Abstract
Exercise is typically one of the first management strategies advised for patients newly diagnosed with type 2 diabetes. Together with diet and behavior modification, exercise is an essential component of all diabetes and obesity prevention and lifestyle intervention programs. Exercise training, whether aerobic or resistance training or a combination, facilitates improved glucose regulation. High-intensity interval training is also effective and has the added benefit of being very time-efficient. While the efficacy, scalability, and affordability of exercise for the prevention and management of type 2 diabetes are well established, sustainability of exercise recommendations for patients remains elusive.
Type 2 diabetes has emerged as a major public health and economic burden of the 21st century. Recent statistics from the Centers for Disease Control and Prevention suggest that diabetes affects 29.1 million people in the United States,1 and the International Diabetes Federation estimates diabetes effects 366 million people worldwide.2
As these shocking numbers continue to increase, the cost of caring for patients with diabetes is placing enormous strain on the economies of the US and other countries. In order to manage and treat a disease on the scale of diabetes, the approaches need to be efficacious, sustainable, scalable, and affordable.
Of all the treatment options available, including multiple new medications and bariatric surgery (for patients who meet the criteria, discussed elsewhere in this supplement),3–5 exercise as part of a lifestyle approach6 is a strategy that meets the majority of these criteria.
The health benefits of exercise have a long and storied history. Hippocrates, the father of scientific medicine, was the first physician on record to recognize the value of exercise for a patient with “consumption.”7 Today, exercise is recommended as one of the first management strategies for patients newly diagnosed with type 2 diabetes and, together with diet and behavior modification, is a central component of all type 2 diabetes and obesity prevention programs.
The evidence base for the efficacy, scalability, and affordability of exercise includes multiple large randomized controlled trials; and these data were used to create the recently updated exercise guidelines for the prevention and treatment of type 2 diabetes, published by the American Diabetes Association (ADA), American College of Sports Medicine (ACSM), and other national organizations.8–10
Herein, we highlight the literature surrounding the metabolic effects and clinical outcomes in patients with type 2 diabetes following exercise intervention, and point to future directions for translational research in the field of exercise and diabetes.
It is known that adults who maintain a physically active lifestyle can reduce their risk of developing impaired glucose tolerance, insulin resistance, and type 2 diabetes.8 It has also been established that low cardiovascular fitness is a strong and independent predictor of all-cause mortality in patients with type 2 diabetes.11,12 Indeed, patients with diabetes are 2 to 4 times more likely than healthy individuals to suffer from cardiovascular disease, due to the metabolic complexity and underlying comorbidities of type 2 diabetes including obesity, insulin resistance, dyslipidemia, hyperglycemia, and hypertension.13,14
Additionally, elevated hemoglobin A1c (HbA1c) levels are predictive of vascular complications in patients with diabetes, and regular exercise has been shown to reduce HbA1c levels, both alone and in conjunction with dietary intervention. In a meta-analysis of 9 randomized trials comprising 266 adults with type 2 diabetes, patients randomized to 20 weeks of regular exercise at 50% to 75% of their maximal aerobic capacity (VO2max) demonstrated marked improvements in HbA1c and cardiorespiratory fitness.11 Importantly, larger reductions in HbA1c were observed with more intense exercise, reflecting greater improvements in blood glucose control with increasing exercise intensity.
In addition to greater energy expenditure, which aids in reversing obesity-associated type 2 diabetes, exercise also boosts insulin action through short-term effects, mainly via insulin-independent glucose transport. For example, our laboratory and others have shown that as little as 7 days of vigorous aerobic exercise training in adults with type 2 diabetes results in improved glycemic control, without any effect on body weight.15,16 Specifically, we observed decreased fasting plasma insulin, a 45% increase in insulin-stimulated glucose disposal, and suppressed hepatic glucose production (HGP) during carefully controlled euglycemic hyperinsulinemic clamps.15
Although the metabolic benefits of exercise are striking, the effects are short-lived and begin to fade within 48 to 96 hours.17 Therefore, an ongoing exercise program is required to maintain the favorable metabolic milieu that can be derived through exercise.
EXERCISE MODALITIES
Aerobic exercise
The vast majority of the literature about the effects of exercise on glycemic parameters in type 2 diabetes has been centered on interventions involving aerobic exercise. Aerobic exercise consists of continuous, rhythmic movement of large muscle groups, such as in walking, jogging, and cycling. The most recent ADA guidelines state that individual sessions of aerobic activity should ideally last at least 30 minutes per day and be performed 3 to 7 days of the week (Table 1).18 Moderate to vigorous (65%–90% of maximum heart and rate) aerobic exercise training improves VO2max cardiac output, which are associated with substantially reduced cardiovascular and overall mortality risk in patients with type 2 diabetes.19
TABLE 1.
American Diabetes Association recommendations for exercise in type 2 diabetes
Aerobic exercise: At least 150 minutes/week of moderate to vigorous exercise
|
Resistance exercise: Progressive moderate to vigorous resistance training should be completed 2 to 3 times/week on nonconsecutive days
|
| Flexibility and balance training are recommended 2 to 3 times/week for older adults |
| Participation in supervised training programs is recommended to maximize health benefits of exercise in type 2 diabetes |
Notably, aerobic exercise is a well-established way to improve HbA1c, and strong evidence exists with regard to the effects of aerobic activity on weight loss and the enhanced regulation of lipid and lipoprotein metabolism.8 For example, in a 2007 report, 6 months of aerobic exercise training in 60 adults with type 2 diabetes led to reductions in HbA1c (−0.63% ± 0.41 vs 0.31% ± 0.10, P < .001), fasting plasma glucose (−18.6 mg/dL ± 4.4 vs 4.28 mg/dL ± 2.57, P < .001), insulin resistance (−1.52 ± 0.6 vs 0.56 ± 0.44, P = .023; as measured by homeostatic model assessment), fasting insulin (−2.91 mU/L ± 0.4 vs 0.94 mU/L ± 0.21, P = .031), and systolic blood pressure (−6.9 mm Hg ± 5.19 vs 1.22 mm Hg ± 1.09, P = .010) compared with the control group.14
Furthermore, meta-analyses reviewing the benefits of aerobic activity for patients with type 2 diabetes have repeatedly confirmed that compared with patients in sedentary control groups, aerobic exercise improves glycemic control, insulin sensitivity, oxidative capacity, and important related metabolic parameters.11 Taken together, there is ample evidence that aerobic exercise is a tried-and-true exercise modality for managing and preventing type 2 diabetes.
Resistance training
During the last 2 decades, resistance training has gained considerable recognition as a viable exercise training option for patients with type 2 diabetes. Synonymous with strength training, resistance exercise involves movements utilizing free weights, weight machines, body weight exercises, or elastic resistance bands.
Primary outcomes in studies evaluating the effects of resistance training in type 2 diabetes have found improvements that range from 10% to 15% in strength, bone mineral density, blood pressure, lipid profiles, cardiovascular health, insulin sensitivity, and muscle mass.18,20 Furthermore, because of the increased prevalence of type 2 diabetes with aging, coupled with age-related decline in muscle mass, known as sarcopenia,21 resistance training can provide additional health benefits in older adults.
Dunstan et al21 reported a threefold greater reduction in HbA1c in patients with type 2 diabetes ages 60 to 80 compared with nonexercising patients in a control group. They also noted an increase in lean body mass in the resistance-training group, while those in the nonexercising control group lost lean mass after 6 months. In a shorter, 8-week circuit weight training study performed by the same research group, patients with type 2 diabetes had improved glucose and insulin responses during an oral glucose tolerance test.22
These findings support the use of resistance training as part of a diabetes management plan. In addition, key opinion leaders advocate that the resistance-training-induced increase in skeletal muscle mass and the associated reductions in HbA1c may indicate that skeletal muscle is a “sink” for glucose; thus, the improved glycemic control in response to resistance training may be at least in part the result of enhanced muscle glycogen storage.21,23
Based on increasing evidence supporting the role of resistance training in glycemic control, the ADA and ACSM recently updated their exercise guidelines for treatment and prevention of type 2 diabetes to include resistance training.9
Combining aerobic and resistance training
The combination of aerobic and resistance training, as recommended by current ADA guidelines, may be the most effective exercise modality for controlling glucose and lipids in type 2 diabetes.
Cuff et al24 evaluated whether a combined training program could improve insulin sensitivity beyond that of aerobic exercise alone in 28 postmenopausal women with type 2 diabetes. Indeed, 16 weeks of combined training led to significantly increased insulin-mediated glucose uptake compared with a group performing only aerobic exercise, reflecting greater insulin sensitivity.
Balducci et al25 demonstrated that combined aerobic and resistance training markedly improved HbA1c (from 8.31% ± 1.73 to 7.1% ± 1.16, P < .001) compared with the control group and globally improved risk factors for cardiovascular disease, supporting the notion that combined training for patients with type 2 diabetes may have additive benefits.
Of note, Snowling and Hopkins26 performed a head-to-head meta-analysis of 27 controlled trials on the metabolic effects of aerobic, resistance, and combination training in a total of 1,003 patients with diabetes. All 3 exercise modes provided favorable effects on HbA1c, fasting and postprandial glucose levels, insulin sensitivity, and fasting insulin levels, and the differences between exercise modalities were trivial.
In contrast, Schwingshackl and colleagues27 performed a systematic review of 14 randomized controlled trials for the same 3 exercise modalities in 915 adults with diabetes and reported that combined training produced a significantly greater reduction in HbA1c than aerobic or resistance training alone.
Future research is necessary to quantify the additive and synergistic clinical benefits of combined exercise compared with aerobic or resistance training regimens alone; however, evidence suggests that combination exercise may be the optimal strategy for managing diabetes.
High-intensity interval training
High-intensity interval training (HIIT) has emerged as one of the fastest growing exercise programs in recent years. HIIT consists of 4 to 6 repeated, short (30-second) bouts of maximal effort interspersed with brief periods (30 to 60 seconds) of rest or active recovery. Exercise is typically performed on a stationary bike, and a single session lasts about 10 minutes.
HIIT increases skeletal muscle oxidative capacity, glycemic control, and insulin sensitivity in adults with type 2 diabetes.28,29 A recent meta-analysis that quantified the effects of HIIT programs on glucose regulation and insulin resistance reported superior effects for HIIT compared with aerobic training or no exercise as a control.28 Specifically, in 50 trials with interventions lasting at least 2 weeks, participants in HIIT groups had a 0.19% decrease in HbA1c and a 1.3-kg decrease in body weight compared with control groups.
Alternative high-intensity exercise programs have also emerged in recent years such as CrossFit, which we evaluated in a group of 12 patients with type 2 diabetes. Our proof-of-concept study found that a 6-week CrossFit program reduced body fat, diastolic blood pressure, lipids, and metabolic syndrome Z-score, and increased insulin sensitivity to glucose, basal fat oxidation, VO2max, and high-molecular-weight adiponectin.30 HIIT appears to be another effective way to improve metabolic health; and for patients with type 2 diabetes who can tolerate HIIT, it may be a time-efficient, alternative approach to continuous aerobic exercise.
BENEFITS OF EXERCISE FOR SPECIFIC METABOLIC TISSUES
Within 5 years of the discovery of insulin by Banting and Best in 1921, the first report of exercise-induced improvements in insulin action was published, though the specific cellular and molecular mechanisms that underpin these effects remain unknown.31
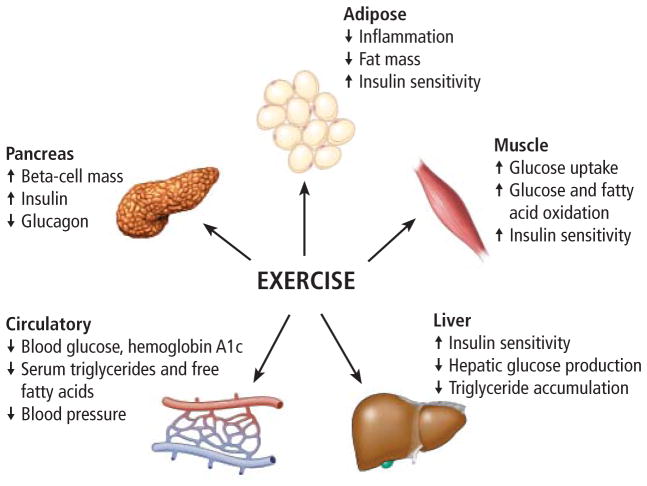
There is general agreement that the acute or short-term exercise effects are the result of insulin-dependent and insulin-independent mechanisms, while longer-term effects also involve “organ crosstalk,” such as from skeletal muscle to adipose tissue, the liver, and the pancreas, all of which mediate favorable systemic effects on HbA1c, blood glucose levels, blood pressure, and serum lipid profiles (Figure 1).
FIGURE 1.
Tissue-specific metabolic effects of exercise in patients with type 2 diabetes.
Skeletal muscle
Following a meal, skeletal muscle is the primary site for glucose disposal and uptake. Peripheral insulin resistance originating in skeletal muscle is a major driver for the development and progression of type 2 diabetes.
Exercise enhances skeletal muscle glucose uptake using both insulin-dependent and insulin-independent mechanisms, and regular exercise results in sustained improvements in insulin sensitivity and glucose disposal.32
Of note, acute bouts of exercise can also temporarily enhance glucose uptake by the skeletal muscle up to fivefold via increased (insulin-independent) glucose transport.33 As this transient effect fades, it is replaced by increased insulin sensitivity, and over time, these 2 adaptations to exercise result in improvements in both the insulin responsiveness and insulin sensitivity of skeletal muscle.34
The fuel-sensing enzyme adenosine monophosphate-activated protein kinase (AMPK) is the major insulin-independent regulator of glucose uptake, and its activation in skeletal muscle by exercise induces glucose transport, lipid and protein synthesis, and nutrient metabolism.35 AMPK remains transiently activated after exercise and regulates several downstream targets involved in mitochondrial biogenesis and function and oxidative capacity.36
In this regard, aerobic training has been shown to increase skeletal muscle mitochondrial content and oxidative enzymes, resulting in dramatic improvements in glucose and fatty acid oxidation10 and increased expression of proteins involved in insulin signaling.37
Adipose tissue
Exercise confers numerous positive effects in adipose tissue, namely, reduced fat mass, enhanced insulin sensitivity, and decreased inflammation. Chronic low-grade inflammation has been integrally linked to type 2 diabetes and increases the risk of cardiovascular disease.38
Several inflammatory adipokines have emerged as novel predictors for the development of atherosclerosis,39 and fat-cell enlargement from excessive caloric intake leads to increased production of pro-inflammatory cytokines, altered adipokine secretion, increased circulating fatty acids, and lipotoxicity concomitant with insulin resistance.40
It has been suggested that exercise may suppress cytokine production through reduced inflammatory cell infiltration and improved adipocyte function.41 Levels of the key pro-inflammatory marker C-reactive protein is markedly reduced by exercise,14,42 and normalization of adipokine signaling and related cytokine secretion has been validated for multiple exercise modalities.42
Moreover, Ibañez et al43 demonstrated that in addition to significant improvements in insulin sensitivity, resistance exercise training reduced visceral and subcutaneous fat mass in patients with type 2 diabetes.
Liver
The liver regulates fasting glucose through gluconeogenesis and glycogen storage. The liver is also the primary site of action for pancreatic hormones during the transition from pre- to postprandial states.
As with skeletal muscle and adipose tissue, insulin resistance is also present within the liver in patients with type 2 diabetes. Specifically, impaired suppression of HGP by insulin is a hallmark of type 2 diabetes, leading to sustained hyperglycemia.44
Approaches using fasting measures of glucose and insulin do not distinguish between peripheral and hepatic insulin resistance.45 Instead, hepatic insulin sensitivity and HGP are best assessed by the hyperinsulinemic-euglycemic clamp technique, along with isotopic glucose tracers.15
Although more elaborate, magnetic resonance spectroscopy may also be used to assess intrahepatic lipid content, as its accumulation has been shown to drive hepatic insulin resistance.46 Indirect measures of hepatic dysfunction may be made from increased levels of the circulating hepatic enzymes alkaline phosphatase, alanine transaminase, and aspartate transaminase.16
From an exercise perspective, we have shown that 7 days of aerobic training, in the absence of weight loss, improves hepatic insulin sensitivity.15 It has also been shown that hepatic AMPK is stimulated during exercise, suggesting that an AMPK-induced adaptive response to exercise may facilitate improved suppression of HGP.47 We have also shown that a longer 12-week aerobic exercise intervention reduces hepatic insulin resistance, with and without restricted caloric intake.48 Further, HGP correlated with reduced visceral fat, suggesting that this fat depot may play an important mechanistic role in improved hepatic function.
Pancreas
Insulin resistance in adipose tissue, muscle, or the liver places greater demand on insulin secretion from pancreatic beta cells. For many, this hypersecretory state is unsustainable, and the subsequent loss of beta-cell function marks the onset of type 2 diabetes.49 Fasting plasma glucose, insulin, and glucagon levels are generally poor indicators of beta-cell function.
Clinical research studies typically use the oral glucose tolerance test and hyperglycemic clamp technique to more accurately measure the dynamic regulation of glucose homeostasis by the pancreas.50 However, few studies have examined the effects of exercise on beta-cell function in type 2 diabetes.
Dela and colleagues51 showed that 3 months of aerobic training improved beta-cell function in type 2 diabetes, but only in those who had some residual function and were less severely diabetic. We have shown that a 12-week aerobic exercise intervention improves beta-cell function in older obese adults and in patients with type 2 diabetes.52,53 We have also found that improvements in glycemic control that occur with exercise are better predicted by changes in insulin secretion as opposed to peripheral insulin sensitivity.54 It has also been shown that a relatively short (8-week) HIIT program improved beta-cell function in patients with type 2 diabetes.55 And we recently found that a 6-week CrossFit training program improved beta-cell function in adults with type 2 diabetes.30
SUMMARY, CONCLUSIONS, AND FUTURE DIRECTIONS
Regular exercise produces health benefits beyond improvements in cardiovascular fitness. These include enhanced glycemic control, insulin signaling, and blood lipids, as well as reduced low-grade inflammation, improved vascular function, and weight loss.
Both aerobic and resistance training programs promote healthier skeletal muscle, adipose tissue, liver, and pancreatic function.18 Greater whole-body insulin sensitivity is seen immediately after exercise and persists for up to 96 hours. While a discrete bout of exercise provides substantial metabolic benefits in diabetic cohorts, maintenance of glucose control and insulin sensitivity are maximized by physiologic adaptations that only occur with weeks, months, and years of exercise training.15,33
Exercise intensity,11 volume, and frequency56 are associated with reductions in HbA1c; however, a consensus has not been reached on whether one is a better determinant than the other.
The most important consideration when recommending exercise to patients with type 2 diabetes is that the intensity and volume be optimized for the greatest metabolic benefit while avoiding injury or cardiovascular risk. In general, the risk of exercise-induced adverse events is low, even in adults with type 2 diabetes, and there is no current evidence that screening procedures beyond usual diabetes care are needed to safely prescribe exercise in asymptomatic patients in this population.18
Future clinical research in this area will provide a broader appreciation for the interactions (positive and negative) between exercise and diabetes medications, the synergy between exercise and bariatric surgery, and the potential to use exercise to reduce the health burden of diabetes complications, including nephropathy, retinopathy, neuropathy, and peripheral arterial disease.
Moreover, basic research will likely identify the detailed molecular defects that contribute to diabetes in insulin-targeted tissues. The emerging science surrounding cytokines, adipokines, myokines, and, most recently, exerkines is likely to deepen our understanding of the mechanistic links between exercise and diabetes management.
Finally, although we have ample evidence that exercise is an effective, scalable, and affordable approach to prevent and manage type 2 diabetes, we still need to overcome the challenge of discovering how to make exercise sustainable for patients.
KEY POINTS.
Exercise is often the first lifestyle recommendation made to patients newly diagnosed with type 2 diabetes.
Together with diet and behavior modification, exercise is central to effective lifestyle prevention and management of type 2 diabetes.
All exercise, whether aerobic or resistance training or a combination, facilitates improved glucose regulation.
In addition to the cardiovascular benefits, long-term exercise promotes healthier skeletal muscle, adipose tissue, and liver and pancreas function.
Exercise programs for patients with type 2 diabetes should be of sufficient intensity and volume to maximize the metabolic benefit while avoiding injury and cardiovascular risk.
Acknowledgments
Dr. Kirwan reported research grant support from NIH R01DK108089, NIH R01HD088061, NIH U34DK107917, NIH R21AR067477, and Metagenics Inc.
Footnotes
Jessica Sacks and Stephan Nieuwoudt reported no financial interests or relationships that pose a potential conflict of interest with this article.
Contributor Information
JOHN P. KIRWAN, Department of Pathobiology, Lerner Research Institute, Cleveland Clinic; Department of Physiology and Biophysics, Case Western Reserve University; Metabolic Translational Research Center, Endocrinology & Metabolism Institute, Cleveland Clinic, Cleveland, OH.
JESSICA SACKS, Department of Pathobiology, Lerner Research Institute, Cleveland Clinic, Department of Physiology and Biophysics, Case Western Reserve University, Cleveland, OH.
STEPHAN NIEUWOUDT, Department of Pathobiology, Lerner Research Institute, Cleveland Clinic; Department of Physiology and Biophysics, Case Western Reserve University, Cleveland, OH.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. US Department of Health and Human Services; 2014. [Google Scholar]
- 2.Whiting DR, Guariguata L, Weil C, Shaw J. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94:311–321. doi: 10.1016/j.diabres.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 3.Korner J, Bessler M, Cirilo LJ, et al. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005;90:359–365. doi: 10.1210/jc.2004-1076. [DOI] [PubMed] [Google Scholar]
- 4.Schauer PR, Bhatt DL, Kirwan JP, et al. for the STAMPEDE Investigators. Bariatric surgery versus intensive medical therapy for diabetes—3-year outcomes. N Engl J Med. 2014;370:2002–2013. doi: 10.1056/NEJMoa1401329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012;366:1567–1576. doi: 10.1056/NEJMoa1200225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wing RR, Bolin P, Brancati FL, et al. for the Look AHEAD Research Group. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–154. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tipton CM. The history of “Exercise Is Medicine” in ancient civilizations. Adv Physiol Educ. 2014;38:109–117. doi: 10.1152/advan.00136.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zanuso S, Jimenez A, Pugliese G, Corigliano G, Balducci S. Exercise for the management of type 2 diabetes: a review of the evidence. Acta Diabetol. 2010;47:15–22. doi: 10.1007/s00592-009-0126-3. [DOI] [PubMed] [Google Scholar]
- 9.Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C, White RD. Physical activity/exercise and type 2 diabetes: a consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:1433–1438. doi: 10.2337/dc06-9910. [DOI] [PubMed] [Google Scholar]
- 10.Garber CE, Blissmer B, Deschenes MR, et al. for the American College of Sports Medicine. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 11.Boulé NG, Kenny GP, Haddad E, Wells GA, Sigal RJ. Meta-analysis of the effect of structured exercise training on cardiorespiratory fitness in type 2 diabetes mellitus. Diabetologia. 2003;46:1071–1081. doi: 10.1007/s00125-003-1160-2. [DOI] [PubMed] [Google Scholar]
- 12.Wei M, Gibbons LW, Kampert JB, Nichaman MZ, Blair SN. Low cardiorespiratory fitness and physical inactivity as predictors of mortality in men with type 2 diabetes. Ann Intern Med. 2000;132:605–611. doi: 10.7326/0003-4819-132-8-200004180-00002. [DOI] [PubMed] [Google Scholar]
- 13.Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med. 1998;339:229–234. doi: 10.1056/NEJM199807233390404. [DOI] [PubMed] [Google Scholar]
- 14.Kadoglou NPE, Iliadis F, Angelopoulou N, et al. The anti-inflammatory effects of exercise training in patients with type 2 diabetes mellitus. Eur J Cardiovasc Prev Rehabil. 2007;14:837–843. doi: 10.1097/HJR.0b013e3282efaf50. [DOI] [PubMed] [Google Scholar]
- 15.Kirwan JP, Solomon TPJ, Wojta DM, Staten MA, Holloszy JO. Effects of 7 days of exercise training on insulin sensitivity and responsiveness in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab. 2009;297:E151–E156. doi: 10.1152/ajpendo.00210.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Winnick JJ, Sherman WM, Habash DL, et al. Short-term aerobic exercise training in obese humans with type 2 diabetes mellitus improves whole-body insulin sensitivity through gains in peripheral, not hepatic insulin sensitivity. J Clin Endocrinol Metab. 2008;93:771–778. doi: 10.1210/jc.2007-1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.King DS, Baldus PJ, Sharp RL, Kesl LD, Feltmeyer TL, Riddle MS. Time course for exercise-induced alterations in insulin action and glucose tolerance in middle-aged people. J Appl Physiol (1985) 1995;78:17–22. doi: 10.1152/jappl.1995.78.1.17. [DOI] [PubMed] [Google Scholar]
- 18.Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39:2065–2079. doi: 10.2337/dc16-1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sluik D, Buijsse B, Muckelbauer R, et al. Physical activity and mortality in individuals with diabetes mellitus: a prospective study and meta-analysis. Arch Intern Med. 2012;172:1285–1295. doi: 10.1001/archinternmed.2012.3130. [DOI] [PubMed] [Google Scholar]
- 20.Gordon BA, Benson AC, Bird SR, Fraser SF. Resistance training improves metabolic health in type 2 diabetes: a systematic review. Diabetes Res Clin Pract. 2009;83:157–175. doi: 10.1016/j.diabres.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 21.Dunstan DW, Daly RM, Owen N, et al. High-intensity resistance training improves glycemic control in older patients with type 2 diabetes. Diabetes Care. 2002;25:1729–1736. doi: 10.2337/diacare.25.10.1729. [DOI] [PubMed] [Google Scholar]
- 22.Dunstan DW, Puddey IB, Beilin LJ, Burke V, Morton AR, Stanton KG. Effects of a short-term circuit weight training program on glycaemic control in NIDDM. Diabetes Res Clin Pract. 1998;40:53–61. doi: 10.1016/s0168-8227(98)00027-8. [DOI] [PubMed] [Google Scholar]
- 23.Castaneda C, Layne JE, Munoz-Orians L, et al. A randomized controlled trial of resistance exercise training to improve glycemic control in older adults with type 2 diabetes. Diabetes Care. 2002;25:2335–2341. doi: 10.2337/diacare.25.12.2335. [DOI] [PubMed] [Google Scholar]
- 24.Cuff DJ, Meneilly GS, Martin A, Ignaszewski A, Tildesley HD, Frohlich JJ. Effective exercise modality to reduce insulin resistance in women with type 2 diabetes. Diabetes Care. 2003;26:2977–2982. doi: 10.2337/diacare.26.11.2977. [DOI] [PubMed] [Google Scholar]
- 25.Balducci S, Leonetti F, Di Mario U, Fallucca F. Is a long-term aerobic plus resistance training program feasible for and effective on metabolic profiles in type 2 diabetic patients [letter]? Diabetes Care. 2004;27:841–842. doi: 10.2337/diacare.27.3.841. [DOI] [PubMed] [Google Scholar]
- 26.Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care. 2006;29:2518–2527. doi: 10.2337/dc06-1317. [DOI] [PubMed] [Google Scholar]
- 27.Schwingshackl L, Missbach B, Dias S, König J, Hoffmann G. Impact of different training modalities on glycaemic control and blood lipids in patients with type 2 diabetes: a systematic review and network meta-analysis. Diabetologia. 2014;57:1789–1797. doi: 10.1007/s00125-014-3303-z. [DOI] [PubMed] [Google Scholar]
- 28.Jelleyman C, Yates T, O’Donovan G, et al. The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obes Rev. 2015;16:942–961. doi: 10.1111/obr.12317. [DOI] [PubMed] [Google Scholar]
- 29.Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J Physiol. 2012;590:1077–1084. doi: 10.1113/jphysiol.2011.224725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nieuwoudt S, Fealy CE, Foucher JA, et al. Functional high intensity training improves pancreatic beta-cell function in adults with type 2 diabetes. Am J Physiol Endocrinol Metab. 2017 doi: 10.1152/ajpendo.00407.2016. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lawrence RD. The effect of exercise on insulin action in diabetes. Br Med J. 1926;1:648–650. doi: 10.1136/bmj.1.3406.648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hawley JA, Lessard SJ. Exercise training-induced improvements in insulin action. Acta Physiol (Oxf) 2008;192:127–135. doi: 10.1111/j.1748-1716.2007.01783.x. [DOI] [PubMed] [Google Scholar]
- 33.Magkos F, Tsekouras Y, Kavouras SA, Mittendorfer B, Sidossis LS. Improved insulin sensitivity after a single bout of exercise is curvilinearly related to exercise energy expenditure. Clin Sci (Lond) 2008;114:59–64. doi: 10.1042/CS20070134. [DOI] [PubMed] [Google Scholar]
- 34.Holloszy JO. Exercise-induced increase in muscle insulin sensitivity. J Appl Physiol (1985) 2005;99:338–343. doi: 10.1152/japplphysiol.00123.2005. [DOI] [PubMed] [Google Scholar]
- 35.Hawley JA, Hargreaves M, Zierath JR. Signalling mechanisms in skeletal muscle: role in substrate selection and muscle adaptation. Essays Biochem. 2006;42:1–12. doi: 10.1042/bse0420001. [DOI] [PubMed] [Google Scholar]
- 36.Ruderman NB, Carling D, Prentki M, Cacicedo JM. AMPK, insulin resistance, and the metabolic syndrome. J Clin Invest. 2013;123:2764–2772. doi: 10.1172/JCI67227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mulya A, Haus JM, Solomon TPJ, et al. Exercise training-induced improvement in skeletal muscle PGC-1alpha-mediated fat metabolism is independent of dietary glycemic index. Obesity (Silver Spring) 2017;25:721–729. doi: 10.1002/oby.21799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dandona P, Aljada A, Chaudhuri A, Bandyopadhyay A. The potential influence of inflammation and insulin resistance on the pathogenesis and treatment of atherosclerosis-related complications in type 2 diabetes. J Clin Endocrinol Metab. 2003;88:2422–2429. doi: 10.1210/jc.2003-030178. [DOI] [PubMed] [Google Scholar]
- 39.Kritchevsky SB, Cesari M, Pahor M. Inflammatory markers and cardiovascular health in older adults. Cardiovasc Res. 2005;66:265–275. doi: 10.1016/j.cardiores.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 40.Cusi K. The role of adipose tissue and lipotoxicity in the pathogenesis of type 2 diabetes. Curr Diab Rep. 2010;10:306–315. doi: 10.1007/s11892-010-0122-6. [DOI] [PubMed] [Google Scholar]
- 41.Balducci S, Zanuso S, Nicolucci A, et al. Anti-inflammatory effect of exercise training in subjects with type 2 diabetes and the metabolic syndrome is dependent on exercise modalities and independent of weight loss. Nutr Metab Cardiovasc Dis. 2010;20:608–617. doi: 10.1016/j.numecd.2009.04.015. [DOI] [PubMed] [Google Scholar]
- 42.Jorge MLMP, de Oliveira VN, Resende NM, et al. The effects of aerobic, resistance, and combined exercise on metabolic control, inflammatory markers, adipocytokines, and muscle insulin signaling in patients with type 2 diabetes mellitus. Metabolism. 2011;60:1244–1252. doi: 10.1016/j.metabol.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 43.Ibañez J, Izquierdo M, Argüelles I, et al. Twice-weekly progressive resistance training decreases abdominal fat and improves insulin sensitivity in older men with type 2 diabetes. Diabetes Care. 2005;28:662–667. doi: 10.2337/diacare.28.3.662. [DOI] [PubMed] [Google Scholar]
- 44.Basu R, Chandramouli V, Dicke B, Landau B, Rizza R. Obesity and type 2 diabetes impair insulin-induced suppression of glycogenolysis as well as gluconeogenesis. Diabetes. 2005;54:1942–1948. doi: 10.2337/diabetes.54.7.1942. [DOI] [PubMed] [Google Scholar]
- 45.Wallace TM, Levy JC, Matthews DR. Use and abuse of HOMA modeling. Diabetes Care. 2004;27:1487–1495. doi: 10.2337/diacare.27.6.1487. [DOI] [PubMed] [Google Scholar]
- 46.Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes. 2005;54:603–608. doi: 10.2337/diabetes.54.3.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carlson CL, Winder WW. Liver AMP-activated protein kinase and acetyl-CoA carboxylase during and after exercise. J Appl Physiol (1985) 1999;86:669–674. doi: 10.1152/jappl.1999.86.2.669. [DOI] [PubMed] [Google Scholar]
- 48.Haus JM, Solomon TPJ, Marchetti CM, et al. Decreased visfatin after exercise training correlates with improved glucose tolerance. Med Sci Sports Exerc. 2009;41:1255–1260. doi: 10.1249/MSS.0b013e318195bad5. [DOI] [PubMed] [Google Scholar]
- 49.DeFronzo RA. Pathogenesis of type 2 (non-insulin dependent) diabetes mellitus: a balanced overview. Diabetologia. 1992;35:389–397. doi: 10.1007/BF00401208. [DOI] [PubMed] [Google Scholar]
- 50.Cersosimo E, Solis-Herrera C, Trautmann ME, Malloy J, Triplitt CL. Assessment of pancreatic beta-cell function: review of methods and clinical applications. Curr Diabetes Rev. 2014;10:2–42. doi: 10.2174/1573399810666140214093600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dela F, von Linstow ME, Mikines KJ, Galbo H. Physical training may enhance beta-cell function in type 2 diabetes. Am J Physiol Endocrinol Metab. 2004;287:E1024–E1031. doi: 10.1152/ajpendo.00056.2004. [DOI] [PubMed] [Google Scholar]
- 52.Solomon TPJ, Haus JM, Kelly KR, Rocco M, Kashyap SR, Kirwan JP. Improved pancreatic beta-cell function in type 2 diabetic patients after lifestyle-induced weight loss is related to glucose-dependent insulinotropic polypeptide. Diabetes Care. 2010;33:1561–1566. doi: 10.2337/dc09-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kirwan JP, Kohrt WM, Wojta DM, Bourey RE, Holloszy JO. Endurance exercise training reduces glucose-stimulated insulin levels in 60- to 70-year-old men and women. J Gerontol. 1993;48:M84–M90. doi: 10.1093/geronj/48.3.m84. [DOI] [PubMed] [Google Scholar]
- 54.Solomon TPJ, Malin SK, Karstoft K, Kashyap SR, Haus JM, Kirwan JP. Pancreatic beta-cell function is a stronger predictor of changes in glycemic control after an aerobic exercise intervention than insulin sensitivity. J Clin Endocrinol Metab. 2013;98:4176–4186. doi: 10.1210/jc.2013-2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Madsen SM, Thorup AC, Overgaard K, Jeppesen PB. High intensity interval training improves glycaemic control and pancreatic beta cell function of type 2 diabetes patients. PloS One. 2015;10:e0133286. doi: 10.1371/journal.pone.0133286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Umpierre D, Ribeiro PAB, Schaan BD, Ribeiro JP. Volume of supervised exercise training impacts glycaemic control in patients with type 2 diabetes: a systematic review with meta-regression analysis. Diabetologia. 2013;56:242–251. doi: 10.1007/s00125-012-2774-z. [DOI] [PubMed] [Google Scholar]