Abstract
Context:
Chronic obstructive pulmonary disease (COPD) is not only restricted to the pulmonary inflammation and airway obstruction but is also associated with comorbidities, which affect the therapeutic intervention and the quality of life and survival. Markers that can predict the systemic inflammation and a decline in the pulmonary function are of scientific interest. Adiponectin (APN) appears to be one such biomarker and can be used as a potential indicator of severity and response to treatment in patients of COPD.
Aims:
The study aims to find out the role of APN as a marker of inflammation in the pathogenesis of COPD and explore its relationship with the severity of the disease.
Settings and Design:
This was a cross-sectional study.
Subjects and Methods:
The study group consisted of 60 patients of COPD, which included 30 males admitted with acute exacerbation of COPD (AECOPD) and 30 males with stable COPD. The study group was compared with 30 healthy, age-matched males. APN was estimated by commercially available ELISA kits. Pulmonary function tests were performed on all cases and controls using standardized protocols on SPIROLAB III.
Statistical Analysis Used:
Statistical analysis was performed using Student's t-test and Pearson's correlation coefficient.
Results:
The levels of APN were found to be significantly higher in patients with COPD as compared to the controls and the levels increased with the severity of the disease were 16.10 ± 4.97 ng/ml and 11.43 ± 4.22 ng/ml, respectively, in AECOPD and COPD. A significant positive correlation was found between the levels of APN and interleukin (IL)-8 in patients of COPD, while the levels correlated negatively with percentage of forced expiratory volume in 1 s (FEV1%).
Conclusions:
The results reveal that APN is associated with the inflammatory process of COPD as suggested by its significant inverse relationship with FEV1% and positive correlation with a marker of inflammation such as IL-8. It can thus be used as a biomarker for disease severity and progression in patients of COPD, therefore aiding in risk stratification and therapeutic intervention.
Keywords: Adiponectin, chronic obstructive pulmonary disease, systemic inflammation
Introduction
Chronic obstructive pulmonary disease (COPD) is one of the major global diseases, predicted to be the third leading cause of mortality worldwide by the year 2020.[1] It has been defined by the Global Initiatives of Chronic Obstructive Lung Diseases (GOLD) as a disease state characterized by slowly progressive airflow limitation and includes both emphysema and chronic bronchitis.[2] The chronic nonspecific inflammation, which is the hallmark of COPD, causes the activation of inflammatory cells and release of various inflammatory mediators such as interleukin (IL)-6, IL-8 and tumor-necrosis-factor (TNF)-α, which are responsible for the repeated injury and repair of the airway, causing airway obstruction.[3]
There is growing awareness that COPD is a lung disease not restricted only to pulmonary inflammation and airway remodeling.[4] Systemic effects and extrapulmonary comorbidities are commonly associated, which affect not only the therapeutic intervention but also the quality of life and survival.[5] Cardiovascular disease, musculoskeletal disorders, diabetes mellitus (DM) II, metabolic syndrome are commonly prevalent comorbidities; however, the underlying basis is still under research.[6,7] It has been suggested that inflammatory mediators contribute to skeletal muscle wasting and cachexia and may thus initiate or worsen comorbidities.[8]
According to the latest GOLD updates, assessment of COPD is based on the symptoms of the patients and severity of spirometric abnormality. Percentage of forced expiratory volume in 1 s (FEV1%), a lung function parameter, is the available marker of disease severity and progression but correlates poorly with both symptoms and disease progression.
In the interest of improving the diagnosis and prognosis of COPD, several biomarkers have been investigated and found to be related to a faster decline in the lung function.[8]
Airway epithelium represents a central site for the mechanisms involved in the complex interactions between environmental triggers, airway inflammation, and metabolic pathways.[9,10] Regarding peripheral organs, muscle, liver, and adipose tissue are a source of wide range of inflammatory mediators that have systemic effects. The potential interaction between abnormal adipose tissue and lung function may be attributed to systemic inflammation, thus providing new insight into the pathogenesis of systemic involvement of COPD.[11]
Adiponectin (APN) is thus a newer cytokine synthesized by the adipocytes which may have a potential role in regulating the inflammatory response in COPD.[12] It has been proposed that epithelial cells in the airway stimulate the expression of IL-8 under APN, suggesting its pro-inflammatory action.[13] However, it has also been illustrated that APN is able to inhibit macrophages producing TNF-α and reduce its synthesis, suggesting that it has some anti-inflammatory effects.[14] At present, the mechanism of APN participation in the inflammation of COPD remains unknown.
Some studies have reported elevated levels of APN in COPD, while another study found it to be associated with a decrease in TNF-α production in macrophages.[15,16] The absence of APN has also been reported to be the cause of emphysema in APN knock-out mice.[17]
The aim of the present study was thus to find out the role of APN as a marker of inflammation in the pathogenesis of COPD and explore its relationship with the severity of the disease.
Subjects and Methods
This cross-sectional, observational study was conducted on 60 patients of COPD, calculated with a prevalence of 4.1% of COPD.[18] Clearance from the Institutional Research and Ethics Committee was obtained, and informed consent was taken from all the participants of the study.
The study group was divided into two subgroups of 30 patients of COPD each. Group I comprised of patients of COPD admitted in the hospital with acute exacerbation (AECOPD) and Group II had patients of COPD who had been in stable status for at least 4 weeks. All patients met the diagnostic criteria of the GOLD for COPD.[2] Patients with stable form of the disease were defined as those who had not been on any glucocorticoid or antibiotic treatment for the last 4 weeks before recruitment. The study group was compared with 30 healthy age- and sex-matched controls.
All participants of the study were normal weight (body mass index [BMI] 18.5–24.9 kg2) male subjects. Patients with severe bronchial asthma, bronchiectasis, any severe systemic illness, or any other APN comorbidities such as obesity and DM were excluded from the study.
Venous blood samples were taken from all the subjects, centrifuged immediately, and stored at −20°C. Plasma levels of APN and IL-8 levels were measured by commercially available ELISA kits (Oregenium for APN and Diaclone for IL-8). Pulmonary function tests were performed on all patients and controls using standardized methods on SPIROLAB III. Forced expiratory flow rates were measured and pulmonary function values were expressed as a percentage of predicted value.
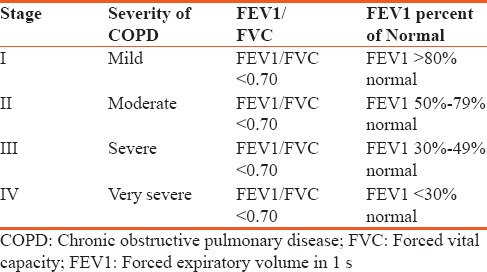
Patients were divided into four categories on the basis of severity according to GOLD staging based on value of FEV1 as shown in Table 1.
Table 1.
Categories of severity of chronic obstructive pulmonary disease
The results were expressed as mean ± standard deviation and statistical comparison was done using Student's t-test. Pearson's coefficient was used for correlation analysis. The difference was considered statistically significant when P < 0.05.
Results
The demographic profile of the subjects of the study group is shown in Table 2. There was no statistically significant difference in the age and BMI of the participants in the three subgroups. The duration of disease was not significantly different between patients of AECOPD and those with stable COPD.
Table 2.
Demographic profile of the subjects of the study group
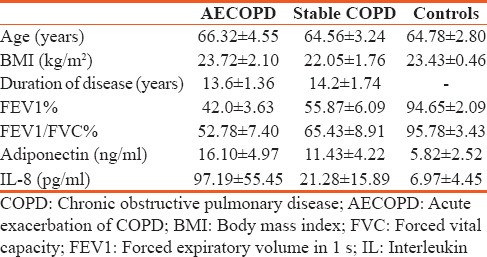
The pulmonary function parameters were found to be normal in the healthy controls and significantly decreased in patients of COPD (P < 0.001). Majority of the patients with AECOPD had Stage III or severe COPD, while patients with the stable form of the disease had Stage II or moderate disease as classified according to mean FEV1% [Table 1].
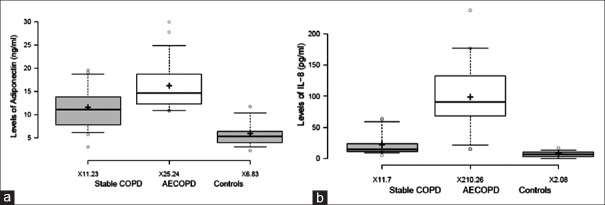
The difference in the plasma levels of APN and IL-8 between the three groups was found to be statistically significant [Table 1] (P < 0.001). The levels were found to be significantly higher in patients with COPD as compared to the controls, and the levels increased with the severity of the disease were significantly higher in the AECOPD as compared to the stable COPD [Figure 1].
Figure 1.
Levels of adiponectin and IL-8 in subjects of the study group. (a) Levels of Adiponectin (b) Levels of IL-8
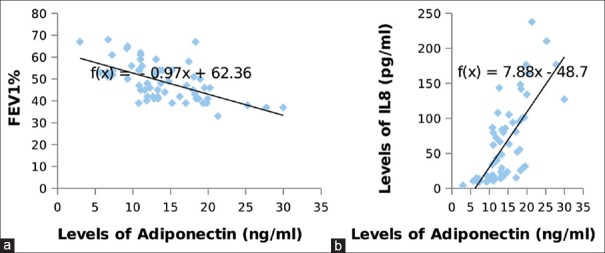
A statistically significant positive correlation (r = 0.720, P < 0.001) was found between the levels of APN and IL-8 in patients of COPD, while the levels correlated negatively with the lung function parameters (r = −0.580, P < 0.001) [Figure 2].
Figure 2.
Correlation between levels of adiponectin with IL-8 & FEV1% in the subjects of the study group. (a) Adiponectin vs FEV1% (b) Adiponectin vs IL-8
Discussion
COPD is a major cause of disability and death all over the world, and in India too, it is recognized as a major health problem requiring management from the primary health care level onward.[18]
COPD is a heterogeneous condition, characterized by progressive airway inflammation.[2] In the pathogenesis of COPD, inflammatory mediators such as IL-8, IL-6, and TNFα are secreted in the airway by the inflammatory cells, which are responsible for repeated injury and repair of the airway, finally causing airway obstruction.[3,19]
Metabolic disorders commonly associated with the COPD contribute to lung function impairment and mortality. A key role for systemic inflammation in the development of both metabolic disorder and lung function impairment has been reported, and therefore, scientific interest has shifted focus on adipocyte-derived cytokines such as APN.
APN is a proteic hormone, suggested to be involved in various metabolic processes such as immunity, insulin resistance, lipid and glucose metabolism, and inflammation.[16,20,21] It is secreted in the serum where it circulates as complexes of different molecular weights. Its properties are mediated by specific receptors that are widely expressed with AdipoR1, AdipoR2, and T-cadherin being present on epithelial and endothelial pulmonary cells, indicating a functional role on lung physiology.[22]
It has been suggested that the epithelial cells in the airway stimulate the expression of IL-8 under it, highlighting its pro-inflammatory role.[13] APN, on the other hand, is also able to inhibit macrophages producing TNFα and reduce its synthesis and biological activity, suggesting that it may have some anti-inflammatory effects.[14] Thus, APN could play both pro-inflammatory and anti-inflammatory roles, limiting the inflammatory response within a certain range.[23]
APN can therefore be a new marker of systemic inflammation in COPD.
Increased levels of APN have been reported in bronchoalveolar lavage fluid (BALF) and induced sputum of patients of COPD as compared to controls.[23] Certain studies have reported an elevation of plasma APN levels in patients with stable and AECOPD.[15,16,24] Another study demonstrated an elevated level of plasma APN in patients of COPD, which correlated inversely with severity of the disease.[25] In contrast, few studies observed no relationship between lung function and plasma APN.[15,16]
The present study not only explored the relationship between levels of APN and IL-8, a known marker of inflammation, but also its association with disease severity in the patients of COPD. Patients with AECOPD were found to have the highest levels of IL-8 and APN as compared to patients with the stable form of the disease, in line with the previous publications.[26,27] FEV1% was also found to be inversely correlated to plasma level of APN, suggesting that systemic inflammation might play a role in the development of airway obstruction.
The strength of the present study is that role of APN has been investigated alongside another established biomarker (IL-8), in relation to the lung function in the same subjects. In addition, the study population included all male subjects within the same BMI range, to avoid sex and weight difference in the plasma levels of APN. Although the sample size of this study is small, it includes patients of COPD in different severity grades, in comparison with healthy controls. The limitation of the study is that it was a cross-sectional study that limits a causal link between APN, IL-8 and lung function changes. Second, a concomitant measurement of APN and IL-8 in the BALF and induced sputum was not carried out, so the results reflect only the systemic changes and not the local concentration in the lungs.
The increased concentration of APN and IL-8 in the serum of patients of COPD and their positive correlation suggest that the inflammatory mediators may be interregulated. It is strongly suggested that APN could be a new marker of systemic inflammation in COPD.
Conclusions
FEV1% is the currently used spirometric predictor of morbidity and mortality in patients of COPD. Factors that predict the decline of FEV1% or in other words a decline of lung function in patients of COPD are of prognostic importance. The results of this study reveal that APN is associated with the inflammatory process of COPD as suggested by its significant inverse relationship with the marker of lung function, i.e., FEV1% and positive correlation with marker of inflammation such as IL-8. It can thus be used as a biomarker for disease severity and progression in patients of COPD, therefore aiding in risk stratification and therapeutic intervention.
Financial support and sponsorship
The study was conducted with the financial grant from the Department of Science and Technology, Chandigarh Administration.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge the financial support extended by the Department of Science and Technology, Chandigarh Administration, for carrying out this work.
References
- 1.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease study. Lancet. 1997;349:1498–504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 2.Global Strategy for the Diagnosis, Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2010. [Last accessed on 2017 Feb 25]. Available from: http://www.goldcopd.org .
- 3.Lapperre TS, Snoeck-Stroband JB, Gosman MM, Stolk J, Sont JK, Jansen DF, et al. Dissociation of lung function and airway inflammation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2004;170:499–504. doi: 10.1164/rccm.200401-112OC. [DOI] [PubMed] [Google Scholar]
- 4.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 5.Bianco A, Mazzarella G, Turchiarelli V, Nigro E, Corbi G, Scudiero O, et al. Adiponectin: An attractive marker for metabolic disorders in chronic obstructive pulmonary disease (COPD) Nutrients. 2013;5:4115–25. doi: 10.3390/nu5104115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nussbaumer-Ochsner Y, Rabe KF. Systemic manifestations of COPD. Chest. 2011;139:165–73. doi: 10.1378/chest.10-1252. [DOI] [PubMed] [Google Scholar]
- 7.Corbi GM, Carbone S, Ziccardi P, Giugliano G, Marfella R, Nappo F, et al. FFAs and QT intervals in obese women with visceral adiposity: Effects of sustained weight loss over 1 year. J Clin Endocrinol Metab. 2002;87:2080–3. doi: 10.1210/jcem.87.5.8516. [DOI] [PubMed] [Google Scholar]
- 8.Kolsum U, Roy K, Starkey C, Borrill Z, Truman N, Vestbo J, et al. The repeatability of interleukin-6, tumor necrosis factor-alpha, and C-reactive protein in COPD patients over one year. Int J Chron Obstruct Pulmon Dis. 2009;4:149–56. doi: 10.2147/copd.s5018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mazzarella G, Esposito V, Bianco A, Ferraraccio F, Prati MV, Lucariello A, et al. Inflammatory effects on human lung epithelial cells after exposure to diesel exhaust micron sub particles (PM1.0) and pollen allergens. Environ Pollut. 2012;161:64–9. doi: 10.1016/j.envpol.2011.09.046. [DOI] [PubMed] [Google Scholar]
- 10.van den Bemt L, van Wayenburg CA, Smeele IJ, Schermer TR. Obesity in patients with COPD, an undervalued problem? Thorax. 2009;64:640. doi: 10.1136/thx.2008.111716. [DOI] [PubMed] [Google Scholar]
- 11.Naveed B, Weiden MD, Kwon S, Gracely EJ, Comfort AL, Ferrier N, et al. Metabolic syndrome biomarkers predict lung function impairment: A nested case-control study. Am J Respir Crit Care Med. 2012;185:392–9. doi: 10.1164/rccm.201109-1672OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller M, Cho JY, Pham A, Ramsdell J, Broide DH. Adiponectin and functional adiponectin receptor 1 are expressed by airway epithelial cells in chronic obstructive pulmonary disease. J Immunol. 2009;182:684–91. doi: 10.4049/jimmunol.182.1.684. [DOI] [PubMed] [Google Scholar]
- 13.Otero M, Lago R, Gomez R, Lago F, Dieguez C, Gómez-Reino JJ, et al. Changes in plasma levels of fat-derived hormones adiponectin, leptin, resistin and visfatin in patients with rheumatoid arthritis. Ann Rheum Dis. 2006;65:1198–201. doi: 10.1136/ard.2005.046540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nakamura H, Yoshimura K, McElvaney NG, Crystal RG. Neutrophil elastase in respiratory epithelial lining fluid of individuals with cystic fibrosis induces interleukin-8 gene expression in a human bronchial epithelial cell line. J Clin Invest. 1992;89:1478–84. doi: 10.1172/JCI115738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tomoda K, Yoshikawa M, Itoh T, Tamaki S, Fukuoka A, Komeda K, et al. Elevated circulating plasma adiponectin in underweight patients with COPD. Chest. 2007;132:135–40. doi: 10.1378/chest.07-0227. [DOI] [PubMed] [Google Scholar]
- 16.Kirdar S, Serter M, Ceylan E, Sener AG, Kavak T, Karadaǧ F, et al. Adiponectin as a biomarker of systemic inflammatory response in smoker patients with stable and exacerbation phases of chronic obstructive pulmonary disease. Scand J Clin Lab Invest. 2009;69:219–24. doi: 10.1080/00365510802474400. [DOI] [PubMed] [Google Scholar]
- 17.Summer R, Little FF, Ouchi N, Takemura Y, Aprahamian T, Dwyer D, et al. Alveolar macrophage activation and an emphysema-like phenotype in adiponectin-deficient mice. Am J Physiol Lung Cell Mol Physiol. 2008;294:L1035–42. doi: 10.1152/ajplung.00397.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jindal SK, Aggarwal AN, Chaudhry K, Chhabra SK, D'Souza GA, Gupta D, et al. A multicentric study on epidemiology of Chronic Obstructive Pulmonary disease and its relationship with tobacco smoking and environmental tobacco smoke exposure. Indian J Chest Dis Allied Sci. 2006;48:23–9. [PubMed] [Google Scholar]
- 19.Culpitt SV, Rogers DF, Shah P, De Matos C, Russell RE, Donnelly LE, et al. Impaired inhibition by dexamethasone of cytokine release by alveolar macrophages from patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2003;167:24–31. doi: 10.1164/rccm.200204-298OC. [DOI] [PubMed] [Google Scholar]
- 20.Franssen FM, O'Donnell DE, Goossens GH, Blaak EE, Schols AM. Obesity and the lung: 5.Obesity and COPD. Thorax. 2008;63:1110–7. doi: 10.1136/thx.2007.086827. [DOI] [PubMed] [Google Scholar]
- 21.Tkacova R. Systemic inflammation in chronic obstructive pulmonary disease: May adipose tissue play a role? Review of the literature and future perspectives. Mediators Inflamm. 2010;2010:585989. doi: 10.1155/2010/585989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bianco A, Nigro E, Monaco ML, Matera MG, Scudiero O, Mazzarella G, et al. The burden of obesity in asthma and COPD: Role of adiponectin. Pulm Pharmacol Ther. 2017;43:20–5. doi: 10.1016/j.pupt.2017.01.004. [DOI] [PubMed] [Google Scholar]
- 23.Xie J, Yang XY, Shi JD, Deng XQ, Long W. A new inflammation marker of chronic obstructive pulmonary disease-adiponectin. World J Emerg Med. 2010;1:190–5. [PMC free article] [PubMed] [Google Scholar]
- 24.Krommidas G, Kostikas K, Papatheodorou G, Koutsokera A, Gourgoulianis KI, Roussos C, et al. Plasma leptin and adiponectin in COPD exacerbations: Associations with inflammatory biomarkers. Respir Med. 2010;104:40–6. doi: 10.1016/j.rmed.2009.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Chan KH, Yeung SC, Yao TJ, Ip MS, Cheung AH, Chan-Yeung MM, et al. Elevated plasma adiponectin levels in patients with chronic obstructive pulmonary disease. Int J Tuberc Lung Dis. 2010;14:1193–200. [PubMed] [Google Scholar]
- 26.Man SF, Connett JE, Anthonisen NR, Wise RA, Tashkin DP, Sin DD, et al. C-reactive protein and mortality in mild to moderate chronic obstructive pulmonary disease. Thorax. 2006;61:849–53. doi: 10.1136/thx.2006.059808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yende S, Waterer GW, Tolley EA, Newman AB, Bauer DC, Taaffe DR, et al. Inflammatory markers are associated with ventilatory limitation and muscle dysfunction in obstructive lung disease in well functioning elderly subjects. Thorax. 2006;61:10–6. doi: 10.1136/thx.2004.034181. [DOI] [PMC free article] [PubMed] [Google Scholar]