both the cleft and non-cleft sides.
③ Nasal width: measured from the ala base to the midpoint of the columella for both the cleft and non-cleft sides.
④ Total nasal width: measured from the ala base on the cleft side to the ala base on the non-cleft side.
⑤ Philtral height: measured from the peak of Cupid's bow to the midpoint of the columella for both the cleft and noncleft sides.
⑥ Cupid's-bow width: measured from the peak of Cupid's bow on one side to the peak on the other side.
4. Control subjects (anthropometric measurements)
Aged matched control subjects were recruited from the outpatient community health immunization clinic at the Lagos University Teaching Hospital.
Vertical lip height, horizontal lip length, nasal width, total nasal width, philtral height, and Cupid's-bow width were measured as defined above.
5. Data analyses
Data analyses were performed using the SPSS for Windows (ver. 17.0; SPSS Inc., Chicago, IL, USA). Means for each preoperative and postoperative variable were generated for each study group, and then the means were compared using Student's t-test. Additionally, the mean values of the measured variables in each group at the three-month postoperative period were compared with the control group's using Student's t-test (P<0.05).
III. Results
A total of 48 subjects requiring unilateral cleft-lip repair were enrolled in this study and their outcomes were analyzed. There were 24 subjects in both the Tennison-Randall (TR) group and the Millard group. Of the 48 subjects, 27 (56.3%) were male, and 21 (43.8%) were female (ratio=1.3:1). There were 12 (50.0%) males and 12 (50.0%) females (ratio=1:1) in the Millard group and there were 15 (62.5%) males and 9 (37.5%) females (ratio=1.7:1) in the TR group. There was no significant difference in the sex ratios between the TR and Millard groups (P=0.383).
Subject age at the time of lip repair ranged from 3 to 12 months. The majority of lip repairs was performed within 3 to 6 months for both surgery groups; Millard group, 21 (87.5%); TR group, 17 (70.8%).(Table 1) There was no statistically significant difference between the two groups (P=0.155).
Table 1. Subject age distribution.
| Age group (mo) | Millard group | Tennison-Randall group | Total |
|---|---|---|---|
| 3–6 | 21 (87.5) | 17 (70.8) | 38 (79.2) |
| 6–12 | 3 (12.5) | 7 (29.2) | 10 (20.8) |
| Total | 24 (100) | 24 (100) | 48 (100) |
Values are presented as number (%).
Complete cleft of the lip, alveolus, and palate was the most common type of cleft deformity among the study subjects (21/48, 43.8%). There were more cleft deformities on the left side (33/48, 68.8%) than on the right side, (15/48, 31.3%; ratio=2.2:1). A higher number of males (27/48, 56.3%) presented with cleft lips compared with females (21/48, 43.8%; male-to-female ratio=1.3:1). There was no significant difference in the cleft-deformity types between the two groups (P=0.281).(Table 2)
Table 2. Pattern of cleft lip distribution.
| Type of cleft | Millard group | Tennison-Randall group | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Right | Left | Male | Female | Right | Left | Male | Female | ||
| Cleft lip only | 1 | 7 | 6 | 2 | 3 | 4 | 5 | 2 | 15 (31.3) |
| Cleft lip and alveolus | 2 | 4 | 2 | 4 | 2 | 4 | 4 | 2 | 12 (25.0) |
| Cleft lip, alveolus, and palate | 3 | 7 | 4 | 6 | 4 | 7 | 6 | 5 | 21 (43.8) |
| Total | 6 | 18 | 12 | 12 | 9 | 15 | 15 | 9 | 48 (100) |
Values are presented as number only or number (%).
Four anthropometry comparisons were made across the TR and Millard groups:
1) Comparison of preoperative measurements of the cleft side verses the non-cleft side and the control, to know the impact of cleft deformity.
2) Comparison of postoperative and preoperative measurements of the cleft side, to know the effect of surgery.
3) Comparison of postoperative measurements of the cleft side versus the non-cleft side and the control, to assess surgical outcome.
4) Comparison of the surgical outcomes from the Tennison-Randall and Millard techniques.
1. Comparison of preoperative anthropometry measurements of the cleft versus the non-cleft side and the control
The mean values of horizontal lip length, vertical lip height, and nasal width on the cleft side were lower than those of the non-cleft side and the controls. These comparisons indicate statistically significant differences.(Table 3)
Table 3. Preoperative anthropometry measurements of cleft side and non-cleft sides and control.
| Variable | Millard group | TR group | ||
|---|---|---|---|---|
| Mean±SD | P-value | Mean±SD | P-value | |
| Horizontal lip length (mm) | ||||
| Cleft side | 15.30±3.06 | 14.80±2.62 | ||
| Non-cleft side | 18.40±3.72 | 0.001* | 16.40±3.07 | 0.008* |
| Control | 17.80±2.73 | 0.017* | 18.31±2.95 | 0.009* |
| Vertical lip height (mm) | ||||
| Cleft side | 12.54±1.84 | 12.02±3.22 | ||
| Non-cleft side | 16.84±3.76 | 0.001* | 14.58±4.00 | 0.001* |
| Control | 15.76±2.64 | 0.001* | 15.38±1.97 | 0.001* |
| Nasal width (mm) | ||||
| Cleft side | 25.20±4.46 | 0.001* | 22.48±3.65 | 0.001* |
| Non-cleft | 18.20±3.23 | 15.48±2.41 | ||
| Total nasal width of subject (mm) | 43.70±6.67 | 0.001* | 36.98±5.87 | 0.001* |
| Total nasal width of control (mm) | 30.78±1.57 | 30.27±3.70 | ||
(TR: Tennison-Randall, SD: standard deviation)
*P<0.05.
2. Comparison of pre- and postoperative lip and nasal width
Postoperatively, there was a significant increase in horizontal lip length and vertical lip height, as well as a significant decrease in nasal width in both surgical groups when compared with the preoperative measurements.(Table 4)
Table 4. Comparison of preoperative and postoperative measurements of lip height and nasal width of the cleft defect in Millard and TR groups.
| Variable | Millard group | TR group | ||
|---|---|---|---|---|
| Mean±SD | P-value | Mean±SD | P-value | |
| Horizontal lip length (mm) | ||||
| Preop cleft side | 15.30±3.07 | 0.001* | 14.80±2.62 | 0.013* |
| Postop cleft side | 19.50±4.48 | 17.08±3.24 | ||
| Vertical lip height (mm) | ||||
| Preop cleft side | 12.54±1.84 | 0.001* | 12.02±3.23 | 0.002* |
| Postop cleft side | 17.60±3.26 | 15.42±3.31 | ||
| Nasal width cleft side (mm) | ||||
| Preop cleft side | 25.20±4.46 | 0.001* | 22.49±3.65 | 0.001* |
| Postop cleft side | 19.17±2.72 | 18.24±3.96 | ||
| Preop total nasal width (mm) | 43.70±6.67 | 0.001* | 36.98±5.87 | 0.025* |
| Postop total nasal width (mm) | 36.76±4.53 | 34.84±5.74 | ||
(TR: Tennison-Randall, SD: standard deviation, Preop: preoperative, Postop: postoperative)
*P<0.05.
3. Comparison of postoperative anthropometry measurement of the cleft side versus the non-cleft side in the two surgical groups and the controls
1) TR group
There were statistically significant differences between horizontal lip length and vertical lip height, nasal width, and philtral height of the cleft side and the non-cleft side (P<0.05).(Table 5)
Table 5. Postoperative anthropometry measurement of cleft side, non-cleft side, and control in Millard and TR groups.
| Variable | Millard group | TR group | ||
|---|---|---|---|---|
| Mean±SD | P-value | Mean±SD | P-value | |
| Horizontal lip length (mm) | ||||
| Cleft side | 19.50±4.48 | 17.08±3.24 | ||
| Non-cleft side | 20.48±3.85 | 0.044* | 18.68±3.04 | 0.004* |
| Control | 17.78±2.73 | 0.092 | 18.31±2.95 | 0.166 |
| Vertical lip height (mm) | ||||
| Cleft side | 17.60±3.26 | 15.42±3.31 | ||
| Non-cleft side | 19.52±3.41 | 0.002* | 17.85±3.25 | 0.001* |
| Control | 15.76±2.64 | 0.051 | 15.38±1.97 | 0.952 |
| Nasal width (mm) | ||||
| Cleft side | 19.17±2.72 | 0.003* | 18.24±3.96 | 0.036* |
| Non-cleft side | 17.75±2.24 | 16.69±2.55 | ||
| Total nasal width of subject (mm) | 34.76±4.53 | 0.001* | 34.84±5.74 | 0.005* |
| Total nasal width of control (mm) | 30.78±1.57 | 30.28±3.71 | ||
| Philtral height (mm) | ||||
| Cleft side | 12.19±2.36 | 12.80±1.71 | ||
| With non-cleft side | 14.88±2.49 | 0.001* | 13.64±2.56 | 0.012* |
| With control | 11.82±1.71 | 0.558 | 11.87±1.57 | 0.033* |
| Cupid's-bow width (mm) | ||||
| Cleft subjects | 12.33±2.49 | 0.001* | 11.58±2.00 | 0.001* |
| Control | 9.34±1.03 | 9.65±0.78 | ||
(TR: Tennison-Randall, SD: standard deviation)
*P<0.05.
The mean postoperative vertical lip height of the TR group patients (15.42 mm) was slightly higher than that of the control group (15.38 mm), but not significantly so. However, there were significant statistical differences in the changes in philtral height (12.80 mm vs 11.87 mm), postoperative total nasal width (34.84 mm vs 30.28 mm), and Cupid's-bow width (11.58 mm vs 9.65 mm) when compared with the controls (P=0.001, P=0.001, and P<0.001, respectively).(Table 5)
2) Millard group
We observed statistically significant differences between postoperative horizontal lip length, vertical lip height, nasal width, and philtral height on the cleft side and the non-cleft side (P<0.05).(Table 5)
Postoperative vertical lip height, horizontal lip length, philtral height, Cupid's-bow width, and postoperative total nasal width, were all greater than those of the control. However, only changes in postoperative total nasal width and Cupid's-bow width were significantly different (P<0.001).(Table 5)
4. Comparison of postoperative anthropometry variables of the repaired cleft in the Tennison-Randall and Millard groups
The Millard group experienced a greater increase in postoperative horizontal lip length and vertical lip height, and a greater reduction in nasal width and total nasal width than the TR group. Meanwhile, the TR group experienced a greater increase in philtral height and Cupid's-bow width. However, only postoperative horizontal and vertical lip heights were significantly different between the two groups (P=0.037 and P=0.026).(Table 6)
Table 6. Postoperative anthropometry variables of repaired cleft side in Millard and TR groups (mm).
| Variable | Millard group | TR group | P-value |
|---|---|---|---|
| Horizontal lip length | 19.50±4.48 | 17.08±3.23 | 0.037* |
| Vertical lip height | 17.60±3.26 | 15.40±3.31 | 0.026* |
| Nasal width | 19.17±2.73 | 18.24±3.96 | 0.349 |
| Total nasal width subject | 36.76±4.53 | 34.84±5.74 | 0.205 |
| Philtral height | 12.19±2.36 | 12.80±1.71 | 0.312 |
| Cupid's-bow width | 12.33±2.49 | 11.58±2.00 | 0.257 |
(TR: Tennison-Randall, SD: standard deviation)
*P<0.05.
Values are presented as mean±standard deviation.
IV. Discussion
Surgical treatment should be based on the best available clinical research to avoid ineffective and biased treatment schemes and to optimize outcomes13,21. In this study, we evaluated cleft repair outcomes three months postoperatively. Our research was guided by the report that healing would be well advanced (i.e., at maturation/remodelling phase) by the 3rd month22. Studies have suggested that, during this maturation stage, collagen fiber remodeling is initiated, leading to attainment of optimal strength at the surgical site, thus determining the final quality of the residual scar by Clark23 in 1996. A three-month postoperative evaluation study was also done by Abdurrazaq et al.12 and Amaratunga24, and both reported comparable outcomes for older patients.
Anthropometry and clinical examination are the best methods to evaluate repaired cleft lip and nose morphology25 because it can quantitatively show the degree of deformity present. Most of the existing studies postoperatively evaluated lip morphology symmetry among UCL and palate patients. However, our study is unique in that we recorded pre- and postoperative anthropometric lip and nose measurements for all our UCL patients.
Preoperatively, horizontal lip length, vertical lip height, and nostril width on the cleft side were compared with those on the non-cleft side, and then among those of the controls. Our results showed that horizontal lip length and vertical lip height were shorter, and nostril width was wider in on the cleft sides than on the non-cleft sides, and compared with those of the control. This is consistent with findings by Chou et al.17 that suggest that UCL patients have a lip tissue hypoplasia on the cleft side. Also, it has been suggested that cleft deformity reflects not only the varying extent of embryological failure, but is also the ultimate result of growth and development impairment26.
Postoperative measurements of horizontal lip length, nostril width, vertical lip height, and philtral height on the cleft side showed marked improvements when compared to that of the non-cleft side. This indicates that surgical repair of a UCL is important and can provide hope to distressed parents and patients. Furthermore, our study demonstrates that repairs by both the TR and Millard techniques were effective. Our findings are consistent with those of Bilwatsch et al.27 and Hakim et al.18, who independently evaluated Millard's and Tennison-Randall techniques, respectively. Hakim et al.18 performed postoperative digital anthropometry on 18 patients who received UCL repairs with rotation-advancement and they compared these to normal controls. They found that there were improvements in the lip and nasal measurements. Similarly, Bilwatsch et al.27 reported improvements after repair with the Tennison-Randall technique.
Comparisons of horizontal lip length, nostril width, vertical lip height, Cupid's bow, and philtral height of the cleft side between patients and controls were not significantly different. This might suggest that the non-cleft side is a poor control for the repaired cleft side, possibly due to a compensatory hypertrophy on the non-cleft side. Symmetry of the cleft side with the control but not with the non-cleft side has been reported in other studies18,28. Consequently, it is now being speculated that the non-cleft side may not be an appropriate control for the cleft side28.
Cupid's bow of repaired UCLs has been shown to be wider than in normal controls11,29, but in our study, Cupid's bow in the TR group was more similar to those of the controls than the Millard group. Our findings thus agree with Bilwatsch et al.27, who reported that the TR technique preserved Cupid's bow by lowering the peak in the margin of the cleft. Those findings, however, stand in contrast with the study by Sameh et al.30, which concluded that the TR technique was less effective than the Millard technique in its ability to preserve Cupid's bow. This inconsistency might be because the Sameh et al.30 evaluation was performed two and a half years postoperatively.
Though postoperative vertical lip height in the TR group was better than that of Millard's group when compared with the control, it can be concluded that neither of these two techniques is significantly better when compared with controls.29.
The overall comparison of the outcomes from the two techniques using anthropometry showed statistically significant differences only in horizontal lip length and vertical lip height (P =0.037 and P =0.026, respectively). However, philtral height and Cupid's-bow width were better after TR, while horizontal lip length and total nasal width improved more after Millard's technique. This overall comparison was consistent with other studies that compared outcomes from Millard and TR repairs of UCLs29,31 in that there is no significant difference between the two techniques.
The Tennison-Randall lip repair is one of the most widely used methods for primary reconstruction. A clear contribution of this technique to cleft surgery is the recognition of its superior ability to preserve Cupid's bow by lowering the peak in the margin of the cleft27. However, one limitation of the Tennison-Randall lip repair is that a scar results across the philtrum in its lower third and, thus, it tends to produce a lip that is too long vertically29.
The Millard rotation-advancement technique, introduced in 1957, is the most widely used procedure for cleft-lip repair because it places most of the scar along the natural philtral border and is more flexible than geometric closure techniques. Furthermore, the Millard technique allows for complete muscular repair and minimizes discarding of normal tissue. Its disadvantages include the need for extensive undermining, risk of nostril stenosis on the cleft side and the potential to cause contraction with its consequent decrease in vertical lip height2.
V. Conclusion
Our study findings show no major difference in the overall results between the Tennison-Randall and Millard rotation-advancement repairs. Thus, either technique could be used for unilateral clefts, taking into consideration the strength and weakness of each technique. And, whichever repair is used, the end result is a function of individual preference, surgeon skill level, and the extent of cleft deformity.
Footnotes
Authors' Contributions: A.M.A. participated in study design, data collection and performed statistical analysis and also wrote the manuscript. O.J. participated in data collection and data analysis, and critically reviewed the manuscript. W.L.A. and M.O.O. participated in the study design, data analysis and critically reviewed the manuscript. A.B. critically reviewed the manuscript. All authors read and approved the final manuscript.
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
Ethics Approval and Consent to Participate: This study was approved by the Research and Ethics Committee of the Lagos University Teaching Hospital, Lagos, Nigeria (IRB no. 34512). Written informed consent was obtained from parents/guardians of subjects before study enrollment.
References
- 1.Demke JC, Tatum SA. Analysis and evolution of rotation principles in unilateral cleft lip repair. J Plast Reconstr Aesthet Surg. 2011;64:313–318. doi: 10.1016/j.bjps.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Arosarena OA. Cleft lip and palate. Otolaryngol Clin North Am. 2007;40:27–60. doi: 10.1016/j.otc.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 3.Sykes JM. Management of the cleft lip deformity. Facial Plast Surg Clin North Am. 2001;9:37–50. [PubMed] [Google Scholar]
- 4.Kirschner RE, LaRossa D. Cleft lip and palate. Otolaryngol Clin North Am. 2000;33:1191–1215. doi: 10.1016/s0030-6665(05)70277-2. [DOI] [PubMed] [Google Scholar]
- 5.Nwoku AL. Experiences on the surgical repair of unoperated adult cleft patients in Nigeria. Niger Med J. 1976;4:417–421. [Google Scholar]
- 6.Millard DR., Jr A radical rotation in single harelip. Am J Surg. 1958;95:318–322. doi: 10.1016/0002-9610(58)90525-7. [DOI] [PubMed] [Google Scholar]
- 7.Kim HY, Park J, Chang MC, Song IS, Seo BM. Modified Fisher method for unilateral cleft lip-report of cases. Maxillofac Plast Reconstr Surg. 2017;39:12. doi: 10.1186/s40902-017-0109-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cutting CB, Dayan JH. Lip height and lip width after extended Mohler unilateral cleft lip repair. Plast Reconstr Surg. 2003;111:17–23. doi: 10.1097/01.PRS.0000036045.22434.D4. [DOI] [PubMed] [Google Scholar]
- 9.van de Ven B, Defrancq J, Defrancq E. Cleft lip surgery: a practical guide. 2nd ed. Zgierz: Drukarna WIST; 2008. pp. 1–27. [Google Scholar]
- 10.Asher-McDade C, Roberts C, Shaw WC, Gallager C. Development of a method for rating nasolabial appearance in patients with clefts of the lip and palate. Cleft Palate Craniofac J. 1991;28:385–390. doi: 10.1597/1545-1569_1991_028_0385_doamfr_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 11.Christofides E. Evaluation of unilateral cleft lip repairs and the evolution of a new technique based on experience and research. J Plast Reconstr Aesthet Surg. 2009;62:50–55. [Google Scholar]
- 12.Abdurrazaq TO, Micheal AO, Lanre AW, Olugbenga OM, Akin LL. Surgical outcome and complications following cleft lip and palate repair in a teaching hospital in Nigeria. Afr J Paediatr Surg. 2013;10:345–357. doi: 10.4103/0189-6725.125447. [DOI] [PubMed] [Google Scholar]
- 13.Al-Omari I, Millett DT, Ayoub AF. Methods of assessment of cleft-related facial deformity: a review. Cleft Palate Craniofac J. 2005;42:145–156. doi: 10.1597/02-149.1. [DOI] [PubMed] [Google Scholar]
- 14.Farkas LG, Hajnis K, Posnick JC. Anthropometric and anthroposcopic findings of the nasal and facial region in cleft patients before and after primary lip and palate repair. Cleft Palate Craniofac J. 1993;30:1–12. doi: 10.1597/1545-1569_1993_030_0001_aaafot_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 15.Sharma VP, Bella H, Cadier MM, Pigott RW, Goodacre TE, Richard BM. Outcomes in facial aesthetics in cleft lip and palate surgery: a systematic review. J Plast Reconstr Aesthet Surg. 2012;65:1233–1245. doi: 10.1016/j.bjps.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Tobiasen JM, Hiebert JM. Facial impairment scales for clefts. Plast Reconstr Surg. 1994;93:31–41. [PubMed] [Google Scholar]
- 17.Chou PY, Luo CC, Chen PK, Chen YR, Samuel Noordhoff M, Lo LJ. Preoperative lip measurement in patients with complete unilateral cleft lip/palate and its comparison with norms. J Plast Reconstr Aesthet Surg. 2013;66:513–517. doi: 10.1016/j.bjps.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Hakim SG, Aschoff HH, Jacobsen HC, Sieg P. Unilateral cleft lip/ nose repair using an equal bows/straight line advancement technique: a preliminary report and postoperative symmetry-based anthropometry. J Craniomaxillofac Surg. 2014;42:e39–e45. doi: 10.1016/j.jcms.2013.05.028. [DOI] [PubMed] [Google Scholar]
- 19.Kernahan DA, Stark RB. A new classification for cleft lip and cleft palate. Plast Reconstr Surg Transplant Bull. 1958;22:435–441. doi: 10.1097/00006534-195811000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Kernahan DA. The striped Y--a symbolic classification for cleft lip and palate. Plast Reconstr Surg. 1971;47:469–470. doi: 10.1097/00006534-197105000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Campbell A, Costello BJ, Ruiz RL. Cleft lip and palate surgery: an update of clinical outcomes for primary repair. Oral Maxillofac Surg Clin North Am. 2010;22:43–58. doi: 10.1016/j.coms.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 22.Kumar V, Abbas AK, Fausto N. Robbins and Cotran pathologic basis of disease. 7th ed. Philadelphia: Elsevier Saunders; 2005. pp. 113–117. [Google Scholar]
- 23.Clark RA. Wound repair. In: Clark RAF, editor. The molecular and cellular biology of wound repair. New York: Plenum Press; 1996. pp. 3–50. [Google Scholar]
- 24.Amaratunga NA. Combining Millard's and Cronin's methods of unilateral cleft lip repair — a comparative study. Asian J Oral Maxillofac Surg. 2004;16:5–9. [Google Scholar]
- 25.Hurwitz DJ, Ashby ER, Llull R, Pasqual J, Tabor C, Garrison L, et al. Computer-assisted anthropometry for outcome assessment of cleft lip. Plast Reconstr Surg. 1999;103:1608–1623. doi: 10.1097/00006534-199905060-00007. [DOI] [PubMed] [Google Scholar]
- 26.Millard DR. Cleft craft: the evolution of its surgery: the unilateral deformity Vol. 1. Boston: Little Brown; 1976. pp. 15–40. [Google Scholar]
- 27.Bilwatsch S, Kramer M, Haeusler G, Schuster M, Wurm J, Vairaktaris E, et al. Nasolabial symmetry following Tennison-Randall lip repair: a three-dimensional approach in 10-year-old patients with unilateral clefts of lip, alveolus and palate. J Craniomaxillofac Surg. 2006;34:253–262. doi: 10.1016/j.jcms.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 28.Xing H, Bing S, Kamdar M, Yang L, Qian Z, Sheng L, et al. Changes in lip 1 year after modified Millard repair. Int J Oral Maxillofac Surg. 2008;37:117–122. doi: 10.1016/j.ijom.2007.08.209. [DOI] [PubMed] [Google Scholar]
- 29.Chowdri NA, Darzi MA, Ashraf MM. A comparative study of surgical results with rotation-advancement and triangular flap techniques in unilateral cleft lip. Br J Plast Surg. 1990;43:551–556. doi: 10.1016/0007-1226(90)90119-k. [DOI] [PubMed] [Google Scholar]
- 30.Sameh E, Amr S, Ashraf E. Evaluation of primary unilateral cleft lip repair: a proposed scoring system. Egypt J Surg. 2009;28:4–7. [Google Scholar]
- 31.Yamada T, Mori Y, Minami K, Mishima K, Sugahara T. Threedimensional facial morphology, following primary cleft lip repair using the triangular flap with or without rotation advancement. J Craniomaxillofac Surg. 2002;30:337–342. doi: 10.1054/jcms.2002.0320. [DOI] [PubMed] [Google Scholar]



