Abstract
Many studies have documented barriers to colorectal cancer screenings. However, there is lack of comprehensive information on the time and costs borne by low-income patients and the persons accompanying the patient (caregiver) for colonoscopies in the United States. We surveyed patients in three health clinics in Philadelphia retrospectively who had undergone free colonoscopies in the previous 18-month period. Participants were asked questions about time and out-of-pockets expenses for themselves and their caregivers. Even when colonoscopies were free to the patient through Colorectal Cancer Control Program funded by the Centers for Disease Control and Prevention, the patient and caregivers still incurred costs in relation to preparing for, undergoing, and recovering from a colonoscopy. These costs can be substantial and may account for some of the low colorectal cancer screening rates especially among the low-income populations. Patients’ and caregivers’ costs need to be considered when designing and implementing colorectal cancer control programs.
Keywords: Colonoscopy, Cancer screening, Patients and caregivers costs and cost analysis
1. Introduction
Colorectal cancer (CRC) screening has been shown effective in reducing mortality from CRC (Zauber et al., 2008). The U.S. Preventive Services Task Force recommends CRC screening for average-risk adults aged 50–75 years using high-sensitivity fecal based test annually, sigmoidoscopies every 5 years with fecal-based testing every 3 years, or a colonoscopy once every 10 years (U.S Preventive Services Task Force, 2008). Yet the take-up rate for any CRC screening remains low: less than 60% of men and women aged 50 and older are up-to-date with CRC screening (Sabatino, White, Thompson, & Klabunde, 2015). Among uninsured, fewer than 1 in 4 received the recommended screening for CRC (Sabatino et al., 2015). In an effort to increase CRC screening rates, the Centers for Disease Control and Prevention (CDC) established the Colorectal Cancer Control Program (CRCCP) in 2009. The CRCCP funded 29 grantees, both states and tribal organizations, for a period of 6 years to support screening provision and promotion activities.
Many studies have documented barriers to cancer screenings in general and CRC screenings in particular. The barriers include low levels of education, language or communication challenges, low socioeconomic status, and lack of insurance coverage (Gimeno Garcia, 2012; Heitman, Au, Manns, McGregor, & Hilsden, 2008; Subramanian, Klosterman, Amonkar, & Hunt, 2004). Cost has also been cited as a barrier (Jones, Devers, Kuzel, & Woolf, 2010; Klabunde et al., 2005). A report conducted by the National Institutes of Health’s Center to Reduce Cancer Health Disparities detailed three main cost categories: direct, indirect, and intangible costs. Direct medical costs are those related to the provision of clinical services, such as facilities and clinician fees, and cost of medical supplies including bowel prep products. Direct nonmedical costs include all costs not directly related to medical services such as transportation and child care costs. Indirect costs are also nonmedical costs and relate to cost of time lost from work (lost productivity cost) by the patient and caregivers as a result of their commitment to the clinical procedure. Intangible costs include costs associated with adverse effects from the clinical procedure on the quality of life (Center to Reduce Cancer Health Disparities (U.S.), 2007).
Few studies had examined the nonmedical costs (which includes direct nonmedical cost and indirect cost) of screening for CRC (Frew, Wolstenholme, Atkin, & Whynes, 1999; Heitman et al., 2008; Henry, Ness, Stiles, Shintani, & Dittus, 2007; Jonas, Russell, Sandler, Chou, & Pignone, 2007; Yabroff, Borowski, & Lipscomb, 2013). In a recent review, Yabroff and colleagues found that of 65 international studies published in 2000–2010, only 18 addressed costs for patient or caregiver time, travel, or lost productivity (Yabroff et al., 2013). These studies did not specifically focus on CRC screening, and they were mostly related to cancer care. There is no study to date that provides a comprehensive assessment of the cost to low-income patients and those who accompany them for colonoscopy screening (caregivers) in the United States. These costs can be an important barrier for undergoing colonoscopy screening.
In this study we examine the costs borne by patients who underwent CRC screening and their caregivers at three community health centers in innercity Philadelphia, Pennsylvania. These clinics all participated in the CRCCP program in Pennsylvania and offered free colonoscopy screening. This article provides an important contribution to the literature as it evaluates a potentially significant barrier to CRC screening among the disadvantaged low-income population who are either uninsured or underinsured.
2. Methods
2.1. Questionnaire development
A questionnaire was developed and pretested that captured patient sociodemographic characteristics as well as time requirements and expenses incurred through the CRC screening process. In developing the questionnaire, we reviewed existing surveys and the published literature in order to use standardized questions where possible. Questions included time spent traveling, time spent waiting at the physician office, and time spent undergoing procedures. The questionnaire also collected details on the travel expenses for precolonoscopy visits, the colonoscopy procedure, and postcolonoscopy visits; bowel prep product and childcare expenses. Patients were also asked about how they traveled to the visits (e.g., private or public transportation) and whether they had someone to accompany them. Questions about the caregiver work status and position were asked to determine their costs incurred in assisting the patient. In this manuscript, “caregivers” refer to spouses, family members, and friends who accompanied the respondent to any colonoscopy appointments. Although colonoscopies were provided free through the CDC’s CRCCP to all patients; in some instances patients had to pay a proportion of the cost for bowel prep products. This would constitute direct medical cost and was captured when relevant.
Once the questionnaire was drafted, it was pretested to finalize wording of the questions and order of presentation. This study was approved by RTI International’s institutional review board and the Office of Management and Budget (OMB Control No. 0920-0963).
2.2. Data collection approach
One of the grantees of the CDC’s CRCCP was Pennsylvania, which funded clinics to provide colonoscopies at no cost to patients. The project team partnered with three funded community health centers in Philadelphia to conduct the study. We used a convenience sample of average risk individuals 50–74 years who has received CRCCP funded colonoscopy screening within an 18 month period (June 2012 to November 2013). Our goal was to complete 150 questionnaires to ensure that adequate sample was available for this exploratory analysis. Medical assistants reviewed patient charts and clinical records to identify patients who underwent CRCCP funded screening colonoscopies. The medical assistants then contacted the selected individuals in person (if they had an upcoming appointment at the center) or via telephone to explain the study and ask whether they would participate. After obtaining patient consent, the medical assistants scheduled an in person visit to complete the questionnaire. All patients who were approached, agreed to participate and there were no refusals. Patients received a $20 gift card as incentive. All questionnaires were administered in English and data collection occurred during November–December 2013. A total of 150 questionnaires were administered in the three sites and deidentified data was compiled for analysis.
2.3. Data analysis
Demographics and work status information were summarized for patients and caregivers. We categorized the time and cost into four activity groups: attend a precolonoscopy office visit, prepare for a visit, attend a colonoscopy visit, and attend a postcolonoscopy office visit. The amount of time spent for each visit was assumed to be the same for the patient and the caregiver (if the patient was accompanied).
We report the actual time and cost estimates in 2013 U.S. dollars for persons who incurred them, and the mean across all questionnaire respondents. To calculate the cost of lost time attending colonoscopy-related visits (opportunity cost), we used wage information ($11.68/h for respondents and $14.97/h for the caregivers) from the Bureau of Labor Statistics and took a weighted average based on occupation reported by those working. This ensures that the time of all individuals (those employed and those not in formal employment) is accounted for (Bureau of Labor Statistics, 2015). Also, if respondents did not report costs to travel to doctors’ offices, we assigned mileage costs of 23 cents per mile, based on Internal Revenue Service mileage allowance for medical purposes, and estimated a distance traveled of 10 miles each way. We learned that clients generally lived near the health centers, and we assumed that caregivers traveled together with the patients.
We do not separately report results based on data for less than 10 respondents, but we do include the information in aggregate results. For example, we do not report time missed for post-colonoscopy visits because few respondents who attended one missed work. However, we do include this time in the total time. We follow the same logic for data reported on costs. So few respondents reported requiring child care that we excluded them from the total costs.
3. Results
Patients who received free colonoscopies are described in Table 1. Three-quarters were women, and on average, they were 58.9 years old (range = 52–81). Most were African Americans (69.3%) and fluent in English (72.7%). Seventy-three percent of respondents had at least a high school diploma or the equivalent. Thirty-eight percent of respondents were employed either full- or part-time, and more than half (56.1%) were employed in the services industry (e.g., home health aide, firefighter, cook, maid, waitress, gardener/landscaper). Only 16.0% had health insurance (private, Medicare, or Medicaid).
Table 1.
Demographics Education, and Employment Status of Patients Undergoing Colonoscopy.
| Variables | N | % |
|---|---|---|
| Age (years) | ||
| 52–59 | 84 | 56.0 |
| 60+ | 66 | 44.0 |
| Female | 112 | 74.7 |
| Race | ||
| Black or African American | 104 | 69.3 |
| Asian | 28 | 18.7 |
| Other | 18 | 12.0 |
| Fluent in English | 109 | 72.7 |
| Highest grade of school or college finisheda | ||
| Less than high school | 41 | 27.3 |
| High school or GED | 53 | 35.3 |
| More than high school | 56 | 37.3 |
| Employment status (patient) | ||
| Working full-time | 35 | 23.3 |
| Working part-time | 22 | 14.7 |
| Not working (includes retired, staying at home to work, keeping house) | 93 | 62.0 |
| Current work status—position (patient) | ||
| Services | 32 | 56.1 |
| Other (e.g. transportation, production and maintenance) | 25 | 43.9 |
| Health insurance | ||
| No insurance | 126 | 84.0 |
| Medicaid/medical coupons/CHIP | 14 | 9.3 |
| Other (Medicare, private coverage) | 10 | 6.7 |
| Relationship of person who accompanied you | ||
| Spouse | 26 | 17.3 |
| Friend | 42 | 28.0 |
| Other family member | 82 | 54.7 |
| Employment status (caregiver) | ||
| Working full-time | 44 | 29.3 |
| Working part-time | 22 | 14.7 |
| Not working (includes retired, staying at home to work, keeping house, don’t know) | 84 | 56.0 |
| Current work status—position (caregiver) | ||
| Services | 25 | 36.8 |
| Professional | 12 | 17.6 |
| Other (e.g. transportation, production and maintenance) | 31 | 45.7 |
Values do not total 100% because of rounding.
Respondents were asked about the people who accompanied them to the various colonoscopy appointments. All respondents had someone accompany them to attend at least one appointment. Most often (72.0%) this person was a family member or spouse. Among caregivers, 29.3% were employed full-time and 14.7% were employed part-time. Many of those who were employed (36.8%) were in the services industry.
Not all employed patients missed work for various parts of the colonoscopy process, likely because they were able to schedule the colonoscopy to fit their work obligations. Of employed respondents, 43.9% had to miss work to attend a precolonoscopy visit. Nearly one-quarter (22.8%) had to miss work to prepare for the colonoscopy, and slightly more than half (50.9%) had to miss work for the colonoscopy itself. On average, employed respondents who missed work missed 6.1–8.0 h for each of the various colonoscopy appointments. Employed respondents missed 6.1 h of work for a precolonoscopy visit and 6.9 h preparing for and 7.4 h attending the colonoscopy.
Table 2 displays the time needed and estimated cost of this lost time for patients undergoing colonoscopies and caregivers. Patients spent approximately 1.2 h at a precolonoscopy visit and 0.9 h traveling to it, which resulted in $24.95 in lost time. Thirty-seven percent of patients had someone accompany them to the precolonoscopy visit, equaling $11.73 in lost time across all caregivers. To prepare for a colonoscopy, patients spent 16.9 h, including reading the bowel preparation instructions. This equaled $196.54 in lost time. Patients spent 0.8 h traveling to and from the endoscopy center and 3.7 h having the colonoscopy resulting in a mean patient value of lost time of $51.97. Patients took 5.1 h to recover from the colonoscopy, translating into $59.80 in lost time. Only 13.3% of respondents reported having a postcolonoscopy visit. Across all respondents, patients spent 0.1 h in travel and 0.1 h at the visit, and this translated into $2.68 in lost time. In total, patients needed 28.8 h to undergo the colonoscopy screening, resulting in an indirect average cost of $335.95, while it cost the caregiver $79.03.
Table 2.
Mean Number of Hours Needed for a Colonoscopy and Estimated Value of Time Spent.
| Variables | N | Incurred by Patients | % of patients reporting activity | Incurred by Caregivera | |
|---|---|---|---|---|---|
|
|
|
||||
| Mean hours per patient (across all patients) | Mean cost per patient (across all patients) | Mean cost per patient (across all patients) | |||
| Attend precolonoscopy office visit | |||||
| Visited a nurse or doctor before the colonoscopy | 150 | n/a | n/a | n/a | n/a |
| Average hours spent at doctor’s office | 150 | 1.2 | $14.13 | 36.7 | $6.64 |
| Average hours spent traveling to the doctor’s office | 150 | 0.9 | $10.82 | 36.7 | $5.09 |
| Subtotal | 2.1 | $24.95 | $11.73 | ||
| Prepare for colonoscopy | |||||
| Average hours spent reading bowel preparation instructionsb | 150 | 0.3 | $3.12 | n/a | n/a |
| Average hours spent preparing for colonoscopy | 150 | 16.6 | $193.42 | n/a | n/a |
| Subtotal | 16.9 | $196.54 | n/a | ||
| Attend colonoscopy visit | |||||
| Average hours spent getting to and from the endoscopy center | 150 | 0.8 | $9.34 | 100 | $11.98 |
| Average hours spent at endoscopy center | 150 | 3.7 | $42.63 | 100 | $54.64 |
| Average hours it took to recover from the colonoscopy | 150 | 5.1 | $59.80 | n/a | n/a |
| Subtotal | 9.6 | $111.78 | $66.62 | ||
| Attend postcolonoscopy visit | |||||
| Average hours spent getting to and from post-colonoscopy visit | 20 | 0.1 | $1.25 | 2.7 | $0.32 |
| Average hours spent at post-colonoscopy visit | 20 | 0.1 | $1.43 | 2.7 | $0.37 |
| Subtotal | 0.2 | $2.68 | $0.69c | ||
| Total average cost of lost time | $335.95 | $79.03 | |||
| Total average time in hours | 28.8 h per patient; 5.3 h for caregiver | ||||
Weighted average wage for respondent = $11.68.
Weighted average wage for accompanying person (caregiver) = $14.97.
Amount of time spent per visit was assumed to be the same for both patient and person accompanying patient.
One person indicated they did not remember how many minutes it took to read the instructions, so we imputed the average.
Subtotal is based on small sample.
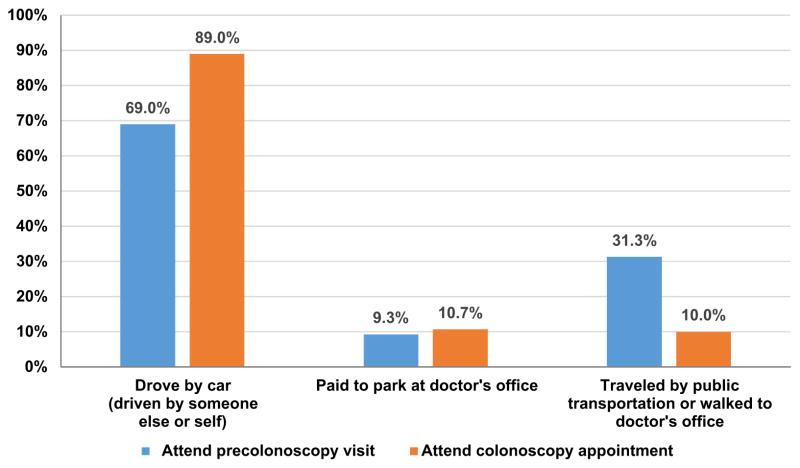
Fig. 1 compares how respondents traveled to the precolonoscopy and the colonoscopy visits. Most respondents traveled to the precolonoscopy and colonoscopy visits by car (69% and 89%, respectively). A small percentage of respondents paid to park at the doctor’s office (9.3% and 10. 7% for the precolonoscopy and colonoscopy visit, respectively). Three times as many respondents took public transportation or walked to the precolonoscopy appointment compared to the colonoscopy visit (31.3 versus 10.3%).
Fig. 1.
How Respondents Traveled to Doctors’ Appointments.
Note: One person did not report mode of transportation for colonoscopy appointment.
Table 3 shows travel and other costs for all colonoscopy visits. Across all patients, the travel costs were $13.10. The cost for traveling to the precolonoscopy visit was $5.54 and the travel cost to attend the colonoscopy was $6.75. Few attended a postcolonoscopy visit and the cost to travel to it was $0.81 when averaged across all patients. The average cost of the bowel preparation product was $4.36.
Table 3.
Travel and Other Costs for Colonoscopy Office Visits.
| N | % of patients reporting activity | Mean cost per patient reporting activity | Mean cost per patient (across all patients) | |
|---|---|---|---|---|
| Travel Cost | ||||
| Attend precolonoscopy office visit | ||||
| Cost to travel to doctor’s office by cara,b | 103 | 68.7 | $23.30 | $4.17 |
| Cost to travel to doctor’s office by public transportationc | 41 | 27.3 | $5.00 | $1.37 |
| Subtotal | $28.30 | $5.54 | ||
| Attend colonoscopy visit | ||||
| Cost to travel to doctor’s office by cara,b | 134 | 89.3 | $26.30 | $6.28 |
| Cost to travel to doctor’s office by public transportationc | 14 | 9.3 | $5.00 | $0.47 |
| Subtotal | $31.30 | $6.75 | ||
| Attend postcolonoscopy visit | 13 | 8.7 | $25.35 | $0.81 |
| Costs of travel to attend postcolonoscopy visitb,d | ||||
| Subtotal | $25.35 | $0.81 | ||
| Total travel cost | $13.10 | |||
| Cost of bowel preparation product | 61 | 40.7 | $10.71 | $4.36 |
| Total | $17.46 | |||
Includes cost of payment to be driven to doctor’s office, cost to park at doctor’s office and mileage costs.
Assumed 10-mile distance to endoscopy center (round trip = 20 miles). Used 2013 IRS mileage for medical purpose of 23 cents. Excluded respondents who reported payment for transportation or took public transportation.
For transportation cost, the percentage of patients will not sum to 100% as some individuals walked and one person did not report mode of transportation for colonoscopy visit.
Only 20 respondents attended a postcolonoscopy visit. Due to small sample size, the following categories comprise the total but could not be reported separately: cost of payment to be driven to doctor’s office; cost to park at colonoscopy appointment; cost to travel to doctor’s office by bus, train, or taxi; mileage costs for postcolonoscopy visit.
4. Discussion
In this study, based on retrospective self-reports, patients spent, on average, 23.7 h preparing for, traveling for and having a colonoscopy, and an additional 5.1 h, on average, recovering from the colonoscopy. This translated into a total cost of $335.95 for the patient in lost time and $79.03 for the caregiver. In addition, an estimated $17.46 was incurred in travel and other costs. Even when colonoscopy is provided free of charge to the patient, additional costs may be incurred which could be a significant barrier for low income individuals to receive CRC screening.
A few international studies have estimated the non-medical costs of screening colonoscopies but these estimates are not directly comparable to the present study that collected data on a low-income patients in the United States. Using patient questionnaires to collect nonmedical costs of both fecal occult blood test (FOBTs) and colonoscopies, researchers in Canada found that the costs for both patients and caregivers averaged Can$308 (2006 U.S. $271) for colonoscopy and Can$36 (2006 U.S. $32) for FOBTs (Heitman et al., 2008). Examining the indirect cost of flexible sigmoidoscopies through the use of patient surveys in Great Britain, researchers found that indirect costs totaled approximately £23 (1999 U.S. $14.20) (Frew et al., 1999). A study that was performed in the United States did not report costs but estimated that the time required to complete the screening colonoscopy process as approximately 21 h, (Jonas et al., 2007) which is similar to the time reported in this study.
Overall, the total cost of undergoing a “free” colonoscopy screening is substantial for a low-income patient, especially when the average hourly wage estimate used in this analysis for the patient was $11.68. This relatively high cost could explain the reason for the lower levels of compliance with screening recommendations among people with low education and generally low socioeconomic status (Centers for Disease Control and Prevention, 2013). Further, many service workers lack paid sick time, which may further impact the use of endoscopy tests (Peipins, Soman, Berkowitz, & White, 2012). The largest time cost was related to bowel preparation and undergoing the colonoscopy procedure; therefore, potentially, noninvasive fecal-based tests could result in lower burden in terms of time lost. Fecal tests, though, require much more frequent screening than colonoscopy and, therefore, may not effectively save much money over the long term. The need to repeat screening tests at regular intervals is also an important issue: if the need for multiple repeated screens is not met, especially for annual fecal tests, then there is a substantial reduction in the effectiveness of the test (Subramanian, Bobashev, & Morris, 2009; Subramanian, Bobashev, & Morris, 2010). In addition, colonoscopy may be an appropriate surveillance test for high-risk individuals (those with a family history of CRC or other risk factors) (U.S. Preventive Services Task Force, 2015). Colonoscopy is also required for diagnostic follow-up testing when fecal-based tests are positive; therefore, understanding approaches to improve completion of the screening process with colonoscopies is an important aspect of any CRC initiative that relies on fecal tests.
The role of financial incentives to increase patient compliance with colonoscopy screening recommendations is an understudied area of research. Pignone et al. (2014), using a discrete choice experiment, found that participants undergoing CRC screening preferred rewards or small copayments, compared to large copayments. The most recent review published by the Guide to Community Preventive Services found insufficient evidence to recommend patient incentives (Sabatino et al., 2012). Systematic evaluation of the role of incentives in screening colonoscopy use among the low-income population is needed. In addition, comparative evaluation of the role of fecal-based tests compared with that of colonoscopies is also essential to assess each screening test’s ability to address the low screening rates among the low-income, underinsured, and uninsured populations.
The study has several limitations. First, the retrospective nature of the study could have resulted in recall bias related to the time allotted to specific screening procedures. Second, the estimates are based on a nonrandom sample of patients within one city, so these results may not be generalizable to other populations. In addition, we did not include a comparison group to assess differences in time and cost of undergoing colonoscopy. Third, these cost estimates are likely to be a conservative estimate of the overall cost incurred. For example, costs for bowel preparation were low because we learned that a local store sold the product inexpensively and the health centers were able to provide free kits to some patients. Despite these limitations, the detailed breakout of the costs presented in this study offers program planners and policy makers a good approximation of the costs involved. This estimate can be tailored based on unique situations that may be present in the implementation of other colonoscopy screening programs.
5. Conclusions and lessons learned
The findings from this study offer insights into the economic barriers faced by low-income individuals when undergoing colonoscopy screening, even when the procedure itself is offered at no charge. Additional studies are required to understand the role of financial incentives and the most effective use of these incentives. The decision to undergo colonoscopy screening can be influenced by multiple interlinked factors, so financial incentives should be evaluated alongside other potential barriers. Financial incentives should be included in future assessments of health promotion interventions, as colonoscopy screening requires a substantial time commitment and the cost of lost time is significant, especially for the low-income population.
Acknowledgments
We would like to acknowledge the Pennsylvania Department of Health, Division of Cancer Prevention and Control, the grantee recipient of Centers for Disease Control and Prevention (CDC) Colorectal Cancer Control Program, and in particular April Barry, L.S.W, M.S.W., Colorectal Cancer Program Manager and Joseph Burkhart, Section Chief for the Division of Cancer Prevention and Control, for their assistance in choosing the Philadelphia Department of Health to participate in this study. Ms. Barry and Mr. Burkhart provided extensive training to Philadelphia Department of Health staff to ensure the parameters of the CDC study were executed appropriately by the Philadelphia Department of Health.
Abbreviations
- CDC
Centers for Disease Control and Prevention
- CRC
colorectal cancer
- CRCCP
Colorectal Cancer Control Program
- FOBT
fecal occult blood test
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. RTI International was supported by Centers for Disease Control and Prevention Contract Number 200-2008-27958, Task Order 01.
References
- Bureau of Labor Statistics. [Accessed 25 January, 2016];Labor force statistics from the current population survey: Annual table: Employment status by detailed age group, sex, and race. 2015 from http://www.bls.gov/cps/cpsaat03.pdf.
- Center to Reduce Cancer Health Disparities (U.S.) Economic costs of cancer health disparities: Summary of meeting proceedings. Rockville, MD: Dept. of Health & Human Services, National Institutes of Health, National Cancer Institute; 2007. [Google Scholar]
- Centers for Disease Control & Prevention. Vital signs: Colorectal cancer screening test use—United States, 2012. MMWR. Morbidity and Mortality Weekly Report. 2013;62:881–888. [PMC free article] [PubMed] [Google Scholar]
- Frew E, Wolstenholme JL, Atkin W, Whynes DK. Estimating time and travel costs incurred in clinic based screening: Flexible sigmoidoscopy screening for colorectal cancer. Journal of Medical Screening. 1999;6:119–123. doi: 10.1136/jms.6.3.119. [DOI] [PubMed] [Google Scholar]
- Gimeno Garcia AZ. Factors influencing colorectal cancer screening participation. Gastroenterology Research and Practice. 2012:483417. doi: 10.1155/2012/483417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heitman SJ, Au F, Manns BJ, McGregor SE, Hilsden RJ. Nonmedical costs of colorectal cancer screening with the fecal occult blood test and colonoscopy. Clinical Gastroenterology and Hepatology. 2008;6:912–917. e911. doi: 10.1016/j.cgh.2008.03.006. [DOI] [PubMed] [Google Scholar]
- Henry SG, Ness RM, Stiles RA, Shintani AK, Dittus RS. A cost analysis of colonoscopy using microcosting and time-and-motion techniques. Journal of General Internal Medicine. 2007;22:1415–1421. doi: 10.1007/s11606-007-0281-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas DE, Russell LB, Sandler RS, Chou J, Pignone M. Patient time requirements for screening colonoscopy. American Journal of Gastroenterology. 2007;102:2401–2410. doi: 10.1111/j.1572-0241.2007.01387.x. [DOI] [PubMed] [Google Scholar]
- Jones RM, Devers KJ, Kuzel AJ, Woolf SH. Patient-reported barriers to colorectal cancer screening: A mixed-methods analysis. American Journal of Preventive Medicine. 2010;38:508–516. doi: 10.1016/j.amepre.2010.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klabunde CN, Vernon SW, Nadel MR, Breen N, Seeff LC, Brown ML. Barriers to colorectal cancer screening: A comparison of reports from primary care physicians and average-risk adults. Medical Care. 2005;43:939–944. doi: 10.1097/01.mlr.0000173599.67470.ba. [DOI] [PubMed] [Google Scholar]
- Peipins LA, Soman A, Berkowitz Z, White MC. The lack of paid sick leave as a barrier to cancer screening and medical care-seeking: Results from the National Health Interview Survey. BMC Public Health. 2012;12:520. doi: 10.1186/1471-2458-12-520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pignone MP, Crutchfield TM, Brown PM, Hawley ST, Laping JL, Lewis CL, et al. Using a discrete choice experiment to inform the design of programs to promote colon cancer screening for vulnerable populations in North Carolina. BMC Health Services Research. 2014;14:611. doi: 10.1186/s12913-014-0611-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabatino SA, Lawrence B, Elder R, Mercer SL, Wilson KM, DeVinney B, et al. Effectiveness of interventions to increase screening for breast, cervical and colorectal cancers: Nine updated systematic reviews for the Guide to Community Preventive Services. American Journal of Preventive Medicine. 2012;43:97–118. doi: 10.1016/j.amepre.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Sabatino SA, White MC, Thompson TD, Klabunde CN. Cancer screening test use—United States, 2013. MMWR. Morbidity and Mortality Weekly Report. 2015;64:464–468. [PMC free article] [PubMed] [Google Scholar]
- Subramanian S, Klosterman M, Amonkar MM, Hunt TL. Adherence with colorectal cancer screening guidelines: A review. Preventive Medicine. 2004;38:536–550. doi: 10.1016/j.ypmed.2003.12.011. [DOI] [PubMed] [Google Scholar]
- Subramanian S, Bobashev G, Morris RJ. Modeling the cost-effectiveness of colorectal cancer screening: Policy guidance based on patient preferences and compliance. Cancer Epidemiology, Biomarkers and Prevention. 2009;18:1971–1978. doi: 10.1158/1055-9965.EPI-09-0083. [DOI] [PubMed] [Google Scholar]
- Subramanian S, Bobashev G, Morris RJ. When budgets are tight there are better options than colonoscopies for colorectal cancer screening. Health Affairs. 2010;29:1734–1740. doi: 10.1377/hlthaff.2008.0898. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Screening for colorectal cancer: U.S. preventive services task force recommendation statement. Annals of Internal Medicine. 2008;149:627–637. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Final update summary: Colorectal cancer: Screening. Rockville, MD: USPSTF Program Office; 2015. [Accessed December 1, 2015]. from http://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/colorectal-cancer-screening. [Google Scholar]
- Yabroff KR, Borowski L, Lipscomb J. Economic studies in colorectal cancer: Challenges in measuring and comparing costs. Journal of the National Cancer Institute. Monographs. 2013;2013:62–78. doi: 10.1093/jncimonographs/lgt001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zauber AG, Lansdorp-Vogelaar I, Knudsen AB, Wilschut J, van Ballegooijen M, Kuntz KM. Evaluating test strategies for colorectal cancer screening: A decision analysis for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2008;149:659–669. doi: 10.7326/0003-4819-149-9-200811040-00244. [DOI] [PMC free article] [PubMed] [Google Scholar]