Abstract
Introduction:
The individuals suffering from various disabilities form a considerable proportion of the community. The psychological reactions associated with a deformity can be devastating to the disabled, parents, caregivers, and family which often lead to attitudes of hopelessness in the lives of these disabled individuals.
Objectives:
To assess the oral health status and treatment needs among 5–12-year-old children attending special school in Western Maharashtra, India.
Materials and Methods:
A descriptive cross-sectional study was conducted among 5–12-year-old children attending specials school in Western Maharashtra, India. The study group consisted of 100 children (62 males and 38 females). The oral health status was assessed by using decayed, missing, and filled teeth (DMFT) index, Community Periodontal Index, Dentition status and treatment needs. Information on disability status, intelligent quotient, and systemic diseases were recorded.
Results:
The mean age of the study population was 9.35 ± 2.92 years. There were 62 (62%) males and 38 (38%) females in the study population. Among the total children examined, 50% of the children were suffering from mental retardation (MR), followed by MR with cerebral palsy (20%). The overall mean decayed and filled teeth and DMFT scores were 3.53 ± 1.02 and 3.89 ± 1.30, respectively, and decayed component had the highest score in both the groups. A statistically significant difference has been observed among the gender (P < 0.001).
Conclusion:
There is a high proportion of dental treatment needs required for these children which reflect the barriers to access and utilize oral health care among these children. As dentist, we should emphasize on health education, periodic recall, and monitoring among these individuals.
Keywords: Decayed and filled teeth/decayed, missing and filled teeth, intelligent quotient, mental retardation, specially challenged
Introduction
Individual suffering from various disabilities forms a considerable percentage of the community. The psychological reactions associated with a deformity affects the disabled, parents, caregivers, and family members which often can lead to the attitudes of hopelessness in the lives of these disabled individuals.[1,2] The global prevalence of mentally challenged persons has ranged from 9% to 19%.[3,4] Out of 200 million children worldwide in developing countries, it was estimated that 80% of these were suffering from various types of disability.[5] As per the reports of National Sample Survey Organization (NSSO, India) conducted in 2002, 1.8% (18.5 million) of the total population of the country were disabled. Among them, the percentage with multiple disabilities was estimated to be around 10.63%.[2,4]
In developing countries, specially challenged condition is one among the main causes of deprivation and dependency. Specially challenged people tend to have a life of seclusion from the normal life of the community as a result of physical, social, psychological barriers, or the nonacceptance by the society. These children had little access to services or to decision-making that relates to their future and have no part in community production and consumption.[3]
The oral diseases are one of the most prevalent ailments among these disabled children worldwide, and dental care is the greatest unattended health need of these disabled.[5] There is a general agreement that the specially challenged children have higher rates of poor oral hygiene, gingivitis, and periodontitis than the general population.[3,6] Several studies have reported a higher prevalence of untreated dental disease in disabled children than in normal children.[2,7,8]
Universally, it is noticed that the moderate or severe gingivitis has been increased with the age and degree of mental retardation (MR). Local factors such as the tooth morphology, malocclusion, macroglossia, bruxism, and lack of normal masticatory function have been suggested as contributing factors for dental diseases.[9] In the society, many mentally challenged persons find it hard to survive as their nutritional status is low and services are inadequate and neglected. When these specially challenged children go for dental treatment, it is important that the dentist can understand the patient's problems, natural history, general conditions, and its complications on health. There has been inadequate information on the oral health status and dental treatment needs of the mentally disabled children. It is observed that the parents and guardians of these children have not been made aware of the importance of oral health and may lack knowledge of health-care system and also limited financial resources available to them. It is also noticed that the home care has been so neglected that most of them require extensive dental treatment.[2,10]
Hence, the present study was undertaken to assess the oral health status and dental treatment needs and oral hygiene practices among 5–12-year-old children attending special schools in Western Maharashtra, India.
Materials and Methods
A descriptive cross-sectional study was conducted among 5–12-year-old specially challenged children attending special schools in Western Maharashtra, India. The study group was consisted of 100 children (62 males and 38 females). Before start of the study, an ethical clearance was obtained from Institutional Ethics committee of the University. An official permission was obtained from higher authorities of schools. A prior consent was obtained from the parents or guardians of the special children of the schools. The study was carried over a period of one year from July 2015 to June 2016.
A pilot study was conducted on 15 specially challenged children to assess the feasibility and the time required to check for the medical records, oral health examination, and for the data collection. World Health Organization oral health assessment 1997 was used to collect the data. A single examiner carried out the examination on children enrolled for the pilot study at different interval of time with the similar conditions, and the reproducibility was found to be 95%. The special children with an intelligence quotient (IQ) of ≤85 were included in our study. Similarly, uncooperative children depending on the basis of their medical conditions and those who did not give consent were excluded out of the study.
Type III clinical examination as recommended by American Dental Association specifications was followed for the oral examination. The oral health status was recorded by using the dentition status and treatment needs index, decayed, missing and filled teeth (DMFT) index, and community periodontal index (CPI) by using appropriate methods. Sufficient numbers of required instruments were used for the oral examination. All aseptic precautions were carried out at the time of oral examination. The school children requiring complex treatment were referred to dental hospital. Recorded data were transferred from the precoded survey pro forma to Microsoft excel sheet in a computer. The statistical average, mean, and standard deviation were employed to represent the different measurements. The school medical record of each individual was reviewed with the help of the school authorities. The data on disability status, IQ, systemic diseases were recorded. The findings of the intraoral examination were reported to the school authorities and parents after the survey. After the examination, dental health education was delivered in the local language to all the parents, teachers, and caregivers. Statistical Analysis: descriptive statistics including number and percentages for categorical variables, means and standard deviations for continuous variables were calculated. Mann–Whitney (two-tailed) was used to compare between the independent samples for gender group. Kruskal–Wallis test was used to compare the treatment needs of various types of disability. P ≤ 0.05 was set as the significance level. The data were analyzed using the Statistical Package for Social Sciences (SPSS version 17.0; SPSS Inc., Chicago, IL, USA).
Results
Table 1 shows the demography of the study population. The mean age of the study population was 9.35 ± 2.92 years. There were 62 (62%) males and 38 (38%) females. MR was the most common disability among the children examined (50%), followed by MR with cerebral palsy (20%), MR with autism (11%), Down's Syndrome (8%), MR with visual impairment (8%), and MR with speech and hearing disability (3%). The IQ was assessed, and it was found that an IQ with moderate (54%), borderline and mild (33%), severe and profound (13%) was noticed. In our study, 68% of the children lived with their family members, whereas 32% of the children were residents of the respective institutions. In our study, most of the children brushed their teeth once daily (80%) and under the supervision of the caregiver (65%), twice daily (14%), and irregular (6%).
Table 1.
Demographic characteristics of study population
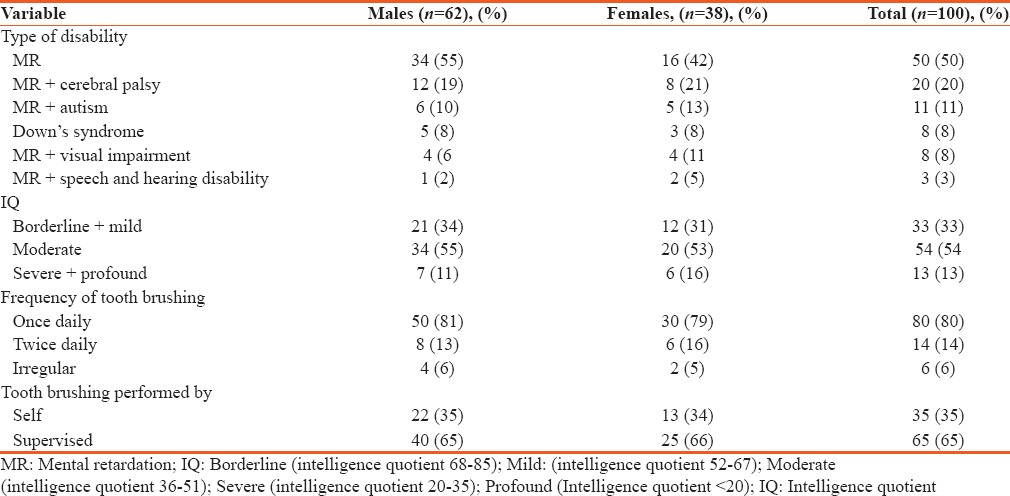
Table 2 depicted the mean caries prevalence according to gender and type of disability. The overall mean decayed and filled teeth (dft) and mean DMFT scores were 3.53 ± 1.02 and 3.89 ± 1.30, respectively, and the decayed component had the highest score in both the cases. There was a statistically significant difference among the gender (P = 0.001). Based on the type of disability, there was statistically significant difference for the mean dft/DMFT. Children with MR and cerebral palsy had the highest dft/DMFT score of 9.15 ± 1.03 and 4.80 ± 1.36, respectively. The children with Down's syndrome had the highest dft score of 4.0 ± 1.30. The decayed components (dt and DT) however were higher than the missing and filled components in all the disability groups.
Table 2.
Mean caries prevalence according to gender and type of disability
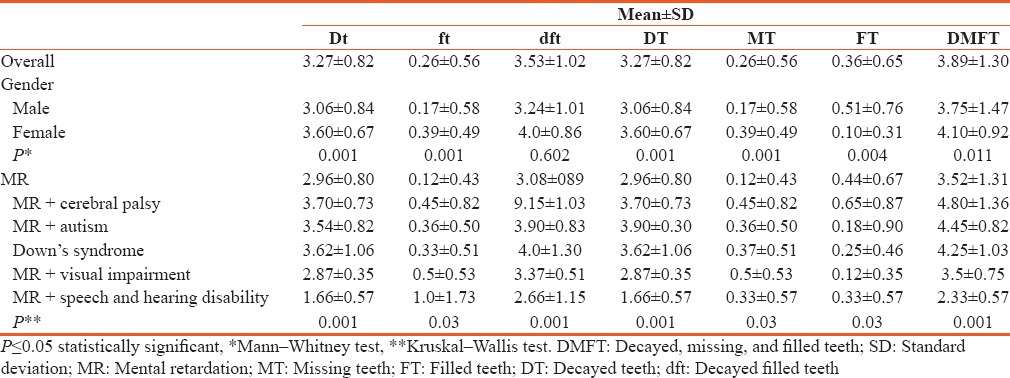
Table 3 shows the CPI scores recorded indicated that 11% had a healthy periodontium with a score of 0, 35% with score of 2 which indicates the presence of calculus, and 6% were not recorded. There was no statistically significant difference for the different CPI scores according to gender and type of disability.
Table 3.
Distribution of community periodontal index scores according to gender and type of disability
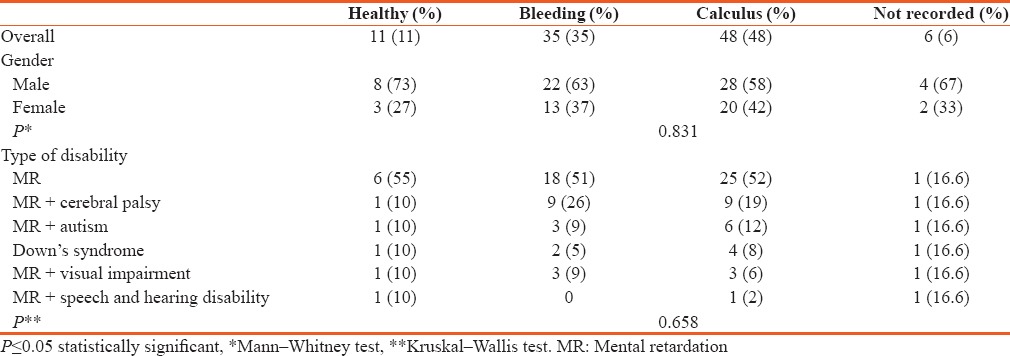
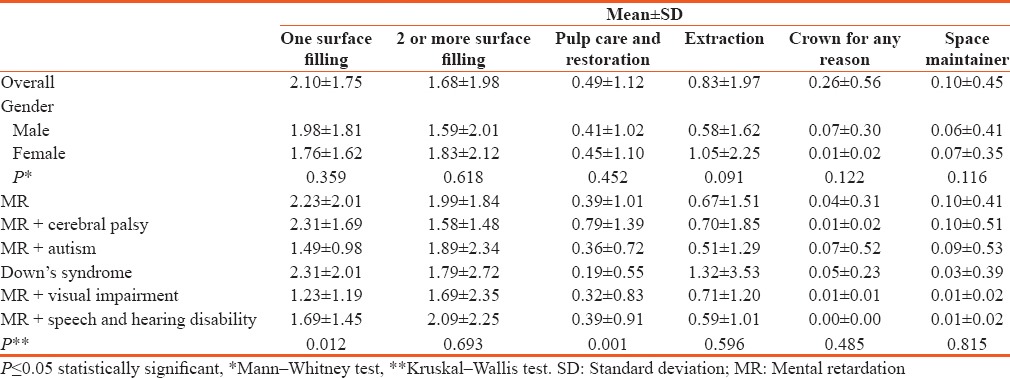
Table 4 shows the mean prevalence requiring the different types of dental treatment. In our study population, the need for restorative treatments was the most prevalent need, 2.10 ± 1.75 for one surface fillings and 1.68 ± 1.98 for two or more surface fillings, 0.83 ± 1.97 for tooth extraction, 0.49 ± 1.12 for pulp care and restoration, 0.26 ± 0.56 for crown for any reason, and 0.10 ± 0.45 for space maintainer. There was no statistically significant difference in the dental treatment needs based on gender distribution. However, one surface fillings and pulp care were statistically significant treatment needs among the different disability groups (P < 0.05) of the study population.
Table 4.
Distribution of the mean prevalence of disabled children requiring the different forms of treatment according to gender and type of disability
Discussion
Oral diseases are one of the common health problems among individuals with mental disabilities. The prevalence and severity of oral disease among this group are higher when compared to the general population.[6] As a result of low physical abilities with subsequent difficulties in maintaining oral hygiene, these individuals have poor oral cleanliness.[11,12,13,14]
Oral health may be affected by limited understanding on the importance of oral health management,[15] difficulties in communicating oral health needs,[16] anticonvulsant medications that impact on gingival health,[17] and a fear of treatment procedures.[18] Physical restraints and general anesthesia are commonly used to treat adults with disabilities who have fear and communication difficulties related to oral health.[19] The oral health management of individuals with disabilities often depends on other people, such as parents or employees with assisted living services.[20]
This study was conducted to assess the oral health status of specially challenged children of western Maharashtra, India. In context of oral hygiene practices, it was observed that nearly two-third of the children brushed “once daily.” These findings reflect the findings of study conducted in South India in which nearly 91% of the children brushed “once daily.” Supervised brushing was observed in majority of the children. These findings are similar to those in studies conducted by Gardens et al. in 2014.[2]
Oral hygiene of majority of the study participants was compromised due to the presence of calculus and/or bleeding gums with no significant difference among the disability types. Many studies have reported similar findings, and this has been attributed to improper bushing technique and inadequate knowledge of oral hygiene practices despite the high prevalence of parental attention.[2,11,21] Similar findings are reported in studies conducted in Turkey by Altun et al.[22] among 136 disabled individuals and Gizani et al.[21] in Belgium among 12-year-old disabled children which showed poor oral hygiene in 31.8% of children, with no significant differences found among disability types. Several other studies [12,14,23] have also found poor results for periodontal health and oral cleanliness among children with disabilities. These results may be due to low physical abilities, which could cause difficulties in tooth brushing among disabled children.
Similarly, effective removal of plaque and debris depends on the manual dexterity and low powers of concentration and lack of motor skills on part of the individual. Most of the studies have shown that people with disabilities have poor oral hygiene due to deficit of the above skills.[24] DMFT index was used to measure the dental caries levels among the study population. The overall DMFT and dft levels were higher in females compared to males. These findings are similar to those found in many other studies conducted in Saudi Arabia, North Korea, Israel, and Canary islands.[22,25,26,27] Overall DMFT levels in our study population were around 3.53 for deciduous dentition and 3.89 in permanent dentition. Similarly, higher levels of caries were reported in other studies.[24,26] Gizani et al.[21] reported a mean DMFT value of 2.9. Important factor to be considered here is that improvement of the oral health depends on the awareness of their families of the importance of oral hygiene habits.
Dental caries levels increased with increase in the severity of MR. In our study, we found higher proportion of decayed teeth and very few filled teeth which points to the fact that the dental care for these children was nearly nonexistent. We found a significant difference in caries burden in children of different disabilities. Children with MR and Down's syndrome had significantly higher caries burden. Similar findings have been reported by Gardens et al.[2] Furthermore, it was found in our study that the filled teeth and missing teeth were present among the study participants. This can be attributed to the fact that majority of the children were noninstitutional and had access to dental services. The treatment needs reflect the high need for restorative and rehabilitative world.[2,12,28]
Conclusion
A high proportion of treatment needs found in this study reflect the barriers to access and utilize oral health care among these children. Furthermore, a high cost of dental treatment may further discourage the children and their caregivers from getting the treatment. Concerned authorities should take necessary steps in improving the oral health of these children and take steps to provide the caretakers the monetary support needed to achieve optimum health of children. As dentist, we should emphasize on health education and periodic recall and monitoring among these individuals.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Fereday J, Oster C, Darbyshire P. Partnership in practice: What parents of a disabled child want from a generic health professional in Australia. Health Soc Care Community. 2010;18:624–32. doi: 10.1111/j.1365-2524.2010.00935.x. [DOI] [PubMed] [Google Scholar]
- 2.Gardens SJ, Krishna M, Vellappally S, Alzoman H, Halawany HS, Abraham NB, et al. Oral health survey of 6-12-year-old children with disabilities attending special schools in Chennai, India. Int J Paediatr Dent. 2014;24:424–33. doi: 10.1111/ipd.12088. [DOI] [PubMed] [Google Scholar]
- 3.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization world mental health surveys. JAMA. 2004;291:2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 4.Tesini DA. An annotated review of the literature of dental caries and periodontal disease in mentally retarded individuals. Spec Care Dentist. 1981;1:75–87. doi: 10.1111/j.1754-4505.1981.tb01232.x. [DOI] [PubMed] [Google Scholar]
- 5.Purohit BM, Singh A. Oral health status of 12-year-old children with disabilities and controls in Southern India. WHO South East Asia J Public Health. 2012;1:330–8. doi: 10.4103/2224-3151.207029. [DOI] [PubMed] [Google Scholar]
- 6.Atsuo A, Murakami J, Akiyama S, Morisaki I. Etiologic factors of early onset periodontal disease in down's syndrome. Jpn Dent Sci Rev. 2008;44:118–27. [Google Scholar]
- 7.Nelson LP, Getzin A, Graham D, Zhou J, Wagle EM, McQuiston J, et al. Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr Dent. 2011;33:29–36. [PubMed] [Google Scholar]
- 8.Evans DJ, Greening S, French AD. A study of the dental health of children and young adults attending special schools in South Glamorgan. Int J Paediatr Dent. 1991;1:17–24. doi: 10.1111/j.1365-263x.1991.tb00316.x. [DOI] [PubMed] [Google Scholar]
- 9.James AE. The Invulnerable Child. New York: Guilford Press; 1987. Risk, Vulnerability, and Resilience; an overview; pp. 3–48. [Google Scholar]
- 10.Klingberg G, Hallberg U. Oral health-Not a priority issue a grounded theory analysis of barriers for young patients with disabilities to receive oral health care on the same premise as others. Eur J Oral Sci. 2012;120:232–8. doi: 10.1111/j.1600-0722.2012.00961.x. [DOI] [PubMed] [Google Scholar]
- 11.Ivancić Jokić N, Majstorović M, Bakarcić D, Katalinić A, Szirovicza L. Dental caries in disabled children. Coll Antropol. 2007;31:321–4. [PubMed] [Google Scholar]
- 12.Iida H, Lewis CW. Utility of a summative scale based on the Children with Special Health Care Needs (CSHCN) screener to identify CSHCN with special dental care needs. Matern Child Health J. 2012;16:1164–72. doi: 10.1007/s10995-011-0894-6. [DOI] [PubMed] [Google Scholar]
- 13.Shaw L, Maclaurin ET, Foster TD. Dental study of handicapped children attending special schools in Birmingham, UK. Community Dent Oral Epidemiol. 1986;14:24–7. doi: 10.1111/j.1600-0528.1986.tb01488.x. [DOI] [PubMed] [Google Scholar]
- 14.Hennequin M, Faulks D, Roux D. Accuracy of estimation of dental treatment need in special care patients. J Dent. 2000;28:131–6. doi: 10.1016/s0300-5712(99)00052-4. [DOI] [PubMed] [Google Scholar]
- 15.Shapira J, Efrat J, Berkey D, Mann J. Dental health profile of a population with mental retardation in Israel. Spec Care Dentist. 1998;18:149–55. doi: 10.1111/j.1754-4505.1998.tb01137.x. [DOI] [PubMed] [Google Scholar]
- 16.Dunning JM. Principles of Dental Public Health. Cambridge: Harvard University Press; 1986. [Google Scholar]
- 17.Stabholz A, Mann J, Sela M, Schurr D, Steinberg D, Shapira J, et al. Caries experience, periodontal treatment needs, salivary pH, and Streptococcus mutans counts in a preadolescent down syndrome population. Spec Care Dentist. 1991;11:203–8. doi: 10.1111/j.1754-4505.1991.tb01732.x. [DOI] [PubMed] [Google Scholar]
- 18.Casamassimo PS, Seale NS, Ruehs K. General dentists' perceptions of educational and treatment issues affecting access to care for children with special health care needs. J Dent Educ. 2004;68:23–8. [PubMed] [Google Scholar]
- 19.Forsberg H, Quick-Nilsson I, Gustavson KH, Jagell S. Dental health and dental care in severely mentally retarded children. Swed Dent J. 1985;9:15–28. [PubMed] [Google Scholar]
- 20.Jain M, Bharadwaj SP, Kaira LS, Bharadwaj SP, Chopra D, Prabu D, et al. Oral health status and treatment need among institutionalised hearing-impaired and blind children and young adults in Udaipur, India. A comparative study. Oral Health Dent Manag. 2013;12:41–9. [PubMed] [Google Scholar]
- 21.Gizani S, Declerck D, Vinckier F, Martens L, Marks L, Goffin G, et al. Oral health condition of 12-year-old handicapped children in Flanders (Belgium) Community Dent Oral Epidemiol. 1997;25:352–7. doi: 10.1111/j.1600-0528.1997.tb00954.x. [DOI] [PubMed] [Google Scholar]
- 22.Altun C, Guven G, Akgun OM, Akkurt MD, Basak F, Akbulut E, et al. Oral health status of disabled individuals attending special schools. Eur J Dent. 2010;4:361–6. [PMC free article] [PubMed] [Google Scholar]
- 23.Reuland-Bosma W, van Dijk J. Periodontal disease in down's syndrome: A review. J Clin Periodontol. 1986;13:64–73. doi: 10.1111/j.1600-051x.1986.tb01416.x. [DOI] [PubMed] [Google Scholar]
- 24.Rao D, Amitha H, Munshi AK. Oral hygiene status of disabled children and adolescents attending special schools of South Canara, India. Hong Kong Dent J. 2005;2:107–12. [Google Scholar]
- 25.Tiller S, Wilson KI, Gallagher JE. Oral health status and dental service use of adults with learning disabilities living in residential institutions and in the community. Community Dent Health. 2001;18:167–71. [PubMed] [Google Scholar]
- 26.Rao DB, Hegde AM, Munshi AK. Caries prevalence amongst handicapped children of South Canara district, Karnataka. J Indian Soc Pedod Prev Dent. 2001;19:67–73. [PubMed] [Google Scholar]
- 27.Brown JP, Schodel DR. A review of controlled surveys of dental disease in handicapped persons. ASDC J Dent Child. 1976;43:313–20. [PubMed] [Google Scholar]
- 28.Lewis CW. Dental care and children with special health care needs: A population-based perspective. Acad Pediatr. 2009;9:420–6. doi: 10.1016/j.acap.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


