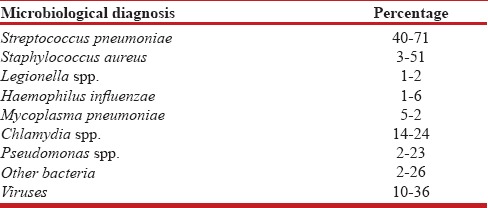
Pneumonia can be defined as inflammation of lung parenchyma occurring usually secondary to infection. It is one of the leading causes of morbidity in general population as well as in hospitalized patients. It had been rightly referred to as “Captain of the Men of Death” by Sir William Osler in the past as it is still a common cause of significant mortality in a select group of patients. There are varied spectrums of presentation of pneumonia depending on the setting in which it occurs. Likewise, causative microorganisms may also vary depending on the setting. Community-acquired pneumonia (CAP) is a special subgroup occurring outside health-care facility settings and is caused by typical and atypical pathogens [Table 1].[1]
Table 1.
Worldwide etiology of community-acquired pneumonia
This issue of Lung India includes two original studies about the assessment of CAP with a special emphasis on its etiological workup.
Para et al. have studied microbial etiology of hospitalized adults with CAP in a tertiary health-care facility in Kashmir.[2] They have aimed to comprehensively identify both typical and atypical organisms associated with CAP with the help of blood and sputum culture, urinary antigen for pneumococcus and legionella, serology for mycoplasma and chlamydia, and realtime reverse transcriptase-polymerase chain reaction for influenza viruses.
In this study, among typical CAP microbial agents, Streptococcus pneumoniae was the most predominant organism. Klebsiella pneumoniae, methicillinresistant Staphylococcus aureus, Pseudomonas aeruginosa, methicillinsensitive S. aureus, and Acinetobacter spp. were recovered in a small subgroup of patients. Among atypical organisms, Legionella pneumophila and influenza viruses were most prominent, while Mycoplasma pneumoniae, Chlamydia pneumonia, Mycobacterium tuberculosis, and mixed pathogens were present in some patients. As far as the study population is concerned, 44% of the participants were smokers with an age range of 18–93 years. Hypertension, chronic obstructive pulmonary disease (COPD), diabetes, chronic kidney disease, and heart failure were the main comorbid conditions present in the study population. It has been concluded in this study that infections by typical pathogens were more severe with higher CURB65 score at admission and more bilateral radiographic involvement as compared to atypical agents which were characterized by milder form of clinical disease.
In a study by Udwadia et al. from Mumbai, S. pneumoniae, C. pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, P. aeruginosa, Staphylococcus, and Salmonella typhi were typical organisms and M. pneumoniae and L. pneumophila were atypical pathogens isolated in their study population of CAP.[3]
In different studies across the world, S. pneumoniae has been found to be the most common organism identified in CAP, while in hospitalized patients, S. aureus, P. aeruginosa, and K. pneumoniae are commonly found.[4] S. aureus has been shown to complicate CAP in individuals with influenza viral pneumonia. K. pneumoniae occurs primarily in individuals with chronic alcoholism. P. aeruginosa is found in CAP occurring in patients with bronchiectasis or cystic fibrosis.
Overall, the recovery of microbiological agent in CAP is difficult due to a variety of reasons. Blood culture typically has a low sensitivity. On top of that, most of the patients presenting to health-care facilities are already on antibiotics, making it difficult to grow the organism. In addition, problem in culture of sputum and other respiratory specimens is related mainly to the quality of sample and contamination with mixed bacterial flora.
In another original study being published in this issue of Lung India, Kumar et al. from Mysore have tried to identify the etiology of CAP in children between 2 months and 16 years of age for atypical microbial pathogens.[5] Children not having an etiological diagnosis by conventional culture were subjected to immunofluorescence assay by Pneumoslide IgM test. The most common organism was M. pneumoniae which was found more frequently between 5 months and 2 years of age. The most common virus was respiratory syncytial virus. Mixed pathogens were identified in a few children. It could have been more informative for readers if authors would have presented microbiological data of children with CAP having etiological diagnosis of a typical agent by conventional culture.
Various factors including age, comorbid conditions such as COPD, diabetes, smoking, and alcohol use, and seasonality are important in influencing the clinical presentation and etiology of pneumonia.[1,6]
There are certain age-related differences in the presentation of CAP. In infants and small children, bacterial CAP tends to be the result of a previous viral infection. Sudden worsening of fever and patient's overall condition may occur in these children. It may also manifest as fever of unknown origin without other signs and symptoms of pneumonia, which is characteristic of pneumococcal CAP. In older children, S. pneumoniae followed by Mycoplasma and Chlamydial pneumonia are commonly found. A significant proportion of CAP (up to 40%) is the result of a mixed infection in children.[7]
Children requiring hospitalization are most likely to have infection caused by pneumococcus, H. influenzae or respiratory syncytial virus, and Mycoplasma. Worldwide, the use of pneumococcal, H. influenzae, and flu vaccines has reduced the frequency of childhood pneumonia. Further reduction possibly requires development of respiratory syncytial virus and M. pneumoniae vaccines.[8] It needs to be emphasized again and again that in developed countries like India, coverage of vaccinations is universally poor.
People in older age group have increased mortality due to CAP as compared to the younger age group and CURB 65 has been found to be less useful in people aged above 65 years. Overall, the microbiological patterns seen in the elderly people with CAP do not differ significantly from those of the younger people and here also S. pneumoniae and H. influenzae are predominant organisms. It has been convincingly found that COPD is a common predisposing condition for CAP, and besides frequent recovery of usual organisms in this setting, many others have pseudomonas and other more sinister forms of Gram-negative bacilli.[1]
Risk of severe pneumonia, empyema, and septicemia is linked with comorbidities. For patients with CAP, diabetes mellitus is one of the most common underlying diseases that may be associated with other comorbidities and complications. Initially, diabetic morbidity was linked to altered immune responses, but now it is proposed to be due to worsening of preexisting cardiovascular and kidney diseases. Similarly, alcoholism may be linked to more severe pneumonia which is associated with septicemia and mortality.[1,9,10]
Season may have a significant influence on occurrence of a particular pathogen. Swine flu has classically been associated with both seasonal and nonseasonal epidemic episodes.[11,12,13] In a study by Chen et al. using Pneumoslide IgM test in children, M. pneumoniae, parainfluenza viruses, and respiratory syncytial virus were found to be associated with seasonality. M. pneumoniae was higher in autumn, L. pneumophila in August and September, adenovirus in June, and influenza B virus in March than that in other months.[14]
From the above-mentioned fact, it can be concluded that overall microbiological etiology of CAP is more or less same throughout the world but may vary depending on the severity, setting, and patient-related factors, especially comorbidity. Therefore, comprehensive etiological workup of cases presenting with severe CAP is important. It should always be stressed upon that pneumonia can be potentially life-threatening, and knowledge of habitual pathogens and their resistance pattern represents the basis for optimal empirical treatment of CAP.
REFERENCES
- 1.Gupta D, Agarwal R, Aggarwal AN, Singh N, Mishra N, Khilnani GC, et al. Guidelines for diagnosis and management of community- and hospital-acquired pneumonia in adults: Joint ICS/NCCP(I) recommendations. Lung India. 2012;29:S27–62. doi: 10.4103/0970-2113.99248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Para RA, Fomda BA, Jan RA, Shah S, Koul PA. Microbial etiology in hospitalized North Indian adults with community-acquired pneumonia. Lung India. 2018;35:108–15. doi: 10.4103/lungindia.lungindia_288_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Udwadia ZF, Doshi AV, Joshi JM. Etiology of community acquired pneumonia in India. Eur Respir J. 2003;22:5445. [Google Scholar]
- 4.Shah BA, Singh G, Naik MA, Dhobi GN. Bacteriological and clinical profile of community acquired pneumonia in hospitalized patients. Lung India. 2010;27:54–7. doi: 10.4103/0970-2113.63606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar KJ, Chowdary KV, Usha HC, Kulkarni M, Manjunath VG. Etiology of community acquired pneumonia among children in India with special reference to atypical pathogens. Lung India. 2018;35:116–20. doi: 10.4103/lungindia.lungindia_391_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruiz M, Ewig S, Marcos MA, Martinez JA, Arancibia F, Mensa J, et al. Etiology of community acquired pneumonia: Impact of age, comorbidity, and severity. Am J Respir Crit Care Med. 1999;160:397–405. doi: 10.1164/ajrccm.160.2.9808045. [DOI] [PubMed] [Google Scholar]
- 7.García-Elorriaga G, Del Rey-Pineda G. Basic concepts on community-acquired bacterial pneumonia in pediatrics. [Last accessed on 2018 Feb 02];Pediatr Infect Dis. 2016 1:3. Available from: http://wwwpediatric-infectious-disease.imedpub.com/basic-concepts-on-communityacquired-bacterial-pneumonia-in-pediatrics.php?aid=8479 . [Google Scholar]
- 8.Nascimento-Carvalho CM. Etiology of childhood community acquired pneumonia and its implications for vaccination. Braz J Infect Dis. 2001;5:87–97. doi: 10.1590/s1413-86702001000200007. [DOI] [PubMed] [Google Scholar]
- 9.Falguera M, Pifarre R, Martin A, Sheikh A, Moreno A. Etiology and outcome of community-acquired pneumonia in patients with diabetes mellitus. Chest. 2005;128:3233–9. doi: 10.1378/chest.128.5.3233. [DOI] [PubMed] [Google Scholar]
- 10.Lim WS, Macfarlane JT, Boswell TC, Harrison TG, Rose D, Leinonen M, et al. Study of community acquired pneumonia aetiology (SCAPA) in adults admitted to hospital: Implications for management guidelines. Thorax. 2001;56:296–301. doi: 10.1136/thorax.56.4.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh V, Sharma BB, Patel V, Poonia S. Clinical profile of pneumonia and its association with rain wetting in patients admitted at a tertiary care institute during pandemic of influenza A (H1N1) pdm09 virus infection. Indian J Chest Dis Allied Sci. 2014;56:21–6. [PubMed] [Google Scholar]
- 12.Chowell G, Bertozzi SM, Colchero MA, Lopez-Gatell H, Alpuche-Aranda C, Hernandez M, et al. Severe respiratory disease concurrent with the circulation of H1N1 influenza. N Engl J Med. 2009;361:674–9. doi: 10.1056/NEJMoa0904023. [DOI] [PubMed] [Google Scholar]
- 13.Cilloniz C, Ewig S, Gabarrus A, Ferrer M, Puig de la Bella Casa J, Mensa J, et al. Seasonality of pathogens causing community-acquired pneumonia. Respirology. 2017;22:778–85. doi: 10.1111/resp.12978. [DOI] [PubMed] [Google Scholar]
- 14.Chen K, Jia R, Li L, Yang C, Shi Y. The aetiology of community associated pneumonia in children in Nanjing, China and aetiological patterns associated with age and season. BMC Public Health. 2015;15:113. doi: 10.1186/s12889-015-1422-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


