Abstract
Objective
The progressive rise in demand on NHS emergency care resources is partly attributable to increases in attendances of children and older people. A quality gap exists in the care provision for the old and the young. The Five Year Forward View suggested new models of care but that the “answer is not one-size-fits-all”. This article discusses the urgent need for person-centred outcome measures to bridge the gap that exists between demand and provision.
Design
This review is based on evidence gathered from literature searching across several platforms using a variety of search terms to account for the obvious heterogeneity, drawing on key ‘think-tank' evidence.
Settings
Qualitative and quantitative studies examining approaches to caring for individuals at the extremes of age.
Participants
Individuals at the extremes of age (infants and older people).
Main Outcome Measures
Understanding similarities and disparities in the care of individuals at the extremes of age in an emergency and non-emergency context.
Results
There exists several similarities and disparities in the care of individuals at the extremes of age. The increasing burden of health disease on the economy must acknowledge the challenges that exist in managing patients in emergency settings at the extremes of age and build systems to acknowledge the traits these individuals exhibit.
Conclusion
Commissioners of services must optimise the models of care delivery by appreciating the similarities and differences between care requirements in these two large groups seeking emergency care.
Keywords: Elderly, infant, paediatric, geriatric, emergency care, health policy
Introduction
There has been a relentless rise in emergency care demands on the UK health system. This is manifest as overcrowding in emergency departments with increased waiting times and increased risk of adverse events including mortality.1 It is recognised that a large proportion of this increased demand is secondary to increases in attendances of children and older people. This article aims to describe the quality gap that exists in the care provision for the old and the young to allow providers and commissioners of services to consider how to better address the models of care delivery by appreciating the similarities and differences between care requirements in these two large groups seeking emergency care.
Methods
This review is based on evidence gathered from literature searching across several platforms using a variety of search terms to account for the obvious heterogeneity and drawing on key ‘think tank’ evidence provided by organisations including the King’s Fund and relevant national guidelines.
The challenge in numbers
A disproportionate share of health services is used in caring for older people, aged 65 years or more.2 Older people are increasingly attending emergency departments beyond what is expected from population ageing and this is seen in several countries and is projected to continue to increase.3–5 NHS England states long-term health conditions now take 70% of the health budget.6
In the UK, older adults currently represent 17% of the attendees and comprise 40% of the admissions to hospital.7 The Quality Watch A&E Report (2014) identified ‘attendances for those aged 85 and over increasing by nearly 20 per cent more than would be predicted by population growth alone’.8
An emergency department visit for an older person is often a ‘sentinel’ event, associated with functional decline and adverse outcomes.9 Older patients are more likely to be admitted during an emergency department visit and have longer hospital stays.10 After hospitalisation, they also experience functional decline resulting in reduced health-related quality of life and independence.11
While infants are less likely to experience harm following presentation to an emergency department, presentations are increasing at a dramatic rate. There exist, however, important associations between emergency department utilisation and poorer continuity of care outcomes for children. A large study of 46,097 children in the United States found lower continuity of primary care is associated with higher risk of emergency department utilisation and hospitalisation. This situation is becoming increasingly commonplace with increasing demands on precious primary care resources posed by an ageing population.12 The Royal College of Paediatrics and Child Health in their ‘Standards for Children and Young People in Emergency Care Settings’ identified ‘ever increasing attendances at emergency and urgent care settings’.13 In 2007-2008 there were over three million attendances by children (aged 0–16 years) at UK emergency departments.7 In 2013-2014, this figure was over four million (4,575,000).7
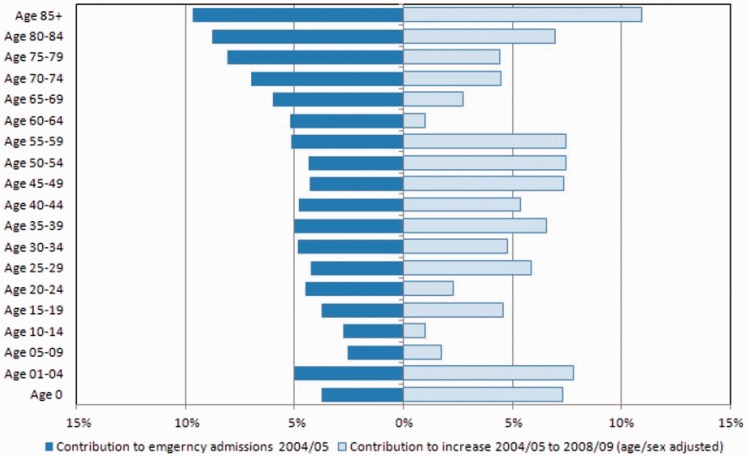
The Nuffield Trust published a report in 2010 titled ‘Trends in Emergency Admissions in England 2004–2009’.14 This provided data on the contributions to the number of emergency admissions in 2004-2005 and the increase between 2004-2005 and 2008-2009 by age band (Figure 1). This showed people aged over 85 years are nearly ten times more likely to have an emergency admission than someone in their 20s, 30s or 40s. Interestingly, it also noted a high rate of admission in the under-fives with this group contributing to a 7% overall increase between 2004 and 2009.14
Figure 1.
Contributions to the number of emergency admissions in 2004-2005 and the increase between 2004-2005 and 2008-2009, by age band. Source: Reproduced with permission from the Nuffield Trust.
The emergency admission rate for children under the age of 15 years in England has increased 28% in the last decade.15 The epidemiological data describe a year-on-year increase since 2003. Admissions for upper respiratory tract infections rose by 22%, lower respiratory tract infections by 40% and urinary tract infections by 43%.15 Similarly, Quality Watch A&E Report 2014 identified that ‘older people have much higher rates of A&E attendance than other groups (334 attendances per 1,000 population for those age 65 and over, compared with 253 for those under 65.’8 The explanation provided was the ‘rising numbers of frail older people with multiple long-term conditions’.8 They align with the widespread views that a focus on care in the community with increased measures for the vulnerable older people with long-term conditions.
Emergency care context
Geriatric patients frequent emergency departments more often than their younger counterparts with ‘distinct patterns of service use and care needs’.9 This study identified ‘current disease-orientated and episodic models of emergency care do not adequately respond to the complex care needs of frail older patients’.9 The Emergency Department is a key interface between primary and secondary care often an environment where ‘crises’ in health and social care are identified.16 The challenge that exists is highlighted by the requirement that ‘any urgent care service response to older people must be person focused and driven by individual needs’. Selected studies demonstrated that screening of high-risk patients is more efficient than age-based screening, and that comprehensive geriatric assessment (CGA) performed in the emergency department,17 followed by appropriate interventions, improved outcomes. Assessment and screening for frailty can predict outcomes as much as acute illness severity.18
There has been a constant increase in presentations of infants to Emergency and Acute care settings in the UK.15 The short-term duration of admissions has led many to question whether there has been a failure of primary care service provision or a change in parental expectation of disease processes. There is evidence, however, that objective acuity is remaining constant indicating a stable disease burden in keeping with population growth.19 A higher mortality in neonates and infants than other age groups suggests that care still needs to be improved for this vulnerable group.20
There is some evidence that provision of specific care pathways may contribute to improved outcomes for the old and the young. In the paediatric population, studies have investigated the use of clinical pathways for common paediatric emergency department presentations. These found positive parental response to use of pathways and lower re-presentation rates.21,22 Despite pathways having been identified in such studies as being ‘evidence-based’, they are not in widespread use and there are clear variations in care provided across many conditions.23
In contrast, care pathways for older people have focused on organising care post hip fractures. One large cohort study found a reduction in postoperative morbidity but no change in in-hospital mortality or cost of inpatient care. However, improvements in the ‘incidence of pressure ulcers, delirium, and health service utilisation’ were noted and are encouraging.24 Screening for falls and post-emergency department interventions interventions have been, likewise, associated with improved outcomes.25,26
Physiologic considerations
Older people and infants present with non-specific features of unwell being. Unwell babies can present with features including crying, poor feeding and altered behaviour which could be a manifestation of conditions which are diverse and can also range from trivial to life-threatening. These can include sepsis, cardiac pathology, intestinal colic or even a piece of mother’s hair twisted around the baby’s toe.
Likewise, frail older people present with falls, confusion, immobility or feeling generally unwell which can be manifestations of sepsis, heart failure, adverse drug effect or even constipation.
Assessment of pain in children who cannot express themselves verbally is based on physiologic parameters as in the Alder Hey Pain Scale.27 This is not dissimilar to using the Abbey scale in older people who cannot express their pain verbally due to speech impediment or confusion.28
Trauma: an ‘impact’ on young and old
In trauma care there are a number of similarities at the extremes of age. The UK’s trauma care system relies on prehospital recognition of major injury in order to identify which patients should be transported direct to a major trauma centre (prehospital triage) with a prealert to the major trauma centre which allows an immediate senior trauma team response and rapid treatment. The application of the prehospital trauma triage tool is often triggered by the paramedics seeing the mechanism of injury – if the patient is in a very smashed-up car, it is easy to ‘think trauma’.
However, at the extremes of age, major trauma has a different set of mechanisms (non-accidental injury in infants and a fall on the level in older people) which do not immediately give an indication that the patient might have serious injury (Trauma Audit and Research Network Reports 2012 and 2017). Communication of exactly what happened is often unclear in both infants and the elderly. This means that at the extremes of age, patients with major trauma are not identified in the prehospital phase and so are not taken to major trauma centres. Even in-hospital identification of major injuries is difficult in these patient groups so treatment continues in a non-specialist trauma unit, which do not have a trauma team reception, consultant-led care, or early investigation and are often thought to have a medical condition. Both infants and elderly people with major trauma are often identified on a medical ward (geriatric or paediatric).
Providing good quality care of these two groups of patients at the extremes of age involves the same set of changes to the current trauma care systems. Late identification is inevitable, as there is no early indication of major injury, so the systems and responses in the trauma unit rather than the major trauma centre are key to providing high quality care. Once the potential for serious injury is realised there needs to be a trauma team response wherever the patient is located in a similar way to the workings of a cardiac arrest team (i.e. anaesthetist, medical registrar, etc.) who are called for prompt and robust delivery of cardiopulmonary resuscitation. There is an argument for calling the trauma team (i.e. orthopaedic doctor, general surgeon, etc.) to a medical ward should there be potential for a serious injury. For both children and older people, the NHS trauma network system needs to acknowledge while a reliance on early identification of major injury for transfer direct to a major trauma centre benefits a significant proportion of patients, investment in staff and training in order to improve the ability of every, trauma unit to respond and give expert care to patients at the extremes of age is still relevant and needed.
Pharmacological considerations
Paediatrics and geriatric patients are distinct from other patient groups with respect to pharmacokinetics and pharmacodynamics. This difference often precipitates dose adjustments. However, studies addressing these important population traits are limited and, as a consequence, regulations have been established to prevent harm. In the older, ‘pharmacokinetics are strongly influenced by morbidity, co-morbidity, multiple drug use or reduced organ function’.29 This has led to the ICH Harmonised Tripartite Guideline: Studies in Support of Special Populations: Geriatrics E7 which describes the importance of robust preparatory work in geriatric volunteers with the disease. Unfortunately, there is a lack of generalisability to older patients in large-scale randomised control studies due to issues with recruitment, frailty and co-morbidity (e.g. statin studies in stroke secondary prevention, mean age 63, SD 0.2).30 Similarly, regulations were introduced in the paediatric populations to ‘ensure that medicines for use in children are of high quality, ethically researched and appropriately authorised’.29 The management of the well-appearing febrile neonate remains a challenge, and there is huge variation in the management of wheeze.31
The response
With the ever-increasing numbers of emergency admissions within acute hospitals, over 65-year-olds represent a significant proportion. Geriatricians have long adopted a biopsychosocial approach in the form of Comprehensive Geriatric Assessment. Since its origins in the 1980s, Comprehensive Geriatric Assessment has attempted to meet the ‘medical, social, functional or psychological needs of this high-risk group’. In recent times, there is strong evidence it is working with Comprehensive Geriatric Assessment increasing the likelihood of older patients being alive or in their own home by 12 months.32 Older people need an assessment framework that takes into account their varying needs before, during and after a crisis. Comprehensive Geriatric Assessment allows care to be tailored to the individual older person and offers the best outcomes.
The Common Assessment Framework in children is a similar framework that addresses holistic needs to better the growth and development in children that addresses the five priorities of ‘Every Child Matters’ (be healthy, stay safe, enjoy and achieve, make a positive contribution, achieve economic wellbeing).33 This policy is designed to eradicate child poverty by 2020, create a world class skill base by 2020 and ultimately build more cohesive, empowered and active communities moving forward.33
Non-emergency comparisons
The King’s Fund highlights discrimination that exists within UK screening programmes.34 However, they acknowledge the ‘extent of local, discretionary or covert age barriers to care is difficult to assess and less open to debate’.34 There is a paucity of studies on screening in older people and there is a lack of current guidelines reporting upper limits (abdominal aortic aneurysm screening is for those aged 65 years and upwards). Interestingly, in the rare circumstances where upper limits have been applied, the UK Colorectal Cancer Screening Pilot and the Danish faecal occult blood screening pilot, poor uptake over 70 years of age and large numbers of missed detectable cancers were identified issues.35 The Five Year Forward View suggests ‘enhanced health in care homes’ as a method of avoiding admissions to hospitals for those with dementia. This population can be hard to engage with and very few robust methods of proactive assessment currently exist to identify those most in need to healthcare professional input in homes before deterioration.
Unlike geriatric populations where screening programmes are invariably extended to older patients, the paediatric populations have well-developed screening programmes targeting a range of inherited disorders. An example is the school hearing programmes, established to examine for a range of hearing impairments in school-age children (four to five years of age). A questionnaire-based study found barriers to follow-up that included ‘children who are unwilling or unable to co-operate, had high non-attendance (23%)’.36 Interestingly, the authors highlight barriers based on screening often being conducted in the absence of carers and a lack of parental concern and understanding precipitating non-attendance at follow-up assessments.
Clearly there is a difference in the challenges in screening these two populations with diverse barriers identified. The significant complexity that exists is multifactorial and factors include biopsychosocial versus single complaints, non-specific presentations, access issues and dependency on carers.
Recently an outcomes standard set was published that addressed patient- and service-reported outcomes in older people.37 This represents an attempt to reduce variation in care provision by suggesting alignment of commissioning and provisioning arrangements based on what matters to older people. This is person-centred care and the underpinning methodology, value-based healthcare delivery, incorporates cost-effectiveness in care.38
No such dataset exists for children although there are those for specific conditions such as for children requiring cleft palate repair.39 These hold early promise and parent-reported outcomes including carer burden are likely to be as important in this group as in the older peoples’ standard set.
Summary
In summary, there are several similarities and disparities in the care of individuals at the extremes of age. The Five Year Forward View suggested new models of care but that the ‘answer is not one-size-fits-all’.6 Although the reference is to the geographical challenge, it is as pertinent to the population being served and there is a real need for person-centred outcome measures to bridge the gap that exists between demand and provision. The increasing burden of health disease on the economy must acknowledge the challenges that exist in managing patients in emergency settings at the extremes of age and build systems to acknowledge the traits these individuals exhibit.
It has been said that ‘the moral test of government is how it treats those who are in the dawn of life, the children; those who are in the twilight of life, the aged; and those in the shadows of life, the sick, the needy and the handicapped’. 40 By recognising the needs of the older person, we are acknowledging it is ‘the most vulnerable who will have most to lose from systems that are unsafe or inadequately designed to address their needs’.17 This moral argument is also an ethical basis for understanding and providing similarities in approaches for caring for people at the extremes of age. The health service could learn from the work done in these groups and address person-centeredness for all patients which can only improve outcomes by addressing demand on an individual basis.
Declarations
Competing Interests
None declared.
Funding
There was no funding or sponsorship of this manuscript. JSM is supported by a Dunhill Medical Trust Research Training Fellowship (RTF97/0117).
Ethics approval
Not required for this study as the review focussed on published literature and did not include any patient recruitment
Guarantor
JSM and DR
Contributorship
JSM, JB and DR had the idea for the article. JSM, DM, TC, JB and DR wrote the article, and JSM and DR are guarantors for the article.
Acknowledgements
None
Provenance
Not commissioned; peer-reviewed by Syed Shahzad
References
- 1.Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust 2006; 184: 208–212. [DOI] [PubMed] [Google Scholar]
- 2.Australian Government. Australia to 2050: Future Challenges. The 2010 Intergenerational Report Overview, Australia: Commonwealth of Australia, 2010.
- 3.Lowthian JA, Jolley DJ, Curtis AJ, Currell A, Cameron PA, Stoelwinder JU, et al. The challenges of population ageing: accelerating demand for emergency ambulance services by older patients, 1995–2015. Med J Aust 2011; 194: 574–578. [DOI] [PubMed] [Google Scholar]
- 4.Lowthian JA, Curtis AJ, Jolley DJ, Stoelwinder JU, McNeil JJ, Cameron PA. Demand at the emergency department front door: 10-year trends in presentations. Med J Aust 2012; 196: 128–132. [DOI] [PubMed] [Google Scholar]
- 5.Lowthian J, Curtis A, Stoelwinder J, McNeil J, Cameron P. Emergency demand and repeat attendances by older patients. Intern Med J 2013; 43: 554–560. [DOI] [PubMed] [Google Scholar]
- 6.NHS England. NHS Five Year Forward View, United Kingdom: NHS England, 2014.
- 7.NHS Digital Hospital Episode Statistics 2016. Hospital Episode Statistics (last checked 16 November 2016), http://content.digital.nhs.uk/hes.
- 8.Blunt I. Focus On: A&E attendances. London: The Health Foundation & Nuffield Trust, 2014.
- 9.Aminzadeh F, Dalziel WB. Older adults in the emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 2002; 39: 238–247. [DOI] [PubMed] [Google Scholar]
- 10.McCusker J, Bellavance F, Cardin S, Trepanier S, Verdon J, Ardman O. Detection of older people at increased risk of adverse health outcomes after an emergency visit: the ISAR screening tool. J Am Geriatr Soc 1999; 47: 1229–1237. [DOI] [PubMed] [Google Scholar]
- 11.Covinsky KE, Palmer RM, Fortinsky RH, Counsell SR, Stewart AL, Kresevic D, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 2003; 51: 451–458. [DOI] [PubMed] [Google Scholar]
- 12.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics 2001; 107: 524–529. [DOI] [PubMed] [Google Scholar]
- 13.Intercollegiate Committee for Royal College of Paediatrics and Child Health. Standards for Children and Young People in Emergency Care Settings. London: Royal College of Paediatrics and Child Health, 2010.
- 14.Blunt I, Bardsley M and Dixon J. Trends in Emergency Admissions in England 2004–2009. London: Nuffield Trust, 2010.
- 15.Gill PJ, Goldacre MJ, Mant D, Heneghan C, Thomson A, Seagroatt V, et al. Increase in emergency admissions to hospital for children aged under 15 in England, 1999–2010: national database analysis. Arch Dis Child 2013; 98: 328–334. [DOI] [PubMed] [Google Scholar]
- 16.Banerjee J, Conroy SP and O’Leary V. The Silver Book: Quality Care for Older People with Urgent and Emergency Care Needs. London: British Geriatrics Society, 2012, http://www.bgs.org.uk/silverbook/campaigns/silverbook (last checked 16 November 2016).
- 17.Ellis G, Marshall T, Ritchie C. Comprehensive geriatric assessment in the emergency department. Clin Interv Aging 2014; 9: 2033–2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romero-Ortuno R, Wallis S, Biram R, Keevil V. Clinical frailty adds to acute illness severity in predicting mortality in hospitalized older adults: an observational study. Eur J Intern Med 2016; 35: 24–34. [DOI] [PubMed] [Google Scholar]
- 19.Roland D, Jones S, Coats T and Davies F. Are increasing volumes of children and young people presenting to Emergency Departments due to increasing severity of illness? Acad Emerg Med (ICEM 2016 Abstracts) 2016; 24: 503-504.
- 20.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 2010; 375: 1969–1987. [DOI] [PubMed] [Google Scholar]
- 21.Norton SP, Pusic MV, Taha F, Heathcote S, Carleton BC. Effect of a clinical pathway on the hospitalisation rates of children with asthma: a prospective study. Arch Dis Child 2007; 92: 60–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Browne GJ, Giles H, McCaskill ME, Fasher BJ, Lam LT. The benefits of using clinical pathways for managing acute paediatric illness in an emergency department. J Qual Clin Pract 2001; 21: 50–55. [DOI] [PubMed] [Google Scholar]
- 23.NHS RightCare. NHS Atlas of Variation in Healthcare of Children and Young People, United Kingdom: NHS England. 2012.
- 24.Beaupre LA, Cinats JG, Senthilselvan A, Lier D, Jones CA, Scharfenberger A, et al. Reduced morbidity for elderly patients with a hip fracture after implementation of a perioperative evidence-based clinical pathway. Qual Saf Health Care 2006; 15: 375–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET: a randomised controlled trial). Lancet 1999; 353: 93–97. [DOI] [PubMed] [Google Scholar]
- 26.Caplan GA, Williams AJ, Daly B, Abraham K. A randomized, controlled trial of comprehensive geriatric assessment and multidisciplinary intervention after discharge of elderly from the emergency department – the DEED II study. J Am Geriatr Soc 2004; 52: 1417–1423. [DOI] [PubMed] [Google Scholar]
- 27.Stewart B, Lancaster G, Lawson J, Williams K, Daly J. Validation of the Alder Hey Triage pain score. Arch Dis Child 2004; 89: 625–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abbey J, Piller N, De Bellis A, Esterman A, Parker D, Giles L, et al. The Abbey pain scale: a 1-minute numerical indicator for people with end-stage dementia. Int J Palliat Nurs 2004; 10: 6–13. [DOI] [PubMed] [Google Scholar]
- 29.Hanning SM, Lopez FL, Wong IC, Ernest TB, Tuleu C and Orlu Gul M. Patient centric formulations for paediatrics and geriatrics: Similarities and differences. Int J Pharm 2016; 512: 355–359. [DOI] [PubMed]
- 30.Amarenco P, Bogousslavsky J, Callahan A, 3rd, Goldstein LB, Hennerici M, Rudolph AE, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med 2006; 355: 549–559. [DOI] [PubMed] [Google Scholar]
- 31.Lyttle MD, O’Sullivan R, Doull I, Hartshorn S, Morris I, Powell CV, et al. Variation in treatment of acute childhood wheeze in emergency departments of the United Kingdom and Ireland: an international survey of clinician practice. Arch Dis Child 2015; 100: 121–125. [DOI] [PubMed] [Google Scholar]
- 32.Ellis G, Whitehead MA, Robinson D, O’Neill D, Langhorne P. Comprehensive geriatric assessment for older adults admitted to hospital: meta-analysis of randomised controlled trials. BMJ 2011; 343: d6553–d6553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Department of Education, United Kingdom: HM Treasury, UK Government. Every Child Matters, 2003.
- 34.The King’s Fund. Briefing Note: Age Discrimination in Health and Social Care. See www.kingsfund.org.uk (2000, last checked 16 November 2016).
- 35.British Geriatrics Society. Screening For Cancer in Older People. See www.bgs.org.uk/pdf_cms/bpg/bpg_cancer_screening.doc. 2010, last checked 16 November 2016).
- 36.Fonseca S, Forsyth H, Neary W. School hearing screening programme in the UK: practice and performance. Arch Dis Child 2005; 90: 154–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.International Consortium for Health Outcomes Measurement. Older Person Reference Guide Version 1.0, USA: International Consortium for Health Outcomes Measurement, 2017.
- 38.Porter ME. What is value in health care? N Engl J Med 2010; 363: 2477–2481. [DOI] [PubMed] [Google Scholar]
- 39.International Consortium for Health Outcomes Measurement. Cleft Lip and Palate Data Collection Reference Guide Version 3.0. USA: International Consortium for Health Outcomes Measurement, 2017.
- 40.Congressional Record. Remarks at the Dedication of the Hubert H. Humphrey Building. 123rd edn. 1977:37287.