Abstract
Background. Dental diseases are among the most prevalent conditions worldwide, with universal access to dental care being one key to tackling them. Systematic quantification of inequalities in dental service utilization is needed to identify where these are most pronounced, assess factors underlying the inequalities, and evaluate changes in inequalities with time.
Objectives. To evaluate the presence and extent of inequalities in dental services utilization.
Search Methods. We performed a systematic review and meta-analysis by searching 3 electronic databases (MEDLINE, Embase, Cochrane Central Database), covering the period from January 2005 to April 2017.
Selection Criteria. We included observational studies investigating the association between regular dental service utilization and sex, ethnicity, place of living, educational or income or occupational position, or insurance coverage status. Two reviewers undertook independent screening of studies and made decisions by consensus.
Data Collection and Analysis. Our primary outcome was the presence and extent of inequalities in dental service utilization, measured as relative estimates (usually odds ratios [ORs]) comparing different (high and low utilization) groups. We performed random effects meta-analysis and subgroup analyses by region, and we used meta-regression to assess whether and how associations changed with time.
Main Results. A total of 117 studies met the inclusion criteria. On the basis of 7 830 810 participants, dental services utilization was lower in male than female participants (OR = 0.85; 95% confidence interval [CI] = 0.74, 0.95; P < .001); ethnic minorities or immigrants than ethnic majorities or natives (OR = 0.71; 95% CI = 0.59, 0.82; P < .001); those living in rural than those living in urban places (OR = 0.87; 95% CI = 0.76, 0.97; P = .011); those with lower than higher educational position (OR = 0.61; 95% CI = 0.55, 0.68; P < .001) or income (OR = 0.66; 95% CI = 0.54, 0.79; P < .001); and among those without insurance coverage status than those with such status (OR = 0.58; 95% CI = 0.49, 0.68; P < .001). Occupational status (OR = 0.95; 95% CI = 0.81, 1.09; P = .356) had no significant impact on utilization. The observed inequalities did not significantly change over the assessed 12-year period and were universally present.
Authors’ Conclusions. Inequalities in dental service utilization are both considerable and globally consistent.
Public Health Implications. The observed inequalities in dental services utilization can be assumed to significantly cause or aggravate existing dental health inequalities. Policymakers should address the physical, socioeconomic, or psychological causes underlying the inequalities in utilization.
PLAIN-LANGUAGE SUMMARY
The option to visit the dentist to receive preventive or therapeutic dental services should be available in an equal manner to everybody in a specific health service. In contrast, and building on 117 studies (with nearly 8 million participants) from various countries across the globe, we found that utilization of dental services is highly unequally distributed among different social, ethnic, economic, and educational groups. Utilization also differed according to where people lived (in cities or rurally). This unequal and unfair utilization of dental services is very likely causing or aggravating existing inequalities in dental health. Policymakers should address the reasons leading to this unequal and unfair utilization. Establishing a truly universal access to dental services might help all people—regardless of their status and where they live—to avoid or successfully manage dental diseases.
Dental diseases are among the most prevalent conditions worldwide, affecting all age groups, burdening billions of people with often irreversible loss of function, impaired aesthetics, and pain or discomfort.1 As with most noncommunicable conditions, dental diseases are largely behaviorally associated and preventable, which is why a growing focus has been on prevention or early detection and management.2–4
Although there is ongoing debate about the value of individual versus public health approaches toward tackling dental diseases,5–7 dental services remain a cornerstone for both prevention and (more so) management of dental diseases. Each year, billions of dollars are spent on dental services.8 Access to these services can be used to characterize the quality of dental care in different countries.9 Having a “universal, financially and physically accessible, high-quality primary care” system has been demanded as 1 key action to tackle noncommunicable diseases such as caries and periodontitis.4(p1) However, dental service utilization seems to be unequally distributed across populations and consumers.10–13
To date, no systematic efforts have been made to quantify the inequality in dental services utilization. Such quantification would be needed to identify countries with more pronounced inequalities, to assess possible factors underlying or moderating these inequalities, and to demonstrate whether inequalities have increased or decreased with time. All of these would be relevant for policymakers and researchers alike. We aimed to systematically assess, appraise, and quantify the inequalities in dental services utilization according to different social, demographic, and economic or educational characteristics.
METHODS
We conducted this review and meta-analysis according to established guidelines.14,15 The study protocol was registered after the initial screening stage (PROSPERO CRD42017064755). Any deviations from the protocol are described in the “Selection” section.
Search Strategy
We systematically screened 3 electronic databases (MEDLINE, Embase, and Cochrane Central Database) for articles published between January 2005 and April 2017. The search strategy was as unspecific as possible, with the expectation of poor indexing, and combined the outcome of interest (utilization OR utilisation OR demand OR utilize OR utilise OR visit) and the medical field of dentistry (dental OR dentist). We did not search for studies published before 2005 because we aimed to retrieve only recent and currently applicable evidence.
We excluded unpublished studies or gray literature because we expected them to contain insufficient reporting for our analysis. We considered articles such as reviews or editorials only when they contained original data. We only included studies published in English. We did not perform hand searches or cross-referencing. Two reviewers (S. M. R., F. S.) independently performed screening of titles or abstracts. We assessed all articles that were found to be potentially eligible in full text against the inclusion criteria.
Selection
Study design and variables.
We included prospective and retrospective cohort, case–control, and cross-sectional studies investigating the association between social, demographic, and socioeconomic or educational variables, and regular utilization of dental services. The independent variables needed to have been measured on individual or household rather than neighborhood level. For example, we excluded studies that reported on utilization by people living in a more versus a less deprived area without assessing the individual income status (except when the area was also useful as a marker for place of living; see “Data Extraction” section).
The independent variables were
Sex (male vs female);
Place of living (living rurally vs urban, or less urban vs highly urban or metropolitan);
Ethnicity (being from an ethnic minority, nonnative, or with limited language vs ethnic majority, native, high language capacities). Note that place of living and ethnicity had been added as independent variables after registration of the review because they were found to be relevant and reporting them here increased the comprehensiveness of our analysis. We also extracted data on inequalities by age as well as general and oral health status but did not include them within this review;
Own or parental educational position (low vs high);
Own or household income (low vs high, also including measures of wealth or financial capacity, such as being able to afford a car);
Occupational position (being unemployed vs employed, or being retired vs employed); and
Insurance coverage status (being uninsured vs insured, or poorly vs well insured).
We characterized regular utilization by regular or recent examination or preventive dental visits. We did not consider emergency visits or visits for specific dental procedures (surgical, orthodontic, prosthodontic treatment). We did not specify how exactly utilization was to be measured because we expected a large range of different definitions. We excluded studies reporting on interventions to influence this association. Studies needed to have used a multivariable model to evaluate the association between independent variables and regular utilization of dental services, accounting for a minimum of 3 of the former, and needed to have included an uncertainty estimate (e.g., 95% confidence interval [CI], P value, standard error) when reporting on this association. If studies presented both a multivariable model fitting these criteria and bivariable analyses, for example, we extracted estimates from only the multivariable model (see “Data Extraction” section).
Participants.
The participants were adults or children with permanent or primary teeth, or no teeth. We excluded studies investigating nonrepresentative groups (e.g., dental students, refugees, pregnant women, patients with severe physical or psychological illness or disability) in the interest of external validity; the same applied to studies with a sampling frame deemed nonrepresentative (such as areas of violent conflict or those affected by natural disasters).
We included only studies fulfilling all of these criteria. Two reviewers (S. M. R., F. S.) decided on inclusion and exclusion by consensus.
Data Extraction
We used a pretested and standardized spreadsheet-based data collection form. We collected study characteristics, including study type, place of conduct, year of conduct and publication; Human Development Index (HDI) of the respective country in the year of conduct (see later in this section); and sampling frame (national or subnational)—sample size, percentage of nonresponse, and percentage of regular utilization, and 2 reviewers (S. F. R., S. M. R.) independently extracted adjusted effect estimates from the most comprehensive report of each study. We contacted study authors if data were missing or for clarifications.
A number of decisions were needed during extraction. We decided study type according to study reporting rather than conduct (e.g., we regarded cross-sectional reports nested within cohort studies as cross-sectional). When 1 study reported on utilization in multiple dimensions of the same independent variable (such as different income categories), we extracted the estimate capturing the largest difference between categories to explore the extent of inequality.16 We extracted adjusted estimates from the model that included the largest number of relevant confounders.17 If the same survey or study was reported on in multiple articles, we included the article with the largest sample size to avoid unit-of-analysis issues. If a study reported on several waves of cross-sectional surveys, we extracted and, where feasible, pooled these by using fixed effects meta-analysis before entering them into our main meta-analysis. If a study reported on surveys in different countries, these were separated wherever possible, as we aimed to display country-specific inequality. We transformed estimates if needed, to provide identically directed input data for meta-analysis. Similarly, we transformed available uncertainty estimates into 95% CIs.17,18 If studies reported separately on different groups of participants from the same survey, we pooled data for meta-analysis.17
Most studies reported estimates by using odds ratios (ORs); only a small minority (15 of the total 117 included studies; see Results) used the risk ratio or prevalence ratio. Because transformation was not possible because of these being adjusted estimates, we entered all of them into 1 meta-analysis but performed sensitivity analyses, excluding those studies that used risk ratio or prevalence ratio instead of OR. The resulting changes in the pooled estimate were minimal (< 3%), however. We imputed effect estimates that were reported as being statistically nonsignificant without any further numerical values presented as recommended by the Cochrane collaboration,17 assuming the estimate to be “1” and the SE to be the mean of the reported SEs for each analysis. Not all studies reported on the year when they were conducted. We imputed missing years via the mean reported period between year of conduct and publication. When HDI19 was not available for all years for all countries, we used the last HDI reported. For 2 studies that sampled participants across Europe20 or across 66 countries worldwide,21 we calculated a mean HDI by using the simple mean of all HDIs from each country in the year of study conduct.
Quality Assessment
We assessed included studies for risk of bias by using the Newcastle–Ottawa Scale (NOS) modified for observational studies.22,23 We assessed the representativeness of the sample (Was the group representative for the target population?), whether national sampling was performed, whether the sample size and method were justified (or inclusive sampling performed), whether sampling bias was present (Were nonresponders reported on? Was nonresponse < 30% or otherwise justified?), whether the exposure was ascertained (Were reports based on interviews, questionnaires, or not described at all?), whether researchers controlled for confounders (because of our inclusion criteria, all studies adhered to this), whether the outcome assessment was robust (blinded external assessment, or via records or self-reports, or none reported assessment method), and whether statistical reporting was complete (because of our inclusion criteria, all studies scored full marks here). We did not exclude studies on the basis of this assessment, which mainly served to underpin our confidence in the yielded estimates.
Data Synthesis and Analysis
To pool estimates, we conducted inverse-generic meta-analysis with Comprehensive Meta-Analysis 2.2.064 (Biostat, Englewood, NJ). We performed 7 analyses, assessing the association of utilization and
sex,
ethnicity,
place of living,
educational position,
income position,
occupational position, and
insurance coverage status.
We assessed heterogeneity by using Cochrane’s Q and I2 statistics.24 Because heterogeneity was always found to be substantial (I2 > 90%), we used random effect models for meta-analysis. To explore the reasons for heterogeneity, we undertook both subgroup analyses (of regions) and mixed effect meta-regressions (on year of study conduct and HDI). For regions, we used the following classification, aiming to capture both regional and possible welfare regimen differences:
North America,
Europe except Scandinavia,
Scandinavia,
Southeast Asia,
high-income Asia,
high-income Oceania,
North Africa and the Middle East,
sub-Saharan Africa, and
South and Middle America.
Note that a large range of other classifications would have been available. In addition, we dichotomized the HDI into low HDI (< 0.80) and high HDI (≥ 0.80) for subgroup analyses. For meta-regression, we used the unrestricted maximum-likelihood method. We adjusted the level of significance for multiple testing; because we performed 14 meta-regression analyses, we regarded only P < .05/14 (i.e., < .004) as significant.17,18 Note that subgroup and meta-regression analysis were exploratory in nature (but had been planned a priori).
We evaluated publication bias or selective reporting by using funnel plots as well as Egger’s regression intercept test.25 Sensitivity analyses assessed the effects of possible publication or reporting bias.26
RESULTS
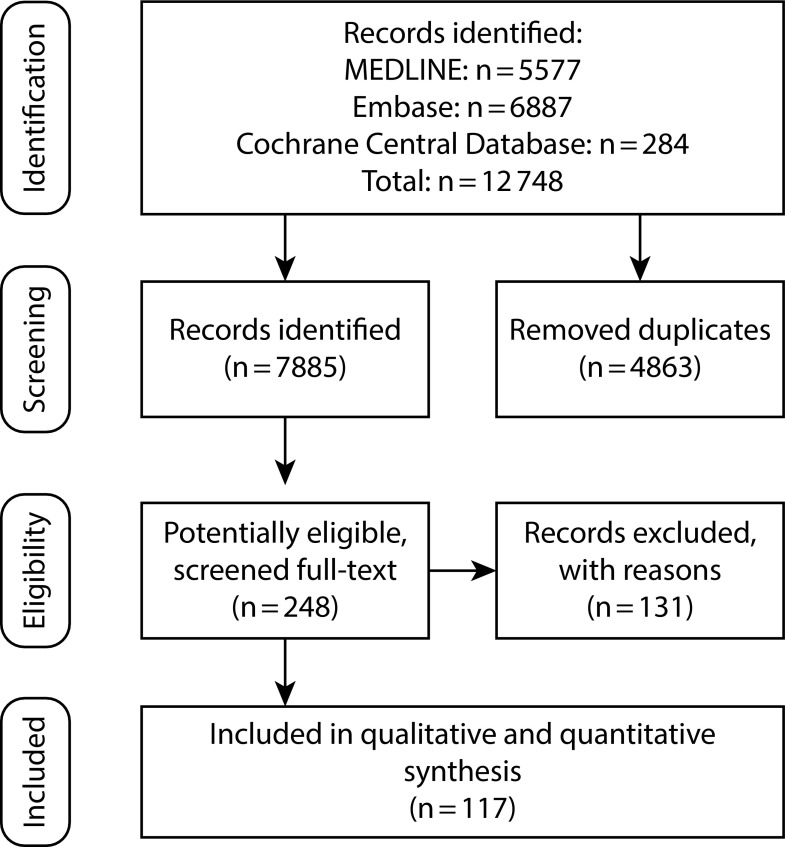
Our search yielded 12 748 records, with 248 articles being possibly eligible after review on abstract level (Figure 1). After full-text review, we excluded 131 studies and included 117 studies (Tables A and B, respectively, available as supplements to the online version of this article at http://www.ajph.org); the included studies involved a total of 7 830 810 participants. The mean (range) year of study conduct was 2005 (1990–2014) and the mean (range) year of publication was 2012 (2005–2017). The mean (range) sample size was 65 805 (190–3 175 584). Fifty-two studies had used a national sample. Studies had been performed in 31 countries; the most frequent were in the United States (n = 36 studies), Brazil (n = 12), and Australia (n = 10). Eighty-nine studies had been conducted in highly developed countries (HDI ≥ 0.8). Quality differed greatly among studies, with 18 studies having NOS scores less than 7, 39 with scores of 7 or 8, and 60 with scores of 9 or more (Table C, available as a supplement to the online version of this article at http://www.ajph.org). The lowest NOS score was 6, the highest was 10.
FIGURE 1—
Flowchart of the Database Search: January 2005 to April 2017
The association between the independent variables and dental services utilization is summarized according to different regions in Table 1. Details can be found in the next paragraphs and in the appendix (Figures A through N, available as supplements to the online version of this article at http://www.ajph.org).
TABLE 1—
Pooled Estimates From Random Effects Meta-Analysis, Expressing the Odds Ratio of Dental Services Utilization: January 2005 to April 2017
| Male Sex (Ref: Female) |
Minority Ethnicity, Nonnative (Ref: Majority Ethnicity, Native) |
Rural Place of Living (Ref: Urban) |
Lower Educational Position (Ref: Higher) |
Lower Income (Ref: Higher) |
Lower Occupational Position (Ref: Higher) |
Uninsured or Poor Insurance Status (Ref: Higher, Fully Insured) |
||||||||
| Region | OR (95% CI) | No. of Studies | OR (95% CI) | No. of Studies | OR (95% CI) | No. of Studies | OR (95% CI) | No. of Studies | OR (95% CI) | No. of Studies | OR (95% CI) | No. of Studies | OR (95% CI) | No. of Studies |
| Central America | 0.77 (0.42, 1.12) | 3 | NA | NA | 0.71 (0.51, 0.91) | 1 | 0.38 (0.25, 0.51) | 1 | 0.77 (0.43, 1.11) | 1 | 0.78 (0.46, 1.10) | 1 | ||
| Europe (excluding Scandinavia) | 0.83 (0.73, 0.93) | 10 | 0.89 (0.54, 1.25) | 2 | 0.79 (0.74, 0.85) | 5 | 0.55 (0.49, 0.60) | 10 | 0.81 (0.62, 1.01) | 8 | 0.91 (0.84, 0.97) | 1 | 0.52 (0.00, 1.11) | 3 |
| High-income Asia | 0.99 (0.97, 1.01) | 3 | NA | NA | 0.32 (0.32, 0.32) | 3 | 0.75 (0.39, 1.12) | 3 | 0.87 (0.49, 1.25) | 3 | NA | |||
| High-income Oceania | 0.80 (0.69, 0.90) | 9 | 0.87 (0.61, 1.13) | 2 | 1.04 (0.60, 1.48) | 2 | 0.48 (0.44, 0.51) | 4 | 0.73 (0.67, 0.85) | 8 | NA | 0.64 (0.53, 0.76) | 9 | |
| North Africa and Middle East | 0.90 (0.77, 1.03) | 5 | NA | 0.97 (0.86, 1.08) | 1 | 0.63 (0.51, 0.76) | 4 | 0.70 (0.57, 0.83) | 1 | 0.99 (0.87, 1.11) | 1 | 0.46 (0.22, 0.70) | 2 | |
| North America | 0.73 (0.67, 0.79) | 23 | 0.64 (0.58, 0.69) | 33 | 0.83 (0.76, 0.89) | 11 | 0.42 (0.40, 0.43) | 30 | 0.59 (0.52, 0.65) | 36 | 1.09 (0.91, 1.27) | 7 | 0.55 (0.48, 0.62) | 32 |
| Scandinavia | 0.67 (0.52, 0.82) | 10 | 0.53 (0.35, 0.71) | 6 | NA | 0.51 (0.50, 0.52) | 8 | 0.47 (0.18, 0.76) | 6 | 0.88 (0.72, 1.05) | 3 | NA | ||
| South and Middle America | 0.85 (0.79, 0.91) | 7 | 0.94 (0.92, 0.96) | 2 | 0.79 (0.33, 1.25) | 2 | 0.6 (0.58, 0.62) | 11 | 0.79 (0.22, 1.38) | 11 | NA | 0.70 (0.57, 0.83) | 1 | |
| Southeast Asia | 0.89 (0.69, 1.09) | 4 | 2.69 (0.97, 4.41) | 1 | 1.04 (0.60, 1.48) | 3 | 0.97 (0.79, 1.15) | 2 | 0.45 (0.23, 0.67) | 3 | 0.95 (0.73, 1.17) | 1 | 0.63 (0.61, 0.65) | 2 |
| Sub-Saharan Africa | 0.89 (0.45, 1.33) | 1 | 4.24 (1.39, 7.09) | 1 | NA | 0.47 (0.23, 0.71) | 1 | 0.79 (0.34, 1.25) | 2 | NA | 0.23 (0.13, 0.33) | 1 | ||
| Total | 0.85 (0.74, 0.95) | 77 | 0.71 (0.59, 0.82) | 47 | 0.87 (0.76, 0.97) | 25 | 0.61 (0.55, 0.68) | 76 | 0.66 (0.54, 0.79) | 81 | 0.95 (0.81, 1.09) | 18 | 0.58 (0.49, 0.68) | 52 |
Note. CI = confidence interval; NA = not applicable; OR = odds ratio.
According to 77 studies, male participants showed significantly lower utilization than female participants (Figure A, available as a supplement to the online version of this article at http://www.ajph.org). Inequality was not significantly different between low-HDI (n = 22) and high-HDI countries (n = 55; P = .05) and it was largely consistent across regions (inequality was absent in high-income Asia, but this was based on only a few studies). Inequality did not significantly change with time (P = .008), and it was not significantly associated with HDI (P = .04). Funnel plot analysis (Figure B, available as a supplement to the online version of this article at http://www.ajph.org) and statistical evaluation (Egger’s P < .02) indicated publication bias, but adjusting for this did not affect the synthesized estimate.
On the basis of 47 studies, those from ethnic minorities or with immigration or nonnative status had significantly lower utilization (Figure C, available as a supplement to the online version of this article at http://www.ajph.org). Inequality was present in high-HDI countries (n = 43; OR = 0.65; 95% CI = 0.57, 0.73), where it was consistent, but not low-HDI countries (n = 4; OR = 1.18; 95% CI = 0.67, 1.67). The estimate was stable with time (P = .80). Inequality was greater in countries with a higher HDI (P = .004). Both funnel plot analysis (Figure D, available as a supplement to the online version of this article at http://www.ajph.org) and statistical evaluation (Egger’s P < .02) indicated publication bias; however, adjusting for it only minimally changed the estimate (OR = 0.71; 95% CI = 0.59, 0.82).
According to 25 studies, individuals from rural places showed significantly lower utilization than those from urban areas (Figure E, available as a supplement to the online version of this article at http://www.ajph.org). Inequality was significantly lower in low-HDI (n = 6) than high-HDI countries (n = 19; P < .001). Inequality was not associated with the year of study conduct (P = .37) or HDI (P = .05). Funnel plot analysis (Figure F, available as a supplement to the online version of this article at http://www.ajph.org) found publication bias, but statistical evaluation did not (Egger’s P = .33). Adjusting the estimate accordingly increased the OR to 0.94 (95% CI = 0.83, 1.04)—that is, the association was not significant any longer.
On the basis of 76 studies, we found significantly lower utilization in those with lower educational position (Figure G, available as a supplement to the online version of this article at http://www.ajph.org). This was consistent across the globe, without significant differences between low-HDI (n = 19) and high-HDI countries (n = 57; P = .59). However, in Southeast Asia and Scandinavia, inequalities were significantly lower than in Western Europe or North America. Inequality was not significantly associated with when a study was conducted (P = .04) or HDI (P = .85). Publication bias was indicated by funnel plot analysis (Figure H, available as a supplement to the online version of this article at http://www.ajph.org), and also statistically (Egger’s P < .001), but adjusting for this did not affect the synthesized estimate.
On the basis of 81 studies, we found significantly lower utilization in those with lower income (Figure I, available as a supplement to the online version of this article at http://www.ajph.org) and significant differences across the globe (P < .001). Notably, inequality was significantly higher in North America and Southeast Asia than in Europe and high-income Oceania. However, there was no significant difference between low-HDI (n = 19) and high-HDI countries (n = 62; P = .08). The estimate was not associated with when a study was conducted (P = .965) or HDI (P = .78). Publication bias was indicated by funnel plot analysis (Figure J, available as a supplement to the online version of this article at http://www.ajph.org) but not by statistical evaluation (Egger’s P = .38). Adjusting the estimate accordingly increased the OR to 0.74 (95% CI = 0.62, 0.85).
According to 18 studies, we found no significant association between occupational position and utilization (Figure K, available as a supplement to the online version of this article at http://www.ajph.org). Again, this was consistent across most countries and regions, without significant differences between low HDI (n = 3) and high HDI (n = 15; P = .94). The inequality increased in recent years (P < .001), but it was not associated with HDI (P = .24). Publication bias was detected not by funnel plot analysis (Figure L, available as a supplement to the online version of this article at http://www.ajph.org) but by statistical evaluation (Egger’s P < .01); adjusting for this did not affect the synthesized estimate.
According to 52 studies, those without insurance coverage showed significantly lower utilization (Figure M, available as a supplement to the online version of this article at http://www.ajph.org). Again, this was consistent across most countries and regions, without significant differences between low-HDI (n = 7) and high-HDI countries (n = 45; P = .97). The degree of inequality did not change significantly in recent years (P = .02), and it was not associated with HDI (P = .93). There was indication of publication bias via funnel plot analysis (Figure N, available as a supplement to the online version of this article at http://www.ajph.org), but not statistical evaluation (Egger’s P = .33). Adjusting the estimate accordingly increased the OR to 0.64 (95% CI = 0.44, 0.82).
DISCUSSION
Regular utilization of dental services is associated with lower dental caries experience, more retained teeth, and better subjective oral health, even after adjustment for a large range of confounders.27–29 Given what is spent on dental services globally,8 we might expect universal and equal access at least in high-income countries. However, according to our review, services are utilized highly unequally. On the basis of more than 7 million participants, we found compelling evidence for persistent inequalities of dental services utilization across the globe. Men, individuals from ethnic minorities or immigrants, those from lower socio-educational or economic background, and those without (or with only limited) insurance coverage consistently showed lower utilization.
Strengths and Limitations
This review has a number of strengths. Data collection was performed systematically, yielding a large set of studies on more than 7 million participants. Moreover, many of the included studies had used national samples; the included populations are thus often representative for a whole country at the time of conducting the study. As a result, our findings were relatively robust, with inequalities largely being consistent across the globe, across the studies, and across time. It is thus unlikely that newer studies will greatly change the synthesized estimates (unless, of course, the “true” inequality changes).
The study also has a number of limitations. First, a large range of factors beyond those evaluated is affected by inequality or is even underlying the observed differences in utilization. Dental anxiety, for example, has been found to be closely associated with educational position. In line with this, the performed exploratory (subgroup or meta-regression) analyses are clearly unable to disentangle the complex network of factors underlying the observed inequalities. They merely highlight possible risk factors and patterns. For further analysis, individual participant data meta-analysis might be helpful. We also did not report on other inequalities of utilization (e.g., according to age or general health status), although we have collected such data. Briefly, we found a lower utilization in younger versus older children and those who are generally not healthy versus those who are healthy. No detailed reporting is done here, although these factors need to be considered for understanding the resulting overall unequal utilization.
Second, we assessed only the extent of inequality, comparing the highest and lowest utilization category. We assessed no absolute estimates of inequality, and we were also not able to assess any gradients in inequality. Moreover, we used a large range of definitions for regular utilization, and the same applies to the large number of different categories (e.g., educational position or income) compared. These factors have likely contributed to the high heterogeneity within our meta-analysis. Third, we included only studies in English. Given that we found a large, consistent body of data, we do not assume this to have necessarily biased our findings. However, some analyses seemed to suffer from publication bias (adjusting for this only limitedly changed our findings), which might have been lower if non–English-language publications had been included. Last, the majority of included studies stemmed from richer countries (nearly one third came from the United States). Our findings should thus not easily be transferred to other countries (e.g., African or Central Asian countries).
Comparison With Other Studies
It was remarkable to see similar or even higher inequalities in many richer versus middle- or low-income countries; a greater HDI does not necessarily come with lower inequality. For example, inequalities by ethnicity, place of living, or insurance coverage status were higher in most of Europe and, particularly, North America (which largely meant the United States) than in Northern Africa and the Middle East or Latin America (data from Africa were scarce). Studies from Scandinavia notably found lower inequalities for education, for example, especially in comparison with North America. This highlights the possible impact of the specific welfare regimens in place: in countries with near-universal (public) coverage (such as most of Scandinavia), inequalities in utilization are more limited than in countries with significant or total private coverage. This is in line with previous findings of redistributive and universal welfare policies leading to more equal access (and possibly better oral health).30,31 In countries with high inequality, expanding dental services at no or low private (out-of-pocket) costs should be considered to increase utilization.32,33
Inequalities by both sociodemographic and educational or economic position were evident. There are a number of explanatory pathways for this finding. First, education and economic position, jointly and often interlinked, determine an individual’s financial means. In countries where dental care does not come for free, this will have an impact on utilization, especially when one considers the potentially catastrophic impact of dental expenses.34 This, again, calls for a universal but also mandatory coverage of dental care (at least to a certain extent), but it also highlights the need to tackle the underlying social determinants of inequality.7,35 Education, in addition, is also closely linked with health literacy and oral health beneficial behavior (such as regular tooth brushing or a healthy diet). Thus, underutilization might be the result of lacking knowledge, which is consequently perpetuated given that oral health education is provided in dental settings in many countries.27 There seems to be the need for oral health awareness on a wider setting or public health level,36 possibly also involving other providers than dentists.37 Given that many risk factors for dental diseases (e.g., sugar intake or smoking) are shared by other diseases (e.g., obesity, diabetes, or cancer), such education might have benefits beyond oral or dental health.38
That the place of living affected utilization might be the result of spatial (i.e., physical) access (e.g., lack of transportation) but could also indicate a limited availability of dental services in rural areas. The observed inequality is a further argument for spatially specific health services planning 39,40 Notably, inequality according to place of living was only found in high-HDI countries. In less-developed countries, it is likely that access is in any case limited, with spatial factors being less important.
Interpretation and Implications
Within the limitations of this review and the therein included studies, but based on more than 7 million participants, dental services utilization was lower in male participants than female participants; ethnic minorities or immigrants; those living rurally versus urban; those with lower versus higher education, or income; and those without (or with poor) insurance coverage status. Inequalities were large and globally consistent, limiting access to care for billions of people.
HUMNA PARTICIPANT PROTECTION
No institutional review board approval was needed because it was a secondary data analysis that used aggregate data.
REFERENCES
- 1.Marcenes W, Kassebaum NJ, Bernabé E et al. Global burden of oral conditions in 1990–2010: a systematic analysis. J Dent Res. 2013;92(7):592–597. doi: 10.1177/0022034513490168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bull World Health Organ. 2005;83(9):661–669. [PMC free article] [PubMed] [Google Scholar]
- 3.Petersen PE. World Health Organization global policy for improvement of oral health—World Health Assembly 2007. Int Dent J. 2008;58(3):115–121. doi: 10.1111/j.1875-595x.2008.tb00185.x. [DOI] [PubMed] [Google Scholar]
- 4.Di Cesare M, Khang YH, Asaria P et al. Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381(9866):585–597. doi: 10.1016/S0140-6736(12)61851-0. [DOI] [PubMed] [Google Scholar]
- 5.Batchelor P, Sheiham A. The limitations of a “high-risk” approach for the prevention of dental caries. Community Dent Oral Epidemiol. 2002;30(4):302–312. doi: 10.1034/j.1600-0528.2002.00057.x. [DOI] [PubMed] [Google Scholar]
- 6.Sheiham A, Alexander D, Cohen L et al. Global oral health inequalities: task group—implementation and delivery of oral health strategies. Adv Dent Res. 2011;23(2):259–267. doi: 10.1177/0022034511402084. [DOI] [PubMed] [Google Scholar]
- 7.Marmot M, Bell R. Social determinants and dental health. Adv Dent Res. 2011;23(2):201–206. doi: 10.1177/0022034511402079. [DOI] [PubMed] [Google Scholar]
- 8.Listl S, Galloway J, Mossey PA, Marcenes W. Global economic impact of dental diseases. J Dent Res. 2015;94(10):1355–1361. doi: 10.1177/0022034515602879. [DOI] [PubMed] [Google Scholar]
- 9.Campbell SM, Roland MO, Buetow SA. Defining quality of care. Soc Sci Med. 2000;51(11):1611–1625. doi: 10.1016/s0277-9536(00)00057-5. [DOI] [PubMed] [Google Scholar]
- 10.Listl S. Cost-related dental non-attendance in older adulthood: evidence from eleven European countries and Israel. Gerodontology. 2016;33(2):253–259. doi: 10.1111/ger.12151. [DOI] [PubMed] [Google Scholar]
- 11.Listl S. Income-related inequalities in dental service utilization by Europeans aged 50+ J Dent Res. 2011;90(6):717–723. doi: 10.1177/0022034511399907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Listl S. Countries with public dental care coverage have lower social inequalities in the use of dental services than countries without such coverage. J Evid Based Dent Pract. 2015;15(1):41–42. doi: 10.1016/j.jebdp.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 13.Listl S. Inequalities in dental attendance throughout the life-course. J Dent Res. 2012;91(7 suppl):91S–97S. doi: 10.1177/0022034512447953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Welch V, Petticrew M, Tugwell P et al. PRISMA-Equity 2012 Extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med. 2012;9(10):e1001333. doi: 10.1371/journal.pmed.1001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conway DI, Quarrell I, McCall DR, Gilmour H, Bedi R, Macpherson LM. Dental caries in 5-year-old children attending multi-ethnic schools in Greater Glasgow—the impact of ethnic background and levels of deprivation. Community Dent Health. 2007;24(3):161–165. [PubMed] [Google Scholar]
- 17.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.10. London, England: The Cochrane Collaboration; 2011. [Google Scholar]
- 18.Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ. 2003;326(7382):219. doi: 10.1136/bmj.326.7382.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. Human Development Reports. 2016. Available at: http://hdr.undp.org/en/data/map. Accessed May 14, 2016.
- 20.Tchicaya A, Lorentz N. Socioeconomic inequalities in the non-use of dental care in Europe. Int J Equity Health. 2014;13(1):7. doi: 10.1186/1475-9276-13-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhandari B, Newton JT, Bernabe E. Income inequality and use of dental services in 66 countries. J Dent Res. 2015;94(8):1048–1054. doi: 10.1177/0022034515586960. [DOI] [PubMed] [Google Scholar]
- 22.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. 2009. Available at: http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf. Accessed May 14, 2016.
- 23.Hanioka T, Ojima M, Tanaka K, Matsuo K, Sato F, Tanaka H. Causal assessment of smoking and tooth loss: a systematic review of observational studies. BMC Public Health. 2011;11(1):221. doi: 10.1186/1471-2458-11-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 25.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 27.Sanders AE, Spencer AJ, Slade GD. Evaluating the role of dental behaviour in oral health inequalities. Community Dent Oral Epidemiol. 2006;34(1):71–79. doi: 10.1111/j.1600-0528.2006.00261.x. [DOI] [PubMed] [Google Scholar]
- 28.Thomson WM, Williams SM, Broadbent JM, Poulton R, Locker D. Long-term dental visiting patterns and adult oral health. J Dent Res. 2010;89(3):307–311. doi: 10.1177/0022034509356779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilbert GH, Foerster U, Dolan TA, Duncan RP, Ringelberg ML. Twenty-four month coronal caries incidence: the role of dental care and race. Caries Res. 2000;34(5):367–379. doi: 10.1159/000016611. [DOI] [PubMed] [Google Scholar]
- 30.Guarnizo-Herreño CC, Tsakos G, Sheiham A, Watt RG. Oral health and welfare state regimes: a cross-national analysis of European countries. Eur J Oral Sci. 2013;121(3 pt 1):169–175. doi: 10.1111/eos.12049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanders AE, Slade GD, John MT et al. A cross-national comparison of income gradients in oral health quality of life in four welfare states: application of the Korpi and Palme typology. J Epidemiol Community Health. 2009;63(7):569–574. doi: 10.1136/jech.2008.083238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bailey SR, Marino M, Hoopes M et al. Healthcare utilization after a Children’s Health Insurance Program Expansion in Oregon. Matern Child Health J. 2016;20(5):946–954. doi: 10.1007/s10995-016-1971-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brickhouse TH, Rozier RG, Slade GD. Effects of enrollment in Medicaid versus the state Children’s Health Insurance Program on kindergarten children’s untreated dental caries. Am J Public Health. 2008;98(5):876–881. doi: 10.2105/AJPH.2007.111468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bernabé E, Masood M, Vujicic M. The impact of out-of-pocket payments for dental care on household finances in low and middle income countries. BMC Public Health. 2017;17(1):109. doi: 10.1186/s12889-017-4042-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Marmot M. Social determinants of health inequalities. Lancet. 2005;365(9464):1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 36.Niederman R, Huang SS, Trescher A-L, Listl S. Getting the incentives right: improving oral health equity with universal school-based caries prevention. Am J Public Health. 2017;107(suppl 1):S50–S55. doi: 10.2105/AJPH.2016.303614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yee A, McGlaston K, Restuccia R. How dental therapists can address the social and racial disparities in access to care. Am J Public Health. 2017;107(suppl 1):S28–S29. doi: 10.2105/AJPH.2016.303641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sheiham A, Watt RG. The Common Risk Factor Approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. 2000;28(6):399–406. doi: 10.1034/j.1600-0528.2000.028006399.x. [DOI] [PubMed] [Google Scholar]
- 39.Jäger R, van den Berg N, Hoffmann W, Jordan RA, Schwendicke F. Estimating future dental services’ demand and supply: a model for Northern Germany. Community Dent Oral Epidemiol. 2016;44(2):169–179. doi: 10.1111/cdoe.12202. [DOI] [PubMed] [Google Scholar]
- 40.Schwendicke F, Jager R, Hoffmann W, Jordan RA, van den Berg N. Estimating spatially specific demand and supply of dental services: a longitudinal comparison in Northern Germany. J Public Health Dent. 2016;76(4):269–275. doi: 10.1111/jphd.12142. [DOI] [PubMed] [Google Scholar]