Abstract
Background
Different health behaviors influence health and illness. Spiritual well-being is one of the most important aspects of health promotion. The aim of this study was to identify the association between spiritual behavior in relation to meditation, worship, and physical exercise during yoga with self-reported disease/illness among women of the Kailali district of Nepal.
Methods
This was a cross-sectional study with 453 randomly selected women in the Kailali district of Nepal within 1 municipality and 4 village development committees (VDC) using cluster sampling. We used a semi-structured interview to collect the data for selected respondents. Socioeconomics, lifestyle, self-care, and spiritual behavior variables were independent variables, and self-reported illness in the past year was a dependent variable. Descriptive statistics, chi square, hierarchical logistic regression for odds ratio, and 95% CI were used when appropriate.
Results
Study results showed that 89% of participants were from the rural area, 29.3% were housewives, 51.4% had no formal education, 43.2% used tobacco, 42.1% did yoga, and 16.9% engaged in regular worship. Self-reported illness was associated with safe toilet-using behavior, tobacco use, junk food consumption, yoga and regular exercise, worship, and regular sleeping habits. Comparing odds ratios and 95% CIs, the women who had safe toilet behavior and did not use tobacco were 2.48 (1.98–7.98) and 2.86 (1.74–7.34) times less likely to be ill, respectively. Likewise, women who consumed junk food; did not regularly exercise, meditate, or worship; and had irregular sleeping habits were 1.65 (1.32–4.61), 2.81(1.91–5.62), 2.56 (2.01–4.88), 4.56 (3.91–8.26), and 2.45 (2.12–5.03) times more likely to become ill, respectively.
Conclusion
Our study concludes that spiritual behavior is effective for better health and low risk for disease occurrence. A spiritual health policy and separate curriculum for basic education and medical education should be promoted globally, and further research is recommended.
Keywords: Spiritual behavior, Yoga, Worship, Healthy behavior, Junk food
INTRODUCTION
Individual behavior is a major factor in determining health and occurrence of disease or illness. Particularly, health status is influenced by lifestyle, food, drink [1], smoking [2], a safe environment, housing and sanitation [3], and, more importantly but less discussed, spiritual behavior [4,5]. There were >100 million deaths in the 20th century, and this number will be 10 times higher in the 21st century due to tobacco [6,7] and alcohol use [8]. There are no exact studies on the prevalence of junk food consumption, but it is a major risk factor for health [9,10]. The situation of specific lifestyles is different by age, sex, and region, but risk behaviors are less common in women due to their deep motivation for spirituality [11]. This is why life expectancy is higher for women than for men.
There are previous studies related to lifestyle in terms of health and disease. Danish adults with unhealthy lifestyles, including alcohol consumption, smoking, and irregular diet patterns, had worse mental and physical illness than those who did not [12]. Likewise, it has already been proven that smoking causes many diseases and disorders, alcohol accelerates many cardiovascular diseases, and junk foods are potential risk factors for malignancy. Physical exercise decreases the risk of disease, maintains good health, strengthens natural immunity [13], and increases lung capacity to reduce respiratory diseases like asthma [14]. Beyond the physical, mental, and social dynamics, humans have special characteristics of intellectual supremacy, kindness, dedication, patience, life goals, and love that improve health and well-being [15]. Due to spirituality, people pray, worship, meditate, and help others. The World Health Organization (WHO) now includes the spiritual dimension [16] of health, but there are not enough studies that include spirituality in health and medical research.
There is some empirical evidence of better health status with spiritual behavior. Oman et al. [17] explored four interpretations of how spirituality/religion influences health. The first is the “any pathway” interpretation, which considers that spirituality/religion can influence health through any of four pathways: health behaviors, social support, psychological states, and “psi” influences. The second interpretation, the “psychobiological” one, considers that spirituality/ religion influences health through psycho-neuro-immunological or psycho-neuro-endocrinological pathways beyond the benefits for health behaviors and social support. A third interpretation, the “super empirical” or “psi” interpretation, considers that spirituality/religion influences health through super-empirical pathways that accelerate healthy behaviors and psychological states. Finally, the “psycho-behavioral” interpretation stresses that spirituality/religion can influence health through various psychological conditions such as character, willpower, focused attention, and increased motivation.
Health and diseases are bodily states determined by many factors. Measurement of biomarkers cannot describe the status of overall health because there are other dimensions of health: social, mental, emotional, and spiritual. In other words, such conditions can be measured by their experiences. The power of women’s spirituality can transform their lives and relationship, and such a phenomenon would ultimately improve their family and social health [18]. To achieve spirituality, humans pray, worship, meditate, practice a simple and healthy lifestyle, and perform social service. There are very limited studies on spiritual behavior, particularly in women. The practice of spirituality is necessary from the grass-roots level and for health care providers [19,20]. Previous research explores the concept of spiritual dimensions but lacks specific behavior associated with illness. Nepal, particularly the Kailali district, is a multicultural area with no appropriate access to the modern health system and harbors many inequalities and unfriendly cultural practices for women’s health [21]. People in this area believe that alternative medicine is as effective as contemporary medicine [22], and one-quarter of the people are below the poverty line [23]. In the study area, people engage in classical yoga practice, physical exercise, and different indigenous health-seeking behaviors. All people can freely attend the yoga centers in the area. Particularly, adult and elderly people join these centers, and women are usually involved in daily worship in the morning and evening. Therefore, it is important to identify the association of illness status of women with their behavior and lifestyle. As a result, the factors responsible for health and illness could be explored, and the results might contribute to specific programs targeted to women. The aim of this study was to identify the association of spiritual behavior in relation to meditation, worship, and physical exercise with self-reported disease/illness among women of the Kailali district of Nepal.
MATERIALS AND METHODS
1. Study design and sampling
This was a community-based cross-sectional study conducted during January and February of 2015. More explicitly, it was descriptive, and some components were framed as analytical. Women in households composed the study unit. The sampling process was set up in two stages. The Kailali district of Nepal was the selected sub-area (village development committee [VDC] and municipality), which was the basic geographical unit and was selected randomly. The study area was divided into clusters 1 through 9. Available households in each cluster were selected by equal proportion sampling so that they would represent the characteristics of the whole community. In the last stage, one participant was selected from the sampling household. If there was more than one woman in a selected household, the oldest was selected, because spirituality is often better realized in those who are older [24]. Ethical approval was received from local authorities of the Kailali district, and verbal consent was obtained from the respondents. All respondents were requested to provide information voluntarily and were assured that they could withdraw at any time during the study.
2. Sampling strategies
The 3R strategy was applied in the sampling process: randomization of participant selection; representativeness by proper estimation of sample size; and reliable information through field researcher selection, training, and data collection with proper supervision.
3. Sampling frame
Households were selected from a list provided by the local government authority: the VDC household record list of the selected area. Cluster sampling was applied to include subgroups of the population in different locations, and women were selected from household rosters during the data collection time.
4. Sample size estimation
The sample size was estimated in two ways. One was 50% picked by choice from the general population, and the other was about 50% of the female population in the community. By formula, it can be calculated as follows:
where N is the sample size, the value of Z is 1.96, p is the percentage of total sample size, the standard choice is 50%, and C is the standard error (0.01). Hence, the sample size was 453.
5. Exclusion criteria
Women who had lived in the residential area for less than six months, households with no women, and women who did not want to participate in the study were excluded.
6. Recruitment of field researchers
The field researchers were screened and selected based on previous experience, academic soundness, and experience with field research. More consciously, the researchers were selected from people with health education backgrounds such as paramedics, nurses, and community health workers because they could more accurately analyze the information than general enumerators.
7. Setting of research tool
A semi-structured questionnaire was developed based on Pender et al.’s health promotional model [25], William C, health lifestyle theory [26], and some indigenous lifestyle behavior like yoga (meditation) and worship-related spiritual behavior obtained after consultation with key persons in the community.
8. Instrument and variables
Data were collected by field researchers using a questionnaire and field guidebook. The collected data were decoded, entered into Microsoft Excel, and then exported to SPSS. After that, data were cleaned and verified by a biostatistician and further analyzed by a researcher. There were four categories of independent variables: socio-demographic, lifestyle, self-care, and spiritual behavior. The dependent variable, illness status, was reported by the respondents.
9. Operational definitions of key variables
-
Self-reported illness
This is used to refer to a patient’s personal experience of disease [33]. Illness occurrence was self-reported in the past year as loss of regular work time due to any illness or being admitted to a hospital for anything other than injury or disability.
-
Junk food and availability in Nepal
There is a variety of junk foods in Nepal, categorized into two groups: snacks (noodles, cookies, Pauroti, Doughnuts, Numkins, Bhujia, chips, Kurkure Cheeseballs, etc.) and drinks (Slice, Coke, Fanta, Sprites, Horlicks, Viva Boosts, Chocos, Tang, etc.) [34].
The details about the physical exercise, Yoga/meditation, worship practice, sleeping habit and consumption of junk food have been presented in Table 1.
Table 1.
Operational definitions of special variables
| Variable | Definition | Reference | Response |
|---|---|---|---|
| Physical exercise | Physical exercise on a regular schedule either in the evening or morning, 30 minutes or more per day in no more than 2 sessions per day, during, before, or after meditation or yoga. | Siddiqui et al. (2010) [27] | Yes/No |
| Yoga/meditation | Meditation for 15 minutes or more per day and ≥3 months per year. | Prasad et al. (2011) [28] and mindfulness meditation method by University of Massachusetts Medical School [29] | Yes/No |
| Worship practice | Worship more than 20 minutes per day in no more than 2 sessions per day. | Salmoirago-Blotcher et al. (2011) [30] | Yes/No |
| Sleeping habit | Regular sleep every night and no reported sleep disturbances | Perry et al. (2013) [31] | Yes/No |
| Consumption of junk food | Use of ready-made foods more than once each day | Naeem (2012) [32] | Yes/No |
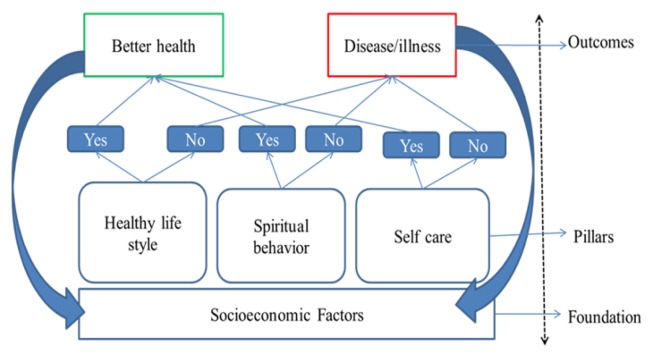
10. Research model
This research model was conceptualized on the foundation of Cockerham [26]’s health and lifestyle theory, Thomsen [35]’s 1998 concept of Spirituality in Medical Practice, and Moore et al. [36]’s 2012 meditation practice (Fig. 1).
Fig. 1.
Conceptual model of spiritual behavior and health.
11. Statistical test
Categorical variables are presented as frequency and percentage with the chi square test. Logistic regression was applied to show the associations between different variables and illness status, and a p-value less than 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 22.
12. Validity and reliability
The research tools were verified in a pilot study in a similar area in Baliya VDC Kailali. The sample size was determined by a scientific method, and the selection of field researchers, application of field guidebooks, and monitoring of the data collection process were done carefully. The data collection process was supervised to minimize bias, and related variables were checked for missing values and outliers. Likewise, the normality of the data was verified by observing a histogram, and the consistency of the data was verified using Cronbach’s alpha of appropriate variables. The study questionnaire was developed based on the theme of William C’s health lifestyle theory and Pender et al. [25]’s health promotion model and contextualized using key people and local experts.
RESULTS
For this study, the participants were 453 women with a mean age of 34.4 years. Among them, more than half were from rural areas and had no formal education. More than two-thirds had dwellings, and about one-third used tobacco and drank alcohol. Of the total women 21.1% regularly exercised with yoga; 17.0% engaged in regular worship, 42.1% used meditation, 34.6% had regular sleep habits, and 18.3% had undergone regular health check-ups in the past year. Safe toilet behavior, tobacco and junk food use, regular exercise, meditation, worship, and health checkups were significantly associated (p < 0.05) with self-reported illness (Table 2).
Table 2.
Descriptive status of the study and associations with reported disease by the respondents
| Major domains | Variables | Category | Disease/Illness (N = 453) | p-value | |
|---|---|---|---|---|---|
|
| |||||
| No (%) | Yes (%) | ||||
| Socioeconomic factors | Place of residence | Urban | 58 (65.2) | 31 (34.8) | 0.334 |
| Rural | 217 (59.6) | 147 (40.4) | |||
| Education | No formal | 134 (57.5) | 99 (42.5) | 0.112 | |
| Secondary | 93 (60.8) | 60 (39.2) | |||
| Higher | 48 (71.6) | 19 (28.4) | |||
| Occupation | Agriculture | 115 (60.8) | 74 (39.2) | 0.326 | |
| Job | 62 (64.5) | 34 (35.5) | |||
| Housewife | 155 (92.2) | 13 (7.8) | |||
| House structure | Relatively safe | 13 (61.9) | 8 (38.1) | 0.861 | |
| Improved | 76 (61.8) | 47 (38.2) | |||
| Dwelling | 186 (60.1) | 123 (39.9) | |||
| Type of floor | Mud | 245 (61.1) | 156 (38.9) | 0.633 | |
| Cement | 30 (57.7) | 22 (42.3) | |||
| Cooking fuel | LP/bio-gas | 44 (56.4) | 34 (43.6) | 0.267 | |
| Firewood and dung | 231 (61.6) | 144 (38.4) | |||
| Self care | Safe toilet | Yes | 37 (62.7) | 22 (37.3) | 0.009 |
| No | 156 (39.5) | 238 (61.5) | |||
| Source of drinking water | Tap water | 31 (55.4) | 25 (44.6) | 0.068 | |
| Tube well | 204 (59.8) | 137 (40.2) | |||
| River stream | 40 (71.4) | 16 (28.6) | |||
| Sleeping at regular time | Yes | 112 (71.3) | 45 (28.7) | <0.001 | |
| No | 163 (55.1) | 133 (44.9) | |||
| Health check-up last year | Yes | 57 (68.7) | 26 (31.3) | 0.062 | |
| No | 218 (58.9) | 152 (41.1) | |||
| Lifestyle factors | Drinking alcohol | No | 172 (59.3) | 118 (40.7) | 0.474 |
| Yes | 103 (63.2) | 60 (36.8) | |||
| Tobacco use | No | 168 (65.3) | 89 (34.7) | 0.005 | |
| Yes | 70 (35.7) | 126 (64.3) | |||
| Junk food (as main food) | No | 208 (66.2) | 106 (33.8) | <0.001 | |
| Yes | 67 (48.2) | 72 (51.8) | |||
| Spiritual behavior | Regular exercise before and after yoga/meditation | Yes | 78 (81.2) | 18 (18.8) | <0.001 |
| No | 197 (55.2) | 160 (44.8) | |||
| Regular yoga/meditation | Yes | 150 (78.4) | 41 (21.6) | <0.001 | |
| No | 121 (46.1) | 141 (53.9) | |||
| Regular worship | Yes | 68 (88.3) | 9 (11.7) | <0.001 | |
| No | 207 (55.1) | 169 (44.9) | |||
Cronbach’s alpha of all above variables is 0.695.
1. Comparison of odds ratio and 95% CI using logistic regression
Table 3 shows the comparison of normal and adjusted odds ratios using logistic regression in different models. Basic characteristics, such as place of residence, education, occupation, house structure, cooking fuel, and alcohol consumption, were not associated with illness. In the comparison of odds ratios and 95% CIs, the women who had safe toilet behavior and did not use tobacco were 2.48 (1.98–7.98) and 2.86 (1.74–7.34) times less likely, respectively, to be ill than women who did not have safe toilet behavior and who used tobacco. Likewise, women who did not eat junk food; regularly exercised, meditated, or worshiped; and had regular sleeping habits were 1.65 (1.32–4.61), 2.81 (1.91–5.62), 2.56 (2.01–4.88), 4.56 (3.91–8.26), and 2.45 (2.12–5.03) times (95% CI) less likely to be ill, respectively. Those results were observed in the full (fifth) model. Adjusted odds ratios revealed that women with self-care factors (safe toilet use, regular sleeping habits, and health check-ups), lifestyle factors (no use of tobacco and junk food), and spiritual behavior (regular worship, yoga/meditation, and exercise) had less risk for illness than women who did not engage in these activities.
Table 3.
Comparison of odds ratio and 95% CI in hierarchical logistic regression
| Major domains | Variables | Category | Outcome (No disease) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Model 1† | Model 2 | Model 3 | Mode l 4 | Model 5 (Full model) | |||
| Socioeconomic factors | Place of residence | Rural | 1 | 1 | 1 | 1 | 1 |
| Urban | 1.26 | 1.18 (0.95–1.49) | 1.12 (0.92–1.12) | 0.98 (0.94–1.26) | 0.81 (0.61–1.5) | ||
| Education | No formal | 1 | 1 | 1 | 1 | 1 | |
| Secondary | 1.62 | 1.52 (0.84–2.94) | 1.32 (0.72–1.12 | 1.08 (0.92–1.57) | 0.92 (0.51–1.7) | ||
| Higher | 1.86 | 1.65 (0.99–1.89) | 1.49 (0.94–1.75) | 1.37 (0.88–1.98) | 1.20 (1.02–1.61) | ||
| Occupation | Agriculture | 1 | 1 | 1 | 1 | 1 | |
| Housewife | 0.130 | .12 (0.03–1.21) | 0.08 (0.05–1.12) | 0.07 (0.04–1.06 ) | 0.62 (0.10–1.86) | ||
| Job | 0.79 | 0.66 (0.1–1.26) | 0.53 (0.21–1.28) | 0.29 (0.18–1.11) | 0.21 (0.09–1.30) | ||
| House structure | Dwelling | 1 | 1 | 1 | 1 | 1 | |
| Improved | 1.05 | 1.04 (0.23–1.25) | 1.04 (0.25–1.10) | 1.01 (0.6–1.15) | 0.92 (0.49–1.21) | ||
| Relatively safe | 1.07 | 1.04 (0.21–1.23) | 1.05 (0.18–1.18) | 1.02 (0.34–0.97) | 1.04 (0.04–0.92) | ||
| Type of floor | Mud | 1 | 1 | 1 | 1 | 1 | |
| Cement | 1.15 | 1.01 (0.21–1.12) | 0.99 (0.24–1.08) | 0.06 (0.01–1.02) | 0.92 (0.71–1.52) | ||
| Cooking fuel | Firewood and dung | 1 | 1 | 1 | 1 | 1 | |
| LP/bio-gas | 0.8 | 0.45 (0.25–1.14) | 0.39 (0.15–1.04) | 0.32 (0.11–1.12) | 0.28 (0.05–1.41) | ||
| Self-care factors | Safe toilet | No | 1 | 1 | 1 | 1 | |
| Yes | 2.56** | 2.53 (2.20–3.94)** | 2.5 (1.07–4.57)** | 2.48 (1.98–7.98)** | |||
| Source of drinking water | River stream | 1 | 1 | 1 | |||
| Tube well | 0.22 | 0.23 (0.16–1.07) | 0.22 (0.18–1.14) | 0.26 (0.18–1.24) | |||
| Tap water | 0.49 | 0.47 (0.21–1.03) | 0.43 (0.14–1.31) | 0.50 (0.30–1.32) | |||
| Sleeping at regular time | No | 1 | 1 | 1 | 1 | ||
| Yes | 2.03** | 1.94 (1.14–3.75)** | 1.92 (1.13–4.47)** | 2.45 (2.12–5.03)** | |||
| Health checkup last year | No | 1 | 1 | 1 | 1 | ||
| Yes | 1.52* | 1.14 (1.01–2.34) | 0.97 (0.45–1.56) | 0.87 (0.54–1.85) | |||
| Lifestyle factors | Drinking alcohol | Yes | 1 | 1 | 1 | ||
| No | 0.84 | 0.72 (0.21–1.56) | 0.68 (0.39–1.42) | ||||
| Tobacco use | Yes | 1 | 1 | 1 | |||
| No | 3.39** | 2.91 (2.11–8.01)*** | 2.86 (1.74–7.34)*** | ||||
| Junk food (as main food) | Yes | 1 | 1 | 1 | |||
| No | 2.1** | 1.71 (1.51–5.56)** | 1.65 (1.32–4.61)** | ||||
| Spiritual behaviors | Regular exercise before and after yoga | No | 1 | 1 | |||
| Yes | 3.51*** | 2.81 (1.91–5.62)*** | |||||
| Regular yoga/meditation | No | 1 | 1 | ||||
| Yes | 4.26*** | 2.56 (2.01–4.88)*** | |||||
| Regular worship | No | 1 | 1 | ||||
| Yes | 6.16*** | 4.56 (3.91–8.26)*** | |||||
unadjusted odds ratio,
p < 0.05,
p < 0.01,
p < 0.001.
DISCUSSION
This study was performed with women in the Kailali district of Nepal in relation to spiritual, lifestyle, and self-care factors with self-reported illness over the past year. This sample represents most rural settings with women as house-wives who have a basic education and average status of wealth that allows for housing, a toilet, cooking fuel, and a floor. Less than one-third of women showed regular spiritual behavior like worship, yoga, and exercise. The women who had safe toilet use and did not use tobacco were two times less likely to be ill than women who did not have safe toilet use and used tobacco. Those women who adopted spiritual behavior reported significantly less illness than women who did not. Interestingly, for illness, spiritual behavior was explicitly important compared to other factors like education, occupation, and housing status.
1. Socioeconomic factors
Socioeconomic factors are the foundation of health and wellbeing, without which humans cannot survive. Socioeconomic factors have great influence on all ages, regions, genders (male and female), and ethnicities, but factors related to self-care, lifestyle, and spiritual behavior are significantly associated with health and diseases/illness for women. Studies have found that household socioeconomic status does not significantly affect women’s health in comparison with gender inequality (among men and women) [37,38]. Therefore, household socioeconomic status might not significantly affect women’s self-reported illness in our study.
2. Self-care and illness
Health and disease are directly related to individual attitude and practice, such as hygiene and sleeping pattern. People with poor sanitation have a high risk for water-borne diseases and worm infestation [23,39]. Likewise, poor, irregular, and short sleep is associated with metabolic disease, obesity, type 2 diabetes, hypertension, and cardiovascular disease, mostly in women [40,41], which coincides with our findings.
3. Women’s lifestyle and illness
It has already been indicated that lifestyle is another pillar responsible for health and illness. Our study revealed that women who did not use tobacco or eat junk food were 2.86 and 1.65 times less likely to be ill than those who did, respectively. Female smokers had less healthy lipid profiles, high white blood cell counts, and unhealthy body mass index and blood glucose compared to nonsmokers. These biomarkers have been shown to be indicators of physical health in Austria [42], India [43], Turkey [44], and the UK [45]. Likewise, regular junk food has been found to significantly increase mental health problems in Australia [46], and the UK [47]. Although those studies were performed in youth, their findings are in line with our results.
4. Spiritual behavior and illness
Recently, the importance of spirituality has been increasingly highlighted, and medical science has applied spirituality to mental and social health. Spiritual activities were more common in primitive ages and are less common in modern times; however, promising results on spiritual research in modern medicine have motivated the resurgence of such activities. People engage in spirituality through prayer, worship, yoga (meditation), and other activities. In addition, spiritual beliefs are encouraged for healthy behavior like healthy diet, exercise, proper use of substances like tobacco and alcohol, healthy sexual relationships, and honesty and kindness. Previous studies are available for comparison with our findings. New Zealand women who regularly exercise, consume natural food, have an internal locus of control, and pursue activities with spiritual implications reported better health status than women who did not [48]. German patients who regularly practiced yoga had better general health status, higher physical functioning, and better physical component scores than those who did not [49]. Yoga has also been reported to be effective in improving health status and quality of life in patients with arthritis [50], cardiovascular conditions [51], and lung diseases [52]. There are few related comparisons of regular worship on diseases status. However, religious involvement reduced disabilities in elderly people in the US [53] and England [54]. Large numbers of participants (70,884) in the Canadian National Population Health Survey who reported that they attended worship services had significantly fewer depressive symptoms compared to those who did not attend such services [55]. These studies support our results; however, those results were broad and not focused only on women.
This study identified three major factors related to poor health: sanitation practice, tobacco use, and spiritual behavior. There are many interventions to prevent disease and improve health status, but there are very few efforts to promote spirituality. Our study showed that way of life explicitly affects health and disease. Nevertheless, there are some limitations in our study. First, the measurement approaches for worship, yoga/meditation, exercise, sleeping habits, and consumption of junk food are very difficult to verify. Moreover, recall and information bias cannot be denied. There are many indigenous spiritual behaviors that are scientific but unorganized and ignored by global and national health systems and policy. The WHO has already accepted the concept of spirituality (16), but a policy like Universal Health Care (UHC) has not materialized to date.
CONCLUSION
It can be concluded that best spiritual practices will promote health status and reduce the prevalence of diseases/ illness. A spiritual health policy and separate curriculum for basic education and medical education should be promoted globally, and further research is recommended.
ACKNOWLEDGEMENTS
The data were collected with the coordination of the KOICA Nepal HIT office and local government of Tikapur Kailali. The English language was edited by Professor Margret Storey, Editage, and eWorldediting. We sincerely thank KOICA Nepal, Professor Margret and Editage. This research was supported by the Korean National Research Foundation of Korea (NRF-2016S1A5B892520).
REFERENCES
- 1.Jahiel RI, Babor TF. Industrial epidemics, public health advocacy and the alcohol industry: lessons from other fields. Addiction. 2007;102:1335–9. doi: 10.1111/j.1360-0443.2007.01900.x. [DOI] [PubMed] [Google Scholar]
- 2.Slade J. The tobacco epidemic: Lessons from history. J Psychoactive Drugs. 1992;24:99–109. doi: 10.1080/02791072.1992.10471631. [DOI] [PubMed] [Google Scholar]
- 3.Krieger J, Higgins DL. Housing and health: Time again for public health action. Am J Public Health. 2002;92:758–68. doi: 10.2105/AJPH.92.5.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thoresen CE. Spirituality and health: Is there a relationship? J Health Psychol. 1999;4:291–300. doi: 10.1177/135910539900400314. [DOI] [PubMed] [Google Scholar]
- 5.Davison SN, Jhangri GS. The relationship between spirituality, psychosocial adjustment to illness, and health-related quality of life in patients with advanced chronic kidney disease. J Pain Symptom Manage. 2013;45:170–8. doi: 10.1016/j.jpainsymman.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 6.White WB. Smoking-related morbidity and mortality in the cardiovascular setting. Prev Cardiol. 2007;10:1–4. doi: 10.1111/j.1520-037X.2007.06050.x. [DOI] [PubMed] [Google Scholar]
- 7.Eriksen M, Mackay J, Ross H. The tobacco atlas. American Cancer Society; Atlanta, GA: 2012. [Google Scholar]
- 8.World Health Organization. Global status report on alcohol and health 2014 [Internet] c2014 [Cited 2017 Dec 1]. Available from: http://apps.who.int/iris/bitstream/10665/112736/1/9789240692763_eng.pdf.
- 9.De Vogli R, Kouvonen A, Gimeno D. The influence of market deregulation on fast food consumption and body mass index: a cross-national time series analysis. Bull World Health Organ. 2014;92:99–107A. doi: 10.2471/BLT.13.120287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Butt S, Leon JB, David CL, Chang H, Sidhu S, Sehgal AR. The prevalence and nutritional implications of fast food consumption among patients receiving hemodialysis. J Ren Nutr. 2007;17:264–8. doi: 10.1053/j.jrn.2007.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Draulans V. Gender and spirituality. In: Bouckaert L, Zsolnai L, editors. Handbook of spirituality and business. Palgrave Macmillan; London, UK: 2011. pp. 49–57. [Google Scholar]
- 12.Pisinger C, Toft U, Aadahl M, Glümer C, Jørgensen T. The relationship between lifestyle and self-reported health in a general population: The inter99 study. Prev Med. 2009;49:418–23. doi: 10.1016/j.ypmed.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 13.Karacabey K. Effect of regular exercise on health and disease. Neuro Endocrinol Lett. 2005;26:617–23. [PubMed] [Google Scholar]
- 14.Hyrkas H, Jaakkola MS, Jaakkola JJK, Heikkinen SAM. American Thoracic Society 2015 International Conference. Denver, CO: American Journal Respiratory Critical Care Medicine; 2015. Effect of regular exercise on asthma control among adults; p. A2030. [Google Scholar]
- 15.Sheldrake P. Spirituality: A brief history. 2nd ed. John Wiley & Sons; Chichester, UK: 2013. [Google Scholar]
- 16.Dhar N, Chaturvedi SK, Nandan D. Spiritual health, the fourth dimension: a public health perspective. WHO South East Asia J Public Health. 2013;2:3–5. doi: 10.4103/2224-3151.115826. [DOI] [PubMed] [Google Scholar]
- 17.Oman D, Thoresen CE. ‘Does religion cause health?’: Differing interpretations and diverse meanings. J Health Psychol. 2002;7:365–80. doi: 10.1177/1359105302007004326. [DOI] [PubMed] [Google Scholar]
- 18.Christ CP. Diving deep & surfacing: Women writers on spiritual quest. 3rd ed. Beacon Press; Boston, MA: 1995. [Google Scholar]
- 19.Chaves LJ, Gil CA. Older people’s concepts of spirituality, related to aging and quality of life. Cien Saude Colet. 2015;20:3641–52. doi: 10.1590/1413-812320152012.19062014. [DOI] [PubMed] [Google Scholar]
- 20.Waldfogel S. Spirituality in medicine. Prim Care. 1997;24:963–76. doi: 10.1016/S0095-4543(05)70319-5. [DOI] [PubMed] [Google Scholar]
- 21.Ranabhat C, Kim CB, Choi EH, Aryal A, Park MB, Doh YA. Chhaupadi culture and reproductive health of women in Nepal. Asia Pac J Public Health. 2015;27:785–95. doi: 10.1177/1010539515602743. [DOI] [PubMed] [Google Scholar]
- 22.Chhabi R, Do YA, Ahn DW, Lee KJ, Kim CB. Changing pattern of complementary and alternative medicine in Tikapur Nepal: A hope for future health. Altern Integr Med. 2014;3:1–5. [Google Scholar]
- 23.Good Neighbors International Nepal. Baseline health survey report of health services improvement in Tikapur (HIT) Insitute for Poverty Alleviation and International Development, Yonsei University; Seoul, Korea: 2012. [Google Scholar]
- 24.Thomas LE, Eisenhandler SA. Aging and the religious dimension. Praeger; Santa Barbara, CA: 1994. [Google Scholar]
- 25.Pender NJ, Murdaugh CL, Parsons MA. The health promotion model. In: Pender NJ, Murdaugh CL, Parsons MA, editors. Health promotion in nursing practice. 4th ed. Prentice Hall; Upper Saddle River, NJ: 2002. pp. 59–79. [Google Scholar]
- 26.Cockerham WC. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav. 2005;46:51–67. doi: 10.1177/002214650504600105. [DOI] [PubMed] [Google Scholar]
- 27.Siddiqui N, Nessa A, Hossain M. Regular physical exercise: way to healthy life. Mymensingh Med J. 2010;19:154–8. [PubMed] [Google Scholar]
- 28.Prasad K, Wahner-Roedler DL, Cha SS. Effect of a single-session meditation training to reduce stress and improve quality of life among health care professionals: a “dose-ranging” feasibility study. Altern Ther Health Med. 2011;17:46–9. [PubMed] [Google Scholar]
- 29.Santorelli SF. Mindfulness-based stress reduction (MBSR): Standards of practice. University of Massachusetts Medical School, Center for Mindfulness in Medicine, Health Care & Society; Worcester, MA: 2014. [Google Scholar]
- 30.Salmoirago-Blotcher E, Fitchett G, Ockene JK, Schnall E, Crawford S, Granek I, Manson J, Ockene I, O’Sullivan MJ, Powell L. Religion and healthy lifestyle behaviors among postmenopausal women: the women’s health initiative. J Behav Med. 2011;34:360–71. doi: 10.1007/s10865-011-9322-z. [DOI] [PubMed] [Google Scholar]
- 31.Perry GS, Patil SP, Presley-Cantrell LR. Raising awareness of sleep as a healthy behavior. Prev Chronic Dis. 2013;10:1–4. doi: 10.5888/pcd10.130081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Naeem Z. Increasing trend of junk food use in Saudi Arabia and health implications. Int J Health Sci. 2012;6:V–VI. doi: 10.12816/0005967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Emson HE. Health, disease and illness: matters for definition. Can Med Assoc J. 1987;136:811–3. [PMC free article] [PubMed] [Google Scholar]
- 34.Resource Centre for Primary Health Care (RECPHEC) Media coverage of junk food and its content analysis on selected Nepali and Indian television channels. Resource Centre for Primary Health Care; Kathmandu, Nepal: 2012. [Google Scholar]
- 35.Thomsen RJ. Spirituality in medical practice. Arch Dermatol. 1998;134:1443–6. doi: 10.1001/archderm.134.11.1443. [DOI] [PubMed] [Google Scholar]
- 36.Moore A, Gruber T, Derose J, Malinowski P. Regular, brief mindfulness meditation practice improves electrophysiological markers of attentional control. Front Hum Neurosci. 2012;6:18. doi: 10.3389/fnhum.2012.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Borooah VK. Gender bias among children in India in their diet and immunisation against disease. Soc Sci Med. 2004;58:1719–31. doi: 10.1016/S0277-9536(03)00342-3. [DOI] [PubMed] [Google Scholar]
- 38.Darnton-Hill I, Webb P, Harvey PW, Hunt JM, Dalmiya N, Chopra M, Ball MJ, Bloem MW, de Benoist B. Micronutrient deficiencies and gender: social and economic costs. Am J Clin Nutr. 2005;81:1198S–205S. doi: 10.1093/ajcn/81.5.1198. [DOI] [PubMed] [Google Scholar]
- 39.Grimes JET, Croll D, Harrison WE, Utzinger J, Freeman MC, Templeton MR. The relationship between water, sanitation and schistosomiasis: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2014;8:e3296. doi: 10.1371/journal.pntd.0003296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 41.Ramtahal R, Khan C, Maharaj-Khan K, Nallamothu S, Hinds A, Dhanoo A, Yeh H-C, Hill-Briggs F, Lazo M. Prevalence of self-reported sleep duration and sleep habits in type 2 diabetes patients in South Trinidad. J Epidemiol Glob Health. 2015;5:S35–S43. doi: 10.1016/j.jegh.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Oliveira Fontes Gasperin L, Neuberger M, Tichy A, Moshammer H. Cross-sectional association between cigarette smoking and abdominal obesity among Austrian bank employees. BMJ Open. 2014;4:e004899. doi: 10.1136/bmjopen-2014-004899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shukla HC, Gupta PC, Mehta HC, Hébert JR. Descriptive epidemiology of body mass index of an urban adult population in western India. J Epidemiol Community Health. 2002;56:876–80. doi: 10.1136/jech.56.11.876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karakas P, BozkIr MG. Clinical research: Anthropometric indices in relation to overweight and obesity among Turkish medical students. Arch Med Sci. 2012;8:209–13. doi: 10.5114/aoms.2012.28546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. N Engl J Med. 1991;324:739–45. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- 46.Oddy WH, Robinson M, Ambrosini GL, Therese A, de Klerk NH, Beilin LJ, Silburn SR, Zubrick SR, Stanley FJ. The association between dietary patterns and mental health in early adolescence. Prev Med. 2009;49:39–44. doi: 10.1016/j.ypmed.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 47.Zahra J, Ford T, Jodrell D. Cross-sectional survey of daily junk food consumption, irregular eating, mental and physical health and parenting style of British secondary school children. Child Care Health Dev. 2014;40:481–91. doi: 10.1111/cch.12068. [DOI] [PubMed] [Google Scholar]
- 48.Cobb-Clark DA, Kassenboehmer SC, Schurer S. Healthy habits: The connection between diet, exercise, and locus of control. J Econ Behav Organ. 2014;98:1–28. doi: 10.1016/j.jebo.2013.10.011. [DOI] [Google Scholar]
- 49.Cramer H, Lauche R, Langhorst J, Dobos G, Paul A. Quality of life and mental health in patients with chronic diseases who regularly practice yoga and those who do not: a case-control study. Evid Based Complement Alternat Med. 2013;2013:702914. doi: 10.1155/2013/702914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Haaz S, Bartlett SJ. Yoga for arthritis: A scoping review. Rheum Dis Clin North Am. 2011;37:33–46. doi: 10.1016/j.rdc.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: A systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 52.Raub JA. Psychophysiologic effects of Hatha Yoga on musculoskeletal and cardiopulmonary function: a literature review. J Altern Complement Med. 2002;8:797–812. doi: 10.1089/10755530260511810. [DOI] [PubMed] [Google Scholar]
- 53.Hybels CF, Blazer DG, George LK, Koenig HG. The complex association between religious activities and functional limitations in older adults. Gerontologist. 2012;52:676–85. doi: 10.1093/geront/gnr156. [DOI] [PubMed] [Google Scholar]
- 54.Park NS, Klemmack DL, Roff LL, Parker MW, Koenig HG, Sawyer P, Allman RM. Religiousness and longitudinal trajectories in elders’ functional status. Res Aging. 2008;30:279–98. doi: 10.1177/0164027507313001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Baetz M, Griffin R, Bowen R, Koenig HG, Marcoux E. The association between spiritual and religious involvement and depressive symptoms in a Canadian population. J Nerv Ment Dis. 2004;192:818–22. doi: 10.1097/01.nmd.0000146735.73827.85. [DOI] [PubMed] [Google Scholar]