Abstract
Purpose:
Policy reforms in the Affordable Care Act encourage health care integration to improve quality and lower costs. We examined the association between system-level integration and longitudinal costs of cancer care.
Methods:
We used linked SEER-Medicare data to identify patients age 66 to 99 years diagnosed with prostate, bladder, esophageal, pancreatic, lung, liver, kidney, colorectal, breast, or ovarian cancer from 2007 to 2012. We attributed each patient to one or more phases of care (ie, initial, continuing, and end of life) according to time from diagnosis until death or end of study interval. For each phase, we aggregated all claims with the primary cancer diagnosis and identified patients treated in an integrated delivery network (IDN), as defined by the Becker Hospital Review list of the top 100 most integrated health delivery systems. We then determined if care provided in an IDN was associated with decreased payments across cancers and for each individual cancer by phase and across phases.
Results:
We identified 428,300 patients diagnosed with one of 10 common cancers. Overall, there were no differences in phase-based payments between IDNs and non-IDNs. Average adjusted annual payments by phase for IDN versus non-IDNs were as follows: initial, $14,194 versus $14,421, respectively (P = .672); continuing, $2,051 versus $2,099 (P = .566); and end of life, $16,257 versus $16,232 (P = .948). However, in select cancers, we observed lower payments in IDNs. For bladder cancer, payments at the end of life were lower for IDNs ($11,041 v $12,331; P = .008). Of the four cancers with the lowest 5-year survival rates (ie, pancreatic, lung, esophageal, and liver), average expenditures during the initial and continuing-care phases were lower for patients with liver cancer treated in IDNs.
Conclusion:
For patients with one of 10 common malignancies, treatment in an IDN generally is not associated with lower costs during any phase of cancer care.
INTRODUCTION
Health care reforms in the Affordable Care Act aim to promote greater integration of local health care delivery systems. Broadly speaking, system-level integration includes the integration and coordination of acute care, ambulatory care, extended care, and community health services. In addition, care providers in an integrated system often work together with shared incentives and infrastructure, such as common electronic medical records.1 Proponents for greater system-level integration argue that much of the duplicative and low-value care identified to date stems from the disjointed nature of our current health care: communication between providers often is lacking, care coordination is ineffective, and care providers are not aligned with a common goal. The aims of an integrated delivery system, therefore, are to provide high-quality, evidence-based care with greater coordination and less duplication across the health care continuum.
Proponents of system-level integration highlight existing data that fully integrated delivery systems perform better from the perspective of both cost and quality, at least for ambulatory and preventive care.2,3 It is unclear, however, whether such systems achieve similar cost efficiencies for patients who require complex, multidisciplinary specialty care, such as that required by patients with cancer. Cancer is a prime condition to evaluate the effects of integrated health care delivery for patients with complex medical conditions, because care often is fragmented with the provision of extraneous services.4 In addition, cancer care is complex, and needs differ across the cancer continuum. Patients often require care that spans several disciplines (eg, medicine, social-work, psychological) and involves multiple providers in a variety of care settings (ie, hospital, home, and outpatient settings). The acuity of treatment also varies according to cancer characteristics, time from diagnosis, and time until death.
Through its focus on increased care coordination, easier information sharing, and provision of an entire spectrum of services, integration has the potential to improve health care quality and decrease costs for complex cancer care.5,6 For example, a patient who receives a cancer diagnosis in an optimally integrated delivery system may obtain treatment in the same system without repetitive diagnostic testing. Before, during, and after the initial treatment, the patient’s comorbidities and specific care needs will be well known to the providers and addressed appropriately. If a hospitalization occurs, the discharge plan will be carefully coordinated, and follow-up will be arranged before discharge.7 Furthermore, if problems develop, the system will have better care coordination to efficiently address a patient’s concerns. The care coordination and decreased utilization would continue throughout the continuing phase and could play a particularly important role at the end of life and for patients with aggressive cancers, in whom repeat diagnostics and in-patient hospitalizations could be decreased and end-of-life goals—such as the potential desire for hospice care—better addressed. Ultimately, if health care integration is successful, patients who receive care within these systems would have decreased readmissions, complications, and redundancies in care, which all would lead to cost savings. Conversely, system-level integration may not change specialist provider behavior or patient care, which would result in no cost savings.
In this context, we hypothesized that treatment in integrated delivery networks (IDNs) would be associated with lower costs for patients with cancer. With Medicare claims data, we examined this question by estimating the costs of cancer care during its continuum (ie, initial, continuing, and end-of-life phases) for patients treated in IDNs compared with those treated in nonintegrated health networks (ie, non-IDNs). We specifically examined differences in payments for patients at the end of life and for those who have cancer diagnoses that have low 5-year survival rates (ie, pancreatic, esophageal, lung, and liver).
METHODS
Data Sources
We used linked SEER-Medicare data from July 2007 through 2012. SEER-Medicare is a patient-level data set that links Medicare claims with information about clinical characteristics, patient demographics, and outcomes from the SEER registries. Claims from this data set are divided into five payment files: Medicare provider analysis and review (MEDPAR: readmissions, index, skilled nursing facility), carrier (professional), outpatient, home health, and hospice. We used all five files for our analyses.
Study Population
The study cohort included patients age 66 to 99 years who were diagnosed with one of 10 cancers (prostate, bladder, esophageal, pancreatic, lung, liver, kidney, colorectal, breast, or ovarian) between 2007 and 2012. We initially identified these patients in the SEER Patient Entitlement and Diagnosis Summary File (PEDSF) by using the International Classification of Diseases (ICD)–0-3 cancer site recode for the cancer of interest. We then confirmed the diagnosis by including only patients with the relevant ICD-0-3 histology codes for each cancer. We excluded patient cases in which the diagnosis was noted only by autopsy or on the death certificate. We also excluded patients without continuous Medicare Parts A and B enrollment from 12 months before diagnosis until end of study interval or death and patients who participated in a Medicare health maintenance organization.
For each patient, we determined patient demographic and cancer characteristics, including sex, age, marital status, ethnicity, year of diagnosis, and cancer stage, with the SEER PEDSF file. Age was defined as the diagnosis date minus the birth date and was a categoric variable. We limited ethnicity to white, black, and other. According to the health system to which the patient was attributed, we used the American Hospital Association Annual Survey data to determine the number of hospital beds, teaching status, hospital ownership, and geographic region, which was categorized as one the following locations: Northeast, Midwest, South, and West.
Attribution of Patients to Phases of Care
In this analysis, we identified three phases of care: initial, continuing, and end-of-life, as described previously.8 Individual patients were attributed to one or more phases of care according to the length of survival from cancer diagnosis to death or the end of the study period. To attribute patients, we used the SEER PEDSF file to determine days of survival by subtracting the diagnosis date from the date of death. Patients who survived fewer than 12 months after diagnosis were attributed only to the end-of-life phase. Those who survived more than 12 months but fewer than 24 months were attributed to the initial and end-of-life phases, and the remainder were attributed to the initial, end-of-life, and continuing care phases. The 12 months during the end-of-life phase were given precedence; then, the 12 months for the initial phase; last, the continuing phase. Each patient could be attributed to the end-of-life phase, the initial and end-of-life phases, or all three phases according to the number of days of survival after diagnosis. Patients who survived throughout the study interval were attributed to the initial and continuing phases of care. Each patient-phase dyad was evaluated distinctly from the other phases with the exception of the overall estimates, in which only patients present in all three phases were included in analyses.
Identification of Patients Treated in Integrated Delivery Systems
To identify patients treated in highly integrated delivery systems, we undertook a two-step process. First, we attributed patients to a health system. Second, we identified the highly integrated health care systems.
To attribute each patient to a health care system, we attributed each patient to a physician and then to a health system for each phase of cancer care. This attribution occurred in three main steps. First, each patient was assigned to the physician who had the plurality of cancer-related claims (ie, the number of claims, not total reimbursement) for each cancer phase. For this step, we limited physician codes for ICD-9 Health Care Financing Administration provider specialty and for Berenson-Eggers type of service to those claims that involved direct patient care. Second, we attributed each physician to a health care system. To do this, we assigned each physician to the health system where the majority of his or her patients were admitted annually. Third, we attributed each patient to a health system for each cancer phase. We did this by calculating the dominant year, or the year with the greatest number of claims, by cancer phase. Each patient’s phase of cancer care then was attributed to the health system by using the dominant year of care and the physician attribution to the health system (ie, step 2).
Next, we measured health care integration by using the Becker Hospital Review list of the top 100 most integrated health delivery systems. The designation of a top-100 integrated delivery system was determined by Becker’s Hospital Review and was based on metrics reported by IMS Health, a health care analytics firm. Ratings measure 33 attributes of a health system in eight domains, which are overall integration, integrated technology, hospital utilization, access, available services, contract capabilities, financial stability, and services.9 We defined an integrated delivery system as a dichotomous variable if the health system was listed in Becker’s Hospital Review top 100 most integrated delivery systems. This rating methodology has been used previously to identify and measure health care integration.9-11
Calculation of Payments According to Phase of Care
For each patient–phase-of-care dyad, we aggregated all standard payments for claims with a primary diagnosis code for the corresponding cancer for each Medicare data file (MEDPAR, carrier claims, outpatient, home health, and hospice). We estimated the average payment per beneficiary in each data file and then per each beneficiary across all files. To account for differences in Medicare reimbursement that were based on geography, teaching status, and disproportionate share payments, we price-standardized all payments by using methods previously described by our research team.12 These methods were adapted from the Dartmouth Institute for Health Policy and Clinical Practice and the Medicare Payment Advisory Commission.
Statistical Analyses
To determine whether payments for cancer care were lower in an IDN compared with a nonintegrated system, we fit phase-specific generalized estimating equation models with the gamma distribution and log link for each cancer type and across all 10 cancers. We fit this model to better account for costs that had a non-normal distribution and for analyses that occurred at the individual patient level, for which patients received care at different hospitals that were in different health systems. We first fit the models with only IDN as a covariable. Next, we fit similar phase-specific models for each of the 10 cancers but adjusted the analysis for patient (age, sex, number of Charlson comorbidities, marital status), hospital (geographic region, number of beds, urban/rural, hospital ownership, surgical volume), and cancer (stage, grade) characteristics. We paid particular attention to end-of-life spending and cancers with the lowest 5-year survival rates (ie, pancreatic, lung, esophageal, and liver cancers).13
All analyses were performed with SAS version 9.4 (SAS Institute, Cary, NC) and used the 5% significance level. The University of Michigan institutional review board deemed this study exempt from review.
RESULTS
We identified 428,300 patients who were diagnosed with one of 10 cancers from 2006 through 2011. Of these, 140,383 (33%) received care from an IDN.
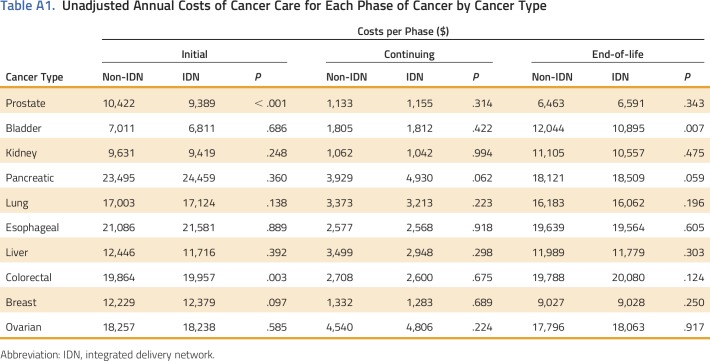
An unadjusted comparison of the costs of cancer care by cancer type and phase within an IDN compared with a non-IDN is listed in Appendix Table A1 (online only). In the initial phase, only prostate cancer was significantly lower in an IDN versus a non-IDN ($9,389 v $10,422; P < .001). There were no statistically significant differences in the continuing phase. At the end-of-life phase, bladder cancer care was lower in an IDN versus a non-IDN ($10,895 v $12,044; P = .007).
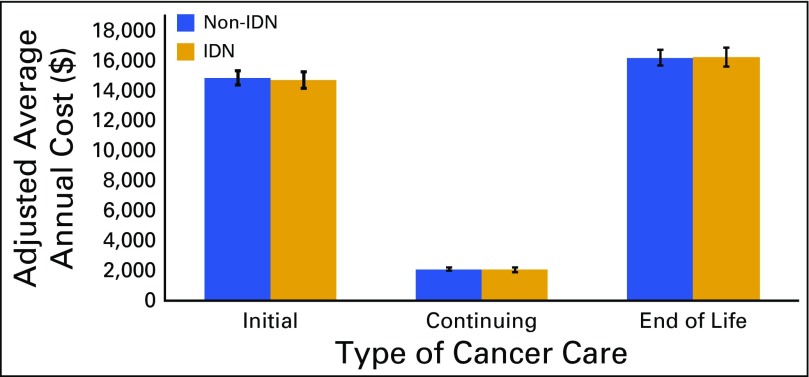
Overall, there were no significant phase-based differences in costs between highly integrated delivery systems and those that were nonintegrated. Average annual costs in the initial phase, continuing phase, and end-of-life phase for IDNs versus non-IDNs were as follows: initial, $14,194 versus $14,421 (P = .672); continuing, $2,051 versus $2,099 (P = .566); and end of life, $16,257 versus $16,232 (P = .948; Fig 1).
Fig 1.
Adjusted average annual costs of cancer care across 10 cancer types for integrated delivery network (IDN) versus non-IDN. Adjusted for patient (age, sex, number of Charlson comorbidities, marital status), hospital (geographic region, number of beds, urban/rural, hospital ownership, surgical volume), and cancer (stage, grade) characteristics.
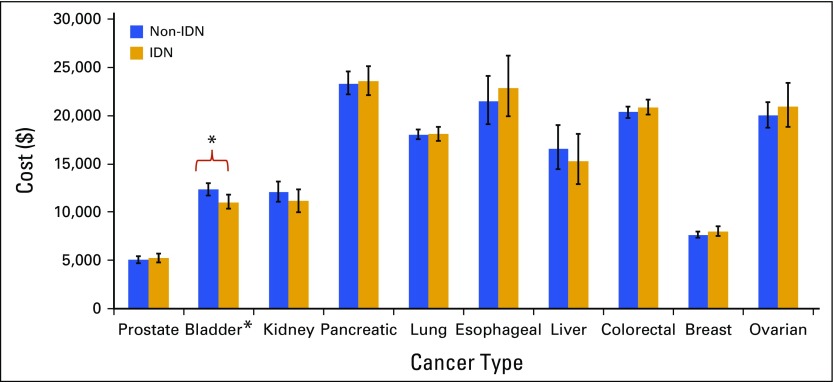
However, in a few select cancers and phases, we observed lower costs for those treated in an IDN. Figure 2 displays the end-of-life costs for integrated versus nonintegrated health delivery systems for each of the 10 cancers. Only bladder cancer realized cost savings when care was provided in an IDN at the end of life compared with a nonintegrated network ($11,041 v $12,331; P = .008).
Fig 2.
Adjusted average annual costs of cancer care for integrated delivery network (IDN) versus non-IDN hospitals at end-of-life. Adjusted for patient (age, sex, number of Charlson comorbidities, marital status), hospital (geographic region, number of beds, urban/rural, hospital ownership, surgical volume), and cancer (stage, grade) characteristics. *P < .05.
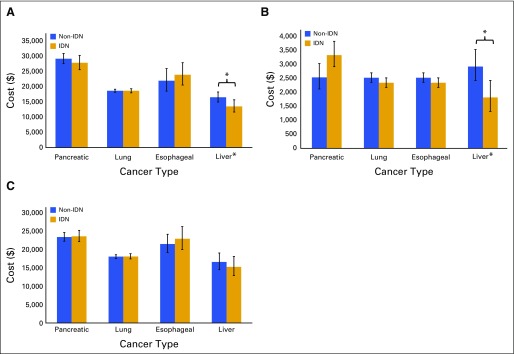
Of the four cancers with the lowest 5-year survival rates (pancreatic, lung, esophageal, and liver13), only patients with liver cancer in the initial and continuing phases had lower average annual expenditures when they received care in an integrated delivery system compared with a nonintegrated system (Fig 3). The cost differentials for liver cancer by phase were as follows: $2,985 (P = .016) for the initial phase, $1,107 (P = .002) for the continuing phase, and $1,301 at end of life (P = .472).
Fig 3.
Adjusted average annual costs of cancer for integrated delivery network (IDN) versus non-IDN hospitals in (A) initial, (B) continuing, and (C) end-of-life phases for cancers with the lowest 5- year survival. Adjusted for patient (age, sex, number of Charlson comorbidities, marital status), hospital (geographic region, number of beds, urban/rural, hospital ownership, surgical volume), and cancer (stage, grade) characteristics. *P < .05.
DISCUSSION
In this study, we examined payments for 10 cancer types according to health system integration. The findings demonstrated few payment differences between IDNs and non-IDNs. Namely, after analyses were adjusted for patient, hospital, and cancer characteristics, there were no differences in phase-based payments for cancer care across the 10 cancers combined, and there were few differences in phase-based payments for individual malignancies. Collectively, these findings suggest that cancer care in IDNs is not associated with lower total costs of care.
Previous investigators have demonstrated that IDNs provide higher-quality primary care and ambulatory services at lower costs.10,14,15 However, the argument for the IDN provision of cost savings for acute inpatient surgery is poor; a recent investigation of in-hospital care for coronary artery bypass graft, back surgery, hip replacement, and colectomy demonstrated similar outcomes and costs between IDN and non-IDNs, with the exception of decreased readmissions for colectomy and a 4% episode cost savings for patients who underwent hip replacement surgery.10 For prostate cancer, receipt of care in an IDN resulted in small decreases in rates of prostate cancer treatment but not in potential overtreatment.9 Our findings, to our knowledge, are novel in that we evaluated the impact of integrated care delivery systems on costs for treatment for a complex diagnosis (ie, cancer) during its entire care continuum (ie, from diagnosis to end of life). Although we found disparities in IDNs and non-IDNs for bladder cancer at the end of life and for liver cancer at the initial and continuing phases, it is unclear whether these are meaningful. Overall, payments for cancer care seem similar across different levels of delivery system integration.
A potential reason for the findings of no payment differences in IDNs is that we evaluated system-level integration. The benefits of system-level integration, including the potential for improved communication and shared electronic health records, may not be facile enough to respond to the manifold needs of patients who have complex medical conditions. Perhaps a more microlevel integration approach, such as service-line specific integration, will better align providers with improved communication, decreased redundancy, increased care coordination, and a common goal but remain nimble enough to provide patient-centered care. The Come Home project, a medical home for patients with cancer, is an example of a service-line approach to cancer care. Some participants in this model have demonstrated significant increases in telephone triaging; reductions in emergency department visits, hospital admissions, and outpatient visits; and high levels of patient satisfaction.16,17
Our study has several limitations. First, we estimated payments for cancer care only for the Medicare population. As a result, findings may not be generalizable to younger patients with cancer. Nonetheless, estimates from the Medicare program are policy relevant given the burden of cancer in this population, including an incidence rate that is 10 times higher, and a death rate from cancer that is 16 times greater, than for patients younger than age 65 years.18 Second, the definition of IDN varies, and we only applied one definition—from Becker’s Hospital Review—to our analyses. This definition of IDNs has been used in major medical journals and is readily quantifiable.3,9,11 In addition, all claims for patients attributed to an IDN may not have occurred within an IDN. However, this scenario is similar to other Medicare payment programs (accountable care organizations and value-based purchasing), in which patients and hospitals are held accountable for claims that occur outside of their facilities. Third, the initial and end-of-life phases were based on 12-month time periods. Because some patients may not have been in the respective phase for the entire 12 months (eg, the patient died 20 months after diagnosis), payments in these phases may be underestimated. Fourth, we only include claims with primary diagnosis codes of the diagnosed malignancy. This approach may underestimate the true costs of cancer care, but it ensures specificity for cancer-related expenditures and has been used in prior work.19 Last, we did not evaluate the composition of payments (eg, readmissions compared with physical therapy or psychological counseling) and the quality of care provided, which could demonstrate differences across IDNs and non-IDNS.
These limitations notwithstanding, the findings have important implications for hospital administrators, policymakers, and payers. For hospital administrators, the findings suggest that system-level integration does not decrease costs of care for all patients. For patients with complex conditions, service-line integration may be more successful. Similarly, from a policy and payer perspective, driving improvement into complex specialty-based care may require a focus on the microlevel (ie, service-line) integration rather than on the macrolevel (ie, system) integration. Unlike policy initiatives that focus on primary care providers and aim to drive system-level integration (eg, accountable care organizations), service-line integration may be better able to affect the decisions made by specialists and their interactions in the health care network. Two examples of service-line approaches recently introduced by the Centers for Medicare and Medicaid Innovation are bundled payments and the OCM. Bundled payments focus on an acute inpatient episode and post-discharge care. In contrast, the OCM provides a service-line approach to management of costs and quality for patients with cancer. For patients who receive chemotherapy, physician groups that participate in the OCM agree to provide increased care coordination with performance and financial liability for the potential of economic reward. Understanding the effects of the OCM payment model will provide significant insight into whether more microlevel integration has greater effects than what we observed for more macrolevel integration. Moving forward, research about quality and costs in the OCM payment model and oncology medical home will be necessary to determine whether more microlevel integrated care delivery systems are beneficial. In addition, evaluation of top-performing providers, regardless of their IDN affiliations, could provide insight into ways to improve oncology care. Last, it perhaps is worthwhile to evaluate different delivery system models, such as cancer-focused systems (ie, National Cancer Institute designation).
ACKNOWLEDGMENT
Supported by the National Cancer Institute Grants No. 1-R01-CA-174768-01-A1 to D.C.M. and 5-T32-CA-180984-03 to D.R.K.
Appendix
Table A1.
Unadjusted Annual Costs of Cancer Care for Each Phase of Cancer by Cancer Type
AUTHOR CONTRIBUTIONS
Conception and design: Deborah R. Kaye, Jonathan Li, Chad Ellimoottil, David C. Miller, Lindsey A. Herrel
Collection and assembly of data: Deborah R. Kaye, Hye Sung Min, Zaojun Ye, David C. Miller, Lindsey A. Herrel
Data analysis and interpretation: Deborah R. Kaye, Hye Sung Min, Edward C. Norton, Zaojun Ye, James M. Dupree, Chad Ellimoottil, David C. Miller, Lindsey A. Herrel
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
System-Level Health-Care Integration and the Costs of Cancer Care Across the Disease Continuum
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Deborah R. Kaye
Travel, Accommodations, Expenses: Medreviews
Hye Sung Min
No relationship to disclose
Edward C. Norton
No relationship to disclose
Zaojun Ye
No relationship to disclose
Jonathan Li
No relationship to disclose
James M. Dupree
Stock or Other Ownership: Procter & Gamble, Lipocine
Grant Funding: Blue Cross Blue Shield of Michigan for the Michigan Value Collaborative
Chad Ellimoottil
Grant Funding: Blue Cross Blue Shield of Michigan for the Michigan Value Collaborative
David C. Miller
Grant Funding: Blue Cross Blue Shield of Michigan for the Michigan Value Collaborative
Lindsey A. Herrel
No relationship to disclose
REFERENCES
- 1. Zuckerman AM: Systemness: The next frontier for integrated health delivery. https://www.beckershospitalreview.com/hospital-management-administration/systemness-the-next-frontier-for-integrated-health-delivery.html. [Google Scholar]
- 2.Hollander P, Nicewander D, Couch C, et al. : Quality of care of Medicare patients with diabetes in a metropolitan fee-for-service primary care integrated delivery system. Am J Med Qual 20:344-352, 2005 [DOI] [PubMed] [Google Scholar]
- 3.Rittenhouse DR, Casalino LP, Shortell SM, et al. : Small and medium-size physician practices use few patient-centered medical home processes. Health Aff (Millwood) 30:1575-1584, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Skolarus TA, Zhang Y, Hollenbeck BK: Understanding fragmentation of prostate cancer survivorship care: Implications for cost and quality. Cancer 118:2837-2845, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bickell NA, LePar F, Wang JJ, et al. : Lost opportunities: Physicians’ reasons and disparities in breast cancer treatment. J Clin Oncol 25:2516-2521, 2007 [DOI] [PubMed] [Google Scholar]
- 6.Chubak J, Tuzzio L, Hsu C, et al. : Providing care for cancer survivors in integrated health care delivery systems: Practices, challenges, and research opportunities. J Oncol Pract 8:184-189, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Berwick DM, Nolan TW, Whittington J: The triple aim: Care, health, and cost. Health Aff (Millwood) 27:759-769, 2008 [DOI] [PubMed] [Google Scholar]
- 8.Mariotto AB, Yabroff KR, Shao Y, et al. : Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst 103:117-128, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hollenbeck BK, Bierlein MJ, Kaufman SR, et al. : Implications of evolving delivery system reforms for prostate cancer care. Am J Manag Care 22:569-575, 2016 [PMC free article] [PubMed] [Google Scholar]
- 10.Miller DC, Ye Z, Gust C, et al. : Anticipating the effects of accountable care organizations for inpatient surgery. JAMA Surg 148:549-554, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nyweide DJ, Weeks WB, Gottlieb DJ, et al. : Relationship of primary care physicians’ patient caseload with measurement of quality and cost performance. JAMA 302:2444-2450, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottlieb DJ, Zhou W, Song Y, et al. : Prices don’t drive regional Medicare spending variations. Health Aff (Millwood) 29:537-543, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. SEER: Age-adjusted SEER incidence and US death rates and 5-year relative survival (percent) by primary cancer site, sex, and time period, 2014. https://seer.cancer.gov/csr/1975_2014/results_merged/topic_survival.pdf. [Google Scholar]
- 14.Mehrotra A, Epstein A.M., Rosenthal MB: Do integrated medical groups provide higher-quality medical care than individual practice associations? Ann Intern Med 145:826-833, 2006 [DOI] [PubMed] [Google Scholar]
- 15.Weeks WB, Gottlieb DJ, Nyweide DE, et al. : Higher health care quality and bigger savings found at large multispecialty medical groups. Health Aff (Millwood) 29:991-997, 2010 [DOI] [PubMed] [Google Scholar]
- 16.Sprandio JD: Oncology patient-centered medical home. J Oncol Pract 8:47s-49s, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Waters TM, Webster JA, Stevens LA, et al. : Community oncology medical homes: Physician-driven change to improve patient care and reduce costs. J Oncol Pract 11:462-467, 2015 [DOI] [PubMed] [Google Scholar]
- 18. Berger NA, Savvides P, Koroukian SM, et al: Cancer in the elderly. Trans Am Clin Climatol Assoc 117:147-155, 2006; discussion 155-156. [PMC free article] [PubMed] [Google Scholar]
- 19.Skolarus TA, Zhang Y, Miller DC, et al. : The economic burden of prostate cancer survivorship care. J Urol 184:532-538, 2010 [DOI] [PubMed] [Google Scholar]