Abstract
Background
Alcohol use is associated with angina incidence but associations between alcohol use and experience of angina among patients with coronary artery disease (CAD) have not been described.
Methods
Outpatients with CAD from 7 clinics in the Veterans Health Administration were surveyed; alcohol use was measured using the validated AUDIT-C scores categorized into 6 groups: non-drinking, low-risk drinking, and mild, moderate, severe, and very severe unhealthy alcohol use. Three domains of self-reported angina symptoms (frequency, stability, and physical function) were measured with the Seattle Angina Questionnaire. Linear regression models evaluated associations between alcohol use groups and angina symptoms. Models were adjusted first for age and then additionally for smoking, comorbidities, and depression.
Results
Patients (n=8,303) had a mean age of 66. In age-adjusted analyses, a U-shaped association was observed between alcohol use groups and all angina outcomes, with patients in non-drinking and severe unhealthy alcohol groups reporting the greatest angina symptoms and lowest functioning. After full adjustment, no clinically important and few statistically important differences were observed across alcohol use in angina stability or frequency. Patients in the non-drinking group had statistically greater functional limitation from angina than those in all groups of unhealthy alcohol use, though differences were small. Patients in all groups of unhealthy alcohol use did not differ significantly from those with low-risk drinking.
Conclusions
Alcohol use was associated with some small statistically but no clinically important differences in angina symptoms among patients with CAD. This cross-sectional study does not support a protective effect of low-level drinking on self-reported angina.
INTRODUCTION
A number of previous studies have identified “U-shaped” associations between alcohol use and cardiovascular disease and related deaths (Gemes et al., 2016; Makita et al., 2012; Rehm et al., 2003; Smyth et al., 2015; Toma et al., 2017). Even after adjustment for multiple potentially confounding factors, studies have demonstrated lower prevalence of cardiovascular disease and/or risk of death among individuals who drink alcohol at low levels than among those who abstain and/or drink at high levels (Camargo et al., 1997b; Diamond, 1989; Fernandez-Sola et al., 1994; Gemes et al., 2016; Gunzerath et al., 2004; Klatsky, 1994; Klatsky et al., 1977; Klatsky et al., 1974; Koskinen and Kupari, 1991; Li and Mukamal, 2004; Maki et al., 1998; Puddey et al., 1999; Rich et al., 1985; Urbano-Marquez et al., 1995; Vliegenthart et al., 2002). While many clinical cardiovascular outcomes have been studied (e.g., prevalence of coronary artery disease, angina incidence, myocardial infarction), no study has assessed associations between alcohol use and patient-reported experience of angina.
Patient experience may capture aspects (e.g., severity) that are difficult to measure clinically but influence clinical outcomes (Mozaffarian et al., 2003). For instance, among patients with coronary artery disease (CAD), self-reported angina symptoms are associated with decreased quality of life (Spertus et al., 2002) and increased risk of death (Mozaffarian et al., 2003). Among general outpatients, any and unhealthy alcohol use are associated with quality of life and self-reported health status (Peytremann-Bridevaux et al., 2004; Williams et al., 2010). However, no study has evaluated the relationship between alcohol use and patient experience of angina among patients with coronary disease. Therefore, we evaluated the cross-sectional association between alcohol use and three domains of patient experience of angina that are known to be predictive of key clinical outcomes (Mozaffarian et al., 2003): frequency and stability of angina, as well as physical limitation associated with angina.
METHODS
Data Source and Study Population
Baseline data from the Ambulatory Care Quality Improvement Trial (ACQUIP) was used for this study. ACQUIP was a multi-site, group-randomized trial of primary care patients from the Veterans Health Administration (VA) between 1997 and 2000. The purpose of the trial was to determine whether health status and patient satisfaction could be improved by giving primary care providers access to systematic assessments of their patients’ health and functioning, in addition to information about clinical guidelines. The trial was completed April 1, 2000, and main analyses showed no effect of the intervention on any primary or secondary outcomes.(Fihn et al., 2004).
Recruitment for ACQUIP was done via surveys, which were mailed to VA patients from primary care clinics in 7 U.S. cities (Birmingham, Little Rock, Richmond, San Francisco, Seattle, West Los Angeles, and White River Junction). Responses to the initial mailed survey (“Health Checklist”) were considered consent to participate. Participants who reported specific conditions (e.g., CAD) on the Health Checklist were sent condition-specific questionnaires at baseline. Additional clinical and administrative data were obtained for all participants from VA’s electronic health record (EHR).
Among 62,487 patients invited to participate in ACQUIP, 36,821 (59%) returned the initial Health Checklist, and 12,505 were determined to have CAD based on a combination of self-reported history of a coronary event, angina, or a revascularization procedure. This combination of self-reported history has a sensitivity of 97% and a specificity of 93% when compared to chart review (Spertus et al., 2000). All patients with CAD were sent a Seattle Angina Questionnaire (SAQ), and 8,543 patients completed and returned it. Among these, 8,303 also completed questions related to alcohol use and are, thus, included in these analyses. The ACQUIP protocol was approved by the Institutional Review Board at each participating site and the secondary analyses presented here were approved by the University of Washington Human Subjects Division and the VA Puget Sound Institutional Review Board.
Measures
Assessment of Angina Symptoms
The Seattle Angina Questionnaire (SAQ) is a valid and reliable self-reported measure of angina and was used to assess self-reported angina symptoms (Spertus et al., 1994; Spertus et al., 1995). The SAQ consists of 5 domains: 1) physical limitation due to angina; 2) angina frequency; 3) angina instability; 4) satisfaction with treatment of angina; and 5) perception of angina effects on quality of life. For most questions, respondents are asked to rate their symptoms over the past 4 weeks using a 5-point Likert scale. For example, in the physical limitation domain, subjects are asked to rate their limitation due to chest pain, chest tightness, or angina over the past 4 weeks for 9 activities (including daily activities such as showering and dressing, moderate activity such as walking a flight of stairs, and strenuous activity such as jogging or moving heavy objects) on a scale ranging from “not at all limited” to “extremely limited.” Scores in each domain are then transformed to a scale of 0 to 100, with lower scores reflecting greater angina symptoms and worse function. Minimally important clinical differences were defined for SAQ subscores as 8 or more for physical limitation, 20 or more for frequency, and 25 or more for stability (Weintraub et al., 2008). We selected three scales of interest a priori in order to capture patient experience of symptoms that are predictive of clinical outcomes of angina. These included: 1) physical limitation due to angina, which consistently predicted death among patients regardless of differences in age, race or comorbidities (Mozaffarian et al., 2003); 2) angina frequency, which has been used as a measure of successful treatment in chronic stable angina (Wiest et al., 2004); and 3) angina instability, which has also been associated with mortality (Mozaffarian et al., 2003).
Alcohol Use Disorders Identification Test-Consumption (AUDIT-C) Questionnaire
The AUDIT-C is a three-item alcohol screening questionnaire (Table I), which identifies patients with the spectrum of unhealthy alcohol use from drinking above national recommended limits to meeting diagnostic criteria for alcohol use disorders (Saitz, 2005). The AUDIT-C has been validated in male and female veterans (Bradley et al., 2003; Bush et al., 1998) as well as in a general U.S. primary care population (Bradley et al., 2007), a representative general national sample (Dawson et al., 2005), and in European populations (Aertgeerts et al., 2001; Rumpf et al., 2002). The AUDIT-C is scored from 0 to 12 and also serves as a measure of alcohol use severity, with higher scores’ representing greater alcohol use severity (Bradley et al., 2004; Rubinsky et al., 2013; Rubinsky et al., 2010). Optimal screening thresholds for detecting unhealthy alcohol use in women and men are scores of ≥3 and ≥4 points, respectively (Bradley et al., 2003; Bradley et al., 2007; Bush et al., 1998).
Table 1.
The AUDIT-C and Scoring System (Total AUDIT-C scores range from 0-12)
|
Assessment of Covariates
Demographics
Patient age and gender were extracted from the EHR. Education (highest level or grade of school completed) and income (average total yearly) were both assessed on the baseline ACQUIP questionnaire. A combination of self-report and EHR data was used to identify patients’ race/ethnicity.
Smoking
Smoking status (never, current, past), intensity (cigarettes per day for current smokers), and recency (years since quit for former smokers) were also ascertained by questionnaire.
Comorbid Conditions
The ACQUIP “Health Checklist” included validated health screening instruments as well as assessments of prior diagnoses for medical conditions common to veterans. Diabetes, congestive heart failure, myocardial infarction, coronary revascularization, hypertension, renal disease, and pulmonary disease were included in the list of self-reported conditions and used for adjustment as in prior work (Mozaffarian et al., 2003). Depression was also assessed on the “Health Checklist” via the Mental Health Inventory (MHI-5), which is a 5-item questionnaire of current depressive symptoms from the Medical Outcomes Study. Scores on the MHI-5 range from 5 to 30, and scores > 17 indicate a positive screen for depression (Berwick et al., 1991).
Analyses
The AUDIT-C score was divided into six categories (alcohol use groups) for analyses, which reflect increasing alcohol consumption (Rubinsky et al., 2013). Alcohol use groups include AUDIT-C scores of 0, 1–3, 4–5, 6–7, 8–9, and 10–12, corresponding to non-drinking, low-level drinking, and mild, moderate, severe, and very severe unhealthy alcohol use, respectively. Categories were chosen for comparability to prior work (Au et al., 2007; Bryson et al., 2008; Greene et al., 2008; Harris et al., 2009; Kinder et al., 2009; Williams et al., 2010) and in order to provide adequate model flexibility.
Because age is strongly associated with AUDIT-C (Au et al., 2007; Rubinsky et al., 2013), all analyses and comparisons are presented at least adjusted for age. Descriptive analyses were directly adjusted for age in quintiles (24-58, 59–65, 66-70, 71-75, and 76-90 years) using the entire population as the referent standard, and p-values for comparisons are derived from likelihood tests with the same adjustment. For each of the three SAQ domains (physical function, frequency, and stability), linear regression models were fit to estimate mean domain scores for each alcohol use group. Regression models were first age-adjusted (age-adjusted model) and then adjusted for all potential confounders including age, race, education, income, smoking status and intensity, depression screening results, diabetes, congestive heart failure, myocardial infarction, coronary revascularization, hypertension, renal disease, and pulmonary disease (fully-adjusted model).
Mean domain scores and 95% confidence intervals are presented across alcohol use groups graphically for both the age- and fully-adjusted models. As above, adjustment was made to the population mean using the entire CAD cohort as a referent group for linear variables such as age, or standardized to the CAD population prevalence using the entire CAD cohort as a referent group for categorical variables, such as smoking. Relationships between the AUDIT-C and angina symptoms were tested for linear trends among drinkers (AUDIT-C categories 1 to 3 through 10+) and for quadratic trends with a linear and quadratic term. Post estimation F-tests evaluated pairwise comparisons of alcohol use groups estimates. All analyses were performed using Stata Version 9.2 (StataCorp., 2005).
RESULTS
Among all participants (n=8,303), the mean age was 66.4 years. Age-adjusted demographic and health history characteristics are presented by AUDIT-C category in Table 2. Respondents were mostly older, white, and male, similar to most VA populations. Significant differences existed across AUDIT-C groups for all characteristics. Those with very severe unhealthy alcohol use (AUDIT-C = 10-12) had a greater proportion of men and smaller proportions of white and married participants than those with non-drinking (AUDIT-C = 0).
Table 2.
Age-Adjusted Characteristics of VA Outpatients with Coronary Artery Disease by Alcohol Use Groups*
| Alcohol Use Groups
|
|||||||
|---|---|---|---|---|---|---|---|
| Non-Drinking
|
Low-level Drinking
|
Mild Unhealthy Use
|
Moderate Unhealthy Use
|
Severe Unhealthy Use
|
Very Severe Unhealthy Use
|
p-value†
|
|
| N | 4427 | 2451 | 800 | 312 | 170 | 143 | |
| % | 53.3 | 29.5 | 9.6 | 3.8 | 2.1 | 1.7 | |
| Characteristics | |||||||
| Age in quintiles | |||||||
| 24 to 58 | 17.2 | 20.3 | 22.2 | 36.7 | 41.2 | 54.9 | |
| 59 to 65 | 20.3 | 20.6 | 20.9 | 24.8 | 26.5 | 19.0 | |
| 66 to 70 | 20.5 | 18.7 | 16.5 | 17.4 | 21.2 | 12.0 | |
| 71 to 75 | 22.7 | 22.3 | 24.7 | 12.9 | 7.7 | 8.5 | |
| 76 to 90 | 19.4 | 18.2 | 15.7 | 8.4 | 3.5 | 5.6 | <0.001 |
| Male | 98.4 | 98.6 | 99.3 | 99.8 | 99.6 | 99.6 | 0.003 |
| White | 84.4 | 82.9 | 83.2 | 77.4 | 80.0 | 80.5 | 0.024 |
| Married | 68.9 | 66.7 | 63.4 | 52.2 | 46.6 | 39.8 | <0.001 |
| Cancer | 13.6 | 11.1 | 11.4 | 14.5 | 12.2 | 12.9 | 0.036 |
| CAD | 47.1 | 47.5 | 45.4 | 39.5 | 41.6 | 28.4 | <0.001 |
| Heart failure | 21.3 | 17.2 | 15.2 | 17.6 | 13.8 | 10.7 | <0.001 |
| Hypertension | 63.7 | 62.8 | 60.9 | 69.8 | 71.5 | 64.8 | 0.022 |
| Diabetes | 31.0 | 26.0 | 16.0 | 18.1 | 13.4 | 16.4 | <0.001 |
| Heart attack | 53.0 | 50.1 | 51.5 | 49.5 | 43.8 | 40.5 | 0.005 |
| Stroke | 19.1 | 13.8 | 11.6 | 11.7 | 16.1 | 15.9 | <0.001 |
| Liver disease | 7.7 | 5.0 | 8.0 | 9.5 | 13.5 | 18.7 | <0.001 |
| Revascularization | 50.4 | 53.5 | 48.3 | 51.8 | 42.1 | 37.0 | 0.0002 |
| Depression | 29.6 | 24.3 | 24.2 | 26.4 | 26.0 | 44.5 | <0.001 |
| Kidney Disease | 16.6 | 13.4 | 10.5 | 13.2 | 11.4 | 19.2 | <0.001 |
| Education | |||||||
| Less than high school | 38.7 | 24.0 | 24.6 | 36.8 | 40.5 | 47.5 | |
| High school graduate | 52.3 | 59.4 | 57.2 | 52.7 | 54.3 | 42.0 | |
| College grad | 9.0 | 16.6 | 18.2 | 10.5 | 5.2 | 10.6 | <0.001 |
| Smoking status | |||||||
| Never | 18.5 | 14.8 | 11.6 | 6.7 | 14.8 | 13.7 | |
| Past | 64.4 | 67.3 | 62.9 | 60.7 | 46.0 | 32.8 | |
| Current smoker | 17.1 | 17.9 | 25.5 | 32.6 | 39.2 | 53.5 | <0.001 |
| Income | |||||||
| <20k | 70.9 | 59.9 | 59.3 | 68.6 | 76.4 | 74.5 | |
| 20-39k | 25.0 | 31.0 | 28.9 | 23.6 | 20.9 | 21.3 | |
| >=40k | 4 | 9.1 | 11.9 | 7.8 | 2.7 | 4.3 | <0.001 |
| MHI-5(mean scores) | 13.4 | 12.6 | 12.5 | 13.4 | 13.6 | 16.9 | <0.001 |
| Cigarettess/per day | |||||||
| 0-0.75packs | 33.0 | 36.4 | 36.5 | 29.8 | 24.3 | 13.1 | |
| 0.75-1.5packs | 47.4 | 51.1 | 51.9 | 54.2 | 54.1 | 54.5 | |
| 1.5 or more | 19.6 | 12.5 | 11.6 | 16.0 | 21.6 | 32.4 | <0.001 |
| Years since quit smoking | |||||||
| <5 years | 18.6 | 18.5 | 18.0 | 26.8 | 24.7 | 26.5 | |
| 6-10 years | 13.5 | 14.3 | 13.9 | 12.9 | 8.9 | 20.8 | |
| >10 years | 67.9 | 67.2 | 68.1 | 60.3 | 66.3 | 52.7 | 0.24 |
Adjusted for age in quintiles
p-values derived from likelihood tests
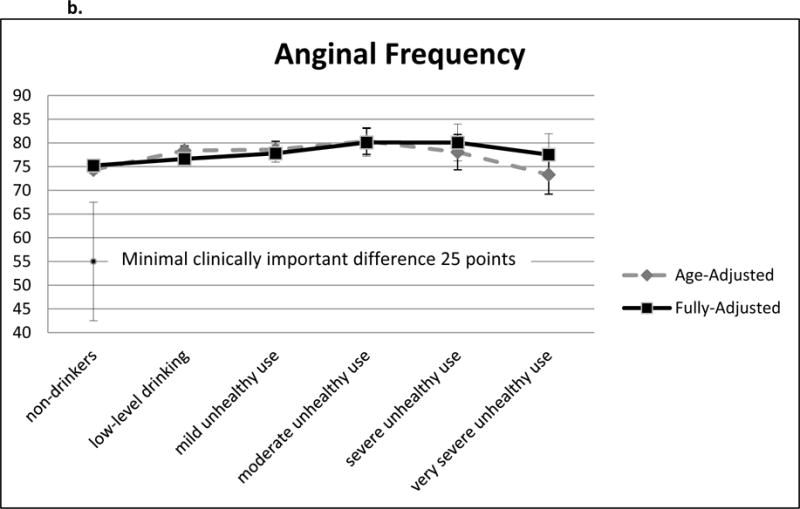
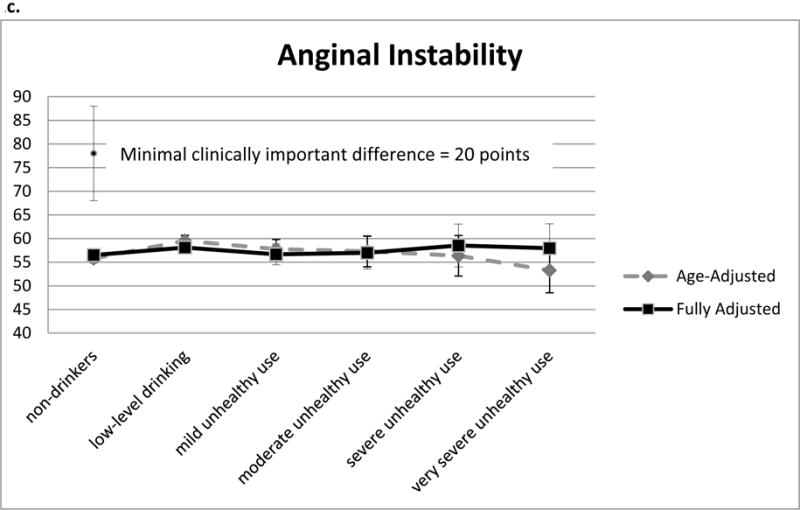
In age-adjusted analyses (dotted gray line in Figures), significant quadratic (inverted U-shaped) association was observed between alcohol use groups and all three domains of angina symptoms such that patients with non-drinking and very severe unhealthy alcohol use reported the greatest angina symptoms and lowest functioning (p< 0.001 for quadratic terms in each model). Additionally, for all three domains, patients with low level drinking and with mild unhealthy alcohol use reported the least angina symptoms and highest functioning in age-adjusted analyses.
Figure 1.
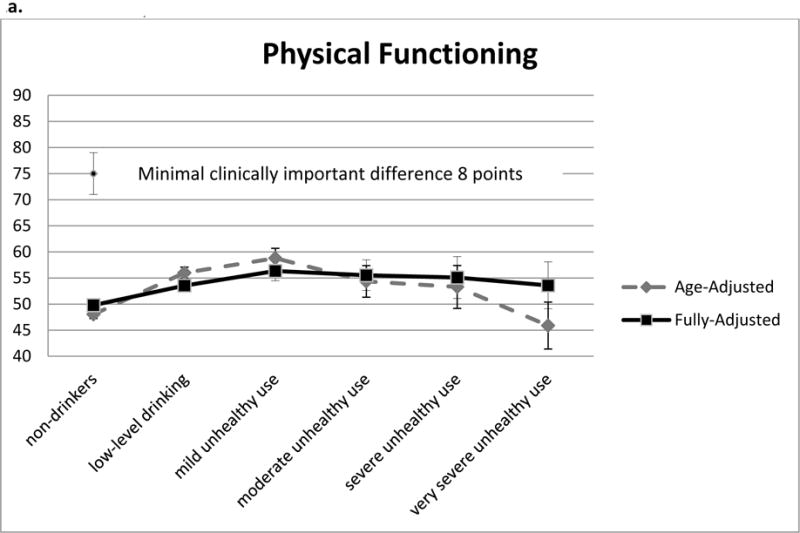
a. Age- and Fully-Adjusted* Mean Score on Physical Limitation Due to Angina by Alcohol Use Groups
b. Age- and Fully-Adjusted* Mean Score on Angina Frequency by Alcohol Use Groups
c. Age- and Fully-Adjusted* Mean Score on Angina Instability by Alcohol Use Groups
*fully adjusted model includes age, race, education, income, smoking status and intensity, depression screening results, diabetes, congestive heart failure, myocardial infarction, coronary revascularization, hypertension, renal disease, and pulmonary disease.
Full adjustment (black line in Figures) attenuated the U-shaped relationship observed in age-adjusted analyses for all three domains of angina symptoms. After full adjustment, patients categorized as non-drinkers had significantly worse functioning and greater severity and frequency of angina than those with low-level drinking, but those with very severe unhealthy alcohol use did not differ significantly from those with low-level drinking. Further, compared to patients with low-level drinking, patients with mild unhealthy alcohol use reported significantly higher physical functioning and patients with moderate unhealthy alcohol use reported significantly less frequency of angina symptom. No other significant differences between those with low-level drinking and other groups were observed in fully-adjusted analyses.
DISCUSSION
Age-adjusted models of the association between alcohol use groups and angina symptoms identified an inverted U-shaped relationship with non-drinkers and very heavy drinkers reporting the greatest angina severity and frequency and the lowest physical functioning. These findings are generally consistent with a large body of literature on alcohol use and other cardiovascular outcomes(Bradley and Merrill, 1999; Gunzerath et al., 2004; Shaper et al., 1988; Shaper and Wannamethee, 2000; Stockwell et al., 2016; Toma et al., 2017. This “U” or “J” shaped pattern of risk is thought to reflect higher rates of abstinence and comorbidity among “sick quitters” or previous heavy drinkers, unmeasured confounding, and possible beneficial effects of alcohol use {Toma, 2017 #12511). After complete adjustment, non-drinkers had somewhat more severe angina symptoms compared to drinkers. Our measure of alcohol use—a validated screening instrument with a past-year timeframe—does not allow differentiation of prior drinkers from lifelong abstainers. Therefore, it is unknown whether the observed differences between non-drinkers and patients who drink is due to continued unmeasured confounding or a potential beneficial effect of drinking (Ronksley et al., 2011; Shaper, 1993; Shaper et al., 1987). This healthy drinker or “sick quitter” effect is not specific to angina symptoms (Stockwell et al., 2016) and does not support a direct causal relationship between low-level (sometimes called “moderate”)(Stockwell et al., 2016) drinking and reduction in either the occurrence or the severity of angina symptoms.
Of the 3 symptom scales assessed, only the physical function scale had significant differences between drinkers and nondrinkers after full adjustment. These statistical differences were not clinically significant, as defined by a change of 8 or more points (Weintraub et al., 2008). The largest difference (~ 7 points) was between patients reporting non-drinking and those reporting mild unhealthy alcohol use, a level known to be associated with adverse outcomes, including decreased adherence to medications for hypertension and hyperlipidemia (Bryson et al., 2008), increased risks of fractures and trauma (Harris et al., 2009), and a higher risk of liver disease, upper GI bleeding, or pancreatitis among those under 50 (Au et al., 2007). There were no clinically important differences in the frequency scale after full adjustment, and there were no statistically significant differences in the stability scale.
While many studies have assessed associations between alcohol use and clinical cardiovascular outcomes (Ronksley et al., 2011), few specifically examine the association between angina and alcohol use, and none have assessed associations between alcohol use and self-reported angina symptoms. The Physicians’ Health Study (PHS) examined the relationship between incident angina and alcohol use. Compared with nondrinkers in PHS, low-level alcohol use (5 to 6 drinks per week) or higher was associated with a decreased incidence of any first diagnosis of angina over 11 years of follow up in male physicians. The relative risk of new angina for drinkers versus nondrinkers ranged from 0.74 (95% CI 0.60-0.90) for low-level drinkers down to 0.44 (0.29-0.66) for heavy drinkers consuming 14 or more drinks per week, levels of consumption which were also associated with increased risks of cancer in the same study. Compared to our analyses, the PHS analyses were additionally adjusted for exercise and aspirin use, but did not adjust for sociodemographic factors in this largely homogenous group of male physicians, or for the presence of other coexisting diseases such as hypertension, depression, pulmonary disease, or history of heart failure (Camargo et al., 1997a). More recently, a study of the CAREMA cohort in the Netherlands investigated the association between levels of alcohol use and incident angina (Merry et al., 2011). In this study, only regular drinking (defined as ≥ 1 glasses/week) relative to never drinking was associated with decreased risk of angina (0.66, 95% CI 0.45 – 0.95), but this difference was attenuated after adjustment for sociodemographic characteristics and other risk factors, and no significant differences across levels of alcohol use were observed (Merry et al., 2011).
Our study examined the burden of angina symptomatology among VA patients previously diagnosed with CAD. Among this group of largely older men, we did not find clinically significant differences in angina symptoms after complete adjustment in key angina domains that are predictive of clinical outcomes of CAD (Mozaffarian et al., 2003), including physical function, frequency, or stability of angina. Solely age-adjusted models displayed very modest U-shaped relationship between alcohol use and angina symptoms, but further adjustment for confounding variables removed any clinically significant relationship between alcohol use and angina symptoms. The American Heart Association has commented on alcohol consumption and heart disease (American Heart Association, 2017; Bradley and Merrill, 1999) and concludes that while there is observational evidence that supports a protective effect for mild to moderate drinking, there is debate whether this is causal, and remains a subject that is important for physicians and patients to discuss on an individual basis. A recent summary of the literature suggests that new research raises concern that even low-moderate alcohol use may not offer cardio-protective effects (Toma et al., 2017), and a recent meta-analysis of observational studies of the association between alcohol use and all-cause mortality adjusted for study design characteristics known to bias results and found no protective effect of low-level drinking (Stockwell et al., 2016). While we found small, statistically significant differences in angina symptoms between all groups of drinkers and nondrinkers in age-adjusted models, in fully adjusted models, no evidence of a protective or significant salutary effect of drinking on patient experiences of angina were observed. Further, the one clinically significant difference in less physical limitation for angina adjusted only for age occurred at a level of alcohol use that is known to be associated with other negative outcomes. While our study was observational and cross-sectional (limiting causal inference), our findings do not support a protective effect of alcohol use on patient experience of angina—in three key domains that predict clinical outcomes of CAD—and add to growing literature that low-level alcohol use may not have beneficial effects on cardiovascular outcomes(Stockwell et al., 2016; Toma et al., 2017).
This study has limitations. The AUDIT-C is a validated screening instrument that is widely used (Bradley et al., 2006) and correlates well with alcohol use and severity of alcohol use (Rubinsky et al., 2013; Rubinsky et al., 2010). However, it is not a detailed alcohol consumption questionnaire. The AUDIT-C has been associated in a graded fashion with many medical outcomes ranging from medication adherence (Bryson et al., 2008) to mortality (Harris et al., 2010; Kinder et al., 2009). While our population consisted of VA patients and may lack generalizability, there is no reason to believe that there would be biological differences in the relationship between alcohol use and angina symptoms between this sample and men in the general population. Similarly, the unique data used in this study were collected between 1997 and 2000. While it is possible that associations between alcohol use and angina symptoms change over time, it is unlikely that results would differ in a later sample. Additionally, angina symptoms and alcohol use were both assessed at baseline, and this cross-sectional data does not address whether prior alcohol use inhibits the development of angina over time. Drinking patterns could change after patients develop angina, and therefore obscure a protective relationship between alcohol use and angina symptoms, but report of use in the past year, after adjustment, does not appear to be associated with angina symptoms as measured by the SAQ. Finally, this study relied almost entirely on self-report data. While our measure of self-reported CAD has very high (>90%) sensitivity and specificity relative to chart review,(Spertus et al., 2000) and the AUDIT-C and SAQ are both validated measures, it is possible that results are subject to social desirability and/or recall bias. These biases would have resulted in misclassification, which could have tempered results (e.g., if patients were categorized into lower drinking categories than that reflecting true past-year drinking, it may have elevated SAQ scores at lower levels of drinking). However, self-report is also a key strength of this study because we were able to assess patient-reported experiences of domains of angina that influence key clinical outcomes (Mozaffarian et al., 2003). Additional strengths help to outweigh the limitations. Specifically, this study included a relatively large group of patients with CAD that also had an adequate prevalence of any and unhealthy alcohol use to allow greater than 99% power to detect a clinically significant 8 point difference in angina symptoms across alcohol use groups. While the lack of statistically or clinically significant differences due to chance alone is possible, it is highly improbable.
CONCLUSIONS
There are very few studies that examine the association between alcohol use and the experience of angina among patients with CAD, and there is current uncertainty about the role of alcohol use in the prevention or amelioration of CAD and its symptoms. In this large study of men, we found that there were no clinically significant differences in angina symptoms associated with alcohol use after adjustment for important confounding variables, and no support that alcohol use is strongly associated with angina symptoms.
Acknowledgments
Funding Sources: This work was funded by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development IAC 05-206. The ACQUIP was funded by Department of Veterans Affairs grants SDR 96-002 and IIR 99-376. Dr. Williams is supported by a Career Development Award from VA Health Services Research & Development (CDA 12-276), and Dr. Bradley is supported by a mid-career mentorship award from NIAAA (K24-AA022128). Dr. Bryson was supported by Department of Veterans Affairs, Veterans Health Administration, Health Services Research & Development Career Development Award (RCD 03-177).
Footnotes
Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs, the University of Washington, or the Kaiser Permanente Washington Health Research Institute.
Disclosures: None to report.
References
- Aertgeerts B, Buntinx F, Ansoms S, Fevery J. Screening properties of questionnaires and laboratory tests for the detection of alcohol abuse or dependence in a general practice population. Br J Gen Pract. 2001;51(464):206–217. [PMC free article] [PubMed] [Google Scholar]
- American Heart Association. Alcohol and Heart Health. 2017 http://www.heart.org/HEARTORG/HealthyLiving/HealthyEating/Nutrition/Alcohol-and-Heart-Health_UCM_305173_Article.jsp#.WOGQCTZMS2w accessed April 2017.
- Au DH, Kivlahan DR, Bryson CL, Blough D, Bradley KA. Alcohol screening scores and risk of hospitalizations for GI conditions in men. Alcohol Clin Exp Res. 2007;31(3):443–451. doi: 10.1111/j.1530-0277.2006.00325.x. [DOI] [PubMed] [Google Scholar]
- Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991;29(2):169–176. doi: 10.1097/00005650-199102000-00008. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Bush KR, Epler AJ, Dobie DJ, Davis TM, Sporleder JL, Maynard C, Burman ML, Kivlahan DR. Two brief alcohol-screening tests from the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003;163(7):821–829. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31(7):1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Kivlahan DR, Zhou XH, Sporleder JL, Epler AJ, McCormick KA, Merrill JO, McDonell MB, Fihn SD. Using alcohol screening results and treatment history to assess the severity of at-risk drinking in Veterans Affairs primary care patients. Alcohol Clin Exp Res. 2004;28(3):448–455. doi: 10.1097/01.alc.0000117836.38108.38. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Merrill JO. Doctor, is wine good for my heart? Lancet. 1999;353(9167):1815–1816. doi: 10.1016/S0140-6736(99)90188-5. [DOI] [PubMed] [Google Scholar]
- Bradley KA, Williams EC, Achtmeyer CE, Volpp B, Collins BJ, Kivlahan DR. Implementation of evidence-based alcohol screening in the Veterans Health Administration. Am J Manag Care. 2006;12(10):597–606. [PubMed] [Google Scholar]
- Bryson CL, Au DH, Sun H, Williams EC, Kivlahan DR, Bradley KA. Alcohol screening scores and medication nonadherence. Ann Intern Med. 2008;149(11):795–804. doi: 10.7326/0003-4819-149-11-200812020-00004. [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP) Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Camargo CA, Hennekens CH, Gaziano JM, Glynn RJ, Manson JE, Stampfer MJ. Prospective study of moderate alcohol consumption and mortality in US male physicians. Arch Intern Med. 1997a;157(1):79–85. [PubMed] [Google Scholar]
- Camargo CA, Stampfer MJ, Glynn RJ, Grodstein F, Gaziano JM, Manson JE. Moderate alcohol consumption and risk for angina pectoris or myocardial infarction in U.S. male physicians. Ann Intern Med. 1997b;126:372–375. doi: 10.7326/0003-4819-126-5-199703010-00005. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, Zhou Y. Effectiveness of the derived Alcohol Use Disorders Identification Test (AUDIT-C) in screening for alcohol use disorders and risk drinking in the US general population. Alcohol Clin Exp Res. 2005;29(5):844–854. doi: 10.1097/01.alc.0000164374.32229.a2. [DOI] [PubMed] [Google Scholar]
- Diamond I. Alcoholic myopathy and cardiomyopathy. N Engl J Med. 1989;320:458–459. doi: 10.1056/NEJM198902163200709. [DOI] [PubMed] [Google Scholar]
- Fernandez-Sola J, Estruch R, Grau JM, Pare JC, Rubin E, Urbano-Marquez A. The relation of alcoholic myopathy to cardiomyopathy. Ann Intern Med. 1994;120:529–536. doi: 10.7326/0003-4819-120-7-199404010-00001. [DOI] [PubMed] [Google Scholar]
- Fihn SD, McDonell MB, Diehr P, Anderson SM, Bradley KA, Au DH, Spertus JA, Burman M, Reiber GE, Kiefe CI, Cody M, Sanders KM, Whooley MA, Rosenfeld K, Baczek LA, Sauvigne A. Effects of sustained audit/feedback on self-reported health status of primary care patients. Am J Med. 2004;116(4):241–248. doi: 10.1016/j.amjmed.2003.10.026. [DOI] [PubMed] [Google Scholar]
- Gemes K, Janszky I, Laugsand LE, Laszlo KD, Ahnve S, Vatten LJ, Mukamal KJ. Alcohol consumption is associated with a lower incidence of acute myocardial infarction: results from a large prospective population-based study in Norway. J Intern Med. 2016;279(4):365–375. doi: 10.1111/joim.12428. [DOI] [PubMed] [Google Scholar]
- Greene CC, Bradley KA, Bryson CL, Blough DK, Evans LE, Udris EM, Au DH. The association between alcohol consumption and risk of COPD exacerbation in a veteran population. Chest. 2008;134(4):761–767. doi: 10.1378/chest.07-3081. [DOI] [PubMed] [Google Scholar]
- Gunzerath L, Faden V, Zakhari S, Warren K. National institute on alcohol abuse and alcoholism report on moderate drinking. Alcohol Clin Exp Res. 2004;28(6):829–847. doi: 10.1097/01.alc.0000128382.79375.b6. [DOI] [PubMed] [Google Scholar]
- Harris AH, Bradley KA, Bowe T, Henderson P, Moos R. Associations between AUDIT-C and mortality vary by age and sex. Popul Health Manag. 2010;13(5):263–268. doi: 10.1089/pop.2009.0060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris AH, Bryson CL, Sun H, Blough D, Bradley KA. Alcohol screening scores predict risk of subsequent fractures. Subst Use Misuse. 2009;44(8):1055–1069. doi: 10.1080/10826080802485972. [DOI] [PubMed] [Google Scholar]
- Kinder LS, Bryson CL, Sun H, Williams EC, Bradley KA. Alcohol screening scores and all-cause mortality in male Veterans Affairs patients. J Stud Alcohol Drugs. 2009;70(2):253–260. doi: 10.15288/jsad.2009.70.253. [DOI] [PubMed] [Google Scholar]
- Klatsky AL. Epidemiology of coronary heart disease – influence of alcohol. Alcohol Clin Exp Res. 1994;18:88–96. doi: 10.1111/j.1530-0277.1994.tb00886.x. [DOI] [PubMed] [Google Scholar]
- Klatsky AL, Friedman G, Siegelaub AB. Alcohol consumption and blood pressure. N Engl J Med. 1977;296:1194–1200. doi: 10.1056/NEJM197705262962103. [DOI] [PubMed] [Google Scholar]
- Klatsky AL, Friedman GD, Siegelaub AB. Alcohol consumption before myocardial infarction. Ann Intern Med. 1974;81:294–301. doi: 10.7326/0003-4819-81-3-294. [DOI] [PubMed] [Google Scholar]
- Koskinen P, Kupari M. Alcohol consumption of patients with supraventricular tachyarrhythmias other than atrial fibrillation. Alcohol Alcohol. 1991;26(2):199–206. doi: 10.1093/oxfordjournals.alcalc.a045101. [DOI] [PubMed] [Google Scholar]
- Li JM, Mukamal KJ. An update on alcohol and atherosclerosis. Curr Opin Lipidol. 2004;15(6):673–680. doi: 10.1097/00041433-200412000-00008. [DOI] [PubMed] [Google Scholar]
- Maki T, Toivonen L, Koskinen P, Naveri H, Harkonen M, Leinonen H. Effect of ethanol drinking, hangover, and exercise on adrenergic activity and heart rate variability in patients with a history of alcohol-induced atrial fibrillation. Am J Cardiol. 1998;82(3):317–322. doi: 10.1016/s0002-9149(98)00299-9. [DOI] [PubMed] [Google Scholar]
- Makita S, Onoda T, Ohsawa M, Tanaka F, Segawa T, Takahashi T, Satoh K, Itai K, Tanno K, Sakata K, Omama S, Yoshida Y, Ishibashi Y, Koyama T, Kuribayashi T, Ogasawara K, Ogawa A, Okayama A, Nakamura M. Influence of mild-to-moderate alcohol consumption on cardiovascular diseases in men from the general population. Atherosclerosis. 2012;224(1):222–227. doi: 10.1016/j.atherosclerosis.2012.07.004. [DOI] [PubMed] [Google Scholar]
- Merry AH, Boer JM, Schouten LJ, Feskens EJ, Verschuren WM, Gorgels AP, van den Brandt PA. Smoking, alcohol consumption, physical activity, and family history and the risks of acute myocardial infarction and unstable angina pectoris: a prospective cohort study. BMC Cardiovasc Disord. 2011;11:13. doi: 10.1186/1471-2261-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozaffarian D, Bryson CL, Spertus JA, McDonell MB, Fihn SD. Anginal symptoms consistently predict total mortality among outpatients with coronary artery disease. Am Heart J. 2003;146(6):1015–1022. doi: 10.1016/S0002-8703(03)00436-8. [DOI] [PubMed] [Google Scholar]
- Peytremann-Bridevaux I, Bradley KA, Bryson CL, McDonell MB, Fihn SD. Alcohol screening results in elderly male veterans: association with health status and mortality. J Am Geriatr Soc. 2004;52(9):1510–1517. doi: 10.1111/j.1532-5415.2004.52414.x. [DOI] [PubMed] [Google Scholar]
- Puddey IB, Rakic V, Dimmitt SB, Beilin LJ. Influence of pattern of drinking on cardiovascular disease and cardiovascular risk factrs–a review. Addiction. 1999;94(5):649–663. doi: 10.1046/j.1360-0443.1999.9456493.x. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos CT. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease: an overview. Addiction. 2003;98:1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- Rich EC, Siebold C, Campion B. Alcohol-related acute atrial fibrillation. A case-control study and review of 40 patients. Arch Intern Med. 1985;145(5):830–833. doi: 10.1001/archinte.145.5.830. [DOI] [PubMed] [Google Scholar]
- Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinsky AD, Dawson DA, Williams EC, Kivlahan DR, Bradley KA. AUDIT-C scores as a scaled marker of mean daily drinking, alcohol use disorder severity, and probability of alcohol dependence in a U.S. general population sample of drinkers. Alcohol Clin Exp Res. 2013;37(8):1380–1390. doi: 10.1111/acer.12092. [DOI] [PubMed] [Google Scholar]
- Rubinsky AD, Kivlahan DR, Volk RJ, Maynard C, Bradley KA. Estimating risk of alcohol dependence using alcohol screening scores. Drug Alcohol Depend. 2010;108(1-2):29–36. doi: 10.1016/j.drugalcdep.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumpf HJ, Hapke U, Meyer C, John U. Screening for alcohol use disorders and at-risk drinking in the general population: psychometric performance of three questionnaires. Alcohol Alcohol. 2002;37(3):261–268. doi: 10.1093/alcalc/37.3.261. [DOI] [PubMed] [Google Scholar]
- Saitz R. Clinical practice. Unhealthy alcohol use. N Engl J Med. 2005;352(6):596–607. doi: 10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Shaper AG. Alcohol, the heart, and health. Am J Public Health. 1993;83(6):799–801. doi: 10.2105/ajph.83.6.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaper AG, Phillips AN, Pocock SJ, Walker M. Alcohol and ischaemic heart disease in middle aged British men. Br Med J (Clin Res Ed) 1987;294(6574):733–737. doi: 10.1136/bmj.294.6574.733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaper AG, Wannamethee G, Walker M. Alcohol and mortality in British men: explaining the U-shaped curve. Lancet. 1988;2(8623):1267–1273. doi: 10.1016/s0140-6736(88)92890-5. [DOI] [PubMed] [Google Scholar]
- Shaper AG, Wannamethee SG. Alcohol intake and mortality in middle aged men with diagnosed coronary heart disease. Heart. 2000;83(4):394–399. doi: 10.1136/heart.83.4.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smyth A, Teo KK, Rangarajan S, O’Donnell M, Zhang X, Rana P, Leong DP, Dagenais G, Seron P, Rosengren A, Schutte AE, Lopez-Jaramillo P, Oguz A, Chifamba J, Diaz R, Lear S, Avezum A, Kumar R, Mohan V, Szuba A, Wei L, Yang W, Jian B, McKee M, Yusuf S, Investigators, P. Alcohol consumption and cardiovascular disease, cancer, injury, admission to hospital, and mortality: a prospective cohort study. Lancet. 2015;386(10007):1945–1954. doi: 10.1016/S0140-6736(15)00235-4. [DOI] [PubMed] [Google Scholar]
- Spertus JA, Dewhurst TA, Dougherty CM, Nichol P, McDonell M, Bliven B, Fihn SD. Benefits of an “angina clinic” for patients with coronary artery disease: a demonstration of health status measures as markers of health care quality. Am Heart J. 2002;143(1):145–150. doi: 10.1067/mhj.2002.119894. [DOI] [PubMed] [Google Scholar]
- Spertus JA, McDonell M, Woodman CL, Fihn SD. Association between depression and worse disease-specific functional status in outpatients with coronary artery disease. Am Heart J. 2000;140(1):105–110. doi: 10.1067/mhj.2000.106600. [DOI] [PubMed] [Google Scholar]
- Spertus JA, Winder J, Dewhurst T, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol. 1994;74:1240–1244. doi: 10.1016/0002-9149(94)90555-x. [DOI] [PubMed] [Google Scholar]
- Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release Special Edition 9.2. Stata Corporation; College Station TX: 2005. [Google Scholar]
- Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do “Moderate” Drinkers Have Reduced Mortality Risk? A Systematic Review and Meta-Analysis of Alcohol Consumption and All-Cause Mortality. J Stud Alcohol Drugs. 2016;77(2):185–198. doi: 10.15288/jsad.2016.77.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toma A, Pare G, Leong DP. Alcohol and Cardiovascular Disease: How Much is Too Much? Curr Atheroscler Rep. 2017;19(3):13. doi: 10.1007/s11883-017-0647-0. [DOI] [PubMed] [Google Scholar]
- Urbano-Marquez A, Estruch R, Fernandez-Sola J, Nicolas JM, Pare JC, Rubin E. The greater risk of alcoholic cardiomyopathy and myopathy in women compared with men. JAMA. 1995;274(2):149–154. doi: 10.1001/jama.1995.03530020067034. [DOI] [PubMed] [Google Scholar]
- Vliegenthart R, Geleijnse J, Hofman A, Meijer WT, van Rooij F, Grobbee D, Witteman J. Alcohol consumption and risk of peripheral arterial disease: the Rotterdam study. Am J Epidemiol. 2002;155(4):332–338. doi: 10.1093/aje/155.4.332. [DOI] [PubMed] [Google Scholar]
- Weintraub WS, Spertus JA, Kolm P, Maron DJ, Zhang Z, Jurkovitz C, Zhang W, Hartigan PM, Lewis C, Veledar E, Bowen J, Dunbar SB, Deaton C, Kaufman S, O’Rourke RA, Goeree R, Barnett PG, Teo KK, Boden WE, Mancini GB. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med. 2008;359(7):677–687. doi: 10.1056/NEJMoa072771. [DOI] [PubMed] [Google Scholar]
- Wiest FC, Bryson CL, Burman M, McDonell MB, Henikoff JG, Fihn SD. Suboptimal pharmacotherapeutic management of chronic stable angina in the primary care setting. Am J Med. 2004;117(4):234–241. doi: 10.1016/j.amjmed.2004.02.044. [DOI] [PubMed] [Google Scholar]
- Williams EC, Peytremann-Bridevaux I, Fan VS, Bryson CL, Kivlahan DR, Bradley KA. The association between alcohol screening scores and health status in male veterans. J Addict Med. 2010;4(1):27–37. doi: 10.1097/ADM.0b013e3181a196b5. [DOI] [PubMed] [Google Scholar]


