CASE REPORT
A 75-year-old female patient presented to the pulmonary medicine outpatient department. She is being referred by her treating physician as a case of right lower lobe pneumonia. She is a diabetic and hypertensive for the last 8 years and is well controlled on medication. She used to work as a head load worker in a coffee plantation and is leading a retired life at present. There was no history of chest trauma or any symptom suggestive of chronic lung diseases. There were no significant illnesses in childhood. She was never a smoker but used to chew tobacco. On examination, she is of short stature and poorly nourished. There is exaggerated thoracic kyphosis and scoliosis to the left. Chest movements are diminished on right lower part with impaired percussion note. Breath sound is diminished on the right side and coarse crackles are heard on right infrascapular region. A presumptive diagnosis of right lower lobe pneumonia with synpneumonic effusion was made. Blood routine and sputum examinations were within normal limits. Her symptoms responded to antibiotic and symptomatic measures. The follow-up X-ray showed a nonhomogenous opacity in the right lower zone [Figure 1]. Computed tomography (CT) thorax with contrast was performed which clinched the diagnosis [Figures 2-4].
Figure 1.
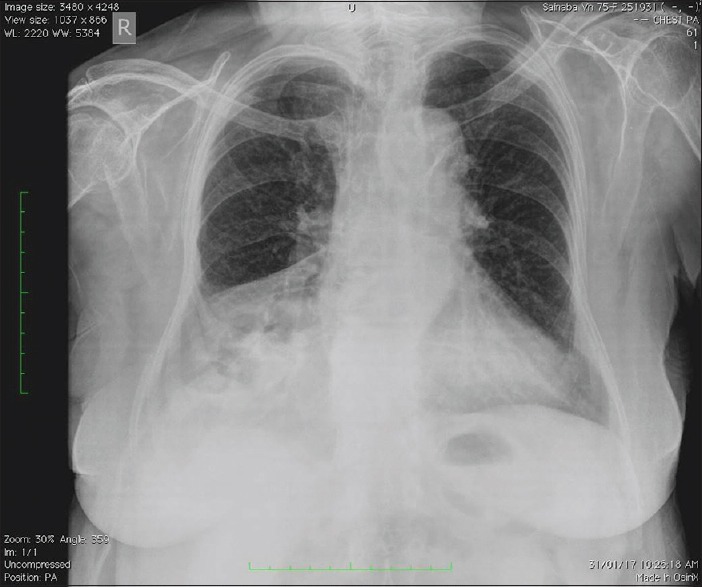
X-ray chest posteroanterior view showing nonhomogeneous opacity right lower zone
Figure 2.

Computed tomography thorax sagittal view showing herniation through anterior foramen
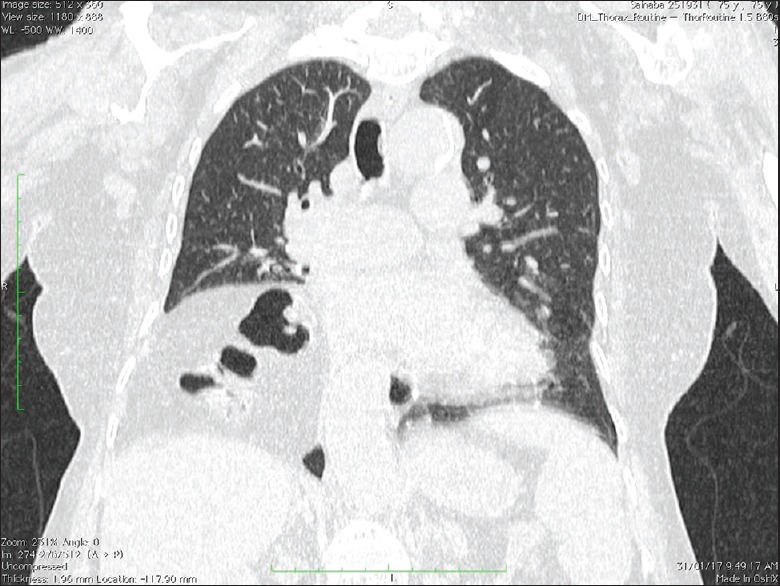
Figure 4.
Computed tomography thorax demonstrating bilateral Morgagni hernia and contrast clearly showing transverse colon on the right side
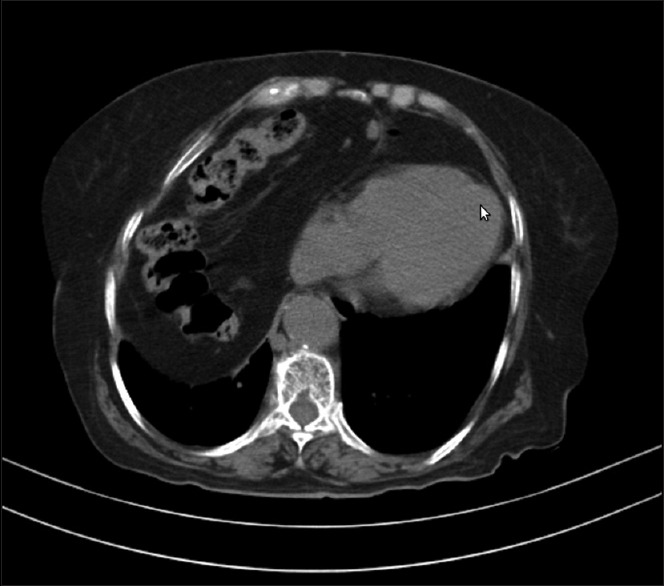
Figure 3.
Computed tomography thorax demonstrating herniation of abdominal contents to thoracic cavity
QUESTIONS
Question 1: What is the diagnosis based on X-ray chest posteroanterior?
Question 2: What is the final diagnosis based on CT findings?
ANSWERS
Answer 1: X-ray chest shows nonhomogenous opacity and there is no air bronchogram. This rules out the possibility of pneumonia. Linear dense opacity within the shadow suggests bowel herniation.
Answer 2: CT thorax demonstrates herniation of omentum and transverse colon through foramen of Morgagni on the right side and herniation of omentum on the left side. Diagnosis is bilateral Morgagni hernia.
DISCUSSION
Congenital Morgagni hernia (CMH) is rare, constituting roughly 2% of all congenital diaphragmatic hernias.[1] Herniation of abdominal content occurs through anterolateral or triangular parasternal gaps in the diaphragm.[2] This mostly occurs on the right side though they can rarely occur on the left or bilaterally.[3] They are generally asymptomatic and incidentally found during an unrelated diagnostic workup.[4] Berman et al.[5] treated only 18 cases of CMH over a period of 40 years and Pokorny et al.[6] reported only four cases of CMH over a period of 25 years. Cigdem et al. treated 16 cases of CMH over a period of 23 years.[7]
Giovanni Battista Morgagni, an Italian anatomist, first described the herniation of abdominal contents through the sternochondral triangles in 1769 based on cadaver observation.[8] Later, in 1828, Larrey described a surgical approach to the pericardial sac through these same triangles. The costochondral triangles have been referred to as the foramen of Morgagni on the right and the space of Larrey on the left. They form when the pars sternalis and a costochondral arch fuse and close around the internal thoracic artery as it becomes the superior epigastric artery. Occasionally, these spaces do not fully close and allow for the herniation of abdominal contents into the thorax.[2,9]
Morgagni hernias can be diagnosed during any period of life including prenatal period.[10] About 90% of these hernias occur on the right side of the sternum and 8% on the left.[11] Bilateral hernia makes up 2% of all Morgagni hernias. The hernias most frequently contain omental fat and transverse colon. They rarely contain liver or stomach.[12] Occasionally herniation may occur into the pericardial cavity resulting in serious cardiorespiratory compromise.[13,14] In adults, Morgagni hernia is also associated with obesity, trauma, weight lifting, or other causes of increased intraabdominal pressure. Our patient was a head load worker and this can be a predisposing factor. In the pediatric age group, the presentation of CMH is variable and nonspecific. Usually, the presentation is that of recurrent chest infection and rarely may present with gastrointestinal symptoms. Our patient also reported with respiratory symptoms rather than gastrointestinal symptoms. Majority of patients suffered repeated attacks of chest infections and received several courses of antibiotics. Some of them were hospitalized several times.
There is an increased risk of associated anomalies with CMH, with a variable incidence ranging from 34% to 50%.[3] One study reported as high as 78.3% associated anomalies in CMH[4] including 34.8% congenital heart disease. Atrial septal defect and ventricular septal defect were the most common associated heart defects. This, however, did not influence the final outcome and had no effect on the overall morbidity. An interesting association was that of CMH and Down's syndrome. In a collective series of 46 children with Morgagni hernia, 16 (34.8%) of them had Down's syndrome.[15] Cigdem et al. in a series of 16 patients with CMH seen over a period of 23 years reported a 31.25% incidence of Down's syndrome.[7] Other rare clinical associations of Morgagni hernia are pulmonary hypoplasia, hypoplasia of the left ventricle, gastric volvulus, midgut volvulus, and bilateral renal hypertrophy. Diagnosis of diaphragmatic hernias is easily made with chest radiographs, ultrasound (US), or CT. Chest radiography often requires anteroposterior images to evaluate hernia severity and lateral images to evaluate hernia location. Images can vary depending on the contents of the hernia. Solid viscera protruding through the hernia may show an opaque hemithorax with or without mediastinal shift. Hollow viscera are often present as loops of bowel within the thorax. An anterior medial mass on chest radiography can be suggestive of a Morgagni hernia. Radiological differential diagnoses include pneumonia, atelectasis, diaphragmatic eventration, mediastinal lipoma, liposarcoma, abscess, and pleuropericardial cyst.[16]
Computed tomography can be used to confirm a suspected diaphragmatic hernia. Multiphase CT can demonstrate the diaphragm and the organs that herniate through it. Omental vessels can be visualized in some diaphragmatic hernias and can help differentiate it from lipomas or liposarcomas. Intravenous contrast can help enhance these vessels and confirm a diagnosis.[12]
US is helpful in assessing diaphragmatic hernias that contain solid viscera. Hepatic echotexture and color Doppler sonogram can confirm liver in thorax.[17] Hernias that contain hollow viscera can be more difficult to evaluate with US. Air in the bowels and lungs, as well as rib shadowing, can often distort the images and make them difficult to interpret.[12]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Torfs CP, Curry CJ, Bateson TF, Honoré LH. A population-based study of congenital diaphragmatic hernia. Teratology. 1992;46:555–65. doi: 10.1002/tera.1420460605. [DOI] [PubMed] [Google Scholar]
- 2.Sandstrom CK, Stern EJ. Diaphragmatic hernias: A spectrum of radiographic appearances. Curr Probl Diagn Radiol. 2011;40:95–115. doi: 10.1067/j.cpradiol.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 3.Al-Salem AH, Zamakhshary M, Al Mohaidly M, Al-Qahtani A, Abdulla MR, Naga MI. Congenital Morgagni's hernia: A national multicenter study. J Pediatr Surg. 2014;49:503–7. doi: 10.1016/j.jpedsurg.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 4.Al-Salem AH. Congenital hernia of Morgagni in infants and children. J Pediatr Surg. 2007;42:1539–43. doi: 10.1016/j.jpedsurg.2007.04.033. [DOI] [PubMed] [Google Scholar]
- 5.Berman L, Stringer D, Ein SH, Shandling B. The late-presenting pediatric Morgagni hernia: A benign condition. J Pediatr Surg. 1989;24:970–2. doi: 10.1016/s0022-3468(89)80193-9. [DOI] [PubMed] [Google Scholar]
- 6.Pokorny WJ, McGill CW, Harberg FJ. Morgagni hernias during infancy: Presentation and associated anomalies. J Pediatr Surg. 1984;19:394–7. doi: 10.1016/s0022-3468(84)80260-2. [DOI] [PubMed] [Google Scholar]
- 7.Cigdem MK, Onen A, Okur H, Otcu S. Associated malformations in Morgagni hernia. Pediatr Surg Int. 2007;23:1101–3. doi: 10.1007/s00383-007-2011-x. [DOI] [PubMed] [Google Scholar]
- 8.Morgagni GB. New York, USA: Hafner; 1960. The Seats and Causes of Diseases Investigated by Anatomy: In Five Books, Containing a Great Variety of Dissections, with Remarks. [Google Scholar]
- 9.Minneci PC, Deans KJ, Kim P, Mathisen DJ. Foramen of Morgagni hernia: Changes in diagnosis and treatment. Ann Thorac Surg. 2004;77:1956–9. doi: 10.1016/j.athoracsur.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 10.Garne E, Haeusler M, Barisic I, Gjergja R, Stoll C, Clementi M. Euroscan Study Group. Congenital diaphragmatic hernia: Evaluation of prenatal diagnosis in 20 European regions. Ultrasound Obstet Gynecol. 2002;19:329–33. doi: 10.1046/j.1469-0705.2002.00635.x. [DOI] [PubMed] [Google Scholar]
- 11.Nasr A, Fecteau A. Foramen of Morgagni hernia: Presentation and treatment. Thorac Surg Clin. 2009;19:463–8. doi: 10.1016/j.thorsurg.2009.08.010. [DOI] [PubMed] [Google Scholar]
- 12.Eren S, Ciris F. Diaphragmatic hernia: Diagnostic approaches with review of the literature. Eur J Radiol. 2005;54:448–59. doi: 10.1016/j.ejrad.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Pironi D, Palazzini G, Arcieri S, Candioli S, Manigrasso A, Panarese A, et al. Laparoscopic diagnosis and treatment of diaphragmatic Morgagni hernia. Case report and review of the literature. Ann Ital Chir. 2008;79:29–36. [PubMed] [Google Scholar]
- 14.Gucciardo L, Deprest J, Done' E, Van Mieghem T, Van de Velde M, Gratacos E, et al. Prediction of outcome in isolated congenital diaphragmatic hernia and its consequences for fetal therapy. Best Pract Res Clin Obstet Gynaecol. 2008;22:123–38. doi: 10.1016/j.bpobgyn.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Kubiak R, Platen C, Schmid E, Gruber R, Ludwig K, Rauh W. Delayed appearance of bilateral morgagni herniae in a child with Down's syndrome. Pediatr Surg Int. 1998;13:600–1. doi: 10.1007/s003830050414. [DOI] [PubMed] [Google Scholar]
- 16.Anthes TB, Thoongsuwan N, Karmy-Jones R. Morgagni hernia: CT findings. Curr Probl Diagn Radiol. 2003;32:135–6. doi: 10.1016/s0363-0188(02)00007-5. [DOI] [PubMed] [Google Scholar]
- 17.Taylor GA, Atalabi OM, Estroff JA. Imaging of congenital diaphragmatic hernias. Pediatr Radiol. 2009;39:1–16. doi: 10.1007/s00247-008-0917-7. [DOI] [PubMed] [Google Scholar]


