Understanding the cost of initiating and operationalizing colorectal cancer (CRC) control programs is essential for planning successful implementation of evidence-based recommendations to reduce disparities in the use and quality of CRC cancer screening services. Currently, only about 58% of adults ages 50–75 years in the United States are up-to-date with CRC screening recommendations; adults without health insurance have a much lower uptake of about 24% (Sabatino, White, Thompson, & Klabunde, 2015). Targeted interventions and programs, especially those focused on the uninsured and underinsured populations, are required to meet the population-wide target of 80% by 2018 set by The National Colorectal Cancer Roundtable (NCCRT, n.d.). The Community Guide contains several evidence-based recommendations for screening promotion interventions but there are very few studies on the economics of screening program implementation (Baron et al., 2010; Sabatino et al., 2012). There is an urgent need to increase the number of ‘implementation economics’ studies to develop the evidence-base to guide funding decision making, design cost-effective programs and ensure optimal use of limited resources. We define ‘implementation economics’ as a sub-discipline within implementation science that focusses on economic evaluation related to cost (cost-of-illness analysis, program cost analysis), cost-effectiveness, cost-benefit, cost-utility, budget impact, and cost minimization.
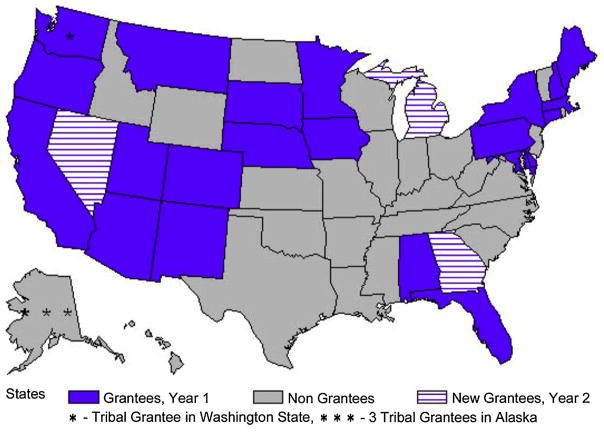
For more than a decade, CDC has funded and provided technical support to a range of grantee programs to implement CRC screening and implementation economics has been a cornerstone of the evaluations of these programs. Between 2005 and 2009, CDC administered the Colorectal Cancer Screening Demonstration Program (CRCSDP) in five programs [Baltimore, Maryland; St. Louis, Missouri; the entire state of Nebraska; Suffolk County, New York; and King, Clallam and Jefferson counties in Washington] (Centers for Disease Control and Prevention, 2013a). These programs provided CRC screening for low-income, underinsured, or uninsured men and women between the ages of 50 and 64 years. In 2009, successes and lessons learned (Centers for Disease Control and Prevention, 2013b; Joseph, DeGroff, Hayes, Wong, & Plescia, 2011) from the CRCSDP informed planning and funding of the first round of CDC’s Colorectal Cancer Control Program (CRCCP) (2009–2015). Through the CRCCP, CDC provided funding to 22 states and 4 tribal organizations to implement CRC programs starting in 2009 and another 3 states were added to the program in 2010. Fig. 1 provides a map of the United States highlighting the CRCCP grantees.
Fig. 1.
CDC’s Colorectal Cancer Control Program Grantees (1999–2015).
The CRCCP represents a new approach for disseminating evidence-based interventions and promoting their use while simultaneously ensuring free screening for a portion of the medically underserved population. The CRCCP grantees used about two thirds of their funds to implement the population-based promotion activities (screening promotion) and the remaining third to deliver direct clinical screening services for low income uninsured individuals (screening provision). The grantees were encouraged to tailor the program to their individual settings within the broad framework provided by the CDC. To implement screening provision the grantees partnered with numerous organizations including Federally Qualified Health Centers, other health care systems, State Medicaid offices, professional organizations, employers and worksites, and private insurers. For screening provision, all grantees used United States Preventive Task Force-recommended tests with some using colonoscopies, others using fecal-based tests and several program providing multiple screening tests.
Several peer-reviewed manuscripts based on the economic evaluation of the earlier CRCSDP have been published (Subramanian, Bobashev, & Morris, 2010; Subramanian et al., 2013; Tangka et al., 2008; Tangka et al., 2013). These studies contributed to the implementation economics literature by quantifying the cost of starting and implementing CRC screening programs, assessing the resources required for specific programmatic activities and evaluating the clinical cost of delivering screening services. In this volume of Evaluation and Program Planning (Hoover et al., 2017; Subramanian et al., 2017; Tangka et al., 2017) we present a collection of three new studies on implementation economics that provide additional evidence to guide future CRC screening programs. These manuscripts provide a comprehensive evaluation as they represent the program, clinical and patient perspectives. Each of these different perspectives offers a unique opportunity to understand the viewpoint of key stakeholders involved in operationalizing screening programs and in combination offer a unique opportunity to assess multi-level factors required to ensure the success of these programs. For instance, understanding patient motivation, facilitators and barriers is critical to ensure individuals initiate screening and remain compliant with recommended screening schedules.
In the first manuscript, Tangka et al. (2017) focus on the program perspective and provide a detailed review of the screening promotion interventions implemented by the CRCCP grantees along with the funding appropriated to each type of intervention. A key goal of the CRCCP was to encourage programs to adopt evidence-based interventions to promote screening with the aim of increasing colorectal screening at the population level. The results showed that all grantees engaged in at least one of The Community Guide-recommended strategies, including patient reminders and provider assessment, and the majority of the funds were expended on the strategies supported by the available evidence base. Approximately one-third of funding was spent on mass media which is not currently recommended due to lack of evidence; this finding was instrumental in shaping CDC’s policies that changed from broad-based recommendations to targeted specific guidance and education on evidence-based interventions (Centers for Disease Control and Prevention, 2015). This study did not directly assess increases in population screening use, but suggested that a 5% increase in CRC screening could have been achieved for less than $35 per person.
In the second manuscript, Subramanian et al. (2017) address the clinical perspective by comparing the non-clinical (programmatic) and clinical cost of screening programs that use Fecal Occult Blood Test (FOBT) or Fecal Immunochemical Test (FIT) versus colonoscopy. Non-clinical costs include all costs not directly related to provision of clinical services such as cost for patient navigation, program management, quality assurance and professional development, partnership development and maintenance, data collection and tracking, and program monitoring and evaluation. Over the 3-year study period, colonoscopy programs had higher clinical costs per person screened than FOBT/FIT. Overall, FOBT/FIT-based and colonoscopy programs had similar non-clinical costs per person served of approximately $1000. The authors conclude that CRC screening programs incur substantial non-clinical costs, regardless of whether the program is colonoscopy or FOBT/FIT-based and therefore both non-clinical and clinical costs could be considered in future program planning and funding decision making.
The last manuscript in this series focuses on the patient perspective and reports on findings from a patient survey. Hoover et al. (2017) reveal that even when colonoscopies were provided free, patients incurred significant costs related to lost productivity and travel. Among the low income population of mostly uninsured individuals in Philadelphia, patients incurred an average cost of about $340 and caregivers who accompanied the patients to visits incurred approximately $80. These patient and caregiver costs may be important barriers that contribute to low CRC screening use, especially among the low-income population.
The lessons learned from these three papers offer valuable insight to the broad range of stakeholders actively engaged in CRC control initiatives. First, through the use of systematic data collection processes, detailed cost and resource use information can be successfully collected from CRC programs, providers, and clients. The data collection tools and surveys developed through the CRCCP evaluation provide standardized instruments for future research. Second, to successfully implement CRC screening promotion and provision activities, programs have to engage in multiple activities related to programmatic oversight and clinical services. Therefore, adequate funding needs to be provided so these interlinked activities can be established and operationalized. Third, it is important to assess costs from multiple perspectives, especially those incurred by patients which are often not included in economic evaluation of cancer screening. Costs borne by patients related to lost wages and transportation can be important barriers that need to be further evaluated.
Additionally lessons learned from these CRC program economic evaluations were incorporated in planning the second round of CRCCP funding (New CRCCP) (2015–2020) through which CDC funded 24 state health departments, 6 universities, and one American Indian tribe (Centers for Disease Control and Prevention, 2015). CDC is continuing its commitment to advance the science of implementation economics by supporting a systematic evaluation of selected current CRCCP grantees. Evaluation of the cost-effectiveness of effective interventions can identify the most efficient use of available resources, contribute to the economics evidence-base for The Community Guide, and help increase CRC screening rates to meet national goals (NCCRT, n.d.). These future economic studies will continue to build on the evidence base initiated through the publications of the compilation of the three papers presented in this volume of Evaluation and Program Planning.
Finally, the lessons learned through these studies can be generalized beyond the CRCCP and CRC screening to other non-communicable disease management programs. Patient compliance and cost-effective delivery of multi-component programs remains a challenge across a wide range of screening and treatment modalities including cervical and breast cancer screening, and hypertension and diabetes management. Performing economic evaluation incorporating a wide variety of perspectives can provide a more comprehensive understanding of facilitators and barriers to help design programs that are both efficient and effective in achieving their goals.
Acknowledgments
Funding
This work was funded in part by Centers for Disease Control and Prevention Contract Number 200–2008-27958, Task Order 01, to RTI International.
Contributor Information
Florence K.L. Tangka, Division of Cancer Prevention and Control, Centers for Disease Control and Prevention, 4770 Buford Highway, NE, Mailstop K-76, Atlanta, GA, 30341-3717, USA.
Sujha Subramanian, RTI International, 307 Waverley Oaks Road, Suite 101, Waltham, MA, 02452 USA.
References
- Baron RC, Melillo S, Rimer BK, Coates RJ, Kerner J, Habarta N, et al. Intervention to increase recommendation and delivery of screening for breast, cervical: And colorectal cancers by healthcare providers a systematic review of provider reminders. American Journal of Preventive Medicine. 2010;38:110–117. doi: 10.1016/j.amepre.2009.09.031. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control, & Prevention. Colorectal cancer screening program evaluation. Program history. Atlanta, GA: Centers for Disease Control and Prevention; 2013a. [Accessed March 6, 2016]. from http://www.cdc.gov/cancer/crccp/supplement.htm. [Google Scholar]
- Centers for Disease Control, & Prevention. Special issue: Comprehensive evaluation of the centers for disease control and prevention’s colorectal cancer screening demonstration program, supplement to cancer i–iii. 2013b;(119):2817–2946. http://www.cdc.gov/cancer/crccp/supplement.htm.
- Centers for Disease Control, & Prevention. Colorectal cancer control program (CRCCP) Atlanta, GA: Centers for Disease Control and Prevention; 2015. [Accessed March 6, 2016]. from http://www.cdc.gov/cancer/crccp/ [Google Scholar]
- Hoover S, Subramanian S, Tangka F, Cole Beebe M, Kramer C, Pacillo G. Patients and caregivers costs for colonoscopy-based colorectal cancer screening: Experience of low-income individuals undergoing free colonoscopies. Evaluation and Program Planning. 2017;62:81–86. doi: 10.1016/j.evalprogplan.2017.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph DA, DeGroff AS, Hayes NS, Wong FL, Plescia M. The Colorectal Cancer Control Program: Partnering to increase population level screening. Gastrointestinal Endoscopy. 2011;73:429–434. doi: 10.1016/j.gie.2010.12.027. [DOI] [PubMed] [Google Scholar]
- National Colorectal Cancer Roundtable (NCCRT) [Accessed January 22, 2016];80% screening rate by 2018 National Colorectal Cancer Roundtable. n.d from http://nccrt.org/tools/80-percent-by-2018.
- Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, et al. Effectiveness of interventions to increase screening for breast, cervical: And colorectal cancers: Nine updated systematic reviews for the Guide to Community Preventive Services. American Journal of Preventive Medicine. 2012;43:97–118. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Sabatino SA, White MC, Thompson TD, Klabunde CN. Cancer screening test use—United States, 2013. MMWR Morbidity and Mortality Weekly Report. 2015;64:464–468. [PMC free article] [PubMed] [Google Scholar]
- Subramanian S, Bobashev G, Morris RJ. When budgets are tight: There are better options than colonoscopies for colorectal cancer screening. Health Affairs. 2010;29:1734–1740. doi: 10.1377/hlthaff.2008.0898. [DOI] [PubMed] [Google Scholar]
- Subramanian S, Tangka FK, Hoover S, Beebe MC, DeGroff A, Royalty J, et al. Costs of planning and implementing the CDC’s colorectal cancer screening demonstration program. Cancer. 2013;119(Suppl 15):2855–2862. doi: 10.1002/cncr.28158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S, Tangka F, Hoover S, Royalty J, DeGroff A, Joseph D. Costs of colorectal cancer screening provision in CDC’s Colorectal Cancer Control Program: Comparisons of colonoscopy and FOBT/FIT based screening. Evaluation and Program Planning. 2017;62:73–80. doi: 10.1016/j.evalprogplan.2017.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangka FK, Subramanian S, Bapat B, Seeff LC, DeGroff A, Gardner J, et al. Cost of starting colorectal cancer screening programs: Results from five federally funded demonstration programs. Preventing Chronic Disease. 2008;5:A47. [PMC free article] [PubMed] [Google Scholar]
- Tangka FK, Subramanian S, Beebe MC, Hoover S, Royalty J, Seeff LC. Clinical costs of colorectal cancer screening in 5 federally funded demonstration programs. Cancer. 2013;119(Suppl 15):2863–2869. doi: 10.1002/cncr.28154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangka FK, Subramanian S, Hoover S, Royalty J, Joseph K, DeGroff A, et al. Costs of promoting cancer screening: Evidence from CDC’s Colorectal Cancer Control Program (CRCCP) Evaluation and Program Planning. 2017;62:67–72. doi: 10.1016/j.evalprogplan.2016.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]