Abstract
Background:
Female patients are more likely to suffer a second anterior cruciate ligament (ACL) injury after ACL reconstruction (ACLR) and return to sport (RTS) compared with healthy female controls. Few studies have examined the energy absorption contribution (EAC) that could lead to this subsequent injury.
Hypothesis:
The ACLR group would demonstrate an altered EAC between joints (hip, knee, and ankle) but no difference in quadriceps, hip abduction, or hip external rotation (ER) strength at the time of RTS.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
A total of 34 female participants (ACLR: n = 17; control: n = 17) were enrolled in the study and matched for age and activity level. Jump landing performance for the initial 50 milliseconds of landing of a lateral-vertical jump was assessed using a 10-camera 3-dimensional motion capture system and 2 force plates. Isokinetic quadriceps strength was measured using a Biodex machine, and hip abduction and ER isometric strength were measured using a handheld dynamometer. All values were normalized to the participant’s height and weight. A 1-way multivariate analysis of variance was used to assess between-group differences in the EAC at the hip, knee, and ankle. Two 1-way analyses of variance were used to independently examine quadriceps, hip abduction, and hip ER strength between the groups.
Results:
Significant differences in the EAC were found between the groups for the involved hip (P = .002), uninvolved hip (P = .005), and involved ankle (P = .023). There were no between-group differences in the EAC for the involved or uninvolved knee or the uninvolved ankle. Patients who underwent ACLR demonstrated significantly decreased quadriceps strength on the involved limb (P = .02) and decreased hip ER strength on both the involved (P = .005) and uninvolved limbs (P = .002). No significant strength differences were found between the groups for the uninvolved quadriceps or for involved or uninvolved hip abduction.
Conclusion:
At RTS, patients who underwent ACLR utilized a greater hip EAC bilaterally and a decreased involved ankle EAC during a lateral-vertical jump. Furthermore, quadriceps strength on the involved limb and hip ER strength of bilateral lower extremities remained decreased. This could place greater stress on the ACL graft and ultimately lead to an increased injury risk.
Keywords: female athlete, ACL, energy absorption, biomechanics, return to sport
Over 250,000 anterior cruciate ligament (ACL) injuries occur annually, with a majority arising in young athletes.24 While the incidence of ACL injuries is common across both sexes, female athletes are 4 to 6 times more likely to suffer an ACL injury compared with their male counterparts in the same sports.1,14 Furthermore, female patients are 5 times more likely to suffer a second ACL injury after ACL reconstruction (ACLR) and return to sport (RTS) compared with healthy female controls.25 These ACL tears are often noncontact injuries resulting from faulty biomechanics during decelerating, landing, and pivoting tasks.14
Numerous studies have looked prospectively at various biomechanical measures and risk factors for ACL injuries. Hewett et al14 were one of the first to delineate biomechanical differences between healthy female controls and those who suffered subsequent ACL injuries. The authors found an increase in the knee abduction angle and knee abduction external moment at both initial contact and maximal displacement during vertical jump landing.14 Similarly, Paterno et al26 detailed 4 biomechanical predictors of a second ACL injury during vertical drop landing: uninvolved hip internal rotation in the initial 10% of landing, frontal-plane knee abduction motion, side-to-side differences in sagittal-plane knee flexion moment at initial contact, and postural stability, as measured by single-leg balance, on the ipsilateral limb. Furthermore, decreased knee flexion angle at initial contact has been found to increase the rate of ACL strain, while decreased hip and trunk flexion angles result in maximum ACL strain magnitude during single-leg forward jump landing.2 These results suggest that ACL strain increases with sagittal-plane landing and deceleration maneuvers, which may place the athlete at a greater risk for injuries; however, more information is warranted with regard to the biomechanical forces across the ACL during sport-specific movements.
Most biomechanical studies and RTS test batteries are limited by the fact that the results examine only sagittal-plane tasks.4,12,21 However, high-risk sports are not uniplanar; therefore, there is a need to examine multiple planes of motion. The few studies that have been published show differences in jump landing biomechanics between the sagittal and frontal planes.32,33,35 Taylor et al35 demonstrated decreased hip and knee flexion angles as well as increased hip adduction and internal rotation and knee abduction moment with double-leg forward versus lateral landing. Sinsurin et al32 also found decreased hip flexion angles in addition to increased ankle dorsiflexion angles with frontal-plane jump landing, which were not present with sagittal-plane jump landing. Furthermore, Sinsurin et al33 showed increased peak knee valgus angles with single-leg lateral and diagonal jump landing compared with forward jump landing. The finding of increased knee valgus during a jump landing task has been shown to be a key predictor of ACL injuries.14,26
Additionally, Zazulak et al37 found that female patients demonstrated poor trunk control and excessive lateral trunk displacement after a sudden force release that mimicked an athletic perturbation, which was a key predictor of knee ligament injuries. Powers28 further described how poor frontal-plane trunk and pelvic stability, primarily contralateral pelvic drop and increased hip adduction angles, increases varus moment at the knee secondary to weak hip abductors. This is consistent with a recent study by Khayambashi et al15 indicating that hip external rotation (ER) strength of ≤20.3% body weight (BW) or hip abduction strength of ≤35.4% BW independently predicted competitive athletes at high risk for noncontact ACL injuries. Numerous studies have correlated decreased hip extension, ER, and abduction strength to increased knee valgus motion during single-leg landing tasks in female patients.18,34 While these studies are integral for understanding biomechanical factors that increase ACL strain, they do not provide insight into potential movement compensation strategies employed by other joints.
Energy absorption has previously been described as a means of using both kinematic and kinetic data to estimate lower extremity muscle activity–producing movements throughout the entire landing activity.22,23 Previous studies have found an altered energy absorption contribution (EAC) from the hip, knee, and ankle during a drop landing task.7,22,23 Participants who were classified as having high energy absorption demonstrated alterations in both sagittal- and frontal-plane mechanics, most notably greater knee extension moment, anterior tibial shear force, peak ground-reaction force, knee valgus angle, and knee varus moment.22,23 These altered landing techniques are more prevalent in female athletes during the first 50 milliseconds of landing16 and are associated with increased loading on passive tissues such as the ACL, thus increasing the risk for injuries. Therefore, looking at both hip strength and lower extremity biomechanics during a functional lateral movement may be more revealing for elucidating biomechanical and energy absorption deficits that contribute to increased ACL injuries.
The primary purpose of this case-control study was to identify potential biomechanical differences in the EAC during the initial 50 milliseconds of landing a lateral-vertical jump (LVJ) between patients who underwent ACLR and healthy age- and activity-matched controls at the time of RTS. Between-limb asymmetries were not examined because of previous research that has shown bilateral changes in strength and neuromuscular control after ACLR.3,11,13,19,25 As such, we found it more compelling to compare patients who underwent ACLR with matched healthy controls as a way to eliminate the possibility of a type II error in which no difference was found because of changes bilaterally. We hypothesized that the ACLR group would demonstrate an altered EAC between joints (hip, knee, and ankle) at the time of RTS compared with matched controls. A secondary aim of the study was to compare normalized isometric quadriceps and gluteal strength between patients who underwent ACLR and healthy age- and activity-matched controls at the time of RTS. We hypothesized that participants who completed the rehabilitation process after ACLR would demonstrate lower normalized quadriceps strength and no differences in normalized isometric hip abduction or ER strength at the time of RTS compared with healthy matched controls.
Methods
Participants
A total of 34 female athletes volunteered to participate in this study. Seventeen participants with a history of ACLR (14.7 ± 1.0 years) at the time of RTS (ACLR group) were compared with 17 age- (14.5 ± 1.1 years), activity-, and limb-matched healthy controls (control group). A summary of demographics for the participants is listed in Table 1. Participants in both groups were considered for the study if they were between the ages of 13 and 25 years and were involved in a level 1 sport (involving cutting, planting, pivoting, jumping, and landing) for at least 50 h/y.6 Participants in the ACLR group were considered if they sustained a first-time ACL injury and had none of the following concomitant injuries: full-thickness chondral defect of ≥1 cm2, grade II or III medial collateral ligament or lateral collateral ligament sprain, posterior cruciate ligament tear (grade III), or simultaneous fracture with an ACL tear.
TABLE 1.
Participant Demographicsa
| ACLR (n = 17) | Control (n = 17) | P Value | |
|---|---|---|---|
| Age, y | 14.7 ± 1.0 | 14.5 ± 1.1 | .52 |
| Height, cm | 164.4 ± 6.2 | 163.5 ± 7.2 | .71 |
| Weight, kg | 64.7 ± 10.6 | 56.8 ± 6.6 | .014 |
aValues are presented as mean ± SD. ACLR, anterior cruciate ligament reconstruction.
Time of RTS was defined as the time at which participants had met criteria for the completion of physical therapy and had begun their RTS progression with the team. Criteria for the completion of physical therapy included passing the following objective criteria: (1) symmetrical knee range of motion (ROM), (2) limb symmetry index (LSI) ≥90% on the Y Balance Test, (3) <4-cm side-to-side difference in anterior reach for the Y Balance Test, (4) passing score (46/54) on the Vail Sport Test, (5) LSI ≥90% on the single hop for distance, and (6) LSI ≥90% on the single-leg triple hop for distance. Participants in the control group were considered for study inclusion if they scored ≥95 on the International Knee Documentation Committee (IKDC) form and did not experience any lower extremity orthopaedic injuries within 3 months before testing.
After the screening process, eligible participants were invited to take part in the study. All participants gave informed consent, and the rights of each person were protected. If the participant was a minor, parental permission and child assent were obtained. The institutional review board of Texas Health Resources approved all research procedures.
After enrollment in the study, information regarding injury history and athletic involvement was collected from each participant. Height and weight were measured for each participant using a Weigh Beam eye-level scale (Detecto).
3-Dimensional Motion Analysis
Retroreflective markers were attached to the spinous process of the seventh cervical vertebra, twelfth thoracic vertebra, between the fourth and fifth lumbar vertebrae, sternum, bilateral acromion process, anterior superior iliac spine, posterior superior iliac spine, greater trochanter, anterior thigh, medial and lateral epicondyles of the femur, anterior shank, medial and lateral malleoli, calcaneus, and first and fifth metatarsal heads. Three additional retroreflective markers were attached on the sacrum as a cluster. All markers were attached to the participant with double-sided tape.
Three-dimensional videos were collected for each task. The Qualisys motion capture system with 10 Oqus cameras (Qualisys) was used to collect 3-dimensional coordinates of reflective markers attached to the participant at a sampling rate of 120 Hz. Two force plates (AMTI) were used to collect ground-reaction forces at a sampling rate of 1200 Hz. The kinematic data and force plate data were time synchronized. After completion of the static trial, markers of the medial femoral epicondyle, medial malleolus, and bilateral anterior superior iliac spine were removed, and participants performed the LVJ.
Lateral-Vertical Jump
Participants began the LVJ task by standing to the side of the force plate at a distance equal to 50% of their height with the testing leg closest to the force plate. Participants were asked to hop onto the force plate by pushing off the ground with their nontesting leg, land with the testing leg on the force plate, and then immediately perform a maximal vertical jump and land back onto the force plate with their testing leg (Figure 1). Immediately after landing on the force plate, the participants were required to stabilize themselves on the force plate for approximately 2 seconds. Participants performed 3 trials on each limb. Trials were excluded and repeated if the participant’s entire foot did not make contact with the force plate, if the nontesting leg made contact with the ground or force plate upon landing or immediately after, or if the participant did not maintain balance.
Figure 1.
Lateral-vertical jump maneuver.
Data Processing and Reduction
Three-dimensional joint coordinates were estimated from the trajectories of the reflective markers. All kinematic and kinetic data were exported into Visual3D software (C-Motion) to process and reduce data. The kinematic and force data were filtered via a fourth-order low-pass Butterworth filter with a zero-phase lag at 10 Hz. The lower extremity joint angles were calculated using an inverse kinematic approach, and the lower extremity internal moment was calculated using an inverse dynamic approach. The EAC was calculated by integrating the negative part of the power curve where joint angular velocity and net joint moment are in opposite directions, indicating eccentric loading22,23 during the first 50 milliseconds from initial contact of the second landing of the LVJ. The EAC for each joint was normalized to the product of height and weight and averaged across 3 trials.
Hip Muscle Strength
Isometric hip strength was measured in abduction and ER. These directions were chosen because weaknesses in these movements have been studied as possible contributing factors to ACL injuries.10,37 All measurements were taken using the ‘‘break test’’ method with a handheld dynamometer (MicroFET 2; Hoggan Scientific).36 A handheld dynamometer, rather than the Biodex system, was selected for assessing hip muscle strength because of time constraints involved with the clinical nature of the study. In addition, the use of a handheld dynamometer to determine hip muscle strength was the standard clinical testing protocol at the affiliated institution. Measurements were taken by 3 physical therapists to ensure consistency. In addition, a pilot reliability study was performed on 10 healthy participants who were included in the control group. The interrater reliability was found to be good for hip abduction (intraclass correlation coefficient [ICC], 0.96; 95% CI, 0.85-0.98) and hip ER (ICC, 0.87; 95% CI, 0.59-0.97). For each direction, 2 consistent trials (±3 lb) were completed on each limb, with a 30-second rest between each consecutive trial. The average of the 2 trials was used for data analysis, and all measurements were normalized to BW.
For each hip muscle strength test, a belt was used to stabilize the participants’ pelvis. In addition, the clinician provided stabilization to control any accessory movements at the pelvis. The clinician instructed the participant to push maximally into the dynamometer for a duration of 3 to 5 seconds. For hip abduction, participants were placed in a side-lying position. The limb that was closest to the table was placed in approximately 30° of hip flexion with 90° of knee flexion.15,34 The participant’s testing limb was taken into a neutral position (relative to abduction/adduction) and slight hip extension with the knee fully extended. The dynamometer was placed immediately distal to the participant’s tibiofemoral joint line.
Hip ER was measured in a prone position, and the knee of the testing limb was flexed to 90°.15,34 The tester stood on the opposite side of the testing limb to apply appropriately directed pressure. The dynamometer was placed at the superior portion of the medial malleolus of the testing limb.
Biodex Testing
The Multi-Joint Testing and Rehabilitation System (Biodex Medical Systems) was used for testing isokinetic quadriceps muscle strength. Participants were seated on the Biodex system and secured with padded straps around the thigh, pelvis, and torso to minimize accessory and compensatory movements during testing.9,17 The femoral condyle of the testing limb was aligned with the Biodex axis of rotation following the manufacturer’s instructions. Participants performed 5 repetitions of submaximal knee extension/flexion to familiarize themselves with the testing motion. To determine knee strength for both the quadriceps and hamstring muscles, participants performed 5 consecutive concentric contractions at 60 deg/s on each limb.5 Finally, the average of the 5 trials was normalized to BW and used for data analysis.17
Statistical Analysis
For all variables, the injured limb of the ACLR group was matched to the limb of the control group based on the side of dominance. The dominant limb was defined as the limb that the participant reported she would choose to kick a ball. All data analyses were performed using SPSS version 23 (IBM). To compare the characteristics of the participants between the 2 groups, independent t tests were used to examine age, height, and weight. A 1-way multivariate analysis of variance was used to assess between-group differences in the EAC at the hip, knee, and ankle. Two 1-way analyses of variance were used to independently compare normalized quadriceps strength and normalized hip abduction and ER strength between the groups. The alpha level was set at P < .05 for all statistical analyses.
Results
Table 1 displays the characteristics between the groups. There were no significant differences in age (P = .52) or height (P = .71) between the groups; however, there was a significant difference between the groups with regard to weight (ACLR: 64.7 ± 10.6 kg; control: 56.8 ± 6.6 kg; P = .014). The mean RTS time was 7.3 months from ACLR.
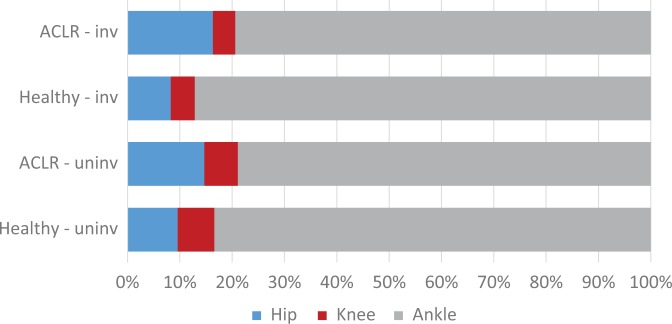
For the EAC during the first 50 milliseconds, there were significant differences between the groups in the involved hip EAC (ACLR: 16.3% ± 8.9%; control: 8.3% ± 4.7%; P = .002) and the uninvolved hip EAC (ACLR: 14.7% ± 4.8%; control: 9.6% ± 5.1%; P = .005). There were no significant differences in the EAC at the involved (P = .86) or uninvolved (P = .86) knee. At the involved ankle, significant between-group differences were seen in the EAC (ACLR: 79.4% ± 8.1%; control: 87.1% ± 10.6%; P = .023), while no differences were seen in the uninvolved ankle EAC (P = .31) (Table 2 and Figure 2).
TABLE 2.
Energy Absorption Contribution for Lateral-Vertical Jump Maneuvera
| ACLR (n = 17) | Control (n = 17) | P Value | |
|---|---|---|---|
| Hip | |||
| Involved | 16.34 ± 8.88 | 8.27 ± 4.70 | .002b |
| Uninvolved | 14.72 ± 4.75 | 9.59 ± 5.11 | .005b |
| Knee | |||
| Involved | 4.25 ± 4.80 | 4.59 ± 6.46 | .864 |
| Uninvolved | 6.35 ± 8.30 | 7.02 ± 13.28 | .862 |
| Ankle | |||
| Involved | 79.41 ± 8.09 | 87.14 ± 10.59 | .023b |
| Uninvolved | 78.93 ± 9.12 | 83.39 ± 15.30 | .310 |
aValues are presented as mean ± SD. ACLR, anterior cruciate ligament reconstruction.
bP < .05.
Figure 2.
Energy absorption contribution for lateral-vertical jump maneuver. ACLR, anterior cruciate ligament reconstruction; inv, involved; uninv, uninvolved.
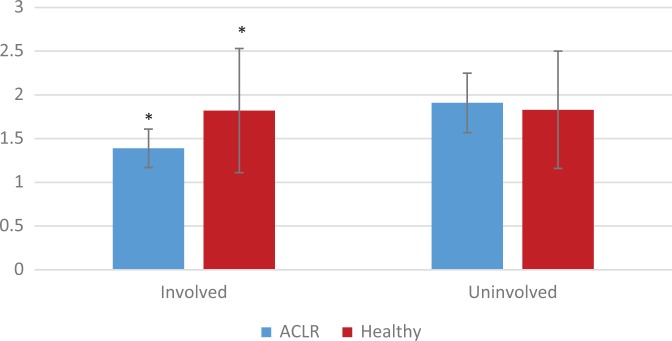
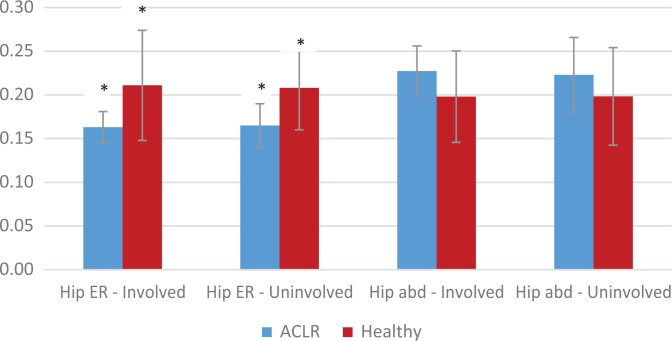
Normalized quadriceps strength was significantly decreased (P = .02) on the involved limb of the ACLR group (1.39 ± 0.23 N·m/kg) compared with the matched limb of the control group (1.82 ± 0.71 N·m/kg). No differences (P = .65) in normalized quadriceps strength were found on the uninvolved limb in the ACLR group (1.91 ± 0.34 N·m/kg) or the matched limb of the control group (1.83 ± 0.67 N·m/kg). At the hip, the ACLR group demonstrated significantly lower normalized hip ER strength on the involved (0.16 ± 0.02 kg/BW; P = .005) and uninvolved (0.17 ± 0.03 kg/BW; P = .002) limbs when compared with the involved (0.21 ± 0.06 kg/BW) and uninvolved (0.21 ± 0.05 kg/BW) limbs of the control group. For hip abduction strength, there were no significant differences between the groups in the involved (P = .053) or uninvolved (P = .157) limb (Table 3).
TABLE 3.
Knee and Hip Strength Measurementsa
| ACLR (n = 17) | Control (n = 17) | P Value | |
|---|---|---|---|
| Knee extension, peak torque/BW | |||
| Involved | 1.39 ± 0.23 | 1.82 ± 0.71 | .02b |
| Uninvolved | 1.91 ± 0.34 | 1.83 ± 0.67 | .65 |
| Hip external rotation, kg/BW | |||
| Involved | 0.16 ± 0.02 | 0.21 ± 0.06 | .005b |
| Uninvolved | 0.17 ± 0.03 | 0.21 ± 0.05 | .002b |
| Hip abduction, kg/BW | |||
| Involved | 0.23 ± 0.03 | 0.20 ± 0.05 | .053 |
| Uninvolved | 0.22 ± 0.04 | 0.20 ± 0.06 | .157 |
aValues are presented as mean ± SD. ACLR, anterior cruciate ligament reconstruction; BW, body weight.
bP < .05.
Discussion
The purpose of this study was to identify differences in the EAC between patients who underwent ACLR compared with healthy age-, limb-, and activity-matched controls. At the time of RTS, participants after ACLR utilized a greater hip and decreased ankle EAC during an LVJ maneuver on the involved limb as well as a greater hip EAC on the uninvolved limb (Table 2 and Figure 2). Furthermore, quadriceps strength on the involved limb and ER strength of bilateral lower extremities remained decreased compared to healthy controls at the time of RTS (Table 3).
The primary findings of the current study support the initial hypothesis that the ACLR group employs different EAC strategies compared to healthy controls during an athletic frontal-plane maneuver. On the involved limb, the EAC from the hip was 2 times greater for the ACLR group and over 1.5 times greater on the uninvolved limb for the ACLR group compared to healthy controls’ involved and uninvolved limbs, respectively. These results demonstrate that patients after ACLR may utilize larger hip contribution to eccentrically decelerate the body to dissipate kinetic energy during the initial 50 milliseconds of the landing phase, which may place increased loads on the ACL. These findings are consistent with results from the studies of Norcross et al,22,23 which classified patients into high, moderate, and low energy absorption groups based on landing strategies that could potentially place greater stress on the ACL. Those who were classified into the high energy absorption group22,23 utilized frontal-plane movement strategies similar to the current findings that suggest greater potential loading to the ACL.
Furthermore, participants in the ACLR group demonstrated a decreased ankle EAC on the involved limb compared with controls; however, there were no differences in the ankle EAC for the uninvolved limb. This may also be caused by changes in neuromuscular control patterns in an attempt to decrease the amplitude of multiple joint movements to minimize degrees of freedom.30 This movement strategy may be employed if there is a lack of strength and/or lack of movement control to direct attention to a smaller number of locations throughout the body. These alterations in the EAC at the hip and ankle demonstrate the difference in neuromuscular control patterns after ACLR.
Despite the EAC differences found in the ankle and hip, no differences in the knee EAC existed between the groups. This finding is in contrast to previous research that demonstrated decreased knee extensor moments, knee flexion angular velocities, rates of knee extensor moments, and knee power absorption in the ACLR limb.29,31 These findings point to a decreased capacity to absorb loads across the reconstructed knee compared with healthy controls. One of the reasons that this may occur is because of a lack of quadriceps strength or overall decreased neuromuscular control hindering the participant from utilizing underlying strength. The current study showed deficits in the involved limb’s quadriceps strength, despite the fact that the EAC at the knee between the groups was similar. This may point to patients in the ACLR group possibly having neuromuscular interruptions that limit their ability to effectively use the surrounding knee musculature in an efficient manner.11,19 However, these hypotheses are beyond the scope of the current study.
Our secondary hypothesis was not supported; at the time of RTS, patients who underwent ACLR continued to demonstrate deficits in isokinetic quadriceps strength (Figure 3) and isometric hip ER strength (Figure 4), compared with age- and activity-matched controls, even when normalized to BW. These findings are consistent with previous studies demonstrating that quadriceps inhibition can persist for up to 2 years after ACLR.3,13 Khayambashi et al15 demonstrated that decreased hip abduction and ER strength significantly increased the risk of noncontact ACL injuries in competitive male and female athletes. While there is limited evidence regarding hip ER strength after ACLR, numerous studies have shown decreased hip abduction and extension strength after ACLR27; thus, it is not surprising that hip ER strength would also be diminished. Despite a mean RTS time of 7.3 months, these results show that the strength deficits may continue to persist long after the injury.
Figure 3.
Knee extension strength normalized to body weight. *P < .05. ACLR, anterior cruciate ligament reconstruction.
Figure 4.
Hip strength normalized to body weight. *P < .05. abd, abduction; ACLR, anterior cruciate ligament reconstruction; ER, external rotation.
Although there was no significant difference in the knee EAC between the groups, the decreased quadriceps strength likely induces a change in neuromuscular control strategies, which results in an increased EAC farther up the kinetic chain. Without adequate strength, there may be a decreased capacity to withstand absolute forces as well as the ability to absorb loads through a required ROM demanded of the joint for a given movement. In the current study, the uninvolved quadriceps strength was not statistically different; however, the uninvolved limb still demonstrated an increased hip EAC compared with the controls. This ultimately suggests that altered neuromuscular control strategies after ACLR affect bilateral limbs, and thus, a change in central motor planning may be involved.11,19 These altered load absorption patterns are directly related to the EAC across joints and may eventually contribute to the movement compensation strategies identified.
The percentage of the EAC between the joints described in this study divaricates from other research that has looked at different tasks and planes of motion, such as the double-leg squat or sagittal-plane drop landing.7,20,22,23 Different tasks will utilize different EACs based on what is being called upon to perform that task. A static movement, for example, will demonstrate less ankle contribution because the plantar flexors are not required to accept the load during a squat as it would for a jump landing task. This is consistent with findings from Norcross et al,22,23 Sinsurin et al,32,33 and Taylor et al,35 which showed differences between sagittal- and frontal-plane energy absorption for a jump landing task; these studies concluded that there is a lack of relationship between energy absorption and interplanar tasks.
Limitations
The current study looked only at female patients, and thus, the results may not be extrapolated to male patients, as previous studies have described differences in biomechanics and the EAC between sexes.7,22,23,25,37 Furthermore, the mean age of the controls in the current study, conducted in a younger population, was 14.5 ± 1.1 years. Therefore, the findings may be not generalizable to other age groups. Because of the high prevalence of ACL tears in young, active patients, we believe that these results are important for this highly affected population.
The results from this study provide insight into the EAC for an LVJ maneuver, but they may not be related to other tasks or planes of movement. Despite the lack of generalization of these results, it is still an important addition to biomechanical and clinical data, as there is a lack of research in frontal-plane EAC. Further research is needed to examine other movements and planes of motion to further understand the EAC and elucidate possible interplanar energy absorption relationships.
Finally, neither dorsiflexion ROM nor plantar flexion strength was obtained in the battery of tests. Limited weightbearing dorsiflexion ROM has been attributed to decreased knee flexion ROM and greater knee varus displacement with double-leg and single-leg squats, both of which contribute to poor biomechanical patterns that place increased strain on the ACL.8 Without ROM or strength data, it is difficult to conclude why patients who underwent ACLR employed a decreased ankle EAC. Future studies should examine the effects of ankle ROM and strength on movement patterns as they relate to the EAC during dynamic movements.
Conclusion
The results of this study indicate that patients after ACLR employ altered landing strategies during an LVJ maneuver at the time of RTS. Specifically, patients who underwent ACLR utilized a greater hip and decreased ankle EAC compared with their healthy counterparts. These changes in landing mechanics may be in part attributed to bilateral quadriceps and involved hip ER strength deficits that continue to be present at the time of RTS after ACLR. Altered neuromuscular control patterns persist through the time when most athletes are allowed to RTS; these biomechanical changes may increase stress on the reconstructed ACL graft and ultimately place these athletes at risk of a subsequent injury.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
Ethical approval for this study was obtained from Texas Health Resources (study No. Pro00005872).
References
- 1. Arendt EA, Agel J, Dick R. Anterior cruciate ligament injury patterns among collegiate men and women. J Athl Train. 1999;34(2):86–92. [PMC free article] [PubMed] [Google Scholar]
- 2. Bakker R, Tomescu S, Brenneman E, Hangalur G, Laing A, Chandrashekar N. Effect of sagittal plane mechanics on ACL strain during jump landing. J Orthop Res. 2016;34(9):1636–1644. [DOI] [PubMed] [Google Scholar]
- 3. Chung KS, Ha JK, Yeom CH, et al. Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? Two-year follow-up after reconstruction. Am J Sports Med. 2015;43(12):3013–3021. [DOI] [PubMed] [Google Scholar]
- 4. Cruz A, Bell D, McGrath M, Blackburn T, Padua D, Herman D. The effect of three jump landing tasks on kinetic and kinematic measures: implications for ACL injury research. Res Sports Med. 2013;21(4):330–342. [DOI] [PubMed] [Google Scholar]
- 5. Cvjetkovic DD, Bijeljac S, Palija S, et al. Isokinetic testing in evaluation rehabilitation outcome after ACL reconstruction. Med Arch. 2015;69(1):21–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 7. Decker MJ, Torry MR, Wyland DJ, Sterett WI, Steadman JR. Gender differences in lower extremity kinematics, kinetics and energy absorption during landing. Clin Biomech. 2003;18(7):662–669. [DOI] [PubMed] [Google Scholar]
- 8. Dill KE, Begalle RL, Frank BS, Zinder SM, Padua DA. Altered knee and ankle kinematics during squatting in those with limited weight-bearing–lunge ankle-dorsiflexion range of motion. J Athl Train. 2014;49(6):723–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Feiring DC, Ellenbecker TS, Derscheid GL. Test-retest reliability of the Biodex isokinetic dynamometer. J Orthop Sports Phys Ther. 1990;11(7):298–300. [DOI] [PubMed] [Google Scholar]
- 10. Geiser CF, O’Connor KM, Earl JE. Effects of isolated hip abductor fatigue on frontal plane knee mechanics. Med Sci Sports Med. 2010;42(3):535–545. [DOI] [PubMed] [Google Scholar]
- 11. Grooms DR, Page SJ, Nichols-Larsen DS, Chaudhari AM, White SE, Onate JA. Neuroplasticity associated with anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2017;47(3):180–189. [DOI] [PubMed] [Google Scholar]
- 12. Hamilton RT, Shultz SJ, Schmitz RJ, Perrin DH. Triple-hop distance as a valid predictor of lower limb strength and power. J Athl Train. 2008;43(2):144–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps activation following knee injuries: a systematic review. J Athl Train. 2010;45(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes. Am J Sports Med. 2005;33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 15. Khayambashi K, Ghoddosi N, Straub RK, Powers CM. Hip muscle strength predicts noncontact anterior cruciate ligament injury in male and female athletes: a prospective study. Am J Sports Med. 2016;44(2):355–361. [DOI] [PubMed] [Google Scholar]
- 16. Krosshaug T, Nakamae A, Boden BP, et al. Mechanisms of anterior cruciate ligament injury in basketball. Am J Sports Med. 2007;35(3):359–367. [DOI] [PubMed] [Google Scholar]
- 17. Laudner K, Evans D, Wong R, et al. Relationship between isokinetic knee strength and jump characteristics following anterior cruciate ligament reconstruction. Int J Sports Phy Ther. 2015;10(3):272–280. [PMC free article] [PubMed] [Google Scholar]
- 18. Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis IS. Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Med. 2004;36(6):926–934. [DOI] [PubMed] [Google Scholar]
- 19. Lepley LK, Lepley AS, Onate JA, Grooms DR. Eccentric exercise to enhance neuromuscular control. Sports Health. 2017;9(4):333–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Montgomery MM, Shultz SJ, Schmitz RJ. The effect of equalizing landing task demands on sex differences in lower extremity energy absorption. Clin Biomech. 2014;29(7):760–766. [DOI] [PubMed] [Google Scholar]
- 21. Narducci E, Waltz A, Gorski K, Leppla L, Donaldson M. The clinical utility of functional performance tests within one-year post-ACL reconstruction: a systematic review. Int J Sports Phy Ther. 2011;6(4):333–342. [PMC free article] [PubMed] [Google Scholar]
- 22. Norcross MF, Lewek MD, Padua DA, Shultz SJ, Weinhold PS, Blackburn T. Lower extremity energy absorption and biomechanics during landing, part II: frontal-plane energy analyses and interplanar relationship. J Athl Train. 2013;48(6):757–763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Norcross MF, Lewek MD, Padua DA, Shultz SJ, Weinhold PS, Blackburn TB. Lower extremity energy absorption and biomechanics during landing, part I: sagittal-plane energy absorption analyses. J Athl Train. 2013;48(6):748–756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Oro FB, Sikka RS, Wolters B, et al. Autograft versus allograft: an economic cost comparison of anterior cruciate ligament reconstruction. Arthroscopy. 2011;27(9):1219–1225. [DOI] [PubMed] [Google Scholar]
- 25. Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014;42(7):1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Paterno MV, Schmitt LC, Ford KR, Rauh MJ. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am J Sports Med. 2010;38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Petersen W, Taheri P, Forkel P, Zantop T. Return to play following ACL reconstruction: a systematic review about strength deficits. Arch Orthop Trauma Surg. 2014;134(10):1417–1428. [DOI] [PubMed] [Google Scholar]
- 28. Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40(2):42–51. [DOI] [PubMed] [Google Scholar]
- 29. Pratt KA, Sigward SM. Knee loading deficits during dynamic tasks in individuals following ACL reconstruction. J Orthop Sports Phys Ther. 2017;47(6):411–419. [DOI] [PubMed] [Google Scholar]
- 30. Seifert L, Button C, Davids K. Key properties of expert movement systems in sport. Sports Med. 2013;43(3):167–178. [DOI] [PubMed] [Google Scholar]
- 31. Sigward SM, Lin P, Pratt K. Knee loading asymmetries during gait and running in early rehabilitation following anterior cruciate ligament reconstruction: a longitudinal study. Clin Biomech. 2016;32:249–254. [DOI] [PubMed] [Google Scholar]
- 32. Sinsurin K, Srisangboriboon S, Vachalathiti R. Side-to-side differences in lower extremity biomechanics during multi-directional jump landing in volleyball athletes. Eur J Sport Sci. 2017;17(6):699–709. [DOI] [PubMed] [Google Scholar]
- 33. Sinsurin K, Vachalathiti R, Jalayondeja W, Limroongreungrat W. Altered peak knee valgus during jump-landing among various directions in basketball and volleyball athletes. Asian J Sports Med. 2013;4(3):195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Suzuki H, Omori G, Uematsu D, Nishino K, Endo N. The influence of hip strength on knee kinematics during a single-legged medial drop landing among competitive collegiate basketball players. Int J Sports Phys Ther. 2015;10(5):592–601. [PMC free article] [PubMed] [Google Scholar]
- 35. Taylor JB, Ford KR, Nguyen A-D, Shultz SJ. Biomechanical comparison of single-and double-leg jump landings in the sagittal and frontal plane. Orthop J Sports Med. 2016;4(6):23259 67116655158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124–128. [DOI] [PubMed] [Google Scholar]
- 37. Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med. 2007;35(7):1123–1130. [DOI] [PubMed] [Google Scholar]