Abstract
Background:
In response to the ongoing infection prevention (IP) challenges in England, a 90-day quality improvement (QI) collaborative programme was developed. The paper discusses the approach, benefits, challenges and evaluation of the programme.
Objective:
The objective of the collaborative was to develop new approaches to enable sustainable and effective IP.
Methodology:
Six trusts in the region participated in the collaborative. Each defined their bespoke IP focus. There was no expectation that statistically significant measurable improvements would be identified during the short time frame. The experiences of the participants were sought both during the programme to facilitate its constant review and at the end of the programme to evaluate its effectiveness. The feedback focused on achievements, barriers to change and benefits of participating in a QI collaborative. To measure the potential success of the projects, participants completed the Model for Understanding Success in Quality framework. (MUSIQ; Kaplan et al., 2012).
Results:
Since each trusts IP focus was bespoke commonalities of success were not evaluated. Participants identified a positive outcome from their QI interventions. The MUSIQ score identified the projects had the potential for success.
Discussion:
The feedback from the participants demonstrated that it is worthy of further development.
Keywords: Evidence-based practice, quality improvement, PDSA
Introduction
Effective infection prevention (IP) has achieved significant reductions since 2010 in both Meticillin-resistant Staphylococcus aureus (MRSA; 57%) bacteraemia and Clostridium difficile (45%) infections (Public Health England, 2016). However, Gram-negative bloodstream infections infections are noted to be on the increase despite all the actions undertaken. The UK Five Year Antimicrobial Resistance Strategy 2013 to 2018 (Department of Health [DH], 2013) states that ‘High standards of IP and control will remain crucial to minimise the risk of infection’. One of the key actions is ‘improving IP and control practices…, both through enhanced dissemination and implementation of best practice and better use of data and diagnostics’.
In response to the ongoing IP challenge and in recognition of the barriers to initiating sustainable change improvements, NHS Improvement which supports National Health Service providers in England to give patients consistently safe, high quality, compassionate care, developed a 90-day IP quality improvement (QI) collaborative programme. Twenty-four hospitals in England were invited to participate. The objective was to promote shared learning, best practice and innovations with colleagues from other provider organisations and to develop new approaches to ensure sustainable and effective IP.
Around two-thirds of healthcare improvements result in a sustainable change (Health Foundation, 2013). The QI collaborative approach was chosen as it involves collaborating with staff in developing, designing and implementing changes, and has demonstrated greater sustainability (Health Foundation, 2013).
This article discusses the IP QI collaborative approach undertaken with the participating six NHS trusts, located in the regional administrative area of Midlands and East, England (University Hospitals of North Midlands NHS Trust, UK, Northampton General Hospital NHS Trust, UK, West Hertfordshire Hospitals NHS Trust, UK, Bedford Hospital NHS Trust, UK, United Lincolnshire Hospitals NHS Trust, UK, and The Royal Wolverhampton NHS Trust, UK). Perceptions of the lead IP nurses were canvassed both during and on completion of the collaborative to review and develop the process. To evaluate the potential success of the collaborative process, the Model for Understanding Success in Quality (MUSIQ) framework (Kaplan et al., 2012) was utilised by the participating teams. There was no expectation when undertaking the collaborative that statistically significant measurable improvements would be identified during the short time frame.
Quality improvement collaborative
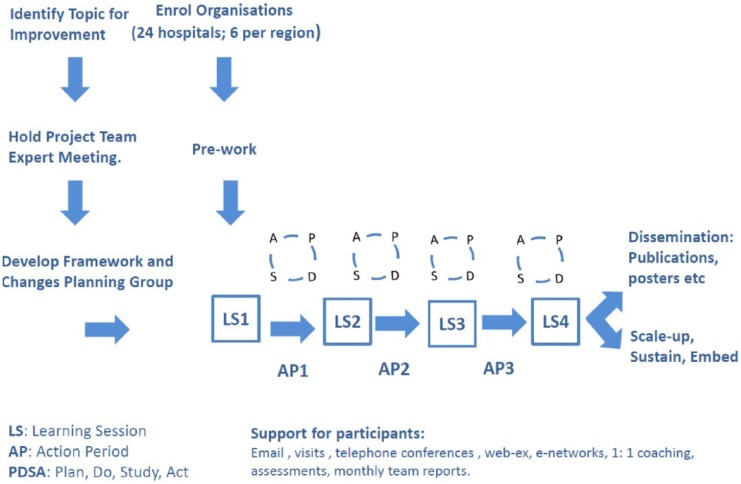
The QI collaborative methodology used for this intervention was amended from the Breakthrough Series methodology designed in 1995 by the Institute of Healthcare Improvement (IHI, 2003; Figure 1). The methodology has been defined as ‘a short-term (6 to 15 month) learning system that brings together a large number of teams from hospitals or clinics to seek improvement in a focussed topic area’. The Health Foundation (2013) acknowledges that there are several barriers to the improvement process (Table 1). However, they also identified that if time is taken to get an intervention’s theory of change, measurement and stakeholder engagement right, then it will deliver the enthusiasm, momentum and profound results (Health Foundation, 2013).
Figure 1.
IP quality improvement collaborative plan (adapted from IHI, 2003).
Table 1.
Barriers to the QI processes.
| There is always a resistance to change and this should be factored into any QI collaborative. The Health Foundation (2013) identified ten challenges to implementing the QI programme: 1. Convincing people that there is a problem 2. Convincing people that the solution chosen is the right one 3. Getting data collection and monitoring systems right 4. Excess ambitions and ‘projectness’ 5. The organisational context, culture and capacities 6. Tribalism and lack of staff engagement 7. Leadership 8. Balancing carrots and sticks – harnessing commitment through incentives and potential sanctions 9. Securing sustainability 10. Considering the side effects of change. |
In this collaborative, a 90-day approach was chosen in order to quickly up-skill the participating teams in the methodology. The purpose of the collaborative was to conduct small scale tests of change (Plan-Do-Study-Act [PDSA] cycles), which, if successful, would be rolled out to deliver sustainable change. If not successful, then the tests of change would be stopped in order not to waste further time and resources.
There are six key focus areas in a QI collaborative. These are identified below in relation to the IP QI collaborative programme undertaken.
Method 1: the six elements of the QI collaboarative (IHI, 2003) as adapted for the project
Identifying an area for improvement: The area for improvement chosen by the project team was to develop new approaches to enable sustainable and effective IP by promoting shared learning, best practice and innovations with colleagues from other provider organisations. Each participating organisation developed their bespoke IP improvement area (Table 2).
Project team recruitment: A QI collaborative project team generally consists of experts in the relevant disciplines, e.g. subject specialists and improvement specialists. The project team for the IP QI collaborative included: the four regional Heads of IP as the subject matter experts; executive leadership with NHS Improvement; and QI specialists. The team created the content of the collaborative and coached the participating teams on improvement methodology and its applications in local areas.
Enrolment of organisations: Twenty-four trusts were formally invited to participate in the QI collaborative. The six trusts in the Midlands and East region all accepted. On acceptance, an initial teleconference was held with each individual organisation. This included the Director of IP and Control (DIPC) and the lead IP nurse. The discussion involved: what the QI collaborative process involved; time commitments; travel commitments; potential improvement focus; and who they may wish to involve in their teams, e.g. multidisciplinary team members they thought appropriate. In some cases, this included the lead IP nurse in the Clinical Commissioning Group, antimicrobial pharmacists, theatre managers, housekeepers, matrons, etc.
- Learning sessions: Four face-to-face learning sessions were arranged. This brought together the multidisciplinary teams from all participating trusts. The IP QI collaborative was conducted over 90 days and incorporated multimodal approaches for developing staff awareness and engagement in the process. The multimodal approach was chosen as it is characterised by the utilisation of a variety of methods which potentially strengthens the success of the project:
- Day Zero event: Introductory meeting. The project team shared experiences of their clinical visits to organisations. This included observations of what worked well and where improvement opportunities exist. In addition, all participating hospitals showcased an area of work relating to IP that the team were proud of.
- 30-day event: The methodologies of developing driver diagrams and PDSA cycles were introduced. The participating teams each brought their potential plans and ideas for discussion.
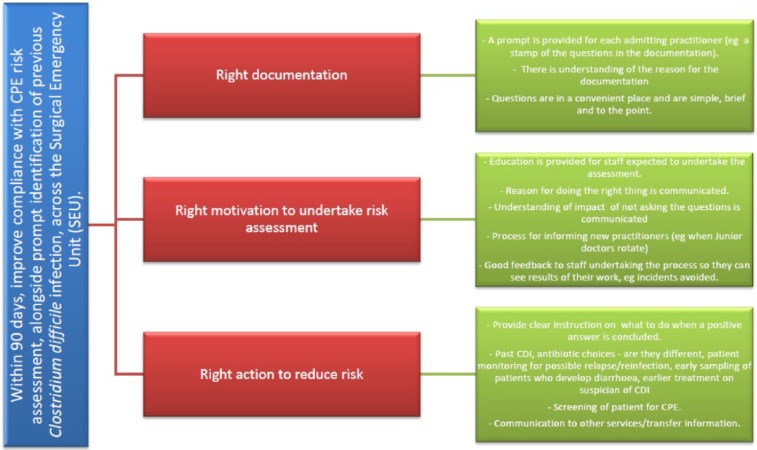
- 60-day event: Participants shared learning; driver diagrams for their projects (Figure 2); results of their initial tests of change (PDSA cycles); and approaches which had been successful and those which had failed. It is as important to identify and note approaches which failed as well as those which have been successful.
- 90-day event – final meeting: The teams came together to present their work to all participants. They showcased the tools they had developed, progress made, their experiences of the QI process and how they intended to scale up and sustain these changes (improvements) in their organisations. A variety of approaches were chosen to present including video clips, posters, case studies, etc.
- Action periods for participants: In the action periods between the learning sessions, the multidisciplinary teams from the participating trusts undertook various activities:
- First stage (action period 1):
- Each multidisciplinary team in the participating trusts identified a different IP topic to focus on. Therefore, their actions varied but generally incorporated the following: collecting and analysing baseline data in order to understand the current position in relation to compliance with The Health and Social Care Act 2008 Code of Practice on the prevention and control of infections and related guidance (DH, 2015). This helped to facilitate which topic to focus on during the QI programme.
- Reviewing the current IP policy in their chosen project area, e.g. isolation policy, cleaning policy, etc.
- Undertaking an audit of practice against the policy to review what is actually happening in the trust/ project area (process mapping) before implementing a change.
- Forming their multidisciplinary teams with all key stakeholders.
- Identifying and setting their project aims, ensuring they were time-specific, measurable and defined the population or system which would be affected.
-
Developing their initial driver diagram, including identification of their proposed initial tests of change. Understanding and adopting the IHI improvement methodology, developing PDSA cycles which they would potentially use to test these changes.During the action period, the project team supported participants utilising teleconferences, webinars, support materials and the development of an NHS networks web page. The amount of support provided was bespoke to each participating team needs. Some trusts had improvement teams which helped facilitate the process, other trusts did not and therefore they required more support from NHS Improvement.
-
Second stage (action periods 2 and 3):In days 31–59, teams undertook small scale tests of change using the PDSA cycles to understand how these interventions would work in their organisations. Local data collection continued in order to evaluate the impact of changes. In this stage, the aim was to share best practice ideas and knowledge to rapidly adopt, adapt or abandon changes that were tested. The programme focused on ‘all teach, all learn’ as all organisations who were invited to participate had good practice examples to share.In days 61–89 teams pulled together the findings from their testing to understand the impact of changes tested. Teams began to scale up the interventions that worked and developed plans for dissemination across their organisations.Support from the project team was provided during the action periods as described previously. However, it was further enriched with project team site visits and peer site visits with other QI collaborative participants. The intention was to foster peer-based support and learning.
Model for Improvement: The organisations which participated in the IP QI collaborative followed the Model for Improvement approach developed by Langley et al. (2009). The approach has three key questions which the participating teams focused on: What are we trying to accomplish? How will we know that the change is an improvement? What changes are needed to deliver the improvement?
Table 2.
IP QI collaborative areas of focus.
| Trust | QI focus |
|---|---|
| Bedford Hospital NHS Trust, UK | Reduction of CDI by targeting, documentation of isolation and specimen collection |
| Northampton General Hospital NHS Trust, UK | Reduction of CDI by targeting, documentation of isolation and specimen collection |
| The Royal Wolverhampton NHS Trust, UK | Improve CPE risk assessment on admission to the Surgical Emergency Unit |
| University Hospitals of North Midlands NHS Trust, UK | Improving assessment, practice and care of urinary catheters |
| United Lincolnshire Hospitals NHS Trust, UK | Reduction of CDI by putting into place interventions for GDH-positive patients |
| West Hertfordshire Hospitals NHS Trust, UK | Improve IPC practices in theatres focusing in environmental and equipment cleanliness |
Figure 2.
Example of driver diagram developed by The Royal Wolverhampton NHS Trust, UK.
Sustainability and spread
The project team ensured that at each discussion/learning session, scale up and spread was part of the change process planning. Some changes required amendments to policies, escalation to Boards, staff training, securing further funding/resources, etc.
Method 2: evaluating the participation experiences of the lead IP nurses
Throughout the QI collaborative, participants fed back their experiences of the process to the project team; this facilitated the programme design and ensured it met learning needs and styles of the participants.
In order to garner the participants’ overall experiences of participating in the QI collaborative, the lead IP nurses completed a brief questionnaire on behalf of their teams at the end of the programme. Responses to the following three key questions were requested: What barriers to change were identified? Were there benefits of participating in a QI collaborative? What small scale changes did you achieve (prior to scale up)?
Method 3: measuring the potential success of QI collaborative in organisations
During learning session 4, the participating teams completed the MUSIQ framework (Kaplan et al., 2012). The MUSIQ framework tool was chosen as it can be used by organisations and QI researchers to understand and optimise contextual factors affecting the success of a QI project, e.g. leadership, resources, team membership, organisational culture, etc.
Ethical approval
Ethical approval and patient consent were not needed to undertake this work as this was not considered study research, but rather service evaluation/quality improvement project (NHS Health Research Authority, 2016).
Results
Evaluating the participation experiences of the lead IP nurses
The perceptions of the lead IP nurses who participated in the QI collaborative are discussed below. The three themes explored included: achievements; barriers to change; and benefits of participating in a QI collaborative. Their perceptions offer an insight into the approach used.
What small-scale changes did you achieve (prior to scale-up)?
Each participating group undertook their own bespoke IP QI topic. Therefore, commonalities of success were not evaluated. Nonetheless, the six teams all identified a positive outcome from their QI interventions. Matron for IP at Northampton General Hospital NHS Trust with a project to improve compliance with isolation practices associated with minimising C. difficile infection observed that: ‘IP Society isolation audit compliance improved from 51% at day 0 to 100% at day 90 and following the collaborative no patient developed CDI for 49 days –a success that had not been achieved at the trust for many years before the collaborative’. At The Royal Wolverhampton NHS Trust the, IP Nurse Manager and the team introduced a Carbapenemase Producing Enterobacteriaceae (CPE) risk-assessment screening tool in to the Surgical Emergency Unit (SEU) where they ‘increased screening in the Surgical Emergency Unit from 0% on inception to 73% after the second PDSA cycle; an average screening rate of 34% was achieved over the 15 weeks pilot. The programme also encouraged development of a trust-wide scale up plan which is now in place’. Following the QI project to improve compliance of IP in theatre 4, Assistant DIPC West Hertfordshire Hospitals NHS Trust reported: ‘At the end of the QI collaborative there was improved ownership and engagement from all staff groups. Equipment cleanliness improved from 70 to 100% in theatres’. Lead Nurse IP at University Hospitals of North Midlands NHS Trust found that ‘Doctors fed back that they were now routinely reviewing the need for short-term catheter on each ward round and long-term catheter weekly during ward round’.
In addition to the potential successes associated with their bespoke QI topic, the lead IP nurses identified additional benefits associated with undertaking the QI. For example, one Associate DIPC Bedford Hospital NHS Trust noted ‘Staff developed a better understanding of IP and started acting on what they were seeing rather than depending upon IP for the answers’. Lead Nurse IP United Lincolnshire Hospitals NHS Trust identified that ‘Increased awareness sparked constructive debate with clinical staff’. This was also supported by the Assistant DIPC West Hertfordshire Hospitals NHS Trust who noted: ‘Individual staff all could articulate the changes and where they wanted to be’.
What barriers to change were identified?
As with any change in practice, the lead IP nurses and members of the multidisciplinary groups identified that challenges and barriers had to be overcome. The themes identified from the six lead IP nurses reflected those highlighted by the Health Foundation, 2013 (Table 1). These are eloquently summarised by the IPC Matron Northampton General Hospital NHS Trust: ‘The “I’m too busy” culture; initially staff were sceptical about the collaborative and the improvements that could be made by QI. They felt that they didn’t have sufficient time available to commit to the QI process. However, once the IP team delivered QI training with them, this barrier was overcome and the ward managers actually embraced the process, drove the improvements and owned the changes made. Also, the fast pace of the collaborative – some weeks wards hadn’t made any progress or completed their actions from the weekly meetings which slowed the momentum at times but this was regained by additional support in that ward by the IP team’. As the lead Nurse IP at United Lincolnshire Hospitals NHS Trust identified, ‘Having a strategic approach is key to success. Don’t give up – use the PDSA cycles to guide approach’.
Were there benefits of participating in a QI collaborative?
As identified, undertaking an IP QI collaborative is still a relatively novel methodology. Therefore, we were keen to identify whether lead IP nurses thought that there were benefits from coming together as a collaborative.
The key elements reported were: a) the benefit they all had from realising they were not alone and b) the sharing of successful and not-so-successful change ideas and processes. Hence, we also asked if they would recommend the IP QI collaborative approach to other hospitals should a further programme be developed. The collective response is summarised by the IP Matron Northampton General Hospital NHS Trust: ‘Having known nothing about QI at the start of this journey I was sceptical that it would generate any meaningful change to practice and to patient care, but it has. Our perception of QI changed so much during the 90 days. Utilising QI methodology and change theory in IP practice has enabled us to generate simple but extremely effective improvements to practice that reduce the risk of infection to our patients. The process is so versatile, once you learn how to use it you will find yourself applying it to other areas of practice, often before you even realise! It’s simple, easy to cascade, easy to implement and it delivers results that benefit patients in a timely manner’. The IP Nurse Manager at Royal Wolverhampton NHS Trust identified one of the benefits as ‘It enhances project management skills; however, you must ensure that the aims and measurables are achievable and realistic, and ensure that key stakeholders are engaged early on in the project for maximum success’. An Associate DIPC Bedford Hospital NHS Trust, UK summarised the benefits of participation as having the platform to ‘share ideas, network, consolidate information and standardise’ with the other participating organisations and, importantly, to realise that ‘you are not alone’.
Measuring the potential success of QI collaborative in organisations
The participating teams scored themselves from 114 to 148 on the scale, thus indicating that they ranged between ‘project could be successful, but possible contextual barriers’ to ‘project has a reasonable chance of success’. In response to these findings, the project team provided additional support in the form of ongoing advice and further visits after completion of the 90-day QI collaborative, as required by the participants.
Discussion
The 90-day multicentre, multitopic IP QI collaborative achieved results which increased the knowledge and practice of improvement science deployment in the participating centres.
The MUSIQ evaluation scores suggest that the projects undertaken by the participating teams have the potential to be successful. A future QI collaborative would benefit from planning post-collaborative support into the programme at the initial design stage. This would ensure that participants were aware of the ongoing support available.
The PDSA cycles rapidly test changes to assess their impact. This helps to ensure new ideas improve quality before implementation on a wider scale, as changes may cause unexpected results/unintended consequences. The participating teams initially used PDSA cycles which were too large and closely resembled research studies rather than small-scale changes. This improved with the support of the project team and demonstrated the importance of the supportive interactions from NHS Improvement. Therefore, it is important to note when undertaking this QI methodology to keep changes small and measure change using regular data checks.
Adopting the QI collaborative methodology for IP was new for both those participating and those leading the collaborative. However, the feedback and evaluation from the lead IP nurses who participated in the collaborative have demonstrated that it is worthy of further development. Future refinements of the process may include: limitation of the topic to a single focus; development of the ongoing support offer once the 90-day QI collaborative has concluded the approach to developing a collective culture of learning; and sharing among our organisations was felt to be successful in both helping IP nurses to deliver improvement in their chosen topic area but also provide QI skills which they have taken forward into other projects.
Limitations of the process
The authors acknowledge the limitations of the IP QI collaborative. This was a 90-day QI collaborative and therefore there was no expectation of identifying statistically significant improvements.
Dückers et al. (2014) noted that interpretation of QI collaborative results must be undertaken with caution and results may be seen more as an encouragement to progress larger studies. Mittman (2004) also identified concerns when reviewing QI collaborative publications as ‘they include outcome measures that rely on participants’ un-validated self-reports or collaborative leaders’ subjective ratings of readily observed phenomena (such as team enthusiasm, commitment, and adherence to the collaborative process) rather than objective measures of clinical practice or outcome change’. However, this should not detract from the benefits such a process can facilitate with respect to initiating and driving small-scale change before scale-up and spread both within a single trust and within the wider collaborative.
Acknowledgments
The Midlands and East IP QI collaborative would like to thank the following for their ongoing support in delivering the collaborative in this region: Ailsa Brotherton, Gaynor Evans, Linda Dempster, Victor Oladele, Richard Seal, Jacqueline McKenna and Ruth May; and the peer reviewers at the Journal of IP for their support in the development of this article.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Department of Health. (2013) UK Five Year Antimicrobial Resistance Strategy 2013 to 2018. London: Department of Health; Available at: https://www.gov.uk/government/publications/uk-5-year-antimicrobial-resistance-strategy-2013-to-2018 (accessed 9 June 2017). [Google Scholar]
- Department of Health. (2015) The Health and Social Care Act 2008 Code of Practice on the prevention and control of infections and related guidance. London: Department of Health; Available at: https://www.gov.uk/government/publications/the-health-and-social-care-act-2008-code-of-practice-on-the-prevention-and-control-of-infections-and-related-guidance (accessed on 9 June 2017). [Google Scholar]
- Dückers MLA, Groenewegen PG, Wagner C. (2014) Quality improvement collaboratives and the wisdom of crowds: spread explained by perceived success at group level. Implementation Science 9: 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Foundation. (2013) Quality Improvement made simple: What everyone should know about health care quality improvement. London: Health Foundation; Available at: http://www.health.org.uk/publication/quality-improvement-made-simple (accessed 9 June 2017). [Google Scholar]
- IP Society. Audit tools. Available at: http://www.ips.uk.net/professional-practice/quality-improvement-tools/quality-improvement-tools/ (accessed 26 July 2016).
- Institute of Healthcare Improvement. (2003) The Breakthrough Series: IHI’s Collaborative Model for Achieving Breakthrough Improvement. IHI Innovation Series white paper. Boston, MA: Institute for Healthcare Improvement. [Google Scholar]
- Kaplan H, Provost L, Froehle C, Margolis P. (2012) The Model for Understanding Success in Quality (MUSIQ): building a theory of context in healthcare quality improvement. British Medical Journal Quality and Safety 21: 13–20. [DOI] [PubMed] [Google Scholar]
- Langley GJ, Moen RD, Nolan KM, Nolan TW, Norman CL, Provost LP. (2009) The Improvement Guide. 2nd ed. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Mittman B. S. (2004) Creating the evidence base for quality improvement collaboratives. Annals of Internal Medicine, 140(11), 897-901. [DOI] [PubMed] [Google Scholar]
- NHS Health Research Authority. (2016) Defining Research. London: Health Research Authority; Available at: www.hra.nhs.uk/documents/2016/06/defining-research.pdf (accessed 9 June 2017). [Google Scholar]
- Public Health England. (2016) Plans to prevent hospital infections include more money for hospitals who reduce infection rates and publishing E. coli rates by local area. London: Public Health England; Available at: https://www.gov.uk/government/news/reducing-infections-in-the-nhs (accessed 13 February 2017). [Google Scholar]