Abstract
Objective:
We sought to determine the utility of health administrative databases for population-based suicide surveillance, as these data are generally more accessible and more integrated with other data sources compared to coroners’ records.
Method:
In this retrospective validation study, we identified all coroner-confirmed suicides between 2003 and 2012 in Ontario residents aged 21 and over and linked this information to Statistics Canada’s vital statistics data set. We examined the overlap between the underlying cause of death field and secondary causes of death using ICD-9 and ICD-10 codes for deliberate self-harm (i.e., suicide) and examined the sociodemographic and clinical characteristics of misclassified records.
Results:
Among 10,153 linked deaths, there was a very high degree of overlap between records coded as deliberate self-harm in the vital statistics data set and coroner-confirmed suicides using both ICD-9 and ICD-10 definitions (96.88% and 96.84% sensitivity, respectively). This alignment steadily increased throughout the study period (from 95.9% to 98.8%). Other vital statistics diagnoses in primary fields included uncategorised signs and symptoms. Vital statistics records that were misclassified did not differ from valid records in terms of sociodemographic characteristics but were more likely to have had an unspecified place of injury on the death certificate (P < 0.001), more likely to have died at a health care facility (P < 0.001), to have had an autopsy (P = 0.002), and to have been admitted to a psychiatric hospital in the year preceding death (P = 0.03).
Conclusions:
A high degree of concordance between vital statistics and coroner classification of suicide deaths suggests that health administrative data can reliably be used to identify suicide deaths.
Keywords: suicide, validation, coroner
Abstract
Objectif :
Nous avons cherché à déterminer l’utilité des bases de données administratives de la santé pour la surveillance du suicide dans la population, car ces données sont généralement plus accessibles et plus intégrées avec d’autres sources de données comparativement aux dossiers des coroners.
Méthode :
Dans cette étude de validation rétrospective, nous avons identifié tous les suicides confirmés par un coroner entre 2003 et 2012 chez les résidents ontariens de 21 ans et plus, et lié cette information aux données des statistiques d’état civil de Statistique Canada. Nous avons examiné le chevauchement entre le domaine des causes de décès sous-jacentes et celui des causes secondaires de décès à l’aide des codes de la CIM-9 et de la CIM-10 pour l’automutilation délibérée (c.-à-d., le suicide), et examiné les caractéristiques sociodémographiques et cliniques des dossiers mal classés.
Résultats :
Parmi les 10 153 décès liés, il y avait un degré très élevé de chevauchement entre les dossiers codés comme étant une automutilation délibérée dans les données des statistiques d’état civil et les suicides confirmés par les coroners à l’aide des définitions de la CIM-9 et de la CIM-10 (sensibilité de 96,88% et de 96,84% respectivement). Cet alignement s’est accru constamment durant la période de l’étude (de 95,9% à 98,8%). D’autres diagnostics des statistiques d’état civil dans des domaines principaux incluaient des signes et symptômes non catégorisés. Les dossiers des statistiques d’état civil qui ont été mal classés ne différaient pas des dossiers valides au chapitre des caractéristiques sociodémographiques, mais ils étaient plus susceptibles de contenir un endroit non spécifié pour la blessure sur le certificat de décès (p < 0,001), plus susceptibles que les décès aient eu lieu dans un établissement de santé (p < 0,001), qu’il y ait eu une autopsie (p = 0,002), et qu’il y ait eu une hospitalisation en psychiatrie dans l’année précédant le décès (p = 0,03).
Conclusions :
Un degré élevé de concordance entre le classement des décès par suicide des statistiques d’état civil et celui des coroners suggère que les données administratives de la santé peuvent être utilisées avec confiance pour identifier les décès par suicide.
In Canada, there are approximately 4050 suicides estimated in a single year, a mortality rate of 11.5 per 100,000 people.1,2 The recent Federal Framework for Suicide Prevention Act identifies suicide as a mental and public health priority and promotes “the use of research and evidence-based practices for the prevention of suicide.”3 This not only highlights that suicide is preventable4–6 but suggests that accurately classifying suicides is necessary for the identification of potential targets for intervention strategies. Health administrative data are well suited for these types of efforts because they allow for population-level surveillance at minimal cost, as coroners’ records may not be as accessible to researchers in some jurisdictions and are not often as well integrated with other data sets. Such integration can facilitate research on the sociodemographic and clinical characteristics, as well as the health service contacts of suicide deaths, which can help identify opportunities for prevention.7 However, the utility of health administrative data for population-based suicide surveillance is determined by the accuracy of methods used to detect and record suicide.
Traditionally, within administrative health records, suicides have been identified through a primary cause of death recorded as deliberate self-harm in the vital statistics database, which relies on documentation obtained from the death certificate. However, the determination of suicidal intent can be complex, and the validity of death certificates for identifying suicides has been questioned, with underreporting being a major concern.8 Several studies have evaluated death certificates from vital registration systems against medical charts and autopsies and have suggested that external causes of injury, including suicides, are often misclassified.8–10 Misclassification may occur not only at the hands of the practitioner completing the death certificate but also at hands of those responsible for coding to the World Health Organization’s standards.11,12 Coroners likely classify suicide deaths more accurately, owing to a standardised process, required by law, to ascertain cause of death for all unnatural or unexpected deaths.13,14 Therefore, coroner’s data, where available, are a useful reference standard with which to compare suicides captured in vital statistics data. Yet, there is little research examining the accuracy of suicide definitions in health administrative databases, including the vital statistics data set, compared to coroner data.
Determining the accuracy of health administrative databases is important for establishing whether such data sources can be reliably used for suicide monitoring and population-based research. In this population-based study, we sought to validate definitions of suicide from vital statistics data against confirmed suicides from the Office of the Chief Coroner for Ontario as a reference standard.
Method
Study Design and Population
In this retrospective validation study, we identified all Ontario adults aged 21 and over who died by suicide between January 1, 2003, and December 31, 2012, using data from the Office of the Chief Coroner (OCC) and linked this information to the Office of the Registrar General–Deaths (ORG-D), Statistics Canada’s Vital Statistics database (95.73% linkage rate). These data sets were linked using unique encoded identifiers and analysed at the Institute for Clinical Evaluative Sciences (ICES). We excluded Ontario residents who died outside of the province and residents from outside of the province who died in Ontario. We also excluded records that could not be linked across databases due to data inconsistencies (such as missing health card numbers, duplicates, and missing OCC death dates).
Reference Standard
As the reference standard, we used mortality data from the OCC for Ontario on all confirmed suicide deaths from January 1, 2003, to December 31, 2012. Ontario law requires that all unnatural or unexpected deaths, which can include suicides, be reported to the coroner so that cause or causes of death can be determined.13 Coroner investigations involve an analysis of all relevant information from multiple, independent sources, including not only the death certificate but also police reports, evidence from the scene (e.g., suicide note), postmortem examinations (ie, autopsies), toxicology reports, and family interviews. These investigations can last up to 2 years and therefore involve a delay from date of death to when OCC data are available to be analysed.14 Deaths that were deemed by the coroner to be of undetermined intent were not included in this study given its focus on determining whether vital statistics are a reasonable proxy for the coroner’s determinations rather than reevaluation of those determinations.
Vital Statistics Data
We used mortality data from the ORG-D to identify individuals who died in Ontario from deliberate self-harm causes. Since January 2000, the ORG-D has recorded information about the underlying causes of death from the death certificate using the World Health Organization’s (WHO’s) International Statistical Classification of Diseases, Tenth Revision (ICD-10).15,16 The underlying cause of death, defined as “the disease or injury which initiated the train of morbid events leading directly to death, or the circumstances of the accident or violence which produced the fatal injury,” is automatically selected from a number of conditions listed on the medical certificate of death.17 In addition, the death certificate includes the immediate cause of death, the condition leading directly to death, and antecedent causes, if any, giving rise to the immediate cause of death. We examined ICD-10 codes X60 to X84 for deliberate self-harm.
Since an earlier ICD revision was used by Statistics Canada between 1979 and 1999, we also determined the validity of suicide definitions using ICD-9 coding (deliberate self-harm codes E950-E909) to enable studies wishing to examine overlapping time frames. A derived ICD-9 variable was created in the ORG-D after 2000 for all ICD-10 records, whereby the underlying cause of death was converted using cross-walk files developed by the Canadian Institute for Health Information (CIHI).18
Statistical Analysis
We first examined the overlap (ie, sensitivity) between records with deliberate self-harm as the underlying cause of death in the ORG-D and definite suicides in OCC data overall, as well as by year. We also checked whether there were deliberate self-harm records in the ORG-D that did not appear in the OCC to identify any unnatural deaths that were not examined by a coroner. We further examined the overlap between all underlying causes of death for linked ORG-D/OCC records, which were grouped using WHO standards.16 We also examined causes of death coded in secondary diagnostic fields, which include immediate and antecedent causes of death (≤12 fields for each record).
We further described cases where there was overlap between the ORG-D and OCC versus cases with no such overlap and captured information on age at the time of death, sex, neighbourhood income quintile, rural/urban dwelling, place of injury, place of death, and underlying causes of death. We also examined whether an autopsy was performed. Using the National Ambulatory Care Reporting System, CIHI’s hospital Discharge Abstract Database, the Ontario Mental Health Reporting System, and the Ontario Health Insurance Plan databases, we further assessed previous mental health and addictions-related contact in the emergency department, hospital, and outpatient settings (a mental health and addictions-related visit to a family practitioner or family physician, or a visit to a psychiatrist) in the year preceding death. The definitions for mental health and addictions-related service contact have been described in detail elsewhere.7
All analyses were conducted using SAS software (version 9.4; SAS Institute, Cary, NC). This study was approved by the institutional review board at Sunnybrook Health Sciences Centre, Toronto, Canada.
Results
Study Cohort
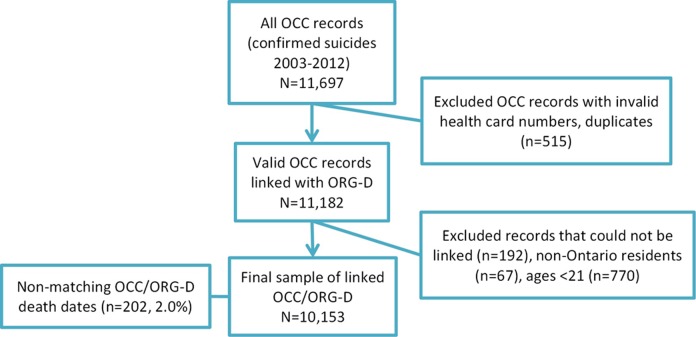
Of 11,697 coroner-confirmed suicide records between 2002 and 2013, we excluded 511 records with invalid health card numbers and 4 records that were duplicates (Figure 1). We then linked 11,182 OCC records to the ORG-D. Of those, 192 (1.89%) had no ORG-D record. After further excluding 67 non-Ontario residents and 770 individuals aged <21, we obtained a final sample of 10,153 linked OCC/ORG-D records. Of those, 202 (2.0%) had nonmatching death dates (of those, 69.3% were within 1 week). Given that both OCC and ORG-D use probabilistic linkage, we used all available ORG-D–linked records, regardless of death date discrepancies. There were 364 records of deliberate self-harm deaths in the ORG-D that were not identified in the OCC data set for confirmed suicides.
Figure 1.
Flowchart of the process used to link OCC and ORG-D data to obtain the study cohort. OCC, Office of the Chief Coroner data set; ORG-D, Office of the Registrar General-Death data set.
Underlying and Secondary Causes of Death
There was a very high degree of overlap between records coded as deliberate self-harm in the ORG-D and coroner-confirmed suicides (Table 1) using both ICD-9 and ICD-10 definitions (96.88% and 96.84% sensitivity, respectively). The alignment between OCC and ORG-D (Figure 2) has increased slightly between 2003 and 2012, with the lowest sensitivity for ICD-10 codes X60 to X84 observed in 2006 (95.69%) and highest in 2012 (98.79%). A large proportion (39.2%) of these overlapping cases were coded in the ORG-D as intentional self-harm by hanging, strangulation, and suffocation, followed by self-poisoning (10.5%), jumping from a high place (7.9%), and firearm discharges (7.7%, for more detail, see Appendix). Of 10,153 linked ORG-D/OCC records between 2003 and 2012, other underlying causes of death were most often coded as symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified (ICD-10 codes R00-R99). Equivalent results were obtained using ICD-9 codes. Vital statistics diagnoses coded in secondary fields among coroner-confirmed suicides (Table 2) included injury and poisoning-related codes (S00-T98), deliberate self-harm (X60-X84), and mental disorders (F00-F99). Of linked OCC/ORG-D records, 126 (12.3%) were recorded as having had an autopsy in 2003; this number has dropped to 69 (6.4%) in 2012.
Table 1.
Overlap between the Underlying Cause of Death Field in the ORG-D and Coroner-Confirmed Suicide Records in 2003 to 2012.
| Of 10,153 Coroner-Confirmed Suicides (Linked with ORG-D) Underlying Causes of Death: ICD-10 Groupa | No. (%)b |
|---|---|
| X60-X84 Deliberate self-harmc,d | 9832 (96.84) |
| R00-R99 Symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified | 106 (1.04) |
| Y10-Y34 External—event of undetermined intent | 85 (0.84) |
| V01-X59 Accidents | 81 (0.8) |
| I00-I99 Diseases of the circulatory system | 18 (0.18) |
| F00-F99 Mental, behavioural, and neurodevelopmental disorders | 9 (0.09) |
| J00-J99 Diseases of the respiratory system | 7 (0.07) |
OCC, Office of the Chief Coroner data set; ORG-D, Office of the Registrar General–Death data set; S, cell with <6 frequency supressed to minimise risk of reidentification.
aSimilar results were obtained using ICD-9 groups.
bData with frequencies ≤5 have been suppressed due to privacy limits.
cICD-9 E950 to E959 codes (96.88% sensitivity).
dThere were almost no deliberate self-harm records outside of OCC data (<0.1% ORG-D deliberate self-harm records with no OCC record).
Figure 2.
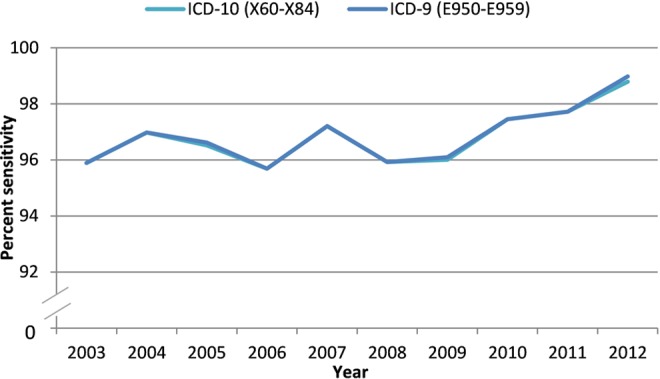
Proportion of coroner-confirmed suicides that have been identified in the ORG-D using primary codes for deliberate self-harm, 2003 to 2012. ORG-D, Office of the Registrar General-Death data set.
Table 2.
Overlap between Secondary Cause of Death Fields in ORG-D and Coroner-Confirmed Suicide Records in 2003 to 2012.
| ICD-10 Group (n = 35,745 Nonmissing Records, Not Mutually Exclusive)a | Secondary Causes of Death Fields 2 to 12 (Summed), No. (%) |
|---|---|
| S00-T98 Injury, poisoning, and certain other consequences of external causes | 17,327 (48.47) |
| X60-X84 Deliberate self-harm | 10,309 (28.84) |
| F00-F99 Mental, behavioural, and neurodevelopmental disorders | 5263 (14.72) |
| I00-I99 Diseases of the circulatory system | 617 (1.73) |
| R00-R99 Symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified | 463 (1.30) |
ORG-D, Office of the Registrar General–Death data set.
aMultiple secondary fields may be filled out for each death record (up to 12 fields); for this table, all nonmissing secondary fields have been summed and only frequencies ≥1% are shown.
Characteristics of Misclassified Records
Among coroner-confirmed suicides between 2003 and 2012, there were no differences between records coded as deliberate self-harm in the ORG-D and those that were misclassified with regards to sex, age, rural dwelling, or neighbourhood income quintile (Table 3). Most suicides occurred among males, individuals aged 25 to 64, and those living in lower-income neighbourhoods and urban centres. However, there were significant (P < 0.001) differences in the place of injury recorded on the death certificate between ORG-D records that matched with the OCC, whereby most injuries occurred at home, and the misclassified records, where most had either a missing or an unspecified place of injury. Misclassified records were also more likely (P < 0.001) to have died at a health care facility. Among the 190 misclassified cases that had an unspecified/missing place of injury on the death certificate, 41% were coded as having died at home and 33% died at a health care facility. By contrast, a smaller proportion (20%) of the 439 valid cases with an unspecified/missing place of injury died at home, while a larger proportion (43%) died at a health care facility. Discordant cases were more likely to have had an autopsy (P = 0.002). Last, there were no significant differences with regards to mental health and addictions-related service utilisation in emergency departments or outpatient settings 1 year prior to suicide. However, misclassified cases were more likely to have been admitted to a psychiatric hospital in the year preceding death (P = 0.03).
Table 3.
Characteristics of Coroner-Confirmed Suicides That Were Coded as Deliberate Self-Harm in the ORG-D and Those That Were Misclassified, 2003 to 2012.
| Characteristic | Self-Harm in ORG-D (n = 9832), No. (%) | Not Self-Harm in ORG-D (n = 321), No. (%) | χ2, P Value |
|---|---|---|---|
| Sex | |||
| Female | 2445 (24.87) | 94 (29.28) | 0.07 |
| Male | 7387 (75.13) | 227 (70.72) | |
| Age category | |||
| ≤24 | 601 (6.11) | 17 (5.3) | 0.76 |
| 25-64 | 7684 (78.15) | 256 (79.75) | |
| ≥65 | 1547 (15.73) | 48 (14.95) | |
| Rural | 1557 (15.84) | 44 (13.71) | 0.30 |
| Neighbourhood income quintilea | |||
| Q1 (lowest) | 2518 (25.61) | 88 (27.41) | 0.16 |
| Q2 | 2032 (20.67) | 82 (25.55) | |
| Q3 | 1909 (19.42) | 54 (16.82) | |
| Q4 | 1717 (17.46) | 48 (14.95) | |
| Q5 (highest) | 1606 (16.33) | 46 (14.33) | |
| Place of injury | |||
| Home | 7183 (73.06) | 110 (34.27) | <0.001 |
| Institution | 200 (2.03) | ≤5 (S) | |
| Outside | 953 (9.69) | 9 (2.8) | |
| Other | 1057 (10.75) | 10 (3.12) | |
| Unspecified/missing | 439 (4.47) | 190 (59.19) | |
| Place of death | |||
| Health care facility | 1684 (17.13) | 90 (28.04) | <0.001 |
| Other/non–health care facilities | 2600 (26.44) | 79 (24.61) | |
| Home | 5548 (56.43) | 152 (47.35) | |
| Autopsy | |||
| Autopsy performed | 950 (9.66) | 49 (15.26) | 0.002 |
| Autopsy not performed | 8106 (82.45) | 242 (75.39) | |
| Missing | 776 (7.89) | 30 (9.35) | |
| MHA service use in the year prior to death | |||
| MHA hospitalisation | 1743 (17.73) | 72 (22.43) | 0.03 |
| MHA ED visit | 2410 (24.51) | 91 (28.35) | 0.12 |
| MHA outpatient physician visit | 5494 (55.88) | 187 (58.26) | 0.40 |
ED, emergency department; MHA, mental health and addictions; ORG-D, Office of the Registrar General–Death data set; S, suppressed to due to small cell counts that may result in identification.
aCategories do not add up to 100%—rows with missing observations were supressed.
Discussion
Summary of Findings
In this large, population-based study, we found that vital statistics data on identification of suicide deaths had a high degree of concordance with the reference-standard coroners’ data. In particular, from 2003 to 2012, using either ICD-10 or ICD-9 diagnostic codes for deliberate self-harm in the underlying cause of death field yielded high sensitivity. Consistency between ICD-9 and ICD-10 for suicides has previously been shown.19 Examining secondary fields in vital statistics data, which include immediate and antecedent causes of death, did not improve the sensitivity of detecting suicides. In fact, most diagnoses coded in secondary fields of the death certificate were coded as undetermined intent, injury or poisoning, accidents, and unspecified signs and symptoms. We also found that coroner-confirmed suicides that were misclassified in vital statistics data were more likely to have had an autopsy, to have died at a health care facility, and to have had an unspecified place of injury.
Interpretation
There is great value in using health administrative databases for suicide surveillance, particularly for identifying opportunities for prevention.7,20 For example, 1 study linked coroner and health administrative data and identified substantial service utilisation in ambulatory settings close to the time of death among suicide descendants, which suggests that implementing intervention strategies at the primary and specialty clinical care level may be worthwhile.7 Yet, coroner records are seldom available for researchers, and extracting such data is often a lengthy and costly undertaking that can undermine timely surveillance. Confidence in definitions of suicide obtained from vital statistics registries could help clinicians, epidemiologists, and health service planners in understanding and managing the risk of suicide when coroner records are not available.
The Canadian provincial and territorial registrars provide data on vital events to Statistics Canada, which is responsible for compiling a national registry annually. The death registration includes the Medical Certificate of Cause of Death, which is completed by the medical practitioner last in attendance or by a coroner or medical examiner. Statistics Canada then classifies the ICD-10 codes for causes of death using a set of selection and modification rules developed by the WHO.21 Trained mortality classification staff use an automated system known as the Mortality Medical Data System (MMDS), developed and maintained by the U.S. National Center for Health Statistics (NCHS).21 Death certificates rejected by the MMDS system are then manually coded in house.
Most deaths in Ontario are due to natural diseases. Any physician in attendance during or having sufficient knowledge of the last illness of the deceased has a legal obligation to promptly complete the death certificate.22 However, under the Ontario Coroners Act, deaths that are sudden and unexpected, including accidents, suicides, homicides, and sudden deaths from previously undiagnosed diseases or suspected medical negligence, are legally reportable and require investigation by a coroner; police officers at the scene must also notify the coroner of the facts and circumstances pertaining to such deaths.13 In addition, deaths occurring in a long-term care home or other residential institution, a psychiatric facility, or a hospital to which a patient was transferred from these locations must be reported to the coroner.13 Of the approximately 15,000 deaths investigated by coroners annually, about 6000 undergo medicolegal autopsy performed by pathologists in forensic pathology units and community hospitals across the province.23 While international evidence suggests that autopsy rates have declined over time and that this has been associated with decreasing suicide rates and misclassification,24 we found that agreement rates between coroner and vital statistics data increased despite declining autopsy rates, suggesting that misclassification is not related to declining autopsy rates.
The use of coroner data as a reference standard has also been debated in the literature. For example, 1 study found that among researcher-defined suicides, the proportion of coroner-defined suicides declined, reaching about 50% in 2005, mostly due to rising classification of accidents, predominantly in cases of medicinal poisoning.25 Despite this, we sought to determine whether diagnoses of deliberate self-harm in vital statistics are a reasonable proxy for coroner determinations, given their relative availability for researchers interested in suicide surveillance, rather than debating the validity of coroner determinations. The high degree of concordance we observed is likely occurring because of the quality of coding practices in the ORG-D and the OCC, which are more aligned than, for example, a researcher-led chart review abstracted by nurse practitioners. Since both the OCC and ORG-D are coding the same source (the death certificate), using the coroner’s final determination, which is further based on additional sources of information, reduces any misclassification that persons reviewing medical charts and autopsies may have made.
The minor degree of discordance we observed between coroner and vital statistics data on suicides may be explained by differences in coding practices, whereby the coroner’s data coded in house may be slightly more accurate, as specialists may be more available to provide feedback in cases of ambiguity when multiple entries are present on the death certificate. It may also be explained by instances where the death initially appears not to require a coroner’s investigation but subsequent information warrants the coroner’s involvement, who produces an updated death certificate. For example, we may speculate that someone who had a suicide attempt by self-poisoning and later died in hospital from hepatic failure would have been correctly coded as dying by suicide by the coroner but might have been classified as dying from a hepatic cause by hospital staff filling out a death certificate for a natural cause of death. We also observed a difference in the place of death recorded in concordant and discordant deaths. It has been previously shown that difficulty linking the death back to the initiating injury can result in misclassification of the death.26 Misclassified cases were also more likely to have had a psychiatric hospitalisation in the year preceding death. It may be that these death certificates were reclassified by the coroner upon discovery of prior mental health contact, as studies suggest that cases with a prior suicide attempt are more likely to be correctly certified by a coroner.26 However, such instances are rare, as coroners are typically the only professionals certifying unnatural deaths. The classification agreement we observed was sufficiently high and provides the basis for meaningful suicide surveillance work using vital statistics data in the absence of coroner records.
Strengths and Limitations
This was a large, population-based study capturing all suicide deaths over a 9-year period in Ontario, the most populous province in Canada (population 13.1 million in 2010). In addition, only coroner-confirmed suicides and not deaths of undetermined intent were used as a reference standard. These cases were subject to rigorous coroner investigations and are thus likely a true representation of suicide deaths in this province. We were also able to ascertain methods of detecting suicides from vital statistics data using both ICD-10 and ICD-9 codes, which can help researchers aiming to conduct investigations in earlier time frames.
Nonetheless, some limitations are worth noting. First, data on deaths that were investigated by the coroner and were deemed to be nonsuicides were not available. Therefore, specificity and predictive value estimates were not produced. However, given the relative rarity of suicides compared to other deaths, sensitivity is of greater importance for case finding. Second, this study was limited to individuals aged 21 and older; researchers wishing to examine children and youth should use caution when applying the definitions we observed, as a higher degree of discordance may occur in younger age groups. Third, we observed 2% of linked records with nonmatching death dates between the 2 data sources. However, given that both OCC and ORG-D use probabilistic linkage and given that most discrepant deaths dates were within 1 week, it is unlikely to have affected our results. Fourth, the circumstances in which a coroner is involved in the determination of causes of death vary across provinces and territories in Canada27 and other developed counties, some of which rely on the medicolegal rather than the coronial system.28 As such, the results of this study may have limited generalisability. Last, it may be that the coroner’s ruling was also affected by subjectivity, with studies reporting that deaths from hanging and gas tend to be more likely assigned as suicides than deaths from poisoning and drowning.26 However, our analysis of misclassified vital statistics cases revealed that most were coded as signs/symptoms and events of undetermined intent rather than accidents.
Conclusion
This study shows that vital statistics data can be used to identify suicide deaths, as determined by coroner verdicts, with a high degree of accuracy. This has considerable implications for future research, as the ability to use vital statistics data can facilitate surveillance, monitoring, and prevention strategies when more detailed investigational data such as coroner’s records are unavailable.
Acknowledgements
We thank Kinwah Fung for her contributions to methodological oversight. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI), the Office of the Chief Coroner for Ontario (OCC), and the Ontario Registrar General (ORG) information on deaths, the original source of which is ServiceOntario. However, the analyses, conclusions, opinions, and statements in the material are those of the authors and not necessarily those of CIHI, the OCC, or the ORG or the Ontario Ministry of Government Services.
Appendix
Frequency of Deliberate Self-Harm Codes (X60-X84) among Coroner-Confirmed Suicides.
| Code | Description | No. | % |
|---|---|---|---|
| X70 | Intentional self-harm by hanging, strangulation, and suffocation | 3980 | 39.2 |
| X64 | Intentional self-poisoning by and exposure to other and unspecified drugs, medicaments, and biological substances | 1069 | 10.5 |
| X80 | Intentional self-harm by jumping from a high place | 798 | 7.9 |
| X74 | Intentional self-harm by other and unspecified firearm discharge | 782 | 7.7 |
| X67 | Intentional self-poisoning by and exposure to other gases and vapours | 565 | 5.6 |
| X61 | Intentional self-poisoning by and exposure to antiepileptic, sedative-hypnotic, antiparkinsonism, and psychotropic drugs, not elsewhere classified | 506 | 5.0 |
| X73 | Intentional self-harm by rifle, shotgun, and larger firearm discharge | 421 | 4.1 |
| X78 | Intentional self-harm by sharp object | 327 | 3.2 |
| X81 | Intentional self-harm by jumping or lying before moving object | 312 | 3.1 |
| X62 | Intentional self-poisoning by and exposure to narcotics and psychodysleptics [hallucinogens], not elsewhere classified | 306 | 3.0 |
| X71 | Intentional self-harm by drowning and submersion | 278 | 2.7 |
| X60 | Intentional self-poisoning by and exposure to nonopioid analgesics, antipyretics, and antirheumatics | 75 | 0.7 |
| X76 | Intentional self-harm by smoke, fire, and flames | 72 | 0.7 |
| X72 | Intentional self-harm by handgun discharge | 57 | 0.6 |
| X82 | Intentional self-harm by crashing of motor vehicle | 55 | 0.5 |
| X83 | Intentional self-harm by other specified means | 53 | 0.5 |
| X66 | Intentional self-poisoning by and exposure to organic solvents and halogenated hydrocarbons and their vapours | 52 | 0.5 |
| X69 | Intentional self-poisoning by and exposure to other and unspecified chemicals and noxious substances | 45 | 0.4 |
| X65 | Intentional self-poisoning by and exposure to alcohol | 34 | 0.3 |
| X63 | Intentional self-poisoning by and exposure to other drugs acting on the autonomic nervous system | 22 | 0.2 |
| X84 | Intentional self-harm by unspecified means | 15 | 0.1 |
| X68 | Intentional self-poisoning by and exposure to pesticides | 6 | 0.1 |
| X75 | Intentional self-harm by explosive material | S | 0.0 |
S, suppressed due to privacy limits.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). It was also supported by the Mental Health and Addictions Scorecard and Evaluation Framework grant from the MOHLTC. Dr. Kurdyak received operational grant funding from the MOHLTC Health Services Research Fund Capacity Award and is supported in part by the Medical Psychiatry Alliance, a collaborative health partnership of the University of Toronto, the Centre for Addiction and Mental Health, the Hospital for Sick Children, Trillium Health Partners, the MOHLTC, and an anonymous donor. The analyses, conclusions, opinions, and statements expressed herein are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
References
- 1. Statistics Canada. Suicide rates: An overview [cited 2017 Mar 24]. Available from: http://www.statcan.gc.ca/pub/82-624-x/2012001/article/11696-eng.htm2012.
- 2. Statistics Canada. CANSIM Table 102-0551—deaths and mortality rate, by selected grouped causes, age group and sex, Canada, annual 2014 [cited 2017 Apr 6].
- 3. Federal Framework for Suicide Prevention Act. S.C. 2012, c. 30.
- 4. Conwell Y, Farley-Toombs C. Evidence supports the obvious: suicides need not happen. Lancet. 2012;379(9820):981–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yip PS, Caine E, Yousuf S, et al. Means restriction for suicide prevention. Lancet. 2012;379(9834):2393–2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization (WHO). Preventing suicide: a global imperative. Geneva (Switzerland): World Health Organization; 2014. [Google Scholar]
- 7. Schaffer A, Sinyor M, Kurdyak P, et al. Population-based analysis of health care contacts among suicide decedents: identifying opportunities for more targeted suicide prevention strategies. World Psychiatry; 2016;15(2):135–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Allebeck P, Allgulander C, Henningsohn L, et al. Causes of death in a cohort of 50 465 young men: validity of recorded suicide as underlying cause of death. Scand J Public Health; 1991;19(4):242–247. [DOI] [PubMed] [Google Scholar]
- 9. Rampatige R, Mikkelsen L, Hernandez B, et al. Systematic review of statistics on causes of deaths in hospitals: strengthening the evidence for policy-makers. Bull World Health Organ; 2014;92(11):807–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ravakhah K. Death certificates are not reliable: revivification of the autopsy. South Med J. 2006;99(7):728–734. [DOI] [PubMed] [Google Scholar]
- 11. Schadé B. Reliability and validity of the classification of death in general practice. Scand J Prim Health Care; 1987;5(2):109–112. [DOI] [PubMed] [Google Scholar]
- 12. Harteloh P, de Bruin K, Kardaun J. The reliability of cause-of-death coding in the Netherlands. Eur J Epidemiol; 2010;25(8):531–538. [DOI] [PubMed] [Google Scholar]
- 13. Coroners Act, R.S.O. 1990, c. C.37, 2012.
- 14. Young JG, Wagner JM. Speaking for the dead to protect the living: the role of the coroner in Ontario. Health Rep; 1994;6(3):339–352; discussion 53. [PubMed] [Google Scholar]
- 15. Statistics Canada. Vital Statistics—Death Database [cited 2017 May 26]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?%20Function=getSurvey&Id=2576412015.
- 16. World Health Organization (WHO). International statistical classification of diseases and related health problems, tenth revision, volumes 1 and 2 (ICD-10). Geneva (Switzerland): World Health Organization; 1992. [Google Scholar]
- 17. Statistics Canada. Vital Statistics Death Database–glossary [cited 2017 Apr 6]. Available from: http://www23.statcan.gc.ca/imdb-bmdi/document/3233_D4_T9_V1-eng.htm2016.
- 18. Canadian Institute for Health Information. Conversion Tables (for use with ICD-10-CA/CCI) [cited 2017 Jul 17]. Available from: https://secure.cihi.ca/estore/productSeries.htm?pc=PCC85.
- 19. Gjertsen F, Bruzzone S, Vollrath ME, et al. Comparing ICD-9 and ICD-10: the impact on intentional and unintentional injury mortality statistics in Italy and Norway. Injury 2013;44(1):132–138. [DOI] [PubMed] [Google Scholar]
- 20. John A, Dennis M, Kosnes L, et al. Suicide Information Database-Cymru: a protocol for a population-based, routinely collected data linkage study to explore risks and patterns of healthcare contact prior to suicide to identify opportunities for intervention. BMJ Open 2014;4(11):e006780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Geran L, Tully P, Wood P, Thomas B; Statistics Canada. Comparability of ICD-10 and ICD-9 for mortality statistics in Canada. 2005. [cited 2017 Jul 21]. Available from: http://www.statcan.gc.ca/pub/84-548-x/84-548-x2005001-eng.htm?%20contentType=application%2Fpdf.
- 22. Office of the Registrar General. Handbook on medical certification of death. Ontario (Canada): Ministry of Consumer and Business Services; 2010. [Google Scholar]
- 23. Ministry of Community Safety and Correctional Services. Ontario Forensic Pathology Service (OFPS): annual report July 27, 2013–July 26, 2014. Toronto, ON: Queen’s Printer for Ontario; 2015.
- 24. Kapusta ND, Tran US, Rockett IR, et al. Declining autopsy rates and suicide misclassification: a cross-national analysis of 35 countries. Arch Gen Psychiatry; 2011;68(10):1050–1057. [DOI] [PubMed] [Google Scholar]
- 25. Gunnell D, Bennewith O, Simkin S, et al. Time trends in coroners’ use of different verdicts for possible suicides and their impact on officially reported incidence of suicide in England: 1990-2005. Psychol Med; 2013;43(7):1415–1422. [DOI] [PubMed] [Google Scholar]
- 26. Parai JL, Kreiger N, Tomlinson G, et al. The validity of the certification of manner of death by Ontario coroners. Ann Epidemiol 2006;16(11):805–811. [DOI] [PubMed] [Google Scholar]
- 27. Statistics Canada. Table C-1: Circumstances under which C/ME investigation is required, provinces and territories, 2006 to 2008 2015. [cited 2017 Jul 21]. Available from: http://www.statcan.gc.ca/pub/82-214-x/2012001/table-tableau/tblc-1-eng.htm.
- 28. Värnik P, Sisask M, Värnik A, et al. Suicide registration in eight European countries: a qualitative analysis of procedures and practices. Forensic Sci Int 2010;202(1):86–92. [DOI] [PubMed] [Google Scholar]