Abstract
Purpose
The aim of this study is to determine the predictable factors that affect the clinical course, especially the hospital stay, the operation performed, and to determine factors that will be helpful in deciding whether in-hospital or outpatient treatment is appropriate.
Methods
We retrospectively collected medical data for patients who had been diagnosed with acute diverticulitis at Inje University Sanggye Paik Hospital between January and December 2016. In total, 117 patients were enrolled in this study. We examined clinical factors, including age, sex, body mass index, pain, body temperature, white blood cell count, C-reactive protein, nil per os (NPO) time, hospital duration, computed tomography (CT) findings, location of diverticulitis, operation performed, and presence of comorbidity (e.g., hypertension and diabetes mellitus).
Results
In the multivariate analysis, the statistically significant factor related with hospital duration was the presence of perforation on the CT scan (P < 0.001). Longer NPO time was related with pain score (>7) (P = 0.011). Operations were mainly performed in patients with left-sided colonic diverticulitis (P = 0.012).
Conclusion
We suggest a perforation finding on the CT scan, a severe pain score at least above 7 on a numeric rating pain scale, and a left-sided lesion are absolute indications for in-hospital management.
Keywords: Diverticulitis, Predictive factors
INTRODUCTION
Diverticulitis is one of the major causes of an acute abdomen in emergency departments [1]. Its incidence has increased over the past decades. According to a large-scale study in the United States between 1998 and 2005, the admission rate for diverticulitis increased to 26%, and elective operations for diverticulitis increased over 29% [2,3]. In Western countries, diverticulosis and diverticulitis mostly occur in the left side of the colon, especially in the sigmoid colon where the intraluminal pressure is higher than it is in other segments of the colon [4]. However, in Eastern countries, especially in Korea, diverticulitis occurs predominantly in the right side of the colon around the cecum [5].
Most people with diverticulosis remain asymptomatic, but 25% will develop an episode of symptomatic diverticular disease. Among the symptomatic diverticulitis patients, about 14.4% to 17.4% require elective surgery [3]. When patients visit the Emergency Department (ED), the priority of diverticulitis treatment has usually been based on the severity of the disease, the clinical history of abdominal pain, physical examination and laboratory findings, and abdominopelvic computed tomography (CT) findings [6]. Classically, acute diverticulitis is essentially a surgical disease that requires multistep decision-making in terms of the timing and the type of operation. Sometimes, doctors face severe septic diverticulitis with a perforation that requires surgical intervention to resolve sepsis and/or to repair or resect a perforated bowel. We, the authors, tried to determine the predictive factors affecting hospital duration and elective surgical intervention in patients with acute diverticulitis and then tried to determine the patient group most in need of in-hospital management.
METHODS
We retrospectively collected medical data on patients who had been diagnosed with acute diverticulitis at Inje University Sanggye Paik Hospital between January and December 2016. Data from a total of 125 diverticulitis cases, including 2 cases of recurrence, involving 123 patients were collected during the study period. This study was approved by the Institutional Review Board of Inje University, Sanggye Paik Hospital. And written informed consent was not needed due to the study being retrospective. Eleven surgery cases were identified. Among them, we excluded 8 emergent surgery cases that had clinical signs of pan-peritonitis initially but then underwent surgery first. Operations were not performed in the 2 cases of recurrence. Therefore, a total of 117 cases involving 115 patients were enrolled in this study. The following clinical factors were documented: age, sex, body mass index (BMI), score on the numeric rating scale (NRS) as the pain scale, body temperature, white blood cell (WBC) count, C-reactive protein (CRP), nil per os (NPO) time, hospital duration, CT findings, location of diverticulitis, operation performed, and presence of comorbidity (e.g., hypertension and diabetes mellitus). In this study, NPO time was defined as the time from ER admission to the first sips of water during the hospital stay. Perforated diverticulitis was defined in CT findings as the presence of any amount of extraluminal free air and abscess formation described by an abdominopelvic radiology specialist.
We analyzed relevant factors affecting the duration of the hospital stay and the operation performed among various clinical factors. First, we examined the age distribution and divided patients into 2 age groups: over 60 years of age and 60 years of age or under. We also divided each of the remaining variables into 2 groups based on similar cutoff values: BMI (23 kg/m2), pain scale (NRS 7), body temperature (37.8℃), WBC count (15,000/µL), CRP (10 mg/dL), NPO time (2 days), hospital duration (6 days), CT findings (perforation/no perforation), location of diverticulitis (right-/left-sided colonic diverticulitis), operation performed (performed/not performed), and comorbidity (present/absent).
The data were analyzed with standard statistical software (Med-Calc ver. 15.11.1, MedCalc, Ostend, Belgium). The chi-square test was used to analyze the discrete variables, and the logistic regression test was used for the multivariate analysis with the stepwise variable selection method. The results were considered statistically significant at a significance level of 5%.
RESULTS
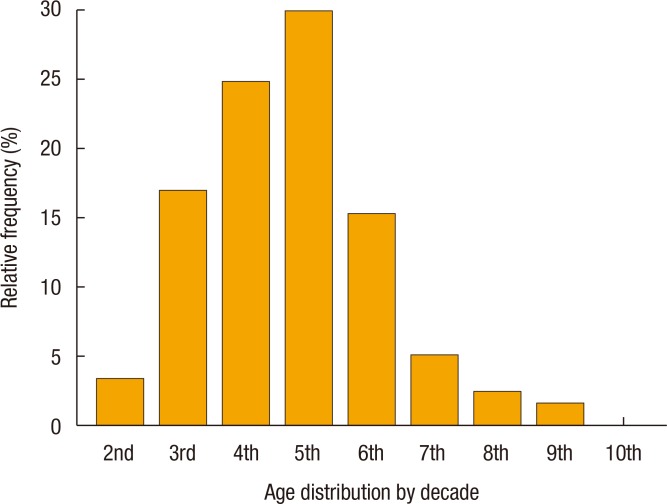
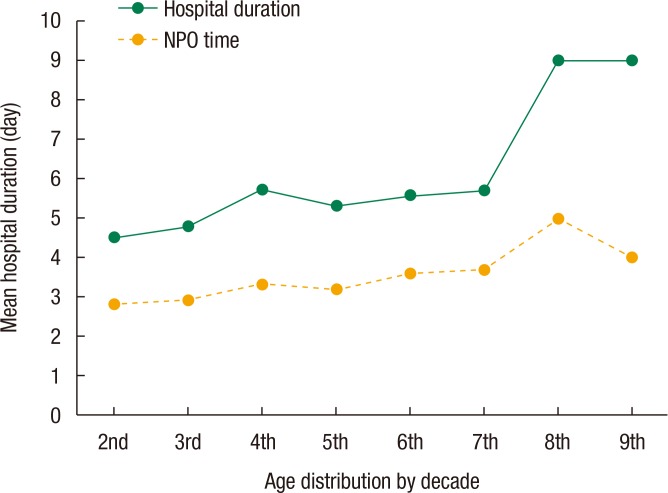
The sex breakout was 62 female (53%) and 55 male patients (47%). The median age was 42.0 years old (95% confidence interval [CI], 39.0–46.0), and the peak incidence of age was the fifth decade, followed by the fourth and the third decades (Fig. 1). The mean hospital stay and the mean NPO time were 5.5 and 3.29 days, respectively. The mean hospital stay and the mean NPO time showed an increasing tendency with increasing age distribution (Fig. 2, Table 1). The median NRS pain score was 6 (95% CI, 5–7), the median body temperature was 37.5℃ (95% CI, 37.2–37.6), and the median BMI was 23.6 kg/m2 (95% CI, 22.5–24.2) (Table 2). One hundred seven cases presented with right-sided colonic diverticulitis, and 10 cases with left. Operations were performed in 3 cases (2.5%): 2 on the left and 1 on the right side of the colon (Tables 3,4,5).
Fig. 1. Age distribution of patients with acute diverticulitis.
Fig. 2. Mean hospital duration and nil per os (NPO) time according to age distribution for patients with acute diverticulitis.
Table 1. Clinical characteristics according to age distribution by decade of acute diverticulitis patients.
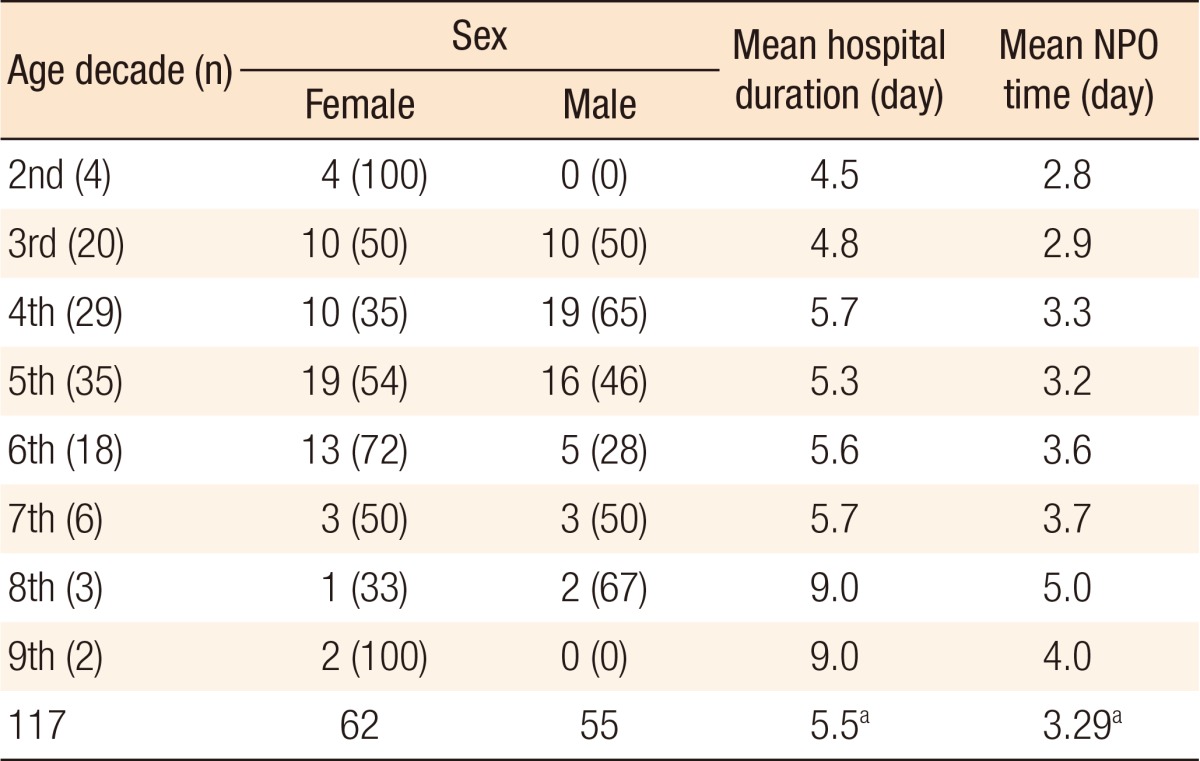
Values are presented as number (%).
NPO, nil per os.
aMean values of total enrolled cases.
Table 2. Clinical characteristics of patients with acute diverticulitis patients in the last year.
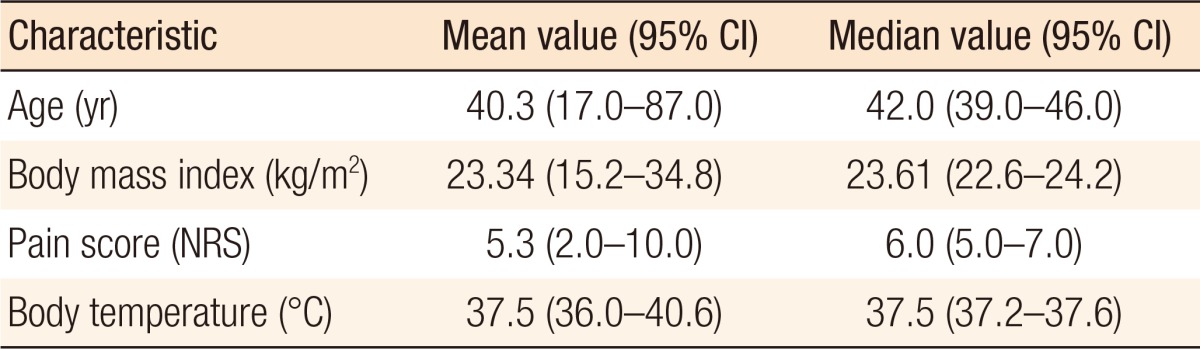
CI, confidence interval; NRS, numeric rating scale.
Table 3. Comparative univariate analysis between the 2 hospital duration groups of patients with acute diverticulitis.
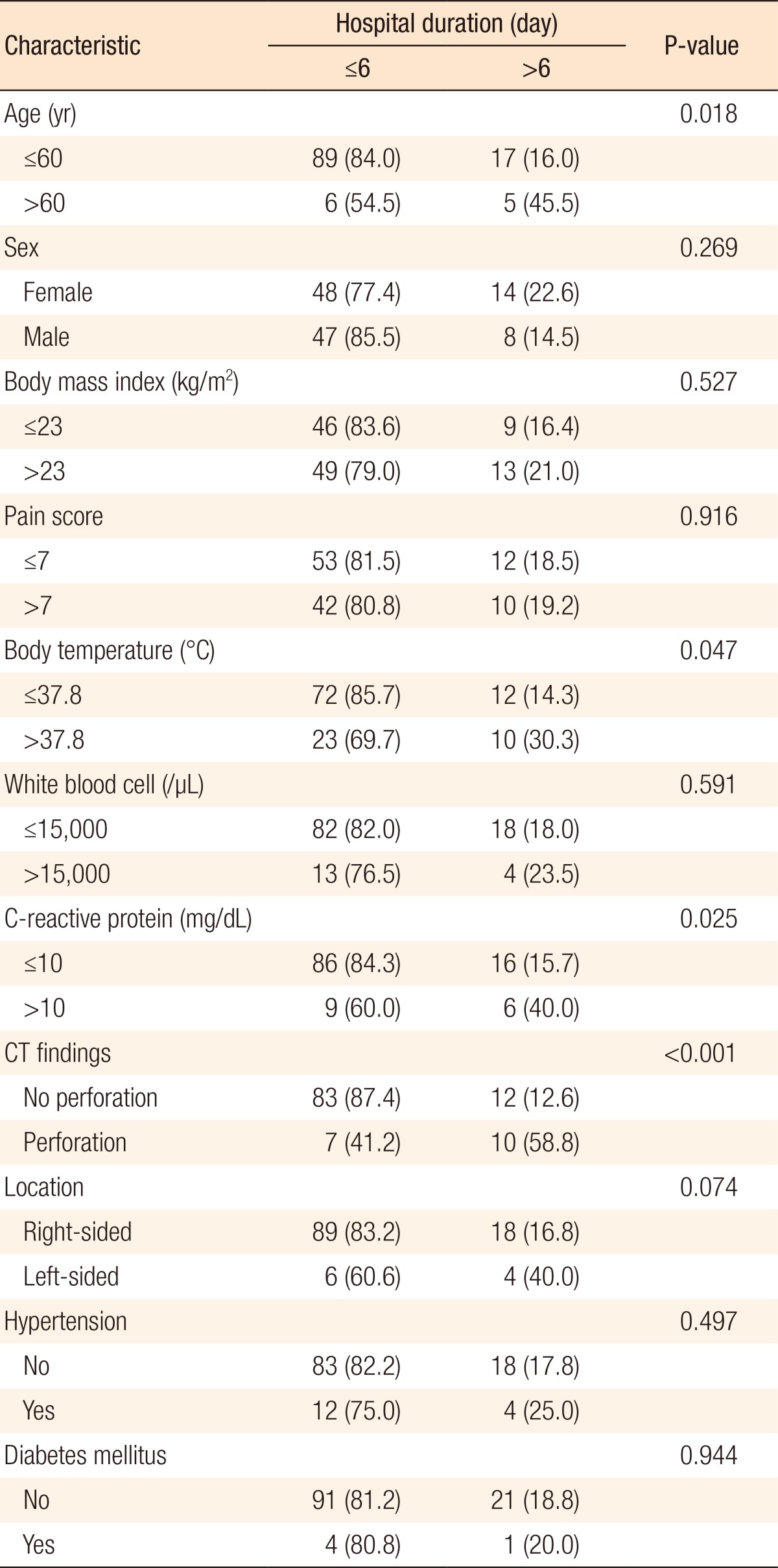
Values are presented as number (%). Percentage (%) represents % of row total in chi-square test.
CT, computed tomography.
Table 4. Comparative univariate analysis between the 2 NPO period groups.
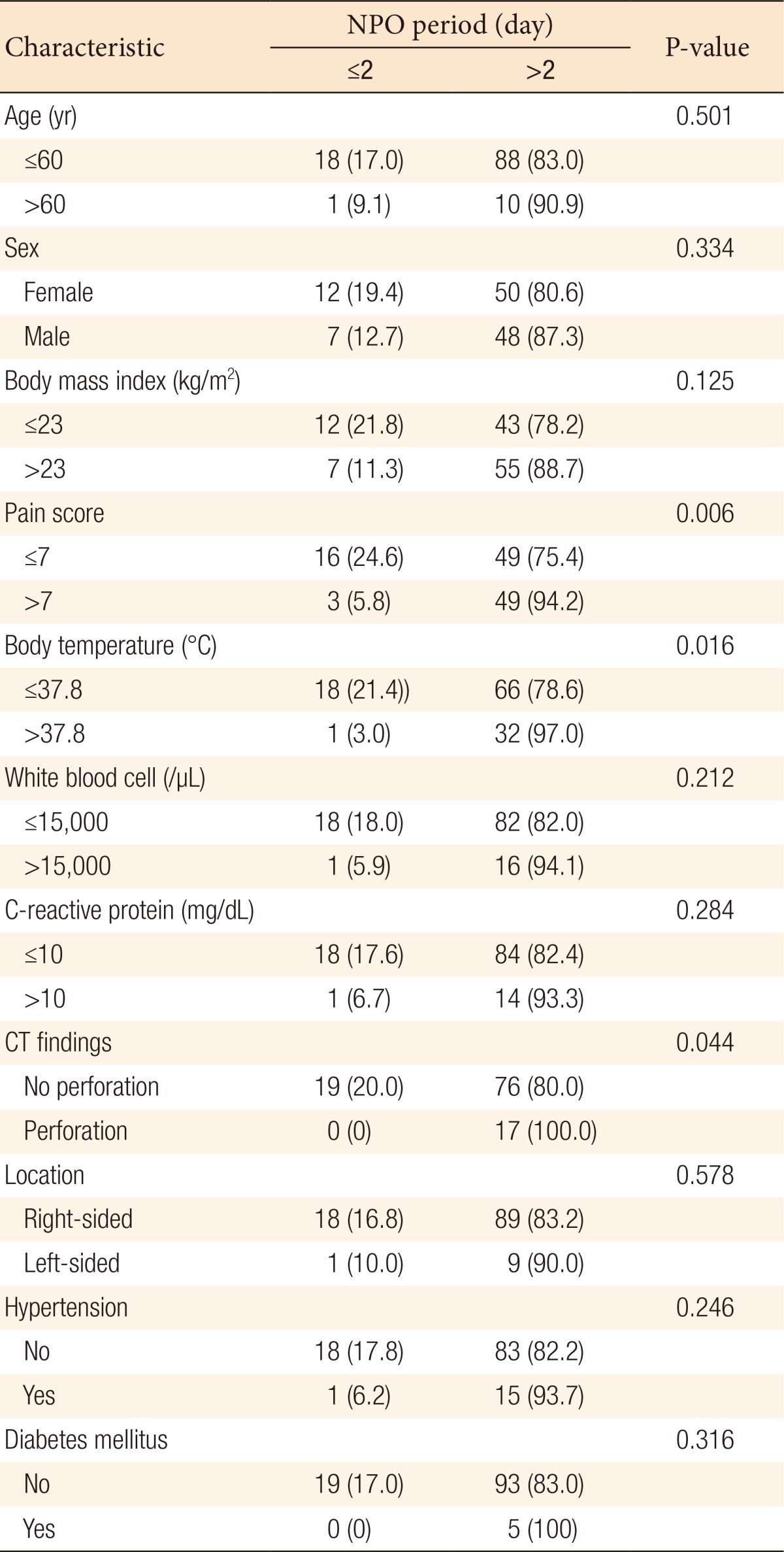
Values are presented as number (%). Percentage (%) represent % of row total in chi-square test.
NPO, nil per os.
Table 5. Comparative univariate analysis between the surgery and the nonsurgery groups.
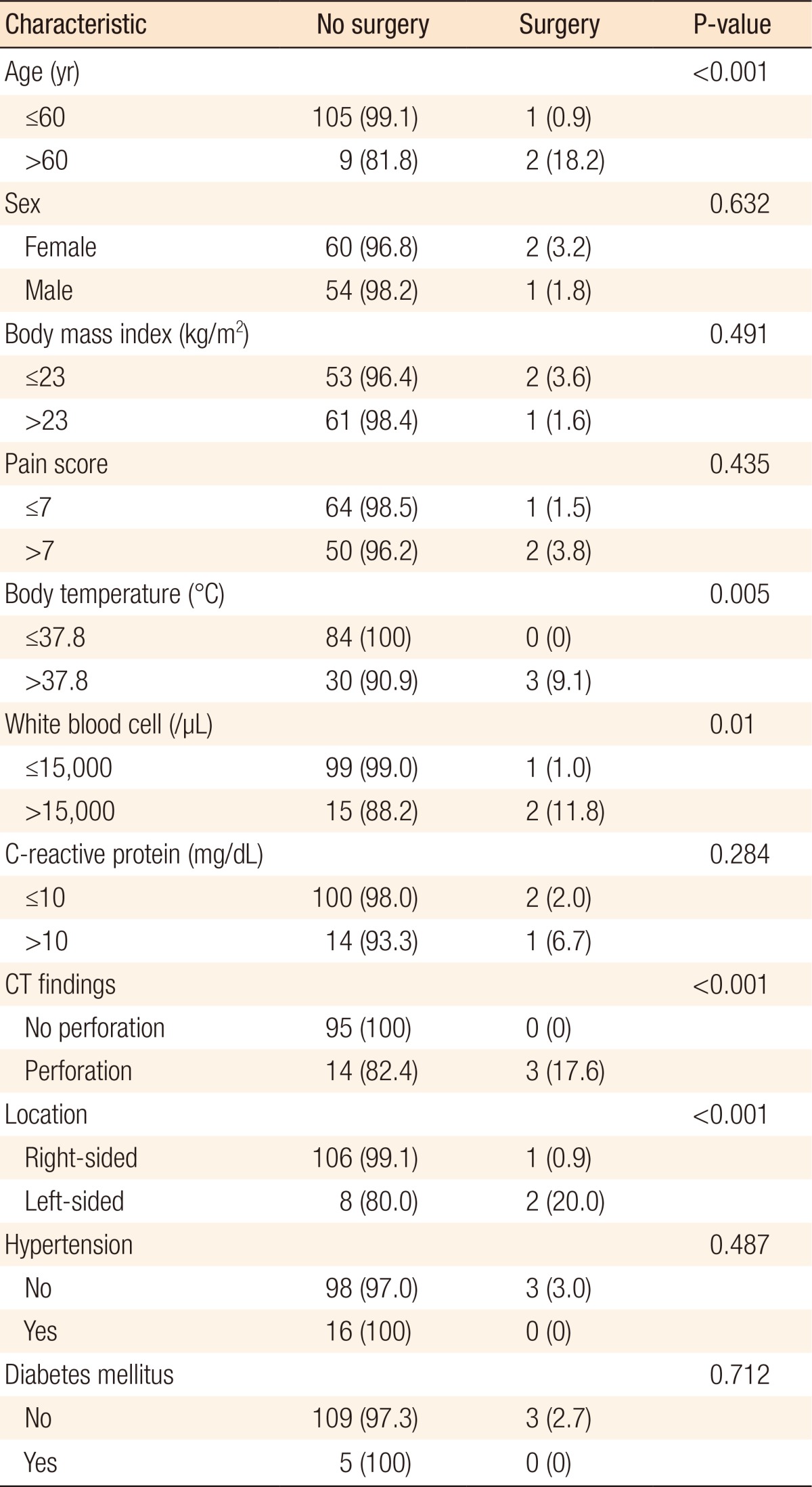
Values are presented as number (%). Percentage (%) represent % of row total in chi-square test.
In the univariate analysis, hospital stay was longer in the groups with older age (>60 years old) (P = 0.018), higher body temperature (>37.8℃) (P = 0.047), higher CRP (>10 mg/dL) (P = 0.025), perforation on the CT scan (P < 0.001), and left-sided colonic diverticulitis (P = 0.074) (Table 3). NPO time was longer in the groups with higher NRS score (>7) (P = 0.006), higher body temperature (>37.8℃) (P = 0.016), and perforation on the CT scan (P = 0.044) (Table 4). Operations were frequently performed in the groups with older age (>60 years old) (P < 0.001), higher body temperature (>37.8℃) (P = 0.005), higher WBC count (>15,000/µL) (P = 0.010), presence of perforation on the CT scan (P < 0.0001), and left-sided colonic diverticulitis (P < 0.001) (Table 5).
In the multivariate analysis, hospital stay was related with statistical significance to a perforation on the CT scan (P < 0.001) (Table 6). Longer NPO time was related with higher NRS score (>7) (P = 0.011) (Table 7). Operations were mainly performed on patients with left-sided colonic diverticulitis (P = 0.012) (Table 8).
Table 6. Clinical factors related with hospital duration longer than 6 days in patients with acute diverticulitis.
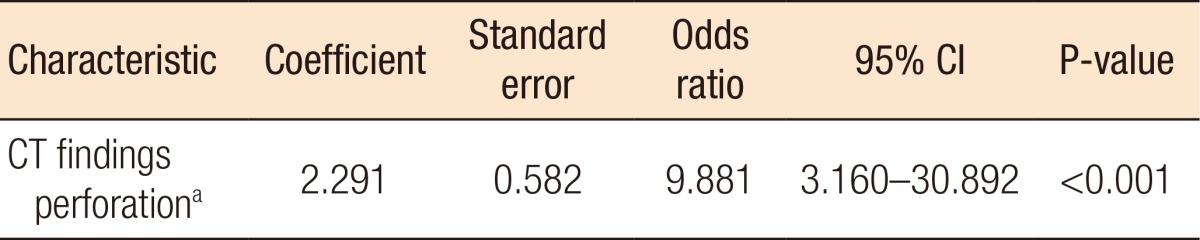
CI, confidence interval; CT, computed tomography.
aOther meaningful variables, age, fever, and C-reactive protein, in the univariate model were not selected for the multivariate logistic regression model.
Table 7. Clinical factors related with NPO time longer than 2 days in patients with acute diverticulitis.
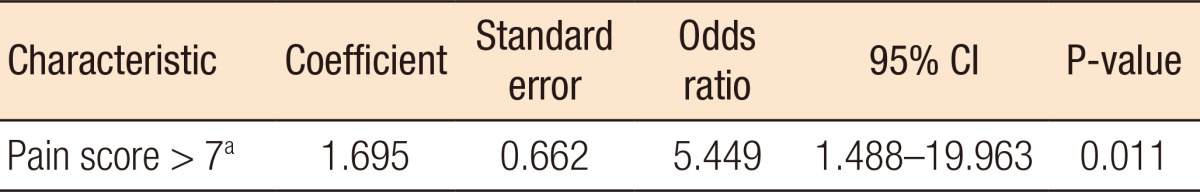
NPO, nil per os; CI, confidence interval.
aOther meaningful variables, fever and perforation on computed tomography finding, in the univariate model were not selected for the multivariate logistic regression model.
Table 8. Clinical factors related with surgery in patients with acute diverticulitis.
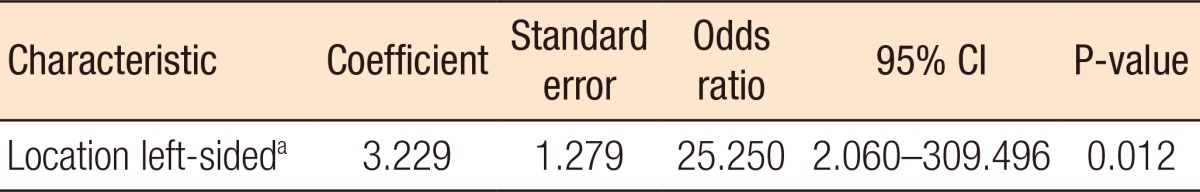
CI, confidence interval.
aOther meaningful variables, age, fever, white blood cell, and perforation on computed tomography finding, in the univariate model were not selected for the multivariate logistic regression model.
DISCUSSION
Many researchers have explored the factors related to the various clinical courses of patients with acute diverticulitis. Investigators have suggested clinical factors such as age, high body temperature, time from symptom onset to diagnosis, location of the lesion, and comorbidity could affect the clinical course of such patients [5,7,8,9,10]. In our study, we observed that 3 factors were statistically meaningful in the clinical course of patients with acute diverticulitis: perforation findings on the CT scan, severe tenderness on physical examination, and left-sided lesions. These 3 factors were found to be related to a longer hospital stay for those patients.
Perforated diverticulitis has a higher possibility to become complicated diverticulitis, and complicated diverticulitis accompanied by peritonitis with perforation, intra-abdominal abscess, and fistula formation is well known to require longer hospitalization [11,12,13]. Our study showed a result similar to that of previous studies: that is, a perforation finding on the CT scan was a statistically significant factor associated with a hospital stay of longer than 6 days.
Bowel rest is also required for patients with severe symptomatic diverticulitis [11,12,13]. For such patients, the recommendation is that they stay in an NPO state until symptoms and clinical signs improve. During this NPO state, patients cannot be placed in the outpatient unit because they cannot be supported by parenteral nutrition. If we could separate those patients that do not require NPO from the patients with acute diverticulitis, we would follow the former as outpatients, thus saving hospital resources and reducing public medical costs. In our study, we observed that patients who had severe pain scores, at least above NRS 7, were kept in an NPO state for more than 2 days as bowel rest.
Many studies have shown that the operation rates for acute diverticulitis in Western and Eastern countries are different. A 5%–10% elective operation rate has been reported in Eastern countries whereas a 15% rate has been reported in Western countries [3,7,11,14]. Researchers have explained this difference between Western and Eastern countries as being due to various reasons, such as disease pathophysiology, age distribution of incidence, location of the disease, ethnicity, and dietary habits. The characteristics of diverticulitis in Western countries are dominance in the left-sided colon and peak incidence at old age [7,10,15]. In our study, we observed that the majority of the patients were less than 60 years old and that the disease occurred dominantly in the right-sided colon. Left-sided colonic diverticulitis frequently requires surgery because of the higher possibility of complications [10,16]. Although only 3 operations were included in our study, left-sided colonic diverticulitis was a statistically significant factor predicting the performance of an operation, which is similar to the results of other previous studies. Moreover, in this study, age, higher body temperature, and higher CRP level were meaningful factors in the univariate analysis. We observed the tendency to have a longer hospital stay in older patients; furthermore, higher body temperature was related to hospital stay, NPO time, and necessity for an operation. However, these factors were not prognostic factors in the multivariate analysis [17].
Recently, many studies have introduced outpatient management for patients with noncomplicated diverticulitis in order to minimize the hospital stay [18,19,20]. Thus, establishing guidelines for distinguishing between patients requiring hospitalization and those that can be treated on an outpatient basis is important for treatment planning. Our study can support more details for identifying patients in our community with diverticulitis who would require a longer hospital stay.
Our study had some limitations. First, all data were collected retrospectively, so some clinical variables, such as scores on the NRS pain scale, signs of peritonitis, and associated gastrointestinal symptoms at the initial evaluation, were not documented on medical records well enough to minimize the clinical bias between cases. Second, the incidence of surgery was very low in this study, so we were unable to clarify the risk factors related to surgery in the patients with acute diverticulitis. In the future, prospective large-scale studies should be conducted to support our results.
In conclusion, we suggest that a perforation finding on the CT scan, a severe NRS pain score of at least above 7, or a left-sided lesion are absolute indications for in-hospital management. Furthermore, age, higher body temperature and CRP level should be considered as relative risk factors when a physician decides whether a patient should be hospitalized or not. When a physician initially encounters a diverticulitis patient in the emergency room or an outpatient facility, he/she should consider admitting that patient because of the expectation that a long hospital stay will be required. Based on our results, we are planning to verify the outpatient management criteria for patients with acute colonic diverticulitis by using a simple scoring system and to conduct a study on the safety and efficacy of outpatient management for patients with acute diverticulitis.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Lopez DE, Brown CV. Diverticulitis: the most common colon emergency for the acute care surgeon. Scand J Surg. 2010;99:86–89. doi: 10.1177/145749691009900208. [DOI] [PubMed] [Google Scholar]
- 2.Jamal Talabani A, Lydersen S, Endreseth BH, Edna TH. Major increase in admission- and incidence rates of acute colonic diverticulitis. Int J Colorectal Dis. 2014;29:937–945. doi: 10.1007/s00384-014-1888-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Etzioni DA, Mack TM, Beart RW, Jr, Kaiser AM. Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210–217. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 4.Andersen JC, Bundgaard L, Elbrønd H, Laurberg S, Walker LR, Støvring J; Danish national guidelines for treatment of diverticular disease. Dan Med J. 2012;59:C4453. [PubMed] [Google Scholar]
- 5.Kim SY, Oh TH, Seo JY, Jeon TJ, Seo DD, Shin WC, et al. The clinical factors for predicting severe diverticulitis in Korea: a comparison with Western countries. Gut Liver. 2012;6:78–85. doi: 10.5009/gnl.2012.6.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bugiantella W, Rondelli F, Longaroni M, Mariani E, Sanguinetti A, Avenia N. Left colon acute diverticulitis: an update on diagnosis, treatment and prevention. Int J Surg. 2015;13:157–164. doi: 10.1016/j.ijsu.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 7.Manabe N, Haruma K, Nakajima A, Yamada M, Maruyama Y, Gushimiyagi M, et al. Characteristics of colonic diverticulitis and factors associated with complications: A japanese multicenter, retrospective, cross-sectional study. Dis Colon Rectum. 2015;58:1174–1181. doi: 10.1097/DCR.0000000000000488. [DOI] [PubMed] [Google Scholar]
- 8.Reisman Y, Ziv Y, Kravrovitc D, Negri M, Wolloch Y, Halevy A. Diverticulitis: the effect of age and location on the course of disease. Int J Colorectal Dis. 1999;14:250–254. doi: 10.1007/s003840050219. [DOI] [PubMed] [Google Scholar]
- 9.Kim JH, Cheon JH, Park S, Kim BC, Lee SK, Kim TI, et al. Relationship between disease location and age, obesity, and complications in Korean patients with acute diverticulitis: a comparison of clinical patterns with those of Western populations. Hepatogastroenterology. 2008;55:983–986. [PubMed] [Google Scholar]
- 10.Chung BH, Ha GW, Lee MR, Kim JH. Management of colonic diverticulitis tailored to location and severity: comparison of the right and the left colon. Ann Coloproctol. 2016;32:228–233. doi: 10.3393/ac.2016.32.6.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Titos-García A, Aranda-Narváez JM, Romacho-López L, González-Sánchez AJ, Cabrera-Serna I, Santoyo-Santoyo J. Nonoperative management of perforated acute diverticulitis with extraluminal air: results and risk factors of failure. Int J Colorectal Dis. 2017;32:1503–1507. doi: 10.1007/s00384-017-2852-2. [DOI] [PubMed] [Google Scholar]
- 12.Sallinen VJ, Mentula PJ, Leppäniemi AK. Nonoperative management of perforated diverticulitis with extraluminal air is safe and effective in selected patients. Dis Colon Rectum. 2014;57:875–881. doi: 10.1097/DCR.0000000000000083. [DOI] [PubMed] [Google Scholar]
- 13.Kim BC. Nonoperative management of acute complicated diverticulitis. Ann Coloproctol. 2014;30:206. doi: 10.3393/ac.2014.30.5.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Song ME, Jung SA, Shim KN, Song EM, Kwon KJ, Kim HI, et al. Clinical characteristics and treatment outcome of colonic diverticulitis in young patients. Korean J Gastroenterol. 2013;61:75–81. doi: 10.4166/kjg.2013.61.2.75. [DOI] [PubMed] [Google Scholar]
- 15.Oh HK, Han EC, Ha HK, Choe EK, Moon SH, Ryoo SB, et al. Surgical management of colonic diverticular disease: discrepancy between right- and left-sided diseases. World J Gastroenterol. 2014;20:10115–10120. doi: 10.3748/wjg.v20.i29.10115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim SH, Byun CG, Cha JW, Choi SH, Kho YT, Seo DY. Comparative study of the clinical features and treatment for right and left colonic diverticulitis. J Korean Soc Coloproctol. 2010;26:407–412. doi: 10.3393/jksc.2010.26.6.407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mäkelä JT, Klintrup K, Rautio T. The role of low CRP values in the prediction of the development of acute diverticulitis. Int J Colorectal Dis. 2016;31:23–27. doi: 10.1007/s00384-015-2410-8. [DOI] [PubMed] [Google Scholar]
- 18.Moya P, Bellon M, Arroyo A, Galindo I, Candela F, Lacueva J, et al. Outpatient treatment in uncomplicated acute diverticulitis: 5-year experience. Turk J Gastroenterol. 2016;27:330–335. doi: 10.5152/tjg.2016.15284. [DOI] [PubMed] [Google Scholar]
- 19.Sánchez-Velázquez P, Grande L, Pera M. Outpatient treatment of uncomplicated diverticulitis: a systematic review. Eur J Gastroenterol Hepatol. 2016;28:622–627. doi: 10.1097/MEG.0000000000000610. [DOI] [PubMed] [Google Scholar]
- 20.Jackson JD, Hammond T. Systematic review: outpatient management of acute uncomplicated diverticulitis. Int J Colorectal Dis. 2014;29:775–781. doi: 10.1007/s00384-014-1900-4. [DOI] [PubMed] [Google Scholar]